Abstract
Purpose:
The American Society of Anesthesia practice guidelines recommend that pediatric and adult patients who undergo ambulatory surgery be screened for obstructive sleep apnea (OSA). With this in mind, our objective was to assess the frequency of screening by anesthesia providers for the signs and symptoms of OSA in children undergoing surgery in an ambulatory setting.
Methods:
Prospective single-blinded observational study of anesthesia providers' preoperative interview of caregivers of consecutive patients younger than age 18 who were scheduled for ambulatory surgery.
Results:
One hundred one children (30 females) were identified, with a mean age of 6.9 ± 5.0 years; 54 were classified as white, 33 as black, and 14 as other. Total OSA-18 scores ranged from 18 to 97, with a mean of 33.1 ± 14.8. The mean score for adenotonsillectomy patients was higher than that for children who underwent procedures other than adenotonsillectomy. Thirty-one percent of children were screened for OSA, and snoring was the most common symptom recorded (28%). Patients who were screened for OSA were more likely to have snoring (p < 0.001), known OSA (p = 0.006), and a scheduled adenotonsillectomy (p = 0.02).
Conclusion:
OSA was not routinely screened for by anesthesia providers prior to ambulatory pediatric surgery. When screening did occur, “snoring” was the most commonly recorded symptom. Paradoxically, patients with undiagnosed OSA who would benefit the most from screening were the least likely to be screened.
Commentary:
A commentary on this article appears in this issue on page 697.
Citation:
Ishman SL, Tawfik KO, Smith DF, Cheung K, Pringle LM, Stephen MJ, Everett TL, Stierer TL. Screening for pediatric obstructive sleep apnea before ambulatory surgery. J Clin Sleep Med 2015;11(7):751–755.
Keywords: screening, pediatric, OSA, sleep apnea, surgery, ambulatory, outpatient surgery
Although large epidemiologic studies estimate that the prevalence of pediatric obstructive sleep apnea (OSA) ranges from 1.2% to 5%,1–3 there is currently no literature on the prevalence of undiagnosed pediatric OSA. For children with known OSA, adenotonsillectomy has remained the first-line treatment, as the benefits of this procedure far outweigh its risks. In light of this, the American Society of Anesthesia (ASA) practice guidelines recommend that all pediatric and adult patients who undergo ambulatory surgery be screened for OSA.4 The objective of the present study was to assess the frequency of screening by anesthesia providers for the signs and symptoms of OSA in children undergoing ambulatory surgery.
METHODS
This study was conducted at the Johns Hopkins Hospital Outpatient Center. Consecutive patients younger than age 18 who were seen from July to October 2009 and scheduled for ambulatory surgery were eligible for inclusion. Patients with non-English speaking or hearing- or language-impaired care-givers were excluded.
BRIEF SUMMARY
Current Knowledge/Study Rationale: It is known that children with OSA are more likely to have perioperative complications than those without OSA. In light of this, the American Society of Anesthesia (ASA) practice guidelines recommend screening all patients for OSA.
Study Impact: In this blinded observational study, we found that anesthesia providers did not routinely screen for OSA prior to ambulatory pediatric surgery and patients with undiagnosed OSA who would benefit the most from screening, were the least likely to be screened. This suggests that anesthesia providers should be educated on the importance of screening children for OSA symptoms prior to surgery.
Specific terms related to the signs and symptoms of OSA were identified prior to initiation of the study (Figure 1). One of two nonmedical observers, unknown to the anesthesia providers, was present during the preoperative assessment of each study participant and was responsible for documenting the use of these terms during the assessment. Observations were carried out in a single-blinded fashion.
Figure 1. Terms and phrases screened for during preoperative evaluation in children undergoing ambulatory procedures.
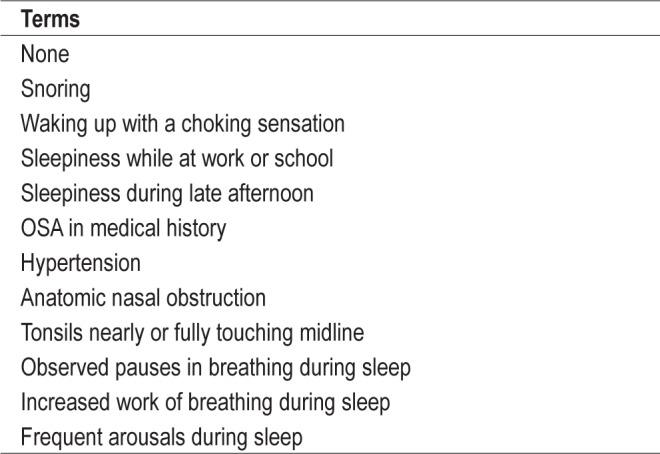
The following screening terms/phrases were never observed during preoperative evaluation: intermittent vocalization during sleep, easily distracted, behavioral problems, overly aggressive, difficulty concentrating, unusual awakening time, poor school performance, morning headaches, craniofacial anomalies affecting airway, odd posture while sleeping.
