Abstract
Aims: To describe inconsistencies in reporting past-year drinking status and heavy drinking occasions (HDOs) on single questions from two different instruments, and to identify associated characteristics and impacts.
Methods: We compared computer-presented Alcohol Use Disorder Identification Test-Consumption (AUDIT-C) with categorical response options, and mental health interview (MHI) with open-ended consumption questions, completed on the same day. Participants were 464 men and 459 women aged 38 (91.7% of surviving birth cohort members). Differences in dichotomous single-item measures of abstention and HDO frequency, associations of inconsistent reporting with sex, socioeconomic status (SES) and survey order, and impacts of instrument choice on associations of alcohol with sex and SES were examined.
Results: The AUDIT-C drinking frequency question estimated higher past-year abstention prevalence (AUDIT = 7.6%, MHI = 5.4%), with one-third of AUDIT-C abstainers being MHI drinkers. Only AUDIT-C produced significant sex differences in abstainer prevalence. Inconsistencies in HDO classifications were bidirectional, but with fewer HDOs reported on the MHI than AUDIT-C question. Lower SES was associated with inconsistency in abstention and weekly+ HDOs. Abstention and higher HDO frequency were associated with lower SES overall, but sex-specific associations differed by instrument.
Conclusions: In this context, data collection method affected findings, with inconsistencies in abstention reports having most impact. Future studies should: (a) confirm self-reported abstention; (b) consider piloting data collection methods in target populations; (c) expect impacts of sex and SES on measurements and analyses.
INTRODUCTION
In order to better understand the relationships between alcohol consumption and a wide variety of alcohol-attributable outcomes, epidemiological studies have used various different measures and methods to collect information about alcohol exposure. Self-reports of past-year drinking status (i.e. abstainers versus drinkers) and frequency of heavy drinking occasions (HDOs) have commonly been used to estimate associations of alcohol consumption with health, social and economic outcomes (Grittner et al., 2013). In the absence of gold standard methods for identifying abstainers and estimating HDO frequency, researchers continue to use a range of questions and approaches to measure these variables (Gmel and Rehm, 2004; Ekholm et al., 2008). As alcohol researchers often use screening instruments and diagnostic interviews to detect hazardous drinking and/or alcohol-related problems, consumption data from single questions within such instruments have sometimes been used as ‘stand-alone’ measures in analyses (Kypri et al., 2009).
The commonly used AUDIT (Alcohol Use Disorders Identification Test) screening instrument begins with three questions about alcohol consumption level and pattern (Saunders et al., 1993). The abbreviated AUDIT-C instrument is comprised of these three AUDIT questions, and has been shown to predict hazardous drinking as well as the full AUDIT (Bush et al., 1998; Reinert and Allen, 2007). Several epidemiological studies have used individual AUDIT-C questions to determine drinking status and to measure HDO frequency (Zarkin et al., 2004; Rodgers et al., 2005; Caamano-Isorna et al., 2008). Alcohol consumption gate questions that are primarily asked to determine whether study participants meet criteria for further assessment (i.e. with a standardized diagnostic interview for alcohol use disorders) can also provide potentially useful data about drinking status and HDO frequency.
The third AUDIT-C question about HDO frequency is a well-validated measure of alcohol misuse (Bradley et al., 2007; Reinert and Allen, 2007), and a gender-specific version of this AUDIT-C question (i.e. lower cut-offs for women than men) has been recommended by NIAAA (2007) and validation studies (Smith et al., 2009). AUDIT-C validation studies for risky drinking have used alcohol consumption interview questions as reference standards (Bush et al., 1998; Bradley et al., 2007). The validity of using the first AUDIT-C question (i.e. past-year drinking frequency) as a ‘stand-alone’ measure of drinking status has rarely been considered in the literature to date (Broyles et al., 2011), despite ongoing research and discussion about abstainer misclassification and its impacts (Klatsky 2008; Rehm et al., 2008; Zeisser et al., 2014).
Inaccurate measures of alcohol consumption can bias estimates of morbidity, mortality, and the social and economic outcomes attributable to alcohol. The performance of even well-established alcohol consumption instruments such as the AUDIT-C and standardized interviews requires ongoing evaluation, particularly when individual components are being used for different analytical purposes than originally intended. Considering the validity and potential biases of alcohol consumption measures for specific sociodemographic subgroups has been identified as a research agenda of some importance (Midanik and Greenfield, 2004; Greenfield and Kerr, 2008). Since alcohol consumption patterns and their impacts have been shown to differ by gender and socioeconomic status (SES) (Cheng and Furnham, 2013; Fone et al., 2013; Probst et al., 2014), differences in reporting by gender or socioeconomic status could be an important source of bias. A study by Rehm et al. (2008) found associations between inconsistent reports of lifetime abstention and sociodemographic factors including gender and ethnicity.
As part of a larger birth cohort study of associations between alcohol consumption and sexual health, this analysis estimates the magnitude and potential impacts of inconsistencies in self-reported drinking status and heavy drinking occasion (HDO) frequency in participants at 38 years of age. We compare single items from two instruments used on the same day: a self-administered computer-presented AUDIT-C survey, and open-ended alcohol consumption screening questions asked as part of a mental health interview (MHI).
For AUDIT-based and MHI-based measures of past-year abstention and HDO frequency, this study measured: (a) the prevalence of inconsistent reporting and degree of discordance; (b) associations of inconsistent reporting with sex, socioeconomic status, and survey order; and (c) impacts of instrument choice on prevalence estimates and on associations of alcohol consumption with sex and socioeconomic status.
METHODS
Participants
Participants were members of the Dunedin Multidisciplinary Health and Development Study, a longitudinal study of a complete birth cohort from Dunedin, New Zealand, born between 1 April 1972 and 31 March 1973. The sample of 1037 children (91% of 1139 eligible births) was first assessed at 3 years of age and most recently at 38 years, when 95% of the 1007 living study members were assessed in 2010–2012. Sociodemographic characteristics of the sample were generally representative of the New Zealand population for this age group, with slightly higher educational attainment and fewer people of Māori ethnicity at age 21 (Dickson et al., 1996). Silva and McCann (1996) have described the early history of the birth cohort. Ethical approval was obtained from the Otago Ethics Committee.
Measures
Alcohol consumption
At the 38-year-old assessment, participants were asked about past-year alcohol consumption during two distinct sections of the assessment day: (a) Alcohol Use Disorders Identification Test-consumption (AUDIT-C) questions in the computer-presented sexual and reproductive health questionnaire, and (b) mental health interview (MHI) questions about alcohol consumption, nested within a comprehensive psychiatric diagnostic interview. AUDIT-C questions had categorical response options, whereas the MHI questions were open-ended. The mental health interviewers had tertiary degrees and clinical experience in a mental health-related field, were blinded to prior assessment results, and administered the face-to-face structured interviews in private.
AUDIT-C and MHI alcohol consumption questions are detailed in Box 1. We defined AUDIT-C abstention based on a response of ‘Never’ to AUD1, and MHI abstention based on a response of ‘None’ to MHI1. Two dichotomous measures of HDO frequency were constructed from the AUD3 and MHI3 responses: (a) less than monthly HDOs versus monthly or more HDOs (<monthly/monthly+ HDOs), and (b) less than weekly HDOs versus weekly or more HDOs (<weekly/weekly+ HDOs). For HDOs reported on the MHI, equal spacing over time was assumed, so that 12 and 52 past-year HDOs were equivalent to monthly and weekly HDOs, respectively. The clustering of responses around 6, 12 and 52 indicated that this was a fair assumption. While the operational definition of HDOs differed slightly for the AUDIT-C and MHI questions (AUD3: 6+ drinks; MHI3: 5+ drinks), we felt that comparing these two questions was acceptable given the large degree of measurement uncertainty already present in these self-reported HDO estimates. Since most people do not keep accurate counts of their drinks and the conversion of actual drinks into standard drinks is fairly complex, we felt that the potential impacts of a single-drink difference in the HDO definition were relatively minor.
Box 1. AUDIT-C and mental health interview (MHI) alcohol consumption questions.
Past-year drinking frequency
AUD1: ‘Thinking about the past 12 months, how often do you have a drink containing alcohol?’ [Never, Monthly or less, 2–4 times a month, 2–3 times a week, 4 or more times a week]
MHI1*: ‘In the past year, how many weeks out of 52, have you had any wine, beer or other drink containing alcohol?’
