Abstract
In recent years, retrograde approach for chronic total occlusions has rapidly evolved, enabling a higher rate of revascularization success. Compared to septal channels, epicardial collaterals tend to be more tortuous, more difficult to negotiate, and more prone to rupture. Coronary perforation is a rare but potentially life-threatening complication of coronary angioplasty, often leading to emergency cardiac surgery. We report a case of a retrograde chronic total occlusion revascularization through epicardial collaterals, complicated by both retrograde and antegrade coronary perforation with tamponade, and successfully managed by coil embolization.
Keywords: Chronic total occlusion, Percutaneous coronary intervention, Coronary perforation, Tamponade, Coil embolization
Abbreviations
- CTO
chronic total occlusion
- D1
first diagonal
- DES
drug-eluting stent
- IABP
intra-aortic balloon pump
- LAD
left anterior descending
- LCx
left circumflex
- PCI
percutaneous coronary intervention
- RCA
right coronary artery
Introduction
The prognostic benefits of chronic total occlusion (CTO) revascularization are well-recognized today [1,2]. However, despite the development of equipment and techniques [3], CTO percutaneous coronary intervention (PCI) remains challenging, with a lower success rate and a higher rate of periprocedural complications than non-CTO lesions [4]. The retrograde approach, particularly via septal channels, can improve recanalization success rates. Although epicardial collaterals in experienced hands may also represent an efficient option, their use is associated with a higher risk of complications [5].
Coronary perforation is a rare, but potentially life-threatening complication of PCI, with an incidence ranging from 0.1% to 0.5% [6]. As the conventional treatment of such a complication, consisting of reversal of anticoagulation and prolonged balloon inflation, is associated with high rates of death, myocardial infarction and need for emergency surgery, other strategies such as covered stent use and coil embolization have recently emerged, showing better outcomes [7].
We report a retrograde CTO revascularization case through epicardial collaterals complicated by perforation with tamponade and successfully managed by both retrograde and antegrade coil embolization.
Case report
An 84-year-old ex-smoker and dyslipidemic male, with a history of pacemaker implantation for third degree atrioventricular block, was admitted for cardiogenic shock one hour after chest pain onset. The electrocardiogram showed an ST depression in lateral leads with Q wave in antero-septal leads. The 2-D echocardiogram revealed an impaired left ejection fraction (35%) with a global hypokinesia. A coronary angiography was performed with intra-aortic balloon pump (IABP) support showing a sub-occlusion of proximal dominant left circumflex (LCx) (Fig. 1A), a proximal occlusion of left anterior descending (LAD) and a tight stenosis of the second segment of a minor right coronary artery (RCA) giving septal and epicardial collaterals to LAD (Fig. 1). According to the clinical setting, electrocardiogram modifications and the presence of retrograde filling of LAD by collaterals from RCA, LCx was considered to be the culprit vessel with a CTO of LAD. PCI of LCx was performed and a drug-eluting stent (DES) was implanted with a good angiographic result, while antegrade approach for LAD CTO was unsuccessfully attempted by a non-CTO operator. The in-hospital stay was uneventful and the patient was discharged after seven days. Two months later, a myocardial scintigraphy revealed viable myocardium in the anterior territory, and the patient was admitted for a second attempt to revascularize LAD CTO by a dedicated CTO operator.
Figure 1.