Before the preoperative assessment was completed by the anesthesia care team, a parent/caregiver of each study participant was asked by the observer to consent to the study and complete the OSA-18 sleep-specific quality of life survey.
The OSA-18
The OSA-18 is a validated disease-specific quality of life questionnaire designed for administration to parents of pediatric patients suspected of having OSA, which includes a number of symptom questions often recommended for screening of OSA including the presence of snoring and witnessed apneas. This questionnaire consists of 18 questions pertaining to 5 domains: sleep disturbance, physical distress, emotional distress, daytime problems, and caretakers' concerns. Parents are asked to rate the frequency of each listed symptom on a scale from 1 to 7; a total score, which can range from 18 to 126, is then calculated. This score has been correlated with nap polysomnography (PSG) results and reflects the impact of OSA on quality of life.5 A score < 60 suggests a small impact, scores between 60 and 80 correlate with a moderate impact, and scores > 80 indicate a large impact.
Statistical Analysis
OSA-18 scores were compared between children who underwent otolaryngology versus non-otolaryngology procedures. In addition, a subanalysis was carried out to compare those who underwent adenotonsillectomy with those who did not undergo this procedure. Because the populations being compared in both analyses were not normally distributed and did not have equal standard deviations, we used the nonparametric Kruskal-Wallis test to assess for differences in OSA-18 scores between groups. The Fisher exact test was used to assess differences in the frequency of screening for OSA in these same patient populations. Spearman rank order correlation was used to assess the correlation between continuous and categorical variables.
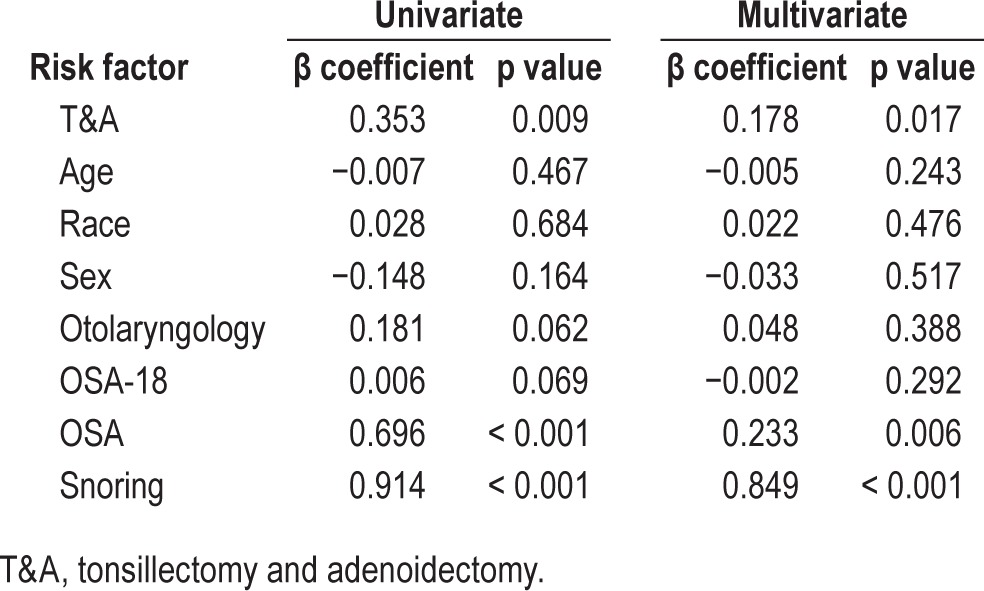
Univariable and multivariable logistic regression analysis was carried out to identify variables that predict the likelihood of being screened for any signs or symptoms of OSA. The variables evaluated included age, race, gender, snoring history, type of surgery, known OSA, and the total OSA-18 score. We defined statistical significance as α ≤ 0.05. This study was approved by the institutional review board of the Johns Hopkins School of Medicine.