Typical drinking quantity
AUD2: ‘How many standard drinks (see picture in folder) do you have on a typical day when you are drinking?’ [1, 2, 3–4, 5–6, 7–9, 10+]
MHI2*: (a) ‘In a typical week when you had something to drink, how many drinks would you have, in total, from Monday to Thursday, on work days?’; (b) ‘And how many drinks, in total, would you usually have from Friday through to Sunday, on weekends?’
Frequency of heavy drinking occasions (HDOs)
AUD3: ‘How often do you have 6 or more standard drinks on one occasion?’ [Never, Less than monthly, Monthly, Weekly, Daily or almost daily]
MHI3: ‘In the past year, how many times did you have five or more drinks in one sitting or occasion (binged)?’
Definitions and pictures of (10 g) drinks were provided for AUDIT-C questions, while the MHI questions were prefaced with the interviewer stating, ‘When I use the term ‘drink’ I mean a glass of wine, a can or bottle of beer, a ‘shot’ or ‘nip’ of hard liquor either alone or in a mixed drink’.
Participants responding ‘Never’ to AUD1 were not asked AUD2 and AUD3 questions due to the skip pattern in the computer-presented questionnaire.
*MHI1, MHI2a and MHI2b are Diagnostic Interview Schedule (DIS-IV) gate questions that determined whether to assess for alcohol abuse/dependence with DSM-IV-TR criteria (Robins et al., 1981, 2000; American Psychiatric Association, 2000).
Consistency of reporting abstention and HDOs
Consistency of AUDIT-C and MHI responses was categorized using the terminology shown in Box 2. A dichotomous measure of inconsistent abstention grouped those with inconsistent reporting on the two instruments (inconsistent AUDIT-C abstainers and inconsistent MHI abstainers) versus those with consistent reporting on the two instruments (consistent abstainers and consistent drinkers). Dichotomous measures of inconsistent HDO frequency were also defined. ‘Inconsistent monthly+ HDOs' grouped inconsistent reporting on the two instruments (inconsistent AUDIT-C monthly+ HDOs and inconsistent MHI monthly+ HDOs) versus consistent reporting on the two instruments, and ‘inconsistent weekly+ HDOs' versus consistent reports of weekly HDOs were defined similarly.
Box 2. Terminology for consistency of reporting.
Abstention: AUD1 and MHI1
Consistent abstainers and consistent drinkers: Participants with congruent AUDIT-C and mental health interview (MHI) reports for past-year abstention or drinking, respectively.
Inconsistent AUDIT-C abstainers: AUDIT-C abstainers who reported drinking once or more in the past year during the MHI.
Inconsistent MHI abstainers: MHI abstainers who reported past-year drinking on the AUDIT-C.
Heavy drinking occasions (HDOs): AUD3 and MHI3
Consistent <monthly HDOs and consistent monthly+ HDOs: Participants with congruent AUDIT-C and MHI reports of less than monthly HDOs or monthly+ HDOs, respectively.
Inconsistent AUDIT-C monthly+ HDOs: Monthly+ HDOs on AUDIT-C but less than monthly on MHI.
Inconsistent MHI monthly+ HDOs: Monthly+ HDOs on MHI but less than monthly on AUDIT-C.
Equivalent terminology was used for consistency of <weekly/weekly+ HDOs.
Socioeconomic status
The New Zealand Socio-Economic Index was used to classify SES at age 38 into six categories (‘1’ = unskilled labourer to ‘6’ = professional) (Milne et al., 2013). SES score was analysed both as a continuous (6-point linear predictor) and categorical (High SES = 5/6, Mid SES = 3/4, Low SES = 1/2) variable, two methods commonly used in alcohol research (van Oers et al., 1999; Jefferis et al., 2007; Viner and Taylor, 2007; Melotti et al., 2013; Paljärvi et al., 2013). Monotonic relationships between SES categories and proportions of abstainers/heavy drinkers were confirmed with cross-tabulations.
Survey order
Approximately one-third of participants had the AUDIT-C before the MHI. Although timing varied, the two questionnaires were generally administered in the afternoon one to two hours apart, with other assessments and a short break between them.
Statistical analyses
Analyses were restricted to 923 participants who answered all AUDIT-C and MHI alcohol consumption questions at age 38 (91.7% of the 1007 surviving cohort members). Stata Version 11.2 was used for all analyses (StataCorp, 2009). Sex-specific distributions were presented for AUDIT-C and MHI measures of typical drinking frequency and HDO frequency (Table 1).
Table 1.
Self-reported AUDIT-C and MHI alcohol consumption of participants at age 38
| AUDIT-C questionsa |
Mental health interview (MHI) questionsb |
||
|---|---|---|---|
| AUD1: typical frequency of drinking in past year | MHI1: number of drinking weeks in past year | ||
| Men (n = 464) | % | Men (n = 464) | % |
| Never | 5.8 | None | 4.5 |
| Monthly or less | 13.8 | 1–12 weeks | 15.3 |
| 13–23 weeks | 6.3 | ||
| 2–4 times a month | 21.1 | 24–48 weeks | 22.8 |
| 49–51 weeks | 4.7 | ||
| 2–3 times a week | 30.8 | 52 weeks | 46.3 |
| 4 or more times a week | 28.4 | Range: 0–52; Median (IQR): 50 (20–52) | |
| Women (n = 459) | % | Women (n = 459) | % |
| Never | 9.4 | None | 6.3 |
| Monthly or less | 22.0 | 1–12 weeks | 25.3 |
| 13–23 weeks | 6.8 | ||
| 2–4 times a month | 23.1 | 24–48 weeks | 20.7 |
| 49–51 weeks | 4.8 | ||
| 2–3 times a week | 22.4 | 52 weeks per year | 36.2 |
| 4 or more times a week | 23.1 | Range: 0–52; Median (IQR): 39 (10–52) | |
| AUD3: frequency of heavy drinking occasions (6+ drinks) in past year | MHI3: number of heavy drinking occasions (5+ drinks) in past year | ||
| Men (n = 437)c | % | Men (n = 464) | % |
| Never | 14.9 | 0 times per year | 20.0 |
| Less than monthly | 32.3 | 1–11 times per year | 31.9 |
| Monthly | 22.7 | 12 times per year | 5.8 |
| 13–51 times per year | 17.2 | ||
| Weekly | 26.3 | 52 times per year | 10.3 |
| 53–259 times per year | 11.4 | ||
| Daily or almost daily | 3.9 | 260–364 times per year | 2.2 |
| 365 times per year | 1.1 | ||
| Range: 0–365; Median (IQR): 10 (2–51) | |||
| Women (n = 416)c | % | Women (n = 459) | % |
| Never | 30.5 | 0 times per year | 34.9 |
| Less than monthly | 39.4 | 1–11 times per year | 38.1 |
| Monthly | 16.1 | 12 times per year | 5.7 |
| 13–51 times per year | 11.1 | ||
| Weekly | 11.3 | 52 times per year | 3.9 |
| 53–259 times per year | 4.8 | ||
| Daily or almost daily | 2.6 | 260–364 times per year | 0.9 |
| 365 times per year | 0.7 | ||
| Range: 0–365; Median (IQR): 3 (0–12) | |||
aAUDIT-C categories represent the options presented to participants on a computer-based questionnaire.
bContinuous responses to open-ended mental health interview questions have been categorized in this table.
cDue to the computer questionnaire skip pattern, AUDIT-C abstainers (i.e. 27 male and 43 female participants who answered ‘Never’ to AUD1) did not answer AUD3.
Consistency analyses for abstention included all 464 men and 459 women (89.8 and 93.7% of male and female participants alive at age 38, respectively). Consistency analyses for HDO frequency included 446 men and 430 women, because of the exclusion of 18 men and 29 women who were consistent abstainers. Due to the survey skip pattern, AUDIT-C abstainers were not asked further AUDIT-C questions. However, since all MHI abstainers responded ‘none’ to the MHI3 question about HDOs, the 23 inconsistent AUDIT-C abstainers were assigned the response ‘Never’ to AUD3.
Cohen's kappa was used to assess the level of agreement between dichotomous measures of: (a) AUDIT-C abstention and MHI abstention; (b) AUDIT-C monthly+ HDOs and MHI monthly+ HDOs; and (c) AUDIT-C weekly+ HDOs and MHI weekly+ HDOs (Cohen, 1960). Kappa analyses were performed overall and by gender, and Altman's guidelines for interpreting kappa were used, for which kappa values of 0.81–1.00 indicate very good strength of agreement, and 0.61–0.80 good agreement (Altman, 1991).
