The “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” project emphasizes professional development in catheter utilization, catheter care, and antimicrobial stewardship as well as promoting patient safety culture, team building, and leadership engagement to reduce catheter-associated urinary tract infection rates in 500 post-acute care facilities and nursing homes.
Keywords: nursing homes, post-acute care facilities, patient safety, CAUTIs
Abstract
Preventing healthcare-associated infection (HAI) is a key contributor to enhancing resident safety in nursing homes. In 2013, the U.S. Department of Health and Human Services approved a plan to enhance resident safety by reducing HAIs in nursing homes, with particular emphasis on reducing indwelling catheter use and catheter-associated urinary tract infection (CAUTI). Lessons learned from a recent multimodal Targeted Infection Prevention program in a group of nursing homes as well as a national initiative to prevent CAUTI in over 950 acute care hospitals called “On the CUSP: STOP CAUTI” will now be implemented in nearly 500 nursing homes in all 50 states through a project funded by the Agency for Healthcare Research and Quality (AHRQ). This “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” will emphasize professional development in catheter utilization, catheter care and maintenance, and antimicrobial stewardship as well as promoting patient safety culture, team building, and leadership engagement. We anticipate that an approach integrating technical and socio-adaptive principles will serve as a model for future initiatives to reduce other infections, multidrug resistant organisms, and noninfectious adverse events among nursing home residents.
The impetus to evaluate, monitor, and enhance resident safety in nursing homes has become increasingly strong as the population receiving care in these facilities expands. Approximately 1.5 million Americans currently reside in 15 700 nursing homes, with 2.5 million short stay admissions in 2010 [1]. Over 40% of all Medicare beneficiaries discharged from hospitals in 2011 required some form of post-acute care [2]. As a result, today's nursing home population is older, sicker, and more functionally dependent than in prior years [3]. The increased acuity of illness in this frail population has been accompanied by an increased risk of adverse events, such as acquiring healthcare-associated infections (HAIs). It is estimated that 22% of Medicare beneficiaries requiring skilled post-acute care experience adverse events during their stay, with infections as one of the most common events [4, 5]. The point prevalence of infections is approximately 5% in Veterans Affairs Community Living Center facilities in the United States [6]. Internationally, a 3-year study of nursing homes in the Netherlands reports a 7.6% prevalence of HAIs, with a range of 0% to 32.4% across facilities [7]. Thus, the overall burden of HAIs in nursing homes parallels and perhaps exceeds that in acute care [8].
Infections in this population are associated with high rates of morbidity and mortality, rehospitalization, extended hospital stay, and substantial healthcare costs [5, 9–12]. Risk factors that predispose older adults to infections include the presence of indwelling devices, recent admission to acute care, functional disability, multi-morbidity, residing in an institutional environment, and the need for extensive healthcare personnel contact [5]. Recognizing the need to prevent infections, the Centers for Medicare & Medicaid Services (CMS) require that nursing homes accepting Medicare and Medicaid residents have infection prevention and control programs [13]. These programs also promote resident safety and are a crucial part of improving quality. Adoption, implementation, and leadership, however, vary substantially in accordance with resident acuity, care philosophy, and culture of the individual facility.
CAUTI in Nursing Homes
Urinary catheters are still frequently used in nursing homes, with catheter prevalence ranging from 5% to 22% of all residents [14–16]. Thus, on any given day, 80 000 to 352 000 of the approximately 1.5 million US post-acute care patients and long-stay residents have a urinary catheter [5, 14–16]. Data from the Minimum Data Set, a federally mandated comprehensive resident assessment, shows that about 13% of all new admissions from acute care to nursing homes arrive with an indwelling urinary catheter [14]. Within a nationwide sample of all Veterans Affairs Community Living Centers providing care for both short-stay post-acute care veterans and long-stay veterans, 14% of 11 500 residents had an indwelling urinary catheter [16]. Use of an indwelling urinary catheter is now one of the publicly reported quality measures for nursing homes [17]. Federal regulations and public reporting has indeed led to increased awareness of when urinary catheters are in place and the need to discontinue inappropriate catheters [18–20]. However, even appropriately placed urinary catheters in nursing home residents often remain in place for prolonged periods during which development of bacteriuria is nearly universal, therefore increasing the risk of catheter-associated urinary tract infection (CAUTI). In a recent study, 166 residents had indwelling catheters for 17 526 device-days, with an average duration of 105 days per catheterized resident [21]. Seventy percent of these residents were post-acute, short-stay residents with less than 90 days of follow-up, and 30% were long-stay residents suggesting a bi-modal pattern in urinary catheter use [21]. In general, residents with indwelling urinary catheters are more functionally disabled than those without [22].