RESULTS
One hundred one children (30 female) with a mean age of 6.9 ± 5.0 years (range 0.8–17.9 years) were included in the study; 54 were classified as white, 33 as black, and 14 as other. Fifteen (14.8%) patients underwent adenotonsillectomy; 2 of these patients were previously diagnosed with OSA. Thirty (29.7%) patients underwent otolaryngology procedures other than adenotonsillectomy; 1 was previously diagnosed with OSA. Fifty-six (55.4%) patients underwent non-otolaryngology procedures; 1 was previously diagnosed with OSA.
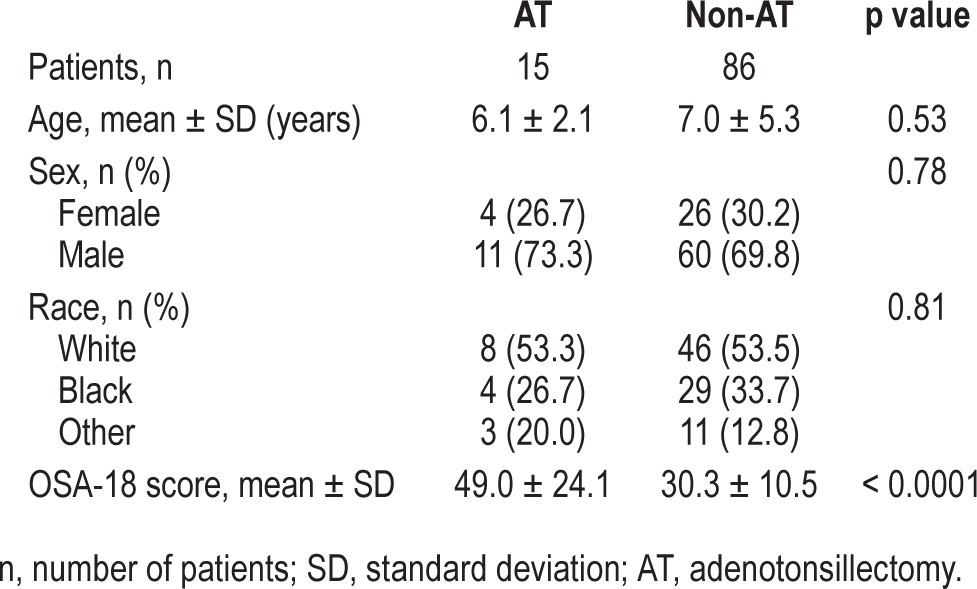
Total OSA-18 scores ranged from 18 to 97, with a mean of 33.1 ± 14.8. The mean score for adenotonsillectomy patients was 49.0 ± 13.1; this score was significantly higher than the score for patients who underwent otolaryngology procedures other than adenotonsillectomy (37.3 ± 13.1) and for those who underwent non-otolaryngology procedures (26.7 ± 6.5) (p < 0.0001 for both). Age, gender, and race did not differ significantly between patient populations in either analysis (Tables 1 and 2).
Table 1.
Baseline clinical characteristics for entire cohort and those undergoing otolaryngology versus nonotolaryngology procedures.