The prevalence of each of the four possible classifications of consistency between the two instruments was described for abstention and HDO measures, both overall and by gender. For inconsistent abstainers and participants with inconsistent monthly+ or weekly+ HDOs, alcohol consumption reports from the other instrument were described. For participants with inconsistent AUDIT-C monthly+ and weekly+ HDOs, the association between gender and proportion of highly discordant MHI reports was assessed with a chi-square test and Fisher's exact test, respectively.
Chi-square tests assessed statistical significance of associations between gender and the dichotomous measures of inconsistent abstention, inconsistent monthly+ HDOs and inconsistent weekly+ HDOs. Secondary analyses were performed to examine associations between gender and inconsistent HDO reports among heavier drinkers. For these exploratory analyses, gender associations with inconsistent monthly+ and weekly+ HDOs were calculated only for participants who reported monthly+ HDOs or weekly+ HDOs on at least one measure, respectively.
Logistic regression was used to model associations of dichotomous measures of inconsistent abstention and inconsistent HDO frequency with survey order and SES. Overall and sex-specific logistic regression models were run for inconsistent monthly+ HDOs and inconsistent weekly+ HDOs, while abstainer sample sizes were insufficient for sex-specific models.
When estimating prevalence and associations of abstention and HDO frequency by instrument, HDO analyses included only past-year drinkers as measured by the drinking frequency question for each instrument (AUDIT-C n = 853; MHI n = 873). For each instrument, chi-square tests assessed statistical significance of associations between gender and the dichotomous measures of abstention and HDO frequency. Logistic regression was used to estimate associations of dichotomous AUDIT-C or MHI measures of alcohol consumption (i.e. past-year drinking or abstention, <monthly or monthly+ HDOs, and <weekly or weekly+ HDOs) with sex, SES score and SES categories. Statistical significance of each variable was calculated with the likelihood ratio chi-square test, and the score test for linear trend of log odds was used for inconsistency trends across SES categories. P-values <0.05 were considered statistically significant to mirror common practice.
RESULTS
Consistency of AUDIT-C and MHI single-item measures of alcohol consumption
Abstention
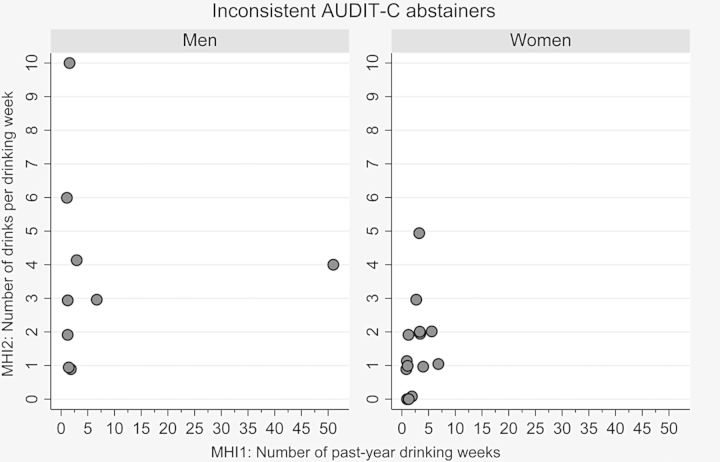
Of the 923 participants who completed the AUDIT-C and MHI, 97% of men and women consistently reported past-year abstention or drinking. Kappa-statistics indicated a ‘good’ quality of agreement between the AUDIT-C and MHI items (i.e. AUD1 and MHI1), with overall and sex-specific Cohen's kappa values ranging from 0.74 to 0.79. Overall, 6.5% of men and 9.4% of women reported abstention on at least one instrument, with more than one-third of these reporting abstention on one instrument and alcohol consumption on the other (Table 2 and Fig. 1).
Table 2.
Summary of inconsistencies between abstention and heavy drinking frequency classifications, based on AUDIT-C and MHI single-item measures
| Men |
Women |
Total |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Past-year abstainers and drinkers | ||||||
| Consistent abstainers | 18 | 3.9 | 29 | 6.3 | 47 | 5.1 |
| Consistent drinkers | 434 | 93.5 | 416 | 90.6 | 850 | 92.1 |
| Inconsistent AUDIT-C abstainers | 9 | 1.9 | 14 | 3.1 | 23 | 2.5 |
| Inconsistent MHI abstainers | 3 | 0.6 | 0 | 0.0 | 3 | 0.3 |
| Total | 464 | 100.0 | 459 | 100.0 | 923 | 100.0 |
| Total inconsistent: 2.6% men and 3.1% women (P-value for sex differencesa = 0.670) | ||||||
| Past-year frequency of heavy drinking occasions (HDOs) in current drinkersb | ||||||
| Monthly HDOs | ||||||
| Consistent <monthly HDOs | 188 | 42.2 | 281 | 65.3 | 469 | 53.5 |
| Consistent monthly+ HDOs | 196 | 43.9 | 100 | 23.3 | 296 | 33.8 |
| Inconsistent AUDIT-C monthly+ HDOs | 35 | 7.8 | 25 | 5.8 | 60 | 6.9 |
| Inconsistent MHI monthly+ HDOs | 27 | 6.1 | 24 | 5.6 | 51 | 5.8 |
| Total | 446 | 100.0 | 430 | 100.0 | 876 | 100.0 |
| Total inconsistent: 13.9% men and 11.4% women (P-value for sex differencesa = 0.265) | ||||||
| Weekly HDOs | ||||||
| Consistent <weekly HDOs | 292 | 65.5 | 363 | 84.4 | 655 | 74.8 |
| Consistent weekly+ HDOs | 94 | 21.1 | 38 | 8.8 | 132 | 15.1 |
| Inconsistent AUDIT-C weekly+ HDOs | 38 | 8.5 | 20 | 4.7 | 58 | 6.6 |
| Inconsistent MHI weekly+ HDOs | 22 | 4.9 | 9 | 2.1 | 31 | 3.5 |
| Total | 446 | 100.0 | 430 | 100.0 | 876 | 100.0 |
| Total inconsistent: 13.5% men and 6.7% women (P-value for sex differencesa = 0.001) | ||||||
aP-values from chi-square tests that assessed the association between sex and dichotomous measures of inconsistent abstention, inconsistent monthly+ HDOs and inconsistent weekly+ HDOs.
bParticipants who reported past-year alcohol consumption on at least one instrument.
Fig. 1.
MHI reports of alcohol consumption frequency and quantity for inconsistent AUDIT-C abstainers (n = 23).
Among all inconsistent abstainers (men: n = 12; women: n = 14), 75% of men and 100% of women were AUDIT-C abstainers but MHI drinkers. These 9 men and 14 women (inconsistent AUDIT-C abstainers) generally reported infrequent, low-volume drinking on the MHI. Figure 1 shows how all except one of these participants reported six or fewer past-year drinking weeks on the MHI, with women generally reporting fewer weekly drinks than men. Three inconsistent AUDIT-C abstainers reported past-year HDOs on the MHI, with one woman reporting five HDOs, one man reporting a single HDO and the other man 17 HDOs. The three men who were inconsistent MHI abstainers were all infrequent ‘monthly or less' AUDIT-C drinkers. Of these, two were also low-volume drinkers (i.e. one drink per drinking day) with no past-year HDOs. The remaining man reported 10+ drinks per drinking day and ‘less than monthly’ HDOs.
Heavy drinking occasions
For the 446 men and 430 women who reported past-year drinking on at least one instrument, kappa-statistics for monthly and weekly HDO classifications all suggested ‘good agreement’ between the MHI3 and AUD3 HDO frequency questions. Overall and sex-specific Cohen's kappa values ranged from 0.72 to 0.74 for dichotomous measures of monthly+ HDOs, and from 0.67 to 0.69 for weekly+ HDO measures. Monthly HDOs (<monthly or monthly+ HDOs) were consistent for 86.1% of men and 88.6% of women, while 86.5% of men and 93.3% of women were consistently classified with regard to weekly HDOs (<weekly or weekly+ HDOs). The most common inconsistency pattern was fewer HDOs reported on the MHI than AUDIT-C, particularly for inconsistent weekly HDOs where 38/60 men (63.3%) and 20/29 women (69.0%) reported fewer MHI than AUDIT-C HDOs.