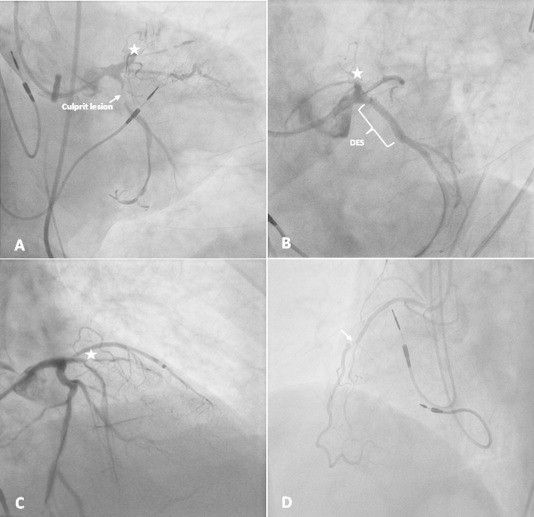
Coronary angiography. (A) Right caudal view showing a thrombotic sub-occlusion of proximal dominant LCx (arrow), and a proximal CTO of LAD. (B) Left caudal view after DES implantation in proximal LCx with good angiographic result. (C) Right cranial view after LCx PCI showing the LAD CTO with side branch at the proximal cap and blunt stump. (D) Left anterior oblique view showing a tight stenosis (arrow) of the second segment of a minor right RCA. Abbreviations: CTO = chronic total occlusion; DES = drug eluting stent; LAD = left anterior descending; LCx = left circumflex; RCA = right coronary artery; PCI = percutaneous coronary intervention. The star shows the proximal cap of LAD CTO.
A double 7-Fr femoral access was performed. A 7-Fr EBU 4 (Cordis Co., USA) was introduced in the left main, while a 7-Fr Amplatz-left 2 (Cordis Co., USA) was employed for RCA. The patient received 5000 UI of unfractionated heparin and an IABP support was used. Bilateral simultaneous injection showed a contralateral retrograde filling of LAD from tortuous screw-like epicardial CC2 (Werner’s Classification) [8] and septal collateral CC1, originating from RCA (Fig. 2). Because of the presence of a side branch at the proximal cap with a blunt stump, a retrograde approach was selected as the initial strategy.
Figure 2.
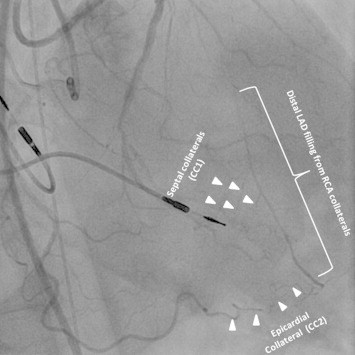
Bilateral injection showing a retrograde filling distal LAD from tortuous screw-like contralateral epicardial collaterals CC2 (Werner’s classification) [8], and septal collaterals CC1, originating from RCA. Abbreviations: LAD = left anterior descending; RCA = right coronary artery.
PCI of RCA with one DES implantation was first performed (Fig. 3A). A retrograde Sion guidewire (Asahi Intecc Co., Japan) and Corsair microcatheter (Asahi Intecc Co., Japan) were used (Fig. 3B), reaching the distal true lumen of LAD via the epicardial collateral. Then, Ultimate Bros (Asahi Intecc Co., Japan) guidewire was able to make a retrograde crossing of the lesion. The externalization was performed with RG3 guidewire (Asahi Intecc Co., Japan) (Fig. 3C). After pre-dilation, a DES was implanted in mid LAD through the retrograde guidewire, while the DES implantation in the median segment of first diagonal was performed through an antegrade Runthrough (Terumo Corp, Japan) guidewire. Thereafter, the retrograde LAD guidewire and the Corsair were retrieved, and an antegrade Runthrough guidewire was inserted in LAD to properly treat LAD-D1 bifurcation.
Figure 3.