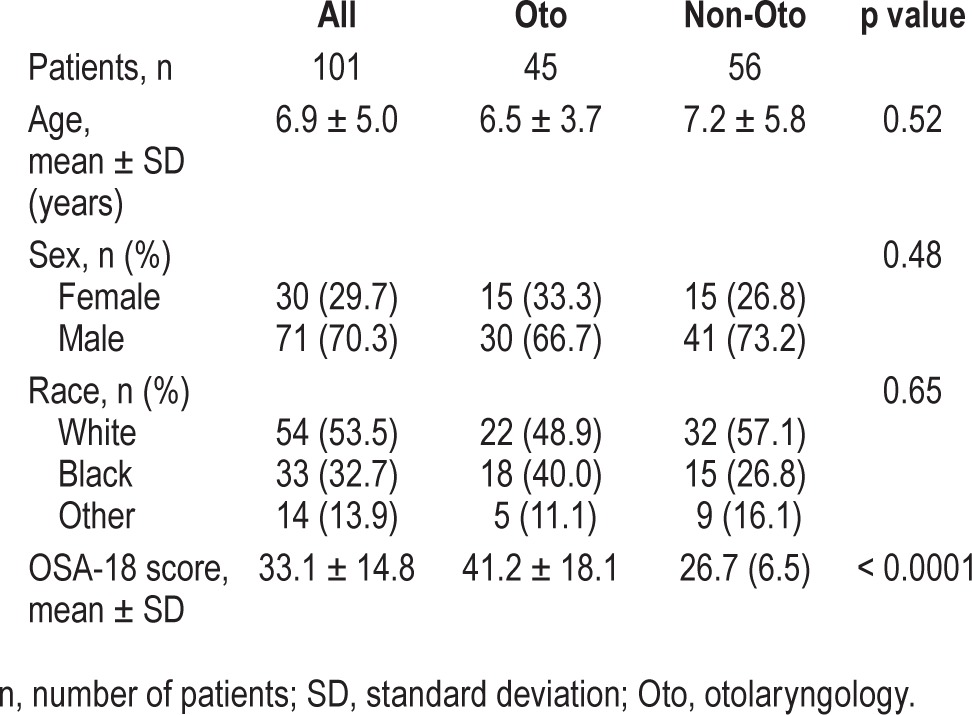
Table 2.
Baseline clinical characteristics for those undergoing adenotonsillectomy versus nonadenotonsillectomy procedures.
In the overall cohort, 37% of children were screened for OSA. Those who underwent otolaryngology procedures were more likely to be screened (47%) than those who underwent non-otolaryngology procedures (29%) (p = 0.0619). Patients who underwent AT were 2.1 times more likely to be screened for OSA than those who did not (p = 0.0092).
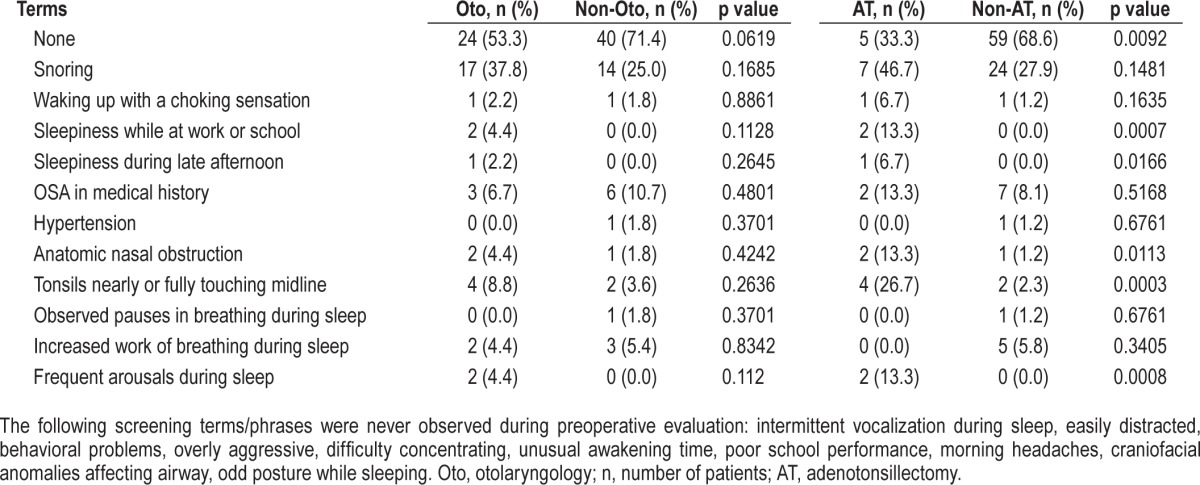
Observers identified “snoring” as the most common OSA-related screening term used by anesthesia providers during preoperative assessment (Table 3). The likelihood of screening for one or more OSA-related signs and symptoms was the same regardless of the patient population. Patients who underwent adenotonsillectomy were more likely to be screened for daytime sleepiness (p = 0.0007), sleepiness during late afternoon (p = 0.0166), anatomic nasal obstruction (p = 0.0113), severe tonsillar hypertrophy (p = 0.0003), and frequent arousals during sleep (p = 0.0008) than those who did not undergo adenotonsillectomy.
Table 3.
Frequency of use of screening terms and phrases during preoperative evaluation in patients undergoing otolaryngologic and non-otolaryngologic procedures.