Urinary tract infection (UTI) is the most common infection among nursing home residents. The rates of UTIs are higher in catheterized residents when compared with noncatheterized residents. A study comparing infection rates between nursing home residents who had indwelling devices and those without indwelling devices showed that catheterized residents had 6.2 clinically defined UTIs per 1000 follow-up days requiring at least 5 days of antibiotics compared to 2.8 UTIs/1000 days in noncatheterized residents [22]. Other complications including prostatitis, prostatic abscess, penile ulcerations, obstruction, and trauma are also significant in chronically catheterized residents. At autopsy, catheterized individuals are more likely to have acute pyelonephritis and renal abscess compared with noncatheterized individuals [23].
The majority of patients with long-term indwelling urinary catheters have persistent asymptomatic bacteriuria. One study of bacteriuria in nursing home residents with indwelling catheters noted that nearly 95% of cultures contained ≥50 000 colony forming units per milliliter in a sample of over 200 specimens [24]. More than 50% of episodes of fever in individuals with chronic indwelling catheters are from a urinary source and can lead to bacteremia, sepsis, and death [14, 25–28]. Nursing home residents with chronic indwelling catheters are more likely to have UTIs with multidrug-resistant organisms (MDROs) than residents without these devices [29]. These residents are frequently colonized with MDROs at other anatomic sites with the potential to transfer to other residents [30–33].
In 2013, the US Department of Health and Human Services declared the reduction of HAIs in nursing homes a priority [34]. Based on emerging evidence, prevention priorities, recommendations from professional organizations, and feasibility of implementation, the US government identifies UTI reduction as one of four major focus areas [34]. In order to achieve these goals, the Agency for Healthcare Research and Quality (AHRQ) is funding a nationwide effort to reduce CAUTI in nursing home populations called: “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI.”
This new initiative draws upon 2 specific sources. First, in a recent National Institute on Aging-funded cluster-randomized interventional study, we evaluated the effect of a Targeted Infection Prevention (TIP) multimodal intervention program in reducing MDRO prevalence and device-associated infections in a group of nursing homes in Southeast Michigan [21]. The multimodal intervention included a structured interactive educational program for the staff, hand hygiene promotion, preemptive barrier precautions when assisting with high-risk activities of daily living (bathing, dressing, grooming, toileting, feeding, ambulation), and active surveillance for MDROs and infections with monthly data feedback. In order to achieve its research aims, the TIP study used a primary patient-oriented approach. The results showed a 23% reduction in overall MDRO prevalence-density rate, a 22% reduction in new methicillin-resistant Staphylococcus aureus (MRSA) acquisition, and a 31% reduction in new clinician diagnosed CAUTIs. The “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” uses educational content and evaluation materials developed as part of the TIP project but adapted for a larger national audience.
Second, the “On the CUSP: Stop CAUTI” initiative [35] implemented the Comprehensive Unit-based Safety Program (CUSP) and CAUTI reduction practices in hospital units, with the aim of reducing CAUTI rates in US hospitals. The key components of this project were to centralize coordination and dissemination efforts, emphasizing both technical and socio-adaptive components, and partnering with specialty organizations and governmental agencies. The “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” builds upon many of the organizational and implementation lessons learned from the “On the CUSP: Stop CAUTI” program as described in more detail below.
IMPLEMENTATION
Principles and Components
The “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” national initiative includes a clinical component to augment knowledge and a socio-adaptive component to enhance safety culture. The overarching principles informing this initiative are: (1) to devise simple, evidence-based interventions based on a systematic evidence review of CAUTI prevention; (2) develop resources to build capacity to track CAUTIs and use real-time data in guiding prevention; (3) align clinical CAUTI prevention educational content with socio-adaptive components that address the overall culture of safety; (4) collaborate with quality innovation networks and CMS-mandated quality improvement and performance improvement programs that have expertise in working with healthcare providers and communities [36].
