Abstract
Introduction
Coronary artery ectasia is an uncommon disease that has been increasingly noticed as the increase in utilization of coronary angiograms. The aim of this study is to characterize coronary artery ectasia in the population of Saudi Arabia.
Methods
This is a retrospective study involved all patient with invasive coronary angiogram that was done at a tertiary hospital in Saudi Arabia from January 2011 to December 2013.
Results
A total of 1115 coronary angiograms were reviewed. Coronary artery ectasia was found in 67 patients (6% of all coronary angiograms). The right coronary artery was involved in 73% of cases. And 43% of the cases had severe ectasia.
Conclusion
The prevalence of coronary artery ectasia in Saudi Arabia among patient who went for coronary angiography is higher than what has been published in previous studies and a significant number of patients have severe disease.
Keywords: Coronary, Ectasia, Atherosclerosis
Introduction
Coronary artery ectasia is an uncommon entity that has been seen with increasing frequency as the utilization of coronary angiograms has expanded, facilitating the diagnosis and management of coronary artery disease. It is defined as dilatation of a coronary artery segment to a diameter at least 1.5 times that of the adjacent normal coronary artery [1–3]. Its first angiographic description was by Munkner et al. in 1958 [4], but the original description of the disease by Morgagni goes back to 1761 [5]. It has an estimated incidence of 1–5% of all invasive coronary angiograms [3,6,7]. Coronary artery ectasia has been attributed to atherosclerosis in about 50% of cases, related to inflammatory and connective tissue disease in 10–20% of cases, and thought to be congenital in origin in 20–30% of ectasia cases [2,8,9]. The aim of this study is to characterize coronary artery ectasia in the population of Saudi Arabia.
Methods
This is a retrospective study including all patients who underwent invasive coronary angiograms in a tertiary hospital in Saudi Arabia from January 2011 to December 2013. The data was collected from medical records and hospital databases. An interventional cardiologist reviewed all angiograms, and ectasia was recognized when a dilated segment of a coronary artery had a diameter at least 1.5 times that of adjacent coronary segment. Coronary ectasia was classified based on the extent of the disease, according to the proposal by Markis et al [10]. Diffuse ectasia involving two or three vessels was classified as type I; diffuse disease in one vessel and localized disease in another vessel as type II; diffuse ectasia in one vessel only as type III; and localized ectasia as type IV. Obstructive coronary artery disease was defined as 50% or more diameter stenosis in the left main coronary artery or 70% or more diameter stenosis in a major coronary artery [11]. Slow flow was defined as sluggish clearing of the coronary artery, that is, when the vessel fills completely but either fills or empties slower than uninvolved vessels in the absence of coronary obstruction [12].
The hospital institutional review board approved the study protocol. The data was analyzed and the baseline characteristics were computed using mean and standard deviation for continuous variables and percentage for dichotomous variables.
Results
A total of 1115 coronary angiograms were reviewed. Coronary artery ectasia was found in 67 patients (6% of all coronary angiograms). The baseline characteristics and the biochemical profiles of the patients are shown in Table 1. The mean age of our patients was 56 ± 12 years and most patients were males, constituting 82% of our sample. About 5% of our patients had history of strokes; 57% had history of previous myocardial infarction; 48% had previous history of angioplasty; 15% had history of coronary artery bypass surgery; and no patient had history of connective tissue disease. Fig. 1 shows that coronary artery ectasia was seen more frequently in the right coronary artery, which has ectasia in 73% of the cases, while ectasia of the left main coronary artery was seen in only 8% of the cases. Fig. 2 shows that severe coronary ectasia was seen in a significant portion of our sample, 21% and 22% for coronary ectasia type I and type II respectively, while localized ectasia was seen in 42% of cases. Fig. 3 shows that obstructive coronary artery disease was seen in 66% of cases and slow flow in 61%. Regional wall motion abnormalities on echocardiography were seen in 54% of the cases. The mean ejection fraction (EF) in class I was 55.7 ± 10.5%; in class II, it was 56.4 ± 16.2%; in class III, it was 45.3 ± 18.9%; and in class IV, it was 53.6 ± 15.8%, and there was no statistically significant difference between the classes (p value = 0.315). Table 2 summarizes the medication patients were taking at the time of the coronary angiogram. Table 3 shows the differences in patient characteristics between different classes of ectasia.
Table 1.
Baseline characteristics and biochemical profile of patients.
| Patient characteristics | N = 67 |
|---|---|
| Age (years) | 56 ± 12 |
| Sex (male %) | 82% |
| Nationality (Saudi %) | 54% |
| Diabetes mellitus | 59% |
| Hypertension | 64% |
| Dyslipidemia | 59% |
| Smoking | 31% |
| Chronic renal failure | 11% |
| Hemoglobin (g/dL) | 13.2 ± 2.2 |
| Glycosylated hemoglobin (%) | 7.5 ± 2.1 |
| Total cholesterol (mg/dL) | 168 ± 46.8 |
| LDL cholesterol (mg/dL) | 100.5 ± 41.7 |
| HDL cholesterol (mg/dL) | 35.4 ± 12.2 |
| Triglyceride (mg/dL) | 152.9 ± 95.3 |
| Serum creatinine (mg/dL) | 1.3 ± 1.5 |
| Ejection fraction (%) | 53.4 ± 15.5 |
Figure 1.