As shown in Table 4, patients who were screened for OSA were more likely to have snoring, known OSA and a scheduled adenotonsillectomy when evaluated with both single (p < 0.001, p < 0.001, and p = 0.009, respectively) and multivariable (p < 0.001, p = 0.006, and p = 0.02, respectively) regression. There was no correlation between the likelihood of screening for any symptoms and the total OSA-18 score (p = 0.22), age (p = 0.48), race (p = 0.85), or gender (p = 0.16).
Table 4.
Regression analysis of variables predictive of preoperative screening for OSA prior to ambulatory surgery in children.
DISCUSSION
Our results suggest that anesthesia providers do not consistently screen for OSA in pediatric patients undergoing ambulatory surgery. We found that patients with a history of known OSA and those undergoing adenotonsillectomy were more likely to be screened during the preoperative encounter than children without known OSA or those undergoing other procedures. In children who were screened for OSA, anesthesia providers most commonly asked questions pertaining to snoring.
The ASA practice guidelines for the management of patients with OSA recommend that all adult and pediatric patients over 1 year of age, be screened for OSA prior to undergoing surgery. For patients in whom OSA is suspected, these guidelines recommend that questions regarding snoring, apnea, frequent arousals, morning headaches, and daytime sleepiness be included in the preoperative patient interview.4
The ASA guidelines are based on the premise that children and adults with OSA are at increased risk for perioperative morbidity and mortality.4 Specifically, an increased incidence of postoperative respiratory complications has been reported for children with known OSA at the time of surgery.6–15 In a review of 2,315 patients younger than 6 years of age who underwent adenotonsillectomy for obstructive breathing, 6.4% developed postoperative respiratory complications,12 including oxygen desaturation, apnea, or increased work of breathing; atelectasis; edema; pneumomediastinum; pneumothorax; and pleural effusion. Many of these complications required interventions such as insertion of a nasopharyngeal airway, continuous positive airway pressure, endotracheal intubation, and mechanical ventilation. The authors of this study suggest that preoperative screening for OSA may enable anesthesia providers to implement preparatory and intraoperative measures to minimize these risks.
Although studies in adults estimate that up to 80% of patients with OSA are undiagnosed,16 the prevalence of undiag-nosed pediatric OSA has not been investigated. Furthermore, investigations of the incidence of postoperative respiratory complications in pediatric patients with OSA are limited to cohorts undergoing adenotonsillectomy. The true risk of peri-operative complications that result from undiagnosed pediatric OSA is therefore unknown.
In our cohort, rates of screening for signs and symptoms associated with OSA were low. Even for children undergoing adenotonsillectomy or who had known OSA, symptom screening was not universal. Screening for OSA is intended to benefit patients with previously undiagnosed OSA. Paradoxically, these patients were the least likely to be screened in our study.
There were a number of limitations to our study. Our sample population was small; in turn, the frequency of positive findings was small. Given that we did not record the incidence of screening questions for disorders other than OSA, we cannot estimate the frequency with which anesthesiologists screen for other important medical conditions (e.g., asthma, chronic lung disease, malignant hyperthermia). Therefore, we cannot make conclusions as to whether failure to screen for OSA was attributable to a lack of awareness of OSA or to a more general lack of interest in screening for any medical condition that could influence perioperative decision-making in the care of ambulatory surgery patients. The use of OSA-18, although it is used in clinical practice and was available when this study was conducted, represents another limitation to our study. A recent study from our group suggests that the OSA-18 is neither sufficiently sensitive to detect OSA nor sufficiently specific to determine the absence of OSA.17 There remains a need to develop screening tools to aid the anesthesiologist in preoperative detection of OSA. Additionally, because body mass index (BMI) was not recorded, we could not determine the overweight or obesity status of participants. BMI data should be included in future studies, since obesity has been associated with an increased risk for OSA,1 and this factor may influence providers' decisions to screen for OSA. Also, we did not collect data concerning physical examination by anesthesia providers, which may have influenced the likelihood that providers screen for OSA. Lastly, observers in our study did not record the incidence of caregiver-initiated conversation regarding OSA symptoms. This may be significant, as anesthesia providers are likely to ask questions when prompted by caregiver reports.