As an initial step to building the clinical component of this initiative, we conducted a systematic review of interventional studies in long-term care settings that evaluated UTI prevention strategies [37]. Briefly, we systematically searched for controlled interventions (randomized or nonrandomized) in English through 25 June 2014 using the electronic databases of Ovid MEDLINE, Cochrane Library via Wiley, CINAHL, Web of Science, and Embase.com. These studies were reviewed for potential interventions to build a nursing home focused CAUTI prevention bundle. A total of 26 records describing 25 controlled interventions were included; several reported decreased UTIs, CAUTIs, or urinary catheter use. This systematic review [37] showed that CAUTI prevention bundles have been implemented with some evidence of success in long-term care settings. These bundles include strategies often found in acute-care bundles (eg, hand hygiene, strategies to avoid placement and prompt removal of catheters, proper catheter insertion/maintenance) plus interventions focused on chronic catheter needs, hydration, incontinence, and preemptive barrier precautions.
Based on this review and considering the fact that new indwelling catheter placement is infrequent, the educational program follows the catheter life-cycle [38] with emphasis on avoiding initial catheter placement, and maintenance for prolonged users. We use the mnemonic “C.A.U.T.I” to highlight the key intervention components (Table 1). It includes general infection prevention strategies such as hand hygiene, barrier precautions during assistance with high-risk activities of daily living such as toileting or bathing, education for infection preventionists and frontline staff, and CAUTI prevention-specific strategies including prompt removal of unnecessary catheters on admission, adopting evidence-based practices for catheter maintenance and insertion, and reducing inappropriate catheter use. Other key content areas emphasize alternatives to indwelling urinary catheters, antimicrobial stewardship, and appropriate use of diagnostic tests such as urinalysis and culture.
Table 1.
C.A.U.T.I Clinical Componenta
| C | Catheter free, catheters in any resident should be assessed for necessity; remove the catheter if there is no appropriate indication for use; every resident deserves a chance to be “catheter free” and “infection free”. |
| A | Aseptic insertion of indwelling catheters, with hand hygiene before and after every resident contact, and barrier precautions (gloves and gowns) during assistance with activities of daily living (ADLs) [21]. |
| U | Use of catheters only if indicated; routine assessment of catheter need (daily in short-stay residents, monthly in long-stay residents) should be conducted and alternatives should be considered (such as intermittent catheterization, use of bladder scanner protocols to decrease need for catheterization, and other noncatheter solutions to incontinence). |
| T | Training and mentorship of staff and family regarding catheter care is important, emphasizing the following points: keep the drainage bag below the bladder, no violations of a “closed” drainage system and appropriate use and care of leg bags, and managing “kinks” in tubing. |
| I | Incontinence care planning to address individual resident challenges and solutions are important, including behavioral interventions such as timed and prompted voiding and appropriate medical management. |
Abbreviation: UTI, urinary tract infection.
a This evidence-based bundle is based on a systematic review of interventional studies in long-term care settings that evaluated UTI prevention strategies [37].
The socio-adaptive component focuses on enhancing the overall structure, process, and practice of infection prevention and resident safety in nursing homes using CAUTI prevention as a model. Leadership engagement and support for infection prevention activities, a team approach, staff empowerment in implementing and facilitating a change, and effective communications between the team members, local organizational leads, quality innovation networks, and other healthcare entities including during care transitions is emphasized.
Educational material related to both the clinical and socio-adaptive components is delivered through in-person conferences, web-based presentations, and conference calls (Table 2). Content developed by the national project team is drawn from multiple resources including prior work from team members, the “On the CUSP: STOP CAUTI” initiative for acute care, national evidence-based guidelines for CAUTI, and educational materials identified by the systematic search for CAUTI prevention interventions in long-term care [8, 21, 35, 37, 39–41].
Table 2.