For participants with inconsistent AUDIT-C monthly+ and weekly+ HDOs, many of the inconsistent classifications were due to MHI reports that were slightly below the monthly or weekly cutpoints. However, of participants with inconsistent AUDIT-C monthly+ HDOs, 13/25 women (52%) and 14/35 men (40%) had highly discordant MHI reports of 0–6 HDOs per year, while 7/20 women (35%) and 6/38 men (16%) with inconsistent AUDIT-C weekly+ HDOs had highly discordant MHI reports of 0–12 HDOs per year. These sex differences in proportions of highly discordant reports were not statistically significant.
HDO reports that bordered the monthly and weekly cutpoints were common for participants with inconsistent MHI monthly+ and weekly+ HDOs. Among the 24 women and 27 men with inconsistent MHI monthly+ HDOs, 91.7% of women and 96.3% of men reported ‘less than monthly’ HDOs on the AUDIT-C question, with MHI reports of 12–15 HDOs for 54.2% of women and 59.3% of men. For the 9 women and 22 men with inconsistent MHI weekly+ HDOs, 66.7% of women and 86.4% of men reported monthly AUDIT-C HDOs, with MHI reports exactly on the weekly cutpoint of 52 HDOs for 66.7% of women and 63.6% of men. Marked discordance was seen in six participants (women: n = 3; men: n = 3) who reported 52 or more past-year HDOs on MHI but ‘less than monthly’ AUDIT-C HDOs. Highly discordant reports were also seen in three participants (women: n = 2; men: n = 1) with 12–36 MHI HDOs and ‘never’ HDOs on AUDIT, seven men with MHI reports of 100–350 HDOs and monthly AUDIT-C HDOs, and three women with 68–90 MHI HDOs and monthly AUDIT-C HDOs.
Associations of inconsistent reporting with sex, socioeconomic status and survey order
Table 2 shows that there was no association of sex with inconsistency between dichotomous AUDIT-C and MHI measures of abstinence or monthly+ HDOs, but a statistically significant difference by sex between AUDIT-C and MHI measures of weekly+ HDOs. While the proportion of current drinkers with inconsistent weekly HDOs was significantly higher in men than women, no significant sex differences were found in exploratory analyses that included only heavier drinkers. These analyses found that, among participants who reported weekly+ HDOs on at least one measure (67 women and 154 men), similar proportions of women and men were inconsistent (43.3 and 39.0%, respectively; P = 0.547), suggesting that the sex difference found among current drinkers was due to the higher frequency of weekly+ HDOs in men than women. Among participants who reported monthly+ HDOs on at least one instrument (149 women and 258 men), inconsistency was more common among women than men (32.9 and 24.0%, respectively; P = 0.053).
Lower socioeconomic status (SES) was associated with inconsistent reports of both abstention (trend P = 0.020) and weekly+ HDOs (trend P = 0.013), shown in Table 3. For abstention and weekly+ HDOs, the odds of inconsistent reports in ‘low SES' participants were 4.5 and 2.2 times those of ‘high SES' participants, respectively. When stratified by sex, the association of inconsistent weekly+ HDO reports with decreasing SES was only significant for women (trend P = 0.034). For monthly+ HDOs, there was an opposing finding of less inconsistency with decreasing SES, that was only significant for men (trend P = 0.015). Low abstainer numbers precluded multivariable analysis by sex.
Table 3.
Inconsistent self-reports of abstention and of heavy drinking occasions (HDOs) on AUDIT-C and MHI single-item measures: distributions and unadjusted associations with survey order and socioeconomic statusa
| Men |
Women |
Total |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Totalb | n (%) | OR (95% CI) | P-valuec | Totalb | n (%) | OR (95% CI) | P-valuec | Totalb | n (%) | OR (95% CI) | P-valuec | |
| Inconsistent abstainers (ref: consistent abstainers/drinkers) | ||||||||||||
| Survey order | ||||||||||||
| AUDIT-C 1st | 286 | 7 (2.4%) | 1.00 | 0.711 | ||||||||
| MHI 1st | 626 | 18 (2.9%) | 1.18 (0.49–2.86) | |||||||||
| Socioeconomic status | ||||||||||||
| High SES (5/6) | 283 | 3 (1.1%) | 1.00 | 0.052 | ||||||||
| Mid SES (3/4) | 463 | 14 (3.0%) | 2.91 (0.83–10.2) | |||||||||
| Low SES (1/2) | 174 | 8 (4.6%) | 4.50 (1.18–17.2) | |||||||||
| Trend: 0.020 | ||||||||||||
| Inconsistent monthly+ HDOs (ref: consistent <monthly/monthly+ HDOs)d | ||||||||||||
| Survey order | ||||||||||||
| AUDIT-C 1st | 133 | 30 (22.6%) | 1.00 | <0.001 | 139 | 12 (8.6%) | 1.00 | 0.183 | 272 | 42 (15.4%) | 1.00 | 0.103 |
| MHI 1st | 310 | 31 (10.0%) | 0.38 (0.22–0.66) | 286 | 37 (12.9%) | 1.57 (0.79–3.12) | 596 | 68 (11.4%) | 0.71 (0.47–1.07) | |||
| Socioeconomic status | ||||||||||||
| High SES (5/6) | 120 | 22 (18.3%) | 1.00 | 0.029 | 152 | 19 (12.5%) | 1.00 | 0.513 | 272 | 41 (15.1%) | 1.00 | 0.209 |
| Mid SES (3/4) | 214 | 32 (15.0%) | 0.78 (0.43–1.42) | 228 | 22 (9.7%) | 0.75 (0.39–1.43) | 442 | 54 (12.2%) | 0.78 (0.51–1.21) | |||
| Low SES (1/2) | 112 | 8 (7.1%) | 0.34 (0.15–0.81) | 48 | 7 (14.6%) | 1.20 (0.47–3.04) | 160 | 15 (9.4%) | 0.58 (0.31–1.09) | |||
| Trend: 0.015 | Trend: 0.936 | Trend: 0.079 | ||||||||||
| Inconsistent weekly+ HDOs (ref: consistent <weekly/weekly+ HDOs)d | ||||||||||||
| Survey order | ||||||||||||
| AUDIT-C 1st | 133 | 16 (12.0%) | 1.00 | 0.538 | 139 | 11 (7.9%) | 1.00 | 0.539 | 272 | 27 (9.9%) | 1.00 | 0.830 |
| MHI 1st | 310 | 44 (14.2%) | 1.21 (0.66–2.23) | 286 | 18 (6.3%) | 0.78 (0.36–1.70) | 596 | 62 (10.4%) | 1.05 (0.65–1.70) | |||
| Socioeconomic status | ||||||||||||
| High SES (5/6) | 120 | 14 (11.7%) | 1.00 | 0.608 | 152 | 6 (3.9%) | 1.00 | 0.109 | 272 | 20 (7.4%) | 1.00 | 0.045 |
| Mid SES (3/4) | 214 | 28 (13.1%) | 1.14 (0.57–2.26) | 228 | 17 (7.5%) | 1.96 (0.75–5.09) | 442 | 45 (10.2%) | 1.43 (0.82–2.48) | |||
| Low SES (1/2) | 112 | 18 (16.1%) | 1.45 (0.68–3.07) | 48 | 6 (12.5%) | 3.48 (1.07–11.3) | 160 | 24 (15.0%) | 2.22 (1.19–4.17) | |||
| Trend: 0.329 | Trend: 0.034 | Trend: 0.013 | ||||||||||
aInconsistency categories are combined for each drinking measure as similar patterns were found in most cases.
bTotals differ due to missing data and eight participants for whom the two surveys were not completed in the same day.
cTrend P-values indicate the significance of a score test for linear trend of log odds; all other P-values indicate the statistical significance of each association using the likelihood ratio (LR) chi-square test.
dHDO analyses included current drinkers (i.e. 446 men and 430 women who reported past-year alcohol consumption on at least one instrument).
Bold values represents the associations that were statistically significant (P < 0.05).
Survey order was generally not associated with inconsistent abstention or HDO reports. However, men who answered the MHI questions first were less likely to have inconsistent monthly+ HDO classifications than men who answered the AUDIT-C questions first (OR = 0.38; P < 0.001).