Distribution of ectasia in the coronary arteries. LM: left main, LAD: left anterior descending artery, LCx: left circumflex artery, RCA: right coronary artery.
Figure 2.
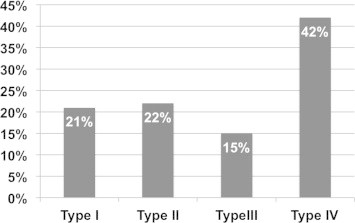
Distribution of different types of coronary ectasia.
Figure 3.

Distribution of obstructive CAD and slow flow in the sample. CAD: coronary artery disease.
Table 2.
Summary of patient medications.
| Medication | N = 67 (%) |
|---|---|
| Aspirin | 97 |
| Warfarin | 8 |
| Statins | 95 |
| Angiotensin converting enzyme inhibitors | 59 |
| Angiotensin receptor blockers | 34 |
| Nitroglycerin | 49 |
| Beta-blockers | 91 |
| Calcium channel blockers | 22 |
Table 3.
Baseline characteristics of patients in different classes of coronary ectasia.
| Patient characteristics | Class 1 | Class 2 | Class 3 | Class 4 | P value |
|---|---|---|---|---|---|
| Age (years) | 55 ± 8 | 59 ± 10 | 58 ± 11 | 55 ± 14 | 0.682 |
| Sex (male %) | 79% | 80% | 90% | 82% | 0.899 |
| Nationality (Saudi %) | 50% | 53% | 50% | 57% | 0.966 |
| Diabetes mellitus | 29% | 71% | 70 | 63% | 0.075 |
| Hypertension | 64% | 73% | 60% | 59% | 0.827 |
| Dyslipidemia | 50% | 47% | 80% | 63% | 0.332 |
| Coronary artery disease | 93% | 100% | 100% | 93% | 0.590 |
| Smoking | 30% | 36% | 33% | 29% | 0.974 |
| Chronic renal failure | 7% | 13% | 20% | 7% | 0.678 |
Discussion
Coronary artery ectasia is an uncommon disease with controversies regarding its management. To our knowledge, this is the first study to characterize coronary artery ectasia in a sample from Saudi Arabia. In our sample, the incidence of coronary artery ectasia among patients who underwent invasive coronary angiography was slightly higher (6%) than what has been published earlier. This can be attributed to the increased prevalence of atherosclerotic coronary artery disease in the region, or the possibility of an increased genetic susceptibility to the development of coronary artery ectasia. This was suggested by the fact that 43% of our sample have a severe form of ectasia (types I and II).
A previous meta-analysis showed that the prevalence of diabetes mellitus in patients with coronary artery ectasia was 8–33% and suggested that diabetes might be a defense against the development of coronary artery ectasia [13]. In contrast, the prevalence of diabetes mellitus in our sample was much higher at 59%. This can be attributed to the fact that the prevalence of diabetes mellitus in the Saudi population is 23.7%, which is considered one of the highest in the world [14]. In addition, a higher prevalence of diabetes mellitus exists among Saudi patients with coronary artery disease: one study has estimated a prevalence of 58.1% in patients with acute coronary syndrome in Saudi Arabia [15]. These conflicting results suggest the need for further studies to evaluate the relationship between diabetes mellitus and coronary artery ectasia. Sixty-one percent of our patients demonstrated slow-flow phenomena, which usually indicates inadequate perfusion of the myocardium [16,17]. In our study, 54% of the patients had wall motion abnormalities on echocardiography, indicative of myocardial ischemia or infarction. One study has shown that coronary flow reserve was significantly reduced in patients with coronary artery ectasia, reflecting a microcirculatory dysfunction leading to myocardial ischemia [18]. However, the clinical importance of slow-flow phenomena in the context of coronary artery ectasia is unknown and needs further evaluation. Several studies have shown that the right coronary artery is the most frequently involved artery with coronary ectasia [7–9,19]. Seventy-three percent of our patients had the right coronary artery involved. The reasons for the higher right coronary artery predisposition to ectasia are not well understood. Table 2 shows that 8% of our patients were taking warfarin, prescribed for stroke prevention in atrial fibrillation. The role of anticoagulation in coronary artery ectasia needs further evaluation.
Our study has some limitations including its small sample size and being a single-center study. As a retrospective study, it lacks information about treatment and outcomes of the patients. In conclusion, coronary artery ectasia has a higher prevalence in Saudi Arabia among patients undergoing invasive coronary angiography, and patients tend to have diffuse disease. Further studies are needed to investigate treatment measures and outcomes of coronary artery ectasia.
Disclosure: Authors have nothing to disclose with regard to commercial support.