Overview of the Educational Curriculum
| Activity | Intended Audience | Timeframe (Project Duration: 14 mo) | Objectives | Specific Topics |
|---|---|---|---|---|
| Learning Sessions (Phase 1) | Organizational leads and Nursing Home facility teams | 3 sessions: Two months before project start, midcourse, and project end | To provide an introduction to the program and didactic sessions on clinical and cultural program interventions. |
|
| Onboarding Webinars (Phase 1) | Nursing Home Facility Teams: Focus on direct care healthcare professionals | 5 weekly sessions before project start | To prepare facility teams for implementing cultural and clinical interventions. To present methods to collect, submit and track data to assess progress. |
|
| Training Modules (Phase 2) | Nursing Home Facility Teams: Focus on Infection Preventionists | 4 Biweekly sessions following onboarding | To promote skills development around broad infection prevention topics. |
|
| National Content Calls (Phase 2) | Nursing Home Facility Teams and Organizational Leads | Monthly | To present on clinical and socio-adaptive topics |
Clinical Content:
|
Socio-adaptive content:
| ||||
| Organizational Lead Coaching Calls (Phase 2) | Long-Term Care Facility Teams | Monthly | Facilitated by the organizational lead with support from assigned national project team faculty, this monthly call series provides facility teams an opportunity to discuss how the project is progressing for them, learn from each other, share successes and barriers, and review data on how they are doing within their cohort. | |
| Organizational Lead Calls (Phase 2) | Organizational Leads | Monthly | This monthly call series provides an opportunity for all organizational leads, no matter what cohort, to learn from each other, ask the national project team questions, share successes and barriers, and provide feedback to the national project team on what support or resources they need. | |
Implementation Challenges and Approach
The gap between research and practice remains wide. Recommendations, guidelines, and position papers developed by the ”resource groups,” which include researchers, innovators, and policy makers, have the potential to enhance nursing home care by promoting interventions of proven benefit and discouraging ineffective interventions. However, introducing guidelines into clinical practice by “end users” requires thoughtful, effective, and efficient dissemination and implementation [42–44].
For example, the Centers for Disease Control and Prevention (CDC) and several national societies have issued recommendations for appropriate catheter use and care to prevent CAUTIs [39–41]. However, the distance between evidence and practice remains. In a survey of nursing home healthcare personnel in Southeast Michigan, 25% were unaware of indications for long-term catheter use, 55% were unaware of established practice to maintain a closed drainage system, and 70% were unaware of recommendations against routine bladder irrigation [45]. Similarly, in a United Kingdom study of nursing homes, 35% of healthcare personnel reported performing regular changes of catheter bags and 55% reported giving routine bladder irrigations, both contrary to UK National Institute for Clinical Excellence recommendations [46]. This gap between evidence-based recommendations and their implementation by end users leads to suboptimal adoption and implementation of proven research practices [44, 47, 48]. By collaborating with quality innovation networks and quality improvement and performance improvement programs, this “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” national initiative aims to effectively bridge the gap between researchers and end users.
Another challenge is turnover of leadership (eg, administrators, director of nursing, infection preventionists) and front-line clinical staff (eg, nurses, nursing aids), which may reduce the effectiveness of the educational and socio-adaptive curriculum. Recognizing this barrier, after every onboarding, training, and content session, participating facilities have access to the online session recording as well as train-the-trainer content materials, handouts and posters that can be easily accessed, downloaded, and personalized by the facility to disseminate to front-line clinical staff.
Each participating nursing home has a designated multidisciplinary project team, including 4 required core team roles: facility team lead; administrative champion; survey coordinator, and data coordinator. There are other additional roles that can be helpful including a nurse champion, physician champion, infection control/preventionist, and key members of the clinical staff (eg, RNs, LPNs, and CNAs). In addition, each facility is asked to identify a backup for each core team role to support the project when the primary role designee is unavailable or in the event of turnover to maintain project continuity.
The sustainability of the project at each participating nursing home is a salient issue. Throughout the duration of the project, sustainability is emphasized through the educational content and coaching calls by helping nursing homes identify and implement strategies to prevent CAUTI that will endure in their facilities. Additionally, engaging the leadership and front-line staff in creating a culture of patient safety during the project using CUSP will foster an environment of sustainability.
Implementation Team Partners
With funding from the AHRQ, several key organizations have joined to implement this “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” (Table 3). Health Research and Educational Trust (HRET), a nonprofit affiliate of the American Hospital Association, is providing the project oversight and coordination with various healthcare organizations to recruit the facilities. With the project duration of 3 years, recruitment of nearly 500 nursing homes into the project will occur over the first 2 years in 5 planned cohorts of facilities across all 50 states. Each cohort will be in the study for 14 months (Figure 1).
Table 3.