Associations of AUDIT-C and MHI single-item measures of alcohol consumption with sex and socioeconomic status
Prevalence estimates
Table 4 shows higher past-year abstention prevalence on the AUDIT-C than MHI, with statistically significant sex differences in abstainer proportions for the AUD1 question (5.8% of men vs. 9.4% of women; P = 0.041) but not the MHI1 question (4.5% of men vs. 6.3% of women; P = 0.228). Monthly+ and weekly+ HDO prevalence was slightly higher for AUDIT-C than MHI reports (i.e. AUD3 and MHI3) in both women and men. Strong associations between sex and HDO frequency were consistently seen.
Table 4.
Unadjusted associations of past-year abstention and of heavy drinking occasions (HDOs) with sex and socioeconomic status (SES): comparison of AUDIT-C and MHI single-item measures of alcohol consumption
| AUDIT-C |
MHI |
|||||||
|---|---|---|---|---|---|---|---|---|
| Totala | n (%) | OR (95% CI) | P-valueb | Totala | n (%) | OR (95% CI) | P-valueb | |
| Abstention | N = 923 | N = 923 | ||||||
| Overall | ||||||||
| Women | 459 | 43 (9.4%) | 1.00 | 0.041 | 459 | 29 (6.3%) | 1.00 | 0.228 |
| Men | 464 | 27 (5.8%) | 0.60 (0.36–0.99) | 464 | 21 (4.5%) | 0.70 (0.39–1.25) | ||
| SES scorec | 920 | 1.29 (1.08–1.54) | 0.004 | 920 | 1.26 (1.03–1.54) | 0.025 | ||
| SES categories | ||||||||
| High SES (5/6) | 283 | 14 (4.9%) | 1.00 | 0.039 | 283 | 11 (3.9%) | 1.00 | 0.053 |
| Mid SES (3/4) | 463 | 34 (7.3%) | 1.52 (0.80–2.89) | 463 | 22 (4.8%) | 1.23 (0.59–2.58) | ||
| Low SES (1/2) | 174 | 20 (11.5%) | 2.50 (1.23–5.08) | 174 | 16 (9.2%) | 2.50 (1.13–5.53) | ||
| SES trend P-value: 0.011 | SES trend P-value: 0.023 | |||||||
| Women | ||||||||
| SES score | 457 | 1.32 (1.04–1.67) | 0.021 | 457 | 1.22 (0.92–1.60) | 0.165 | ||
| SES categories | ||||||||
| High SES (5/6) | 161 | 10 (6.2%) | 1.00 | 0.051 | 161 | 9 (5.6%) | 1.00 | 0.066 |
| Mid SES (3/4) | 240 | 22 (9.2%) | 1.52 (0.70–3.31) | 240 | 12 (5.0%) | 0.89 (0.37–2.16) | ||
| Low SES (1/2) | 56 | 10 (17.9%) | 3.28 (1.29–8.37) | 56 | 8 (14.3%) | 2.81 (1.03–7.70) | ||
| SES trend P-value: 0.016 | SES trend P-value: 0.095 | |||||||
| Men | ||||||||
| SES score | 463 | 1.37 (1.04–1.81) | 0.025 | 463 | 1.41 (1.02–1.93) | 0.031 | ||
| SES categories | ||||||||
| High SES (5/6) | 122 | 4 (3.3%) | 1.00 | 0.215 | 122 | 2 (1.6%) | 1.00 | 0.119 |
| Mid SES (3/4) | 223 | 12 (5.4%) | 1.68 (0.53–5.32) | 223 | 10 (4.5%) | 2.82 (0.61–13.1) | ||
| Low SES (1/2) | 118 | 10 (8.5%) | 2.73 (0.83–8.97) | 118 | 8 (6.8%) | 4.36 (0.91–21.0) | ||
| SES trend P-value: 0.081 | SES trend P-value: 0.050 | |||||||
| Monthly+ HDOsd | N = 853 | N = 873 | ||||||
| Overall | ||||||||
| Women | 416 | 125 (30.0%) | 1.00 | <0.001 | 430 | 124 (28.8%) | 1.00 | <0.001 |
| Men | 437 | 231 (52.9%) | 2.61 (1.97–3.46) | 443 | 223 (50.3%) | 2.50 (1.89–3.31) | ||
| SES scorec | 852 | 1.28 (1.16–1.41) | <0.001 | 871 | 1.24 (1.13–1.37) | <0.001 | ||
| SES categories | ||||||||
| High SES (5/6) | 269 | 86 (32.0%) | 1.00 | <0.001 | 272 | 83 (30.5%) | 1.00 | <0.001 |
| Mid SES (3/4) | 429 | 186 (43.4%) | 1.63 (1.18–2.24) | 441 | 184 (41.7%) | 1.63 (1.18–2.25) | ||
| Low SES (1/2) | 154 | 83 (53.9%) | 2.49 (1.66–3.73) | 158 | 80 (50.6%) | 2.34 (1.56–3.50) | ||
| SES trend P-value: <0.001 | SES trend P-value: <0.001 | |||||||
| Women | ||||||||
| SES score | 415 | 1.26 (1.07–1.48) | 0.004 | 428 | 1.26 (1.07–1.47) | 0.004 | ||
| SES categories | ||||||||
| High SES (5/6) | 151 | 36 (23.8%) | 1.00 | 0.056 | 152 | 37 (24.3%) | 1.00 | 0.076 |
| Mid SES (3/4) | 218 | 69 (31.7%) | 1.48 (0.92–2.37) | 228 | 67 (29.4%) | 1.29 (0.81–2.06) | ||
| Low SES (1/2) | 46 | 19 (41.3%) | 2.25 (1.12–4.51) | 48 | 20 (41.7%) | 2.22 (1.12–4.39) | ||
| SES trend P-value: 0.016 | SES trend P-value: 0.029 | |||||||
| Men | ||||||||
| SES score | 437 | 1.22 (1.07–1.39) | 0.004 | 443 | 1.17 (1.03–1.33) | 0.017 | ||
| SES categories | ||||||||
| High SES (5/6) | 118 | 50 (42.4%) | 1.00 | 0.023 | 120 | 46 (38.3%) | 1.00 | 0.008 |
| Mid SES (3/4) | 211 | 117 (55.5%) | 1.69 (1.07–2.67) | 213 | 117 (54.9%) | 1.96 (1.24–3.09) | ||
| Low SES (1/2) | 108 | 64 (59.3%) | 1.98 (1.16–3.36) | 110 | 60 (54.5%) | 1.93 (1.14–3.27) | ||
| SES trend P-value: 0.010 | SES trend P-value: 0.012 | |||||||
| Weekly+ HDOsd | N = 853 | N = 873 | ||||||
| Overall | ||||||||
| Women | 416 | 58 (13.9%) | 1.00 | <0.001 | 430 | 47 (10.9%) | 1.00 | <0.001 |
| Men | 437 | 132 (30.2%) | 2.67 (1.89–3.77) | 443 | 116 (26.2%) | 2.89 (2.00–4.18) | ||
| SES scorec | 852 | 1.27 (1.13–1.42) | <0.001 | 871 | 1.36 (1.20–1.54) | <0.001 | ||
| SES categories | ||||||||
| High SES (5/6) | 269 | 42 (15.6%) | 1.00 | <0.001 | 272 | 30 (11.0%) | 1.00 | <0.001 |
| Mid SES (3/4) | 429 | 98 (22.8%) | 1.60 (1.07–2.38) | 441 | 89 (20.2%) | 2.04 (1.31–3.18) | ||
| Low SES (1/2) | 154 | 50 (32.5%) | 2.60 (1.62–4.16) | 158 | 44 (27.8%) | 3.11 (1.86–5.21) | ||
| SES trend P-value: <0.001 | SES trend P-value: <0.001 | |||||||
| Women | ||||||||
| SES score | 415 | 1.47 (1.19–1.83) | <0.001 | 428 | 1.64 (1.29–2.09) | <0.001 | ||
| SES categories | ||||||||
| High SES (5/6) | 151 | 12 (7.9%) | 1.00 | 0.010 | 152 | 6 (3.9%) | 1.00 | <0.001 |
| Mid SES (3/4) | 218 | 35 (16.1%) | 2.22 (1.11–4.42) | 228 | 32 (14.0%) | 3.97 (1.62–9.75) | ||
| Low SES (1/2) | 46 | 11 (23.9%) | 3.64 (1.48–8.94) | 48 | 9 (18.8%) | 5.61 (1.88–16.73) | ||
| SES trend P-value: 0.011 | SES trend P-value: <0.001 | |||||||
| Men | ||||||||
| SES score | 437 | 1.12 (0.97–1.29) | 0.126 | 443 | 1.19 (1.03–1.38) | 0.019 | ||
| SES categories | ||||||||
| High SES (5/6) | 118 | 30 (25.4%) | 1.00 | 0.216 | 120 | 24 (20.0%) | 1.00 | 0.117 |
| Mid SES (3/4) | 211 | 63 (29.9%) | 1.25 (0.75–2.08) | 213 | 57 (26.8%) | 1.46 (0.85–2.51) | ||
| Low SES (1/2) | 108 | 39 (36.1%) | 1.66 (0.94–2.93) | 110 | 35 (31.8%) | 1.87 (1.02–3.40) | ||
| SES trend P-value: 0.082 | SES trend P-value: 0.041 | |||||||
aTotals differ due to three participants with missing SES data.