References
- 1.Falsetti H.L., Carrol R.J. Coronary artery aneurysm. A review of the literature with a report of 11 new cases. Chest. 1976;69(5):630–636. doi: 10.1378/chest.69.5.630. [DOI] [PubMed] [Google Scholar]
- 2.Mavrogeni S. Coronary artery ectasia: from diagnosis to treatment. Hellenic J Cardiol. 2010;51(2):158–163. [PubMed] [Google Scholar]
- 3.Swanton R.H., Thomas M.L., Coltart D.J., Jenkins B.S., Webb-Peploe M.M., Williams B.T. Coronary artery ectasia – A variant of occlusive coronary arteriosclerosis. Br Heart J. 1978;40(4):393–400. doi: 10.1136/hrt.40.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munkner T., Petersen O., Vesterdal J. Congenital aneurysm of the coronary artery with an arteriovenous fistula. Acta Radiol. 1958;50(4):333–340. doi: 10.3109/00016925809172312. [DOI] [PubMed] [Google Scholar]
- 5.Lazzarin P., Pasero G., Marson P., Cecchetto A., Zanchin G. Takayasu’s arteritis. A concise review and some observations on a putative case reported by Giovanni Battista Morgagni (1761) Reumatismo. 2005;57(4):305–313. doi: 10.4081/reumatismo.2005.305. [DOI] [PubMed] [Google Scholar]
- 6.Hartnell G.G., Parnell B.M., Pridie R.B. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J. 1985;54(4):392–395. doi: 10.1136/hrt.54.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swaye P.S., Fisher L.D., Litwin P., Vignola P.A., Judkins M.P., Kemp H.G. Aneurysmal coronary artery disease. Circulation. 1983;67(1):134–138. doi: 10.1161/01.cir.67.1.134. [DOI] [PubMed] [Google Scholar]
- 8.Syed M., Lesch M. Coronary artery aneurysm: a review. Prog Cardiovasc Dis. 1997;40(1):77–84. doi: 10.1016/s0033-0620(97)80024-2. [DOI] [PubMed] [Google Scholar]
- 9.Daoud A.S., Pankin D., Tulgan H., Florentin R.A. Aneurysms of the coronary artery. Report of ten cases and review of literature. Am J Cardiol. 1963;11:228–237. doi: 10.1016/0002-9149(63)90064-x. [DOI] [PubMed] [Google Scholar]
- 10.Markis J.E., Joffe C.D., Cohn P.F., Feen D.J., Herman M.V., Gorlin R. Clinical significance of coronary arterial ectasia. Am J Cardiol. 1976;37(2):217–222. doi: 10.1016/0002-9149(76)90315-5. [DOI] [PubMed] [Google Scholar]
- 11.Fihn S.D., Gardin J.M., Abrams J., Berra K., Blankenship J.C., Dallas A.P. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126(25):3097–3137. doi: 10.1161/CIR.0b013e3182776f83. [DOI] [PubMed] [Google Scholar]
- 12.Klein L.W., Kern M.J., Berger P., Sanborn T., Block P., Babb J. Society of cardiac angiography and interventions: suggested management of the no-reflow phenomenon in the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 2003;60(2):194–201. doi: 10.1002/ccd.10620. [DOI] [PubMed] [Google Scholar]
- 13.Huang Q.J., Liu J., Chen M.H., Li J.J. Relation of diabetes to coronary artery ectasia: a meta-analysis study. Anadolu Kardiyol Derg. 2014;14(4):332–337. doi: 10.5152/akd.2014.5327. [DOI] [PubMed] [Google Scholar]
- 14.Al-Nozha M.M., Al-Maatouq M.A., Al-Mazrou Y.Y., Al-Harthi S.S., Arafah M.R., Khalil M.Z. Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004;25(11):1603–1610. [PubMed] [Google Scholar]
- 15.Alnemer K.A., Alfaleh H.F., Alhabib K.F., Ullah A., Hersi A., Alsaif S. Impact of diabetes on hospital adverse cardiovascular outcomes in acute coronary syndrome patients: data from the Saudi project of acute coronary events. J Saudi Heart Assoc. 2012;24(4):225–231. doi: 10.1016/j.jsha.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kloner R.A., Ganote C.E., Jennings R.B. The “no-reflow” phenomenon after temporary coronary occlusion in the dog. J Clin Invest. 1974;54(6):1496–1508. doi: 10.1172/JCI107898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schofer J., Montz R., Mathey D.G. Scintigraphic evidence of the “no reflow” phenomenon in human beings after coronary thrombolysis. J Am Coll Cardiol. 1985;5(3):593–598. doi: 10.1016/s0735-1097(85)80381-8. [DOI] [PubMed] [Google Scholar]
- 18.Akyürek O., Berkalp B., Sayin T., Kumbasar D., Kervancioğlu C., Oral D. Altered coronary flow properties in diffuse coronary artery ectasia. Am Heart J. 2003;145(1):66–72. doi: 10.1067/mhj.2003.48. [DOI] [PubMed] [Google Scholar]
- 19.Harikrishnan S., Sunder K.R., Tharakan J., Titus T., Bhat A., Sivasankaran S. Coronary artery ectasia: angiographic, clinical profile and follow-up. Indian Heart J. 2000;52(5):547–553. [PubMed] [Google Scholar]