The National Project Team, “AHRQ Safety Program for Long-Term Care: HAIs/CAUTI”
| National Project Team | Role |
|---|---|
| Agency for Healthcare Research and Quality (AHRQ) | Project funder, provides guidance for achieving project goals |
| Health Research & Education Trust (HRET) | Project oversight, coordination between different organizations |
| University of Michigan | Develop overall content along with evaluation materials, teaching technical and socio-adaptive concepts, develop and assess toolkit materials |
| Baylor College of Medicine | Assist in developing overall content with emphasis on antimicrobial and catheter stewardship |
| Key Partners | |
| Association for Professionals in Infection Control and Epidemiology | Assist in developing and adapting educational materials as well as evaluation measures, teaching technical concepts |
| Centers for Disease Control and Prevention | Overall project implementation, content development, teaching technical concepts, assist in formalizing CAUTI measurements |
| Contrast Creative | Developing visual graphics and toolkit materials that complement educational content |
| Pennsylvania Patient Safety Authority | Assist in developing content, teaching technical concepts |
| Qualidigm | Developing long-term care resources |
| Society for Hospital Medicine | Key faculty in educational delivery |
Abbreviations: AHRQ, Agency for Healthcare Research and Quality; CAUTI, catheter-associated urinary tract infection; HAI, healthcare-associated infection.
Figure 1.
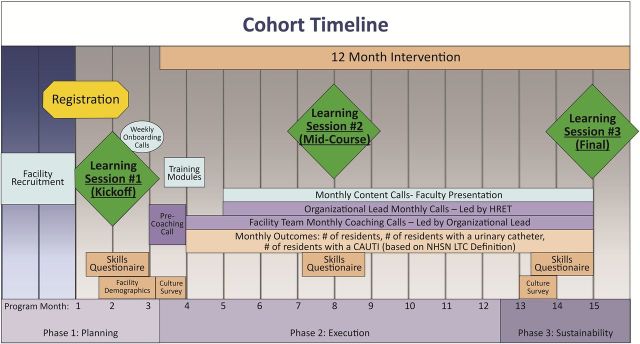
“AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” project timeline for each cohort. Abbreviations: AHRQ, Agency for Healthcare Research and Quality; CAUTI, catheter-associated urinary tract infection; HAI, healthcare-associated infection; HRET, Health Research and Educational Trust; LTC, long-term care; NHSN, National Healthcare Safety Network.
The national project team includes an interdisciplinary group composed of faculty members from geriatrics and aging research, general internal medicine, nursing, infectious diseases, epidemiology, and health services research. Additional national partners include the Association for Professionals in Infection Control and Epidemiology, Abt Associates, Contrast Creative, Pennsylvania Patient Safety Authority, Qualidigm, and the Society of Hospital Medicine. The CDC is an interagency partner.
The national project team has developed additional relationships with national organizations working on nursing home quality improvement. These national organizations in turn support regional, state, or corporation-based organizational leads. The organizational leads recruit and engage the facilities and monitor their progress. This allows the organizational lead to leverage their relationships with their facilities, act as a liaison to the national team, and provide the maximum level of support at the local level.
Learning sessions before the start of this initiative, hosted by each lead organization, inform each facility team on the goals of the project and provide an overview of the interventions, as well as the benefits and expectations of participation (Table 2). To help prepare teams, 5 weekly onboarding webinars are delivered at the start of the project, followed by 4 biweekly webinars to support broad infection prevention practices. Monthly national content and coaching calls provide additional in-depth material on both the clinical and socio-adaptive strategies for CAUTI prevention (Figure 1). There are also opportunities for teams and organizational leads to share their experiences, successes, and barriers.
MEASUREMENT AND EVALUATION
The effectiveness of this “AHRQ Safety Program in Long-Term Care: HAIs/CAUTI” initiative is being evaluated by measuring changes in CAUTI rates, catheter utilization [49], and improvements in staff knowledge on CAUTI prevention and safety culture (Table 4).
Table 4.