bTrend P-values indicate the significance of a score test for linear trend of log odds; all other P-values indicate the statistical significance of each variable using the likelihood ratio (LR) chi-square test.
cSES score = 1 (lowest) to 6 (highest); OR for 1-point decrease in SES.
dHDO analyses included either current AUDIT-C or MHI current drinkers who reported past-year alcohol consumption on the AUDIT-C (437 men and 416 women) or MHI (443 men and 430 women).
Bold values represents the associations that were statistically significant (P < 0.05).
Abstention
Participants with lower SES were more likely to report past-year abstention. The magnitude and significance of overall associations of abstention with SES were similar for AUDIT-C and MHI measures, with differences only seen in sex-specific analyses. For women, only AUDIT-C data produced significant associations between abstention and SES. For men, a significant association between abstention and SES score was seen for both measures, but only the MHI data showed a significant trend with SES categories.
Heavy drinking occasions
Participants were more likely to report monthly+ and weekly+ HDOs as SES decreased. The unadjusted associations of monthly+ HDOs with sex and SES were similar in magnitude and significance for AUDIT-C and MHI measures. In contrast, the associations of weekly+ HDOs with SES differed by sex and by instrument. Associations were consistently stronger for the MHI than AUDIT-C measure, partly due to fewer women in the ‘high SES' reference group reporting weekly+ HDOs on MHI3 than AUD3. Both AUDIT-C and MHI measures showed strong associations between weekly+ HDOs and lower SES for participants overall and for women. However, for men, only MHI weekly+ HDO reports were significantly associated with decreasing SES score and SES categorical trend.
DISCUSSION
In the context of this study, we found that: (a) the AUDIT-C drinking frequency question estimated higher past-year abstention prevalence than the MHI question, mostly due to inconsistent responses by infrequent, low-volume MHI drinkers; (b) the bidirectional inconsistency of heavy drinking occasion frequency was largely around category cutpoints; (c) socioeconomic status was associated with inconsistency in reporting abstention and heavy drinking frequency; and (d) the choice of measure affected the significance and magnitude of sex-specific associations of SES with abstention and weekly+ HDOs.
This inconsistency study did not intend to compare the validity of the AUDIT-C versus MHI single-item measures of past-year abstention. However, interview measures of alcohol consumption have been designated as gold standards in a variety of validation studies (Bush et al., 1998; Bradley et al., 2007). We consider it likely that the MHI1 interview question measured past-year drinking status more accurately than the AUD1 survey question in our study, particularly since the MHI question allowed ‘non-abstinent’ participants to report as infrequently as a single past-year drinking week (in comparison to the lowest possible ‘non-abstinent’ AUD1 response of ‘monthly or less'). Since abstention was uncommon, the apparent overestimation by the AUDIT-C was small in absolute terms but large in relative terms, with a 40% increase in abstention prevalence compared with the MHI measure, and one-third of AUDIT-C abstainers reporting drinking in their mental health interview. Similar levels of inconsistency were found among infrequent drinkers in the 2000 National Alcohol Survey, with 27% of respondents who reported usually drinking ‘less than once per year’ (to an alcohol frequency question with eleven response categories and no timeframe) subsequently acknowledging alcohol consumption to a question that specifically asked about having at least one drink during the past year (Midanik and Greenfield, 2003). In an HIV/AIDS study, Broyles et al. (2011) chose not to skip participants past subsequent AUDIT-C questions when they answered ‘never’ to the first AUDIT-C question (‘How often do you have a drink containing alcohol?’), instead adding a ‘0 drinks' option to the second question. They found that 2.6% of the 345 participants responded ‘never’ to drinking frequency, but positive amounts for typical drinking quantity and/or HDO frequency. Our study showed a similar proportion of inconsistent AUDIT-C abstainers, as 2.5% of 923 participants responded ‘never’ to the first AUDIT-C question but reported drinking on the MHI. In a longitudinal analysis of lifetime abstention across three US surveys, Rehm et al. (2008) showed that 52.9% of lifetime abstainers in the 1992 National Alcohol Survey (i.e. participants who chose the drinking frequency response option, ‘I have never had any kind of beverage containing alcohol’) had previously reported drinking.
The AUDIT-C and MHI measures differ, particularly the open-ended nature of MHI questions versus AUDIT's categorical responses. However, mode of administration may have also contributed to more complete ascertainment of current drinking with the MHI. Benefits of self-administered computer surveys have been documented (Couper, 2000; Kypri et al., 2004; Lind et al., 2013), including fuller disclosure of sensitive information, while advantages of using human interviewers have received less attention (Lind et al., 2013). When Lind et al. (2013) unexpectedly found regular drinking reported more often to an interviewer than to an audio computer-assisted self-interviewing survey, they questioned whether the alcohol questions were actually considered sensitive. Low sensitivity in our study could help explain the higher reports of past-year drinking with the MHI, as the advantages of interviewer administration (e.g. probing or clarification) would be unmitigated. Since the MHI was administered by an interviewer and AUDIT-C by a computer for all participants, we cannot disentangle these potential contributors to inconsistent reporting. Therefore, our discussion focuses mainly on providing in-depth descriptions of the magnitude, associations and impacts of inconsistencies for specific subgroups.
There could be substantial implications if the AUDIT overestimates abstention more generally by misclassifying infrequent, low-volume (‘occasional’) drinkers. Studies in populations with a high proportion of occasional drinkers would be most affected, particularly if the difference between abstainers and occasional drinkers is a focus, or where perceived social desirability further increases self-identification as abstainers (i.e. pregnant women) (Goransson et al., 2003). Computer-presented questionnaires may be chosen for these situations to encourage disclosure (Lind et al., 2013), without recognition of the possibility that misclassification of occasional drinkers as abstainers may increase when drinking frequency questions are administered by computer instead of an interviewer. The first AUDIT question is used in some epidemiological studies to skip abstainers past the remaining questions (Kypri et al., 2004, 2009) and/or exclude them from ‘drinkers-only’ analyses (Kypri et al., 2009). It is not always reported if this has been done, but one-third of those excluded in this way could be occasional drinkers. Gender comparisons can also be affected when inconsistency varies by sex. In our sample, differences between AUDIT-C and MHI estimates of abstention prevalence were more marked in women than men, resulting in statistically significant sex differences for AUDIT-C abstention but not MHI. Gender was significantly associated with misclassification of drinking status in the 2000 National Alcohol Survey (Midanik and Greenfield, 2003), with more women than men misclassified as current drinkers when they were actually past-year abstainers (i.e. responding ‘no’ to a follow-up question about having at least one past-year drink, after initially reporting ‘less than once a month but at least once a year’, ‘don't know’, or ‘refused’ to a usual consumption question that lacked a specific timeframe). A longitudinal analysis by Rehm et al. (2008) found that men were more likely to be inconsistent lifetime abstainers. Finally, although abstainer misclassification would affect total AUDIT-C scores, impacts would be small if most inconsistent abstainers were occasional drinkers with low AUDIT-C scores, as in our study.