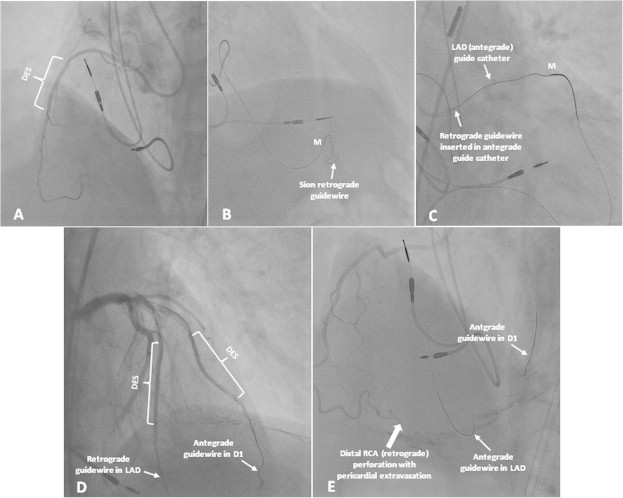
(A) Angiographic result after DES (2.25 × 14 mm) implantation in RCA. (B) Retrograde Sion guidewire and Corsair in tortuous screw-like epicardial collateral. (C) Successful externalization of retrograde RG3 guidewire (Asahi Intecc Co., Japan). (D) Left angiogram after DES implantation in mid LAD through the retrograde guidewire, and in mid-D1through an antegrade guidewire. (E) Right angiogram showing extravasation of contrast media at the distal end of the epicardial collateral, after the removal of retrograde guidewire and insertion of an antegrade guidewire in LAD. Abbreviations: D1 = first diagonal; DES = drug eluting stent; RCA = right coronary artery. The letter « M » showed the radio-opaque tip of the microcatheter.
Shortly afterwards, the patient showed sudden hypotension and dyspnea. Immediate right angiogram revealed an extravasation of contrast material at the distal end of the epicardial collateral (Fig. 3E), and an echocardiogram showed a massive pericardial effusion with tamponade. A pericardiocentesis was performed, yielding 700 ml of blood auto-transfused thereafter via femoral venous catheter. A first AXIUM™ Detachable Coil (ev3, USA) 2.0 × 2.0 mm was delivered retrograde through FineCross microcatheter (Terumo Corp, Japan), and implanted distally in the epicardial collateral (Fig. 4A). Since the extravasation of contrast medium to the pericardium persisted (Fig. 4B), two supplementary coils (3.0 × 4.0 mm and 3.0 × 6.0 mm, respectively) were implanted more distally. The absence of retrograde extravasation was confirmed in repeat angiograms (Fig. 4C). Protamine (2.5 mg) was then administered. As the patient showed hemodynamic stability, we decided to complete the LAD revascularization. A double kissing crush technique was employed to treat the LAD-D1 bifurcation. At the end of the procedure, the pericardial drainage was productive again, and left angiogram revealed an extravasation of contrast at the junction of distal LAD and epicardial collateral (Fig. 5A). Two coils (3.0 × 6.0 mm and 3.0 × 4.0 mm, respectively) were therefore implanted antegrade (Fig. 5B). Final right and left angiograms confirmed the absence of residual extravasation (Fig. 5C). The in-hospital stay was uneventful and the patient was discharged after eight days. At five-month follow-up, he was asymptomatic.
Figure 4.
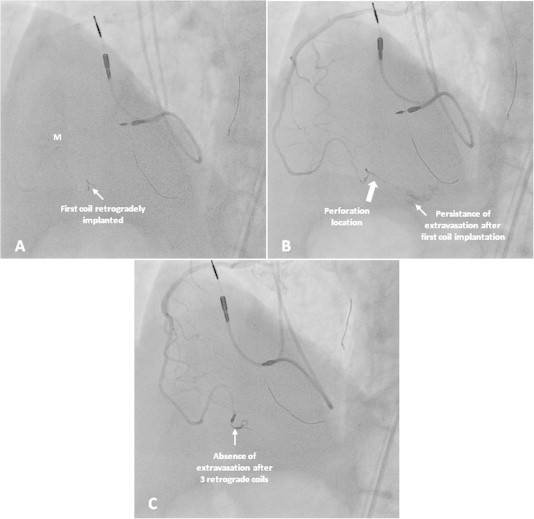
(A) First retrograde coil delivery AXIUM™ Detachable Coil (2.0 × 2.0 mm) through FineCross microcatheter in the epicardial collateral. (B) Selective injection showing persistence of contrast extravasation after first coil embolization. (C) Absence of contrast extravasation after 2 supplementary retrograde coils implantation (3.0 × 4.0 mm and 3.0 × 6.0 mm). The letter « M » showed the radio-opaque tip of the microcatheter.
Figure 5.