Process and Outcome Measures
| Measure | Definition | Frequency of Data Collection and Reporting | Data Collection System |
|---|---|---|---|
| Urinary Catheter Use | Number of urinary catheter-days divided by the total number of resident-days | Daily collection, monthly reporting | HRET Comprehensive Data System |
| NHSN LTC CAUTI rate | Number of NHSN defined CAUTIs divided by the number of urinary catheter-days multiplied by 1000 | Monthly | HRET Comprehensive Data System or CDC NHSN |
| Population based CAUTI rate | Number of NHSN defined CAUTIs divided by the total number of resident-days multiplied by 1000 | Monthly | HRET Comprehensive Data System |
| Staff Skills Questionnaire | Response accuracy by item and category:
|
Collected three times throughout cohort participation during project in-person events | Online survey system (Cvent) |
| AHRQ – Nursing Home Survey on Patient Safety Culture | Response frequencies for each of the 42 items and 12 dimensions, including their composite scores:
|
Twice: once at the beginning and end of cohort participation | Online survey system (Cvent) |
Abbreviations: AHRQ, Agency for Healthcare Research and Quality; CAUTI, catheter-associated urinary tract infection; CDC, Centers for Disease Control and Prevention; HRET, Health Research and Educational Trust; LTC, long-term care; NHSN, National Healthcare Safety Networks.
CAUTIs in nursing homes are variably defined using clinical definitions, original McGeer's surveillance criteria, Loeb's minimum diagnostic criteria to initiate antibiotics, and revised McGeer's surveillance criteria [50–52]. Several of these definitions have been applied and compared in recent studies. Wang and colleagues [22] found that of the 197 clinically defined infections, only 33 (17%) met either Loeb's minimum criteria or McGeer's criteria. In another study using minimum criteria for initiating antibiotics for UTI [50] in residents with advanced dementia, D'Agata et al [53] showed identical results. Training in the use of CAUTI surveillance definitions, appropriate use, and interpretation of urine diagnostics, and the judicious use of antimicrobials are therefore key components of the clinical intervention.
Although teaching use of a new data entry system in long-term care may initially be challenging, reporting data into the CDC's National Healthcare Safety Network (NHSN) will allow facilities to monitor their infection rates and sustain reporting beyond this current project. The NHSN long-term care UTI reporting module uses the nursing home-specific revised McGeer's definitions [52]. An educational curriculum is being used to train facility leads to report data into NHSN. Facilities also have the option of reporting data through the HRET's Comprehensive Data System.
Other outcomes include enhancements in staff knowledge and changes to nursing home safety culture. Staff knowledge pertaining to catheter care, CAUTI, and infection prevention are being assessed through the use of a skills questionnaire. The questionnaire is administered 3 times during the study and includes questions from each topic covered in onboarding and training session webinars (Figure 1). These data are assessed to monitor changes in staff knowledge over time and evaluate the appropriateness of the webinar materials. In addition, each onboarding and training session webinar includes real-time interactive polling questions to assess staff knowledge and facilitate discussion during the webinars. Safety culture is being assessed at the beginning and at the end of the study using the Nursing Home Survey on Patient Safety (Table 4).
CONCLUSIONS
UTIs are the most common infections among residents of nursing homes. Using CAUTI reduction as a model and building on lessons learned from prior National Institute on Aging and AHRQ-funded research in reducing HAIs, we are scaling up our interventions to reach over 500 nursing homes across the nation. Focusing on capacity building, culture change, and sustainability, we are using experienced linkage systems including quality innovation networks and quality improvement and performance improvement programs to bridge the gap between evidence and end-users. Our model has the potential to enhance nursing home resident safety by catalyzing, accelerating, and enhancing the implementation of interventions with known efficacy while engaging nursing home providers with varying levels of infection prevention expertise.
Notes
Disclosures. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support. This work was supported by a contract from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services, Contract Number: HHSA 2902010000251. Other Funding/Support provided by the National Institutes of Health (NIH) (R01 AG032298, R01 AG41780, R18 HS019979 to L. M.; NIH DK092293 to B. W. T.); the University of Michigan Claude D. Pepper Older Americans Independence Center (NIA P30 AG024824 to L. M.); AHRQ (1K08-HS019767-01to J. M.); National Institutes of Health Clinical Loan Repayment Program (2009-2015 to J. M.); Department of Veterans Affairs [VA RRP 12-433 to B. W. T.]; Center for Innovations in Quality, Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston, Texas [CIN13-413 to B. W. T.].
Potential conflicts of interest. All authors: No potential conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Medicare & Medicaid Services. Office of Information Services: Data from the MEDPAR files: Medicare provider analyses and review. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareMedicaidStatSupp/2011.html (Table 6.2). Accessed 9 June 2014.