Misclassification of drinking status and its contribution to apparent protective effects of alcohol on health continues to be a heavily debated topic (Connor, 2006; Fillmore et al., 2007; Chikritzhs et al., 2009; Liang and Chikritzhs, 2011; Stockwell et al., 2012). Misclassification of infrequent drinkers and former drinkers as abstainers is implicated in the observed ‘J-shaped’ protective association between alcohol consumption and health outcomes such as coronary heart disease (CHD), particularly in men (Fillmore et al., 2007; Chikritzhs et al., 2009). The meta-analysis of Fillmore et al. (2007) showed that where ex/occasional drinkers were strictly excluded from abstainer categories, low levels of drinking did not protect against all-cause or CHD mortality. Our study suggests that such misclassification may occur with a commonly used and validated instrument.
Given the importance of abstainer misclassification, we recommend that study participants who identify themselves as abstainers on the first AUDIT question about drinking frequency should be routinely prompted to confirm their response. For example, Harris et al. (2010) accomplished this by including ‘None, I do not drink’ as an additional response option to the second AUDIT question about drinking quantity. Another option that may reduce misclassification is determining past-year abstention with a separate screening question prior to administering alcohol consumption questions, a method that has been used by population health surveys (Ministry of Health, 2008) and studies based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (Dawson et al., 2005; Rubinsky et al., 2013). Adding lower-frequency response options to the first AUDIT question (i.e. between ‘monthly or less' and ‘never’) may reduce misclassification as abstainers, although this has not been tested. These recommendations also apply to other drinking frequency measures used to determine abstention, particularly where questions are similar to the first AUDIT question and are used as a ‘gate’ to further questions.
This study also lends some support to recommendations to include irregular lifetime light drinkers with lifetime abstainers as the most appropriate comparison group in alcohol epidemiology, providing a history of heavier drinking can be ruled out (Rehm et al., 2008). The important distinction in most studies is between those with very low or no lifetime alcohol exposure and all others, and so inclusion reduces misclassification and, potentially, bias in findings. Moreover, our finding that SES scores were associated with both past-year abstention and inconsistent reports of abstention confirms the increased potential for confounding when small numbers of abstainers are used as the reference group (Rehm et al., 2008).
HDO inconsistency was more bidirectional than abstainer inconsistency, but heavy drinking more than once a week was reported less often in the mental health interview despite the MHI definition of heavy drinking occasions requiring one fewer drink than the AUDIT (‘5 or more’ versus ‘6 or more’ drinks on one occasion, respectively). It may be that this question is more sensitive for heavy drinkers in the presence of an interviewer, but it has also been shown previously that survey questions with categorical responses elicit higher HDO frequencies than open-ended questions (Ivis et al., 1997).
The probability of abstainer inconsistency increased markedly as SES decreased. If generalized, this could inflate the association between low SES and abstention commonly reported from research (van Oers et al., 1999; Rodgers et al., 2000; Jefferis et al., 2007; Holahan et al., 2010) and population surveys (Ministry of Health, 2009; Australian Institute of Health and Welfare, 2011), and bias findings where SES is an inadequately-controlled confounder of alcohol's effect on health outcomes (Liang and Chikritzhs, 2012). Midanik and Greenfield (2003) found that dichotomous income and education variables were not significantly associated with misclassification of drinking status in the USA. In our study, weekly+ HDO misclassification in women increased as SES level decreased. However, monthly+ HDO misclassification in men was much less likely as SES decreased and when the MHI was given before the AUDIT-C. Interpretation can only be speculative, but these findings illustrate the importance of a sex-specific approach, and may reflect differences in sensitivity of questions by gender and SES.
In our study, choice of AUDIT-C or MHI measures had little impact on overall associations of alcohol consumption with SES, but several sex-specific associations differed in significance and magnitude. For example, MHI data showed significant associations of abstention with SES score in men but not women. For weekly+ HDOs, the use of MHI instead of AUDIT-C data resulted in SES associations of greater magnitude, and these associations were only significant for men when MHI data were used. Associations of various indicators of low SES with heavy drinking have been previously reported (van Oers et al., 1999; Casswell et al., 2003; Kuntsche et al., 2004; Jefferis et al., 2007; Huckle et al., 2010; Paljärvi et al., 2013), but the potential for differential misclassification of alcohol exposure to affect these associations in a sex-specific manner has not been previously noted.
A limitation of our consistency analysis is the focus on dichotomized alcohol consumption variables (Heavner et al., 2010). We chose this approach for its easily interpretable results that relate directly to issues faced by the numerous studies that use such variables. We focussed on two commonly used indicators of population drinking patterns: proportions of current drinkers and heavy episodic drinkers (Dawson, 2003; Caamano-Isorna et al., 2008; Livingston et al., 2010; Astudillo et al., 2013). Our study population was slightly unusual. Participants are representative of an historical rather than a contemporary population, and the narrow age range may restrict generalizability (while minimizing age-related confounding). Participants have been assessed intermittently throughout their lives and this could have affected responses, although the last visit to the study centre was 6 years previously. Finally, both instruments were administered during a full day of assessments, an uncommon setting for these measures. A strength of the study is the very high response rate, which means that this sample has not been affected by the substantial self-selection seen in most surveys.
CONCLUSIONS
We have shown that inconsistency in reporting of alcohol consumption on the AUDIT-C and MHI measures in this context is sufficient to alter findings, with inconsistent abstention reports having more impact than inconsistent reports of HDO frequency.
The higher level of abstention seen with the AUDIT-C measure could relate to both the range of categorical response options for drinking frequency and the lack of an interviewer to probe responses. We recommend careful consideration of both the instrument and the mode of administration for alcohol data collection, and mechanisms to confirm abstention.
Variation in responses to heavy drinking questions by instrument and subgroup may reflect differences in sensitivity to the questions and the influence of an interviewer. When heavy drinking frequency is central to the investigation, piloting the data collection methods in the target population is warranted.
Associations of SES with abstention, heavy drinking frequency, and inconsistent reporting, many of which differed for men and women, highlight the complex role of SES in alcohol epidemiology and need for a sex-specific approach.
FUNDING
This work was supported by the Health Research Council of New Zealand [12/1086]; the US National Institute of Aging [AG032282] and the UK Medical Research Council [MR/K00381X].
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
We thank the Dunedin Multidisciplinary Health and Development Study members and their families, study director Professor Richie Poulton, and other study staff. We also thank Dr Terrie Moffitt and Dr Nigel Dickson for comments on an earlier draft.