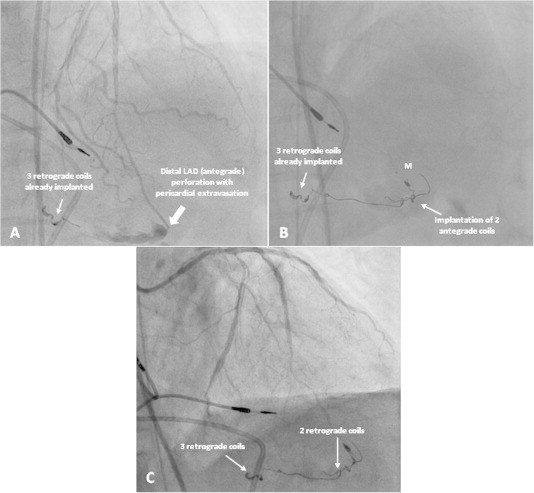
(A) Left angiogram showing contrast extravasation at the junction of distal LAD and epicardial collateral. (B) Antegrade delivery of 2 coils (3.0 × 6.0 mm and 3.0 × 4.0 mm) in epicardial channel. (C) Angiographic success of LAD CTO recanalization and absence of contrast extravasation. Abbreviations: CTO = chronic total occlusion; LAD = left anterior descending; TIMI = Thrombolysis in myocardial infarction. The letter « M » showed the radio-opaque tip of the microcatheter.
Discussion
Over the past few years, the retrograde approach for CTO lesions has rapidly evolved, enabling a higher rate of revascularization success. The tortuosity of the collateral channel remains one of the biggest contributors of difficulties and procedural risks. The use of a dedicated microcatheter such as Corsair, with a more maneuverable structure, allows the guidewire to advance with ease.
Compared to septal channels, epicardial collaterals (particularly from RCA) tend to be more tortuous with potentially inelastic stenosis. Epicardial collaterals are therefore more difficult to negotiate and are prone to rupture when dilated. Moreover, in contrast to intramyocardial channel ruptures resulting in no major complications, epicardial collateral channel ruptures often lead to tamponade [5].
Coronary perforation is a rare but serious complication occurring in 0.1–0.5% of patients undergoing PCI [6], with a relatively high mortality rate ranging from 7 to 17% [7]. It represents one of the most frequent complications experienced by patients undergoing CTO recanalization procedures, and its rate is higher in retrograde than in antegrade approach [4].
Guidewires are a major cause of coronary perforations, particularly those with hydrophilic-coating commonly used in CTO procedures. Balloon ruptures and the use of rotablators for calcified lesions are the other common etiologies of this complication [6,7].
In our patient, the retrograde perforation could have been caused by the advance of the hydrophilic guidewire and/or microcatheter maneuver in severely tortuous epicardial collateral. Initially sealed by the retrograde guidewire, the perforation became patent after its removal and replacement by an antegrade guidewire in LAD. On the other hand, the antegrade delayed perforation might have been due to the intensity of antegrade contrast injection in the ‘fragile,’ damaged junction between LAD and epicardial collateral originating from RCA. This fact underscores the importance of checking the collateral used for retrograde approach by bilateral injections.
The treatment of coronary artery perforation requires a multipronged approach: treating the perforation, maintaining hemodynamic stability with pericardiocentesis and/or with IABP, and reversing the effects of antithrombotic therapy. The treatment options of the perforation most commonly used include low-pressure balloon dilation, implantation of covered stents, coil and microsphere embolization, and emergency cardiac surgery [6,7].
The AXIUM™ Detachable Coils (ev3, USA) consist of a platinum coil attached to a composite implant delivery pusher with a radiopaque positioning marker and a hand-held instant detacher which, when activated, detaches the coil from the delivery pusher tip. The design of an embolization coil involves a wire (usually of steel or platinum) that is wound tightly into a straight primary coil, and then formed into a secondary structure of various designs such as helices in our case. Regarding the manufacturer, the coil delivery to the site of perforation may require a microcatheter, as observed in our case. Coil implantation induces thrombosis, leading ultimately to fibrosis. To reverse heparin effects, protamine should be administered after coil distal delivery to avoid proximal thrombosis, or, better yet, after complete sealing of the perforation. Once the coil is delivered, a small selective distal injection from the microcatheter tip can be performed to detect residual extravasation, requiring further coil embolization.