CONCLUSION
OSA was not routinely screened for by anesthesia providers prior to ambulatory pediatric surgery. When screening did occur, “snoring” was the most commonly recorded symptom. Paradoxically, patients with undiagnosed OSA who would benefit the most from screening were the least likely to be screened.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Bixler EO, Vgontzas AN, Lin HM, et al. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep. 2009;32:731–6. doi: 10.1093/sleep/32.6.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li AM, So HK, Au CT, et al. Epidemiology of obstructive sleep apnoea syndrome in Chinese children: a two-phase community study. Thorax. 2010;65:991–7. doi: 10.1136/thx.2010.134858. [DOI] [PubMed] [Google Scholar]
- 3.O'Brien LM, Holbrook CR, Mervis CV, et al. Sleep and neurobehavioral characteristics of 5- to 7-year-old children with parentally reported symptoms of attention-deficit/hyperactivity disorder. Pediatrics. 2003;111:554–63. doi: 10.1542/peds.111.3.554. [DOI] [PubMed] [Google Scholar]
- 4.Gross JB, Apfelbaum JL, Caplan RA, et al. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Anesthesiology. 2014;120:268–86. doi: 10.1097/ALN.0000000000000053. [DOI] [PubMed] [Google Scholar]
- 5.Franco RA, Jr, Rosenfeld RM, Rao M. First place—resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;123:9–16. doi: 10.1067/mhn.2000.105254. [DOI] [PubMed] [Google Scholar]
- 6.McColley SA, April MM, Carroll JL, Naclerio RM, Loughlin GM. Respiratory compromise after adenotonsillectomy in children with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 1992;118:940–3. doi: 10.1001/archotol.1992.01880090056017. [DOI] [PubMed] [Google Scholar]
- 7.Carithers JS, Gebhart DE, Williams JA. Postoperative risks of pediatric tonsilloadenoidectomy. Laryngoscope. 1987;97:422–9. doi: 10.1288/00005537-198704000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Richmond KH, Wetmore RF, Baranak CC. Postoperative complications following tonsillectomy and adenoidectomy: who is at risk? Int J Pediatr Otorhinolaryngol. 1987;13:117–24. doi: 10.1016/0165-5876(87)90088-7. [DOI] [PubMed] [Google Scholar]
- 9.Crysdale WS, Russel D. Complications of tonsillectomy and adenoidectomy in 9409 children observed overnight. Can Med Assoc J. 1986;135:1139–42. [PMC free article] [PubMed] [Google Scholar]
- 10.Rosen GM, Muckle RP, Mahowald MW, Goding GS, Ullevig C. Postoperative respiratory compromise in children with obstructive sleep apnea syndrome: can it be anticipated? Pediatrics. 1994;93:784–8. [PubMed] [Google Scholar]
- 11.Sanders JC, King MA, Mitchell RB, Kelly JP. Perioperative complications of adenotonsillectomy in children with obstructive sleep apnea syndrome. Anesth Analg. 2006;103:1115–21. doi: 10.1213/01.ane.0000244318.77377.67. [DOI] [PubMed] [Google Scholar]
- 12.Statham MM, Elluru RG, Buncher R, Kalra M. Adenotonsillectomy for obstructive sleep apnea syndrome in young children: prevalence of pulmonary complications. Arch Otolaryngol Head Neck Surg. 2006;132:476–80. doi: 10.1001/archotol.132.5.476. [DOI] [PubMed] [Google Scholar]
- 13.Nixon GM, Kermack AS, Davis GM, et al. Planning adenotonsillectomy in children with obstructive sleep apnea: the role of overnight oximetry. Pediatrics. 2004;113:e19–e25. doi: 10.1542/peds.113.1.e19. [DOI] [PubMed] [Google Scholar]
- 14.Brown KA, Morin I, Hickey C, et al. Urgent adenotonsillectomy: an analysis of risk factors associated with postoperative respiratory morbidity. Anesthesiology. 2003;99:586–95. doi: 10.1097/00000542-200309000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Wilson K, Lakheeram I, Morielli A, et al. Can assessment for obstructive sleep apnea help predict post-adenotonsillectomy respiratory complications? Anesthesiology. 2002;96:313–22. doi: 10.1097/00000542-200202000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Finkel KJ, Searleman AC, Tymkew H, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10:753–8. doi: 10.1016/j.sleep.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Ishman SL, Yang CJ, Cohen AP, et al. Is the OSA-18 predictive of obstructive sleep apnea: comparison to polysomnography. Laryngoscope. 2015;125:1491–5. doi: 10.1002/lary.25098. [DOI] [PubMed] [Google Scholar]