- 2. Medicare post-acute care reforms. Hearing before the Health Subcommittee of the Committee of Ways and Means. House of Representatives, 113th Cong. 1 2013. Testimony of Mark E. Miller, Medicare Payment Advisory Commission. Available at: http://www.medpac.gov/documents/congressional-testimony/20130614_wandm_testimony_pac.pdf Accessed 9 June 2014.
- 3.Jones A, Dwyer L, Bercovitz A, et al. The National Nursing Home Survey: 2004 Overview. Vital Health Stat 2009; 13:1–164. [PubMed] [Google Scholar]
- 4. US Department of Health and Human Services, Office of the Inspector General. Adverse Events in Skilled Nursing Facilities: National Incidence Among Medicare Beneficiaries. Available at: http://oig.hhs.gov/oei/reports/oei-06-11-00370.pdf Accessed 6 June 2014.
- 5.Strausbaugh L, Joseph C. The burden of infection in long-term care. Infect Control Hosp Epidemiol 2000; 21:674–9. [DOI] [PubMed] [Google Scholar]
- 6.Tsan L, Davis C, Langberg R, et al. Prevalence of nursing home-associated infections in the Department of Veterans Affairs nursing home care units. Am J Infect Control 2008; 36:173–9. [DOI] [PubMed] [Google Scholar]
- 7.Eikelenboom-Boskamp A, Cox-Claessens J, Boom-Poels P, et al. Three-year prevalence of healthcare-associated infections in Dutch nursing homes. J Hosp Infect 2011; 78:59–62. [DOI] [PubMed] [Google Scholar]
- 8.Smith PW, Bennett G, Bradley SF, et al. Infection prevention and control in long-term care facilities. Infect Control Hosp Epidemiol 2008; 29:785–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teresi JA, Holmes D, Bloom HG, Monaco C, Rosen S. Factors differentiating hospital transfers from long-term care facilities with high and low transfer rates. Gerontologist 1991; 31:795–806. [DOI] [PubMed] [Google Scholar]
- 10.Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7- and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. J Am Med Dir Assoc 2011; 12:95–203. [DOI] [PubMed] [Google Scholar]
- 11.Boockvar KS, Gruber-Baldini AL, Burton L, Zimmerman S, May C, Magaziner J. Outcomes of infection in nursing home residents with and without early hospital transfer. J Am Geriatr Soc Apr 2005; 53:590–6. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed AA, Hays CL, Liu B, et al. Predictors of in-hospital mortality among hospitalized nursing home residents: an analysis of the National Hospital Discharge Surveys 2005–2006. J Am Med Dir Assoc 2010; 11:52–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Medicare & Medicaid Services. Revisions to Appendix PP – “Interpretive Guidelines for Long-Term Care Facilities,” “Tag F441”, 2009. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/r51soma.pdf Accessed 13 October 2014.
- 14.Rogers MA, Mody L, Kaufman S, et al. Use of urinary collection devices in skilled nursing facilities in five states. J Am Geriatr Soc 2008; 56:854–61. [DOI] [PubMed] [Google Scholar]
- 15.Kunin CM, Douthitt S, Dancing J, et al. The association between the use of urinary catheters and morbidity and mortality among elderly patients in nursing homes. Am J Epidemiol 1992; 135:291–301. [DOI] [PubMed] [Google Scholar]
- 16.Tsan L, Langberg R, Davis C, et al. Nursing-home associated infections in the Department of Veterans Affairs community living centers. Am J Infect Control 2010; 38:461–6. [DOI] [PubMed] [Google Scholar]
- 17. Centers for Medicare & Medicaid Services. Nursing Home Quality Initiative Overview. Available at: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/index.html Accessed 6 June 2014.