REFERENCES
- Altman D. (1991) Practical Statistics for Medical Research. London: Chapman & Hall. [Google Scholar]
- American Psychiatric Association. (2000) Diagnostic and Statistical Manual of Mental Disorders, DSM-IV-TR (text rev.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Astudillo M, Connor J, Roiblatt RE, et al. (2013) Influence from friends to drink more or drink less: a cross-national comparison. Addict Behav 38:2675–82. [DOI] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare. (2011) 2010 National Drug Strategy Household Survey Report. Drug Statistics Series no. 25. Cat no. PHE 145 Canberra: AIHW. [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, et al. (2007) AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 31:1208–17. [DOI] [PubMed] [Google Scholar]
- Broyles LM, Gordon AJ, Sereika SM, et al. (2011) Do words matter? Incongruent responses to inconsistently worded AUDIT-C alcohol screening instruments. Subst Abus 32:202–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, et al. (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 158:1789–95. [DOI] [PubMed] [Google Scholar]
- Caamano-Isorna F, Corral M, Parada M, et al. (2008) Factors associated with risky consumption and heavy episodic drinking among Spanish university students. J Stud Alcohol Drugs 69:308–12. [DOI] [PubMed] [Google Scholar]
- Casswell S, Pledger M, Hooper R. (2003) Socioeconomic status and drinking patterns in young adults. Addiction 98:601–10. [DOI] [PubMed] [Google Scholar]
- Cheng H, Furnham A. (2013) Correlates of adult binge drinking: evidence from a British cohort . PLoS One 8:e78838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chikritzhs T, Fillmore K, Stockwell T. (2009) A healthy dose of scepticism: four good reasons to think again about protective effects of alcohol on coronary heart disease. Drug Alcohol Rev 28:441–4. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46. [Google Scholar]
- Connor J. (2006) The life and times of the J-shaped curve. Alcohol Alcohol 41:583–4. [DOI] [PubMed] [Google Scholar]
- Couper M. (2000) Web surveys: a review of issues and approaches. Public Opin Q 64:464–94. [PubMed] [Google Scholar]
- Dawson DA. (2003) Methodological issues in measuring alcohol use. Alcohol Res Health 27:18–29. [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, et al. (2005) Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res 29:844–54. [DOI] [PubMed] [Google Scholar]
- Dickson N, Paul C, Herbison P, et al. (1996) The lifetime occurrence of sexually transmitted diseases among a cohort aged 21. N Z Med J 109:308–12. [PubMed] [Google Scholar]
- Ekholm O, Strandberg-Larsen K, Christensen K, et al. (2008) Comparison of assessment methods for self-reported alcohol consumption in health interview surveys. Eur J Clin Nutr 62:286–91. [DOI] [PubMed] [Google Scholar]
- Fillmore KM, Stockwell T, Chikritzhs T, et al. (2007) Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann Epidemiol 17:S16–23. [DOI] [PubMed] [Google Scholar]
- Fone DL, Farewell DM, White J, et al. (2013) Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open 3:e002337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gmel G, Rehm J. (2004) Measuring alcohol consumption. Contemp Drug Probl 31:467–540. [Google Scholar]
- Goransson M, Magnusson A, Bergman H, et al. (2003) Fetus at risk: prevalence of alcohol consumption during pregnancy estimated with a simple screening method in Swedish antenatal clinics. Addiction 98:1513–20. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Kerr WC. (2008) Alcohol measurement methodology in epidemiology: recent advances and opportunities. Addiction 103:1082–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grittner U, Kuntsche S, Gmel G, et al. (2013) Alcohol consumption and social inequality at the individual and country levels: results from an international study. Eur J Public Health 23:332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AH, Bradley KA, Bowe T, et al. (2010) Associations between AUDIT-C and mortality vary by age and sex. Popul Health Manag 13:263–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heavner KK, Phillips CV, Burstyn I, et al. (2010) Dichotomization: 2 × 2 (×2 × 2 × 2...) categories: infinite possibilities. BMC Med Res Methodol 10:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Schutte KK, Brennan PL, et al. (2010) Late-life alcohol consumption and 20-year mortality. Alcohol Clin Exp Res 34:1961–71. [DOI] [PubMed] [Google Scholar]
- Huckle T, You RQ, Casswell S. (2010) Socio-economic status predicts drinking patterns but not alcohol-related consequences independently. Addiction 105:1192–202. [DOI] [PubMed] [Google Scholar]
- Ivis FJ, Bondy SJ, Adlaf EM. (1997) The effect of question structure on self-reports of heavy drinking: closed-ended versus open-ended questions. J Stud Alcohol 58:622–4. [DOI] [PubMed] [Google Scholar]
- Jefferis BJ, Manor O, Power C. (2007) Social gradients in binge drinking and abstaining: trends in a cohort of British adults. J Epidemiol Community Health 61:150–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatsky AL. (2008) Invited commentary: never, or hardly ever? It could make a difference. Am J Epidemiol 168:872–5. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Rehm J, Gmel G. (2004) Characteristics of binge drinkers in Europe. Soc Sci Med 59:113–27. [DOI] [PubMed] [Google Scholar]
- Kypri K, Gallagher SJ, Cashell-Smith ML. (2004) An internet-based survey method for college student drinking research. Drug Alcohol Depend 76:45–53. [DOI] [PubMed] [Google Scholar]
- Kypri K, Paschall MJ, Langley J, et al. (2009) Drinking and alcohol-related harm among New Zealand university students: findings from a National web-based survey. Alcohol Clin Exp Res 33:307–14. [DOI] [PubMed] [Google Scholar]
- Liang W, Chikritzhs T. (2011) Reduction in alcohol consumption and health status. Addiction 106:75–81. [DOI] [PubMed] [Google Scholar]
- Liang W, Chikritzhs T. (2012) Does light alcohol consumption during pregnancy improve offspring's cognitive development? Med Hypotheses 78:69–70. [DOI] [PubMed] [Google Scholar]
- Lind LH, Schober MF, Conrad FG, et al. (2013) Why do survey respondents disclose more when computers ask the questions? Public Opin Q 77:888–935. [Google Scholar]
- Livingston M, Wilkinson C, Laslett AM. (2010) Impact of heavy drinkers on others’ health and well-being. J Stud Alcohol Drugs 71:778–85. [DOI] [PubMed] [Google Scholar]
- Melotti R, Lewis G, Hickman M, et al. (2013) Early life socio-economic position and later alcohol use: birth cohort study. Addiction 108:516–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. (2003) Defining ‘current drinkers’ in national surveys: results of the 2000 National Alcohol Survey. Addiction 98:517–22. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. (2004) Methodological articles in addiction journals: do we need more, less, or about the same amount? Addiction 99:145–7. [DOI] [PubMed] [Google Scholar]
- Milne BJ, Byun U, Lee A. (2013) New Zealand Socio-Economic Index 2006. Wellington: Statistics New Zealand. [Google Scholar]
- Ministry of Health. (2008) A Portrait of Health: Key Results of the 2006/07 New Zealand Health Survey. Wellington: Ministry of Health. [Google Scholar]
- Ministry of Health. (2009) Alcohol Use in New Zealand: Key Results of the 2007/08 New Zealand Alcohol and Drug Use Survey. Wellington: Ministry of Health. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. (2007) Helping Patients Who Drink Too Much: A Clinician’s Guide (Updated 2005 Edition). Washington, DC: National Institutes of Health, US Department of Health and Human Services; NIH Publication 07-3769. [Google Scholar]
- Paljärvi T, Suominen S, Car J, et al. (2013) Socioeconomic disadvantage and indicators of risky alcohol-drinking patterns. Alcohol Alcohol 48:207–14. [DOI] [PubMed] [Google Scholar]
- Probst C, Roerecke M, Behrendt S, et al. (2014) Gender differences in socioeconomic inequality of alcohol-attributable mortality: a systematic review and meta-analysis. Drug Alcohol Rev doi:10.1111/dar.12184. [DOI] [PubMed] [Google Scholar]
- Rehm J, Irving H, Ye Y, et al. (2008) Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. Am J Epidemiol 168:866–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. (2007) The Alcohol Use Disorders Identification Test: an update of research findings. Alcohol Clin Exp Res 31:185–99. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, et al. (1981) National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry 38:381–9. [DOI] [PubMed] [Google Scholar]
- Robins L, Cottler L, Bucholz K, et al. (2000) The Diagnostic Interview Schedule for DSM-IV (DIS-IV). St Louis: Washington University School of Medicine, Department of Psychiatry. [Google Scholar]
- Rodgers B, Korten AE, Jorm AF, et al. (2000) Risk factors for depression and anxiety in abstainers, moderate drinkers and heavy drinkers. Addiction 95:1833–45. [DOI] [PubMed] [Google Scholar]
- Rodgers B, Windsor TD, Anstey KJ, et al. (2005) Non-linear relationships between cognitive function and alcohol consumption in young, middle-aged and older adults: the PATH Through Life Project. Addiction 100:1280–90. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Dawson DA, Williams EC, et al. (2013) AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res 37:1380–90. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, et al. (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction 88:791–804. [DOI] [PubMed] [Google Scholar]
- Silva PA, McCann M. (1996) Introduction to the Dunedin Study. In Silva PA, Stanton WR. (eds). From Child to Adult: the Dunedin Multidisciplinary Health and Development Study. Auckland: Oxford University Press, 1–23. [Google Scholar]
- Smith PC, Schmidt SM, Allensworth-Davies D, et al. (2009) Primary care validation of a single-question alcohol screening test. J Gen Intern Med 24:783–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2009) Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. [Google Scholar]
- Stockwell T, Greer A, Fillmore K, et al. (2012) Health benefits of moderate alcohol consumption: how good is the science? BMJ 344:e2276. [DOI] [PubMed] [Google Scholar]
- van Oers JA, Bongers IM, van de Goor LA, et al. (1999) Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol 34:78–88. [DOI] [PubMed] [Google Scholar]
- Viner RM, Taylor B. (2007) Adult outcomes of binge drinking in adolescence: findings from a UK national birth cohort. J Epidemiol Community Health 61:902–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkin GA, Bray JW, Babor TF, et al. (2004) Alcohol drinking patterns and health care utilization in a managed care organization. Health Serv Res 39:553–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeisser C, Stockwell TR, Chikritzhs T. (2014) Methodological biases in estimating the relationship between alcohol consumption and breast cancer: the role of drinker misclassification errors in meta-analytic results. Alcohol Clin Exp Res 38:2297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]