First invented for the endovascular embolization of intra-cranial aneurysms, fistulas, pseudoaneurysms and other neurovascular abnormalities, coil embolization has been successfully employed in cases of distal coronary perforation [9,10].
To the best of our knowledge, this is the first reported case of a CTO procedure complicated by coronary perforation with tamponade, and managed by both retrograde and antegrade coil embolization. Coils might represent useful tools in the armamentarium of interventional cardiologists, particularly those performing CTO procedures, and may help in forestalling emergent cardiac surgery for coronary perforations.
Disclosure: Author has nothing to disclose with regard to commercial support.
References
- 1.Galassi A.R., Tomasello S.D., Crea F., Costanzo L., Campisano M.B., Marzà F. Transient impairment of vasomotion function after successful chronic total occlusion recanalization. J Am Coll Cardiol. 2012;59(8):711–718. doi: 10.1016/j.jacc.2011.10.894. [DOI] [PubMed] [Google Scholar]
- 2.Galassi A.R., Boukhris M., Tomasello S.D., Marzà F., Azzarelli S., Giubilato S. Long-term clinical and angiographic outcomes of the mini-STAR technique as a bailout strategy for percutaneous coronary intervention of chronic total occlusion. Can J Cardiol. 2014;30(11):1400–1406. doi: 10.1016/j.cjca.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Tomasello S.D., Giudice P., Attisano T., Boukhris M., Galassi A.R. The innovation of composite core dual coil coronary guide-wire technology: a didactic coronary chronic total occlusion revascularization case report. J Saudi Heart Assoc. 2014;26(4):222–225. doi: 10.1016/j.jsha.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galassi A.R., Tomasello S.D., Reifart N., Werner G.S., Sianos G., Bonnier H. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 2011;7(4):472–479. doi: 10.4244/EIJV7I4A77. [DOI] [PubMed] [Google Scholar]
- 5.Tomasello S.D., Marzà F., Giubilato S., Galassi A.R. Retrograde approach for revascularization of coronary chronic total occlusion. Minerva Cardioangiol. 2012;60(5):461–472. [PubMed] [Google Scholar]
- 6.Gunning M.G., Williams I.L., Jewitt D.E., Shah A.M., Wainwright R.J., Thomas M.R. Coronary artery perforation during percutaneous intervention: incidence and outcome. Heart. 2002;88(5):495–498. doi: 10.1136/heart.88.5.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fasseas P., Orford J.L., Panetta C.J., Bell M.R., Denktas A.E., Lennon R.J. Incidence, correlates, management, and clinical outcome of coronary perforation: analysis of 16,298 procedures. Am Heart J. 2004;147(1):140–145. doi: 10.1016/s0002-8703(03)00505-2. [DOI] [PubMed] [Google Scholar]
- 8.Werner G.S., Ferrari M., Heinke S., Kuethe F., Surber R., Richartz B.M. Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation. 2003;107(15):1972–1977. doi: 10.1161/01.CIR.0000061953.72662.3A. [DOI] [PubMed] [Google Scholar]
- 9.Assali A.R., Moustapha A., Sdringola S., Rihner M., Smalling R.W. Successful treatment of coronary artery perforation in an abciximab-treated patient by microcoil embolization. Catheter Cardiovasc Interv. 2000;51(4):487–489. doi: 10.1002/1522-726x(200012)51:4<487::aid-ccd25>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 10.Martí V., Castaño C., Guiteras P., Vallés E., Domínguez de Rozas J.M., Augé J.M. Cardiac perforation complicated by cardiac tamponade and sealed with metallic coils. [Article in Spanish] Rev Esp Cardiol. 2004;57(10):990–992. [PubMed] [Google Scholar]