- 18.Hawes C, Mor V, Phillips CD, et al. The OBRA-87 nursing home regulations and implementation of the Resident Assessment Instrument: effects on process quality. J Am Geriatr Soc 1997; 45:977–85. [DOI] [PubMed] [Google Scholar]
- 19.Zhang X, Grabowski DC. Nursing home staffing and quality under the nursing home reform act. Gerontologist 2004; 44:13–23. [DOI] [PubMed] [Google Scholar]
- 20.Werner RM, Konetzka RT, Kim MM. Quality improvement under nursing home compare: the association between changes in process and outcome measures. Med Care 2013; 51:582–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mody L, Krein SL, Saint S, et al. Targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial. JAMA Intern Med 2015; doi:10.1001/jamainternmed.2015.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang L, Lansing B, Symons K, et al. Infection rate and colonization with antibiotic-resistant organisms in skilled nursing facility residents with indwelling devices. Eur J Microbiol Infect Dis 2012; 31:1797–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicolle LE; SHEA Long-Term-Care-Committee. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol 2001; 22:167–75. [DOI] [PubMed] [Google Scholar]
- 24.Smith PW, Seip CW, Schafer SC, et al. Microbiologic survey of long-term care facilities. Am J Infect Control 2000; 28:8–13. [DOI] [PubMed] [Google Scholar]
- 25.Nicolle LE. Urinary catheter-associated infections. Infect Dis Clin North Am 2012; 26:13–27. [DOI] [PubMed] [Google Scholar]
- 26.Maki DG. Nosocomial bacteremia. An epidemiologic overview. Am J Med 1981; 70:719–32. [DOI] [PubMed] [Google Scholar]
- 27.Platt R, Polk BF, Murdock B, et al. Mortality associated with nosocomial urinary tract infection. N Engl J Med 1982; 307:637–42. [DOI] [PubMed] [Google Scholar]
- 28.Maki DG, Tambyah PA. Engineering out the risk of infection with urinary catheters. Emerg Infect Dis 2001; 7:342–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Terpenning MS, Bradley SF, Wan JY, et al. Colonization and infection with antibiotic-resistant bacteria in a long-term care facility. J Am Geriatr Soc 1994; 42:1062–9. [DOI] [PubMed] [Google Scholar]
- 30.Mody L, Maheshwari S, Galecki A, et al. Indwelling device use and antibiotic resistance in nursing homes: identifying a high-risk group. J Am Geriatr Soc 2007; 55:1921–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mody L, Kauffman CA, Donabedian S, et al. Epidemiology of Staphylococcus aureus colonization in nursing home residents. Clin Infect Dis 2008; 46:1368–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fisch J, Lansing B, Wang L, et al. New acquisition of antibiotic resistant organisms in nursing homes. J Clin Microbiol 2012; 50:1698–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fryklund B, Haeggman S, Burman LG. Transmission of urinary bacterial strains between patients with indwelling catheters – nursing in the same room and in separate rooms compared. J Hosp Infect 1997; 36:147–53. [DOI] [PubMed] [Google Scholar]
- 34. US Department of Health and Human Services. National action plan to prevent health care-associated infections: road map to elimination, 2013. Available at: http://www.health.gov/hai/pdfs/hai-action-plan-ltcf.pdf Accessed 13 October 2014.
- 35.Fakih MG, George C, Edson BS, et al. Implementing a national program to reduce catheter-associated urinary tract infection: a quality improvement collaboration of state hospital associations, academic medical centers, professional societies, and governmental agencies. Infect Control Hospital Epidemiol 2013; 34:1048–54. [DOI] [PubMed] [Google Scholar]
- 36. Centers for Medicare and Medicaid Services. CMS launches next phase of new Quality Improvement Program. Available at: http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2014-Press-releases-items/2014-07-18.html Accessed 7 August 2014.
- 37.Meddings J, Saint S, Krein S, et al. Systematic Review of Interventions to Reduce Catheter-Associated Urinary Tract Infection (CAUTI) in the Long-Term Care (LTC) Setting [Poster 879]. In: Presented at IDWeek; 8–12 October 2014; Philadelphia, PA Available at: http://www.idweek.org. Accessed 10 October 2014. [Google Scholar]
- 38.Meddings J, Saint S. Disrupting the life cycle of the urinary catheter. Clin Infect Dis 2011; 52:1291–3. [DOI] [PubMed] [Google Scholar]
- 39.Gould CV, Umscheid CA, Agarwal RK, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol 2010; 31:319–26. [DOI] [PubMed] [Google Scholar]
- 40.Lo E, Nicolle LE, Coffin SE, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014; 35:464–79. [DOI] [PubMed] [Google Scholar]
- 41. American Medical Directors Association (AMDA). Clinical Practice Guideline: Urinary incontinence in the long-term care setting. Columbia, MD: AMDA, 2012. [Google Scholar]
- 42.Saint S, Howell JD, Krein SL. Implementation science: how to jump start infection prevention. Infect Control Hosp Epidemiol 2010; 31:S14–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003; 362:1225–30. [DOI] [PubMed] [Google Scholar]
- 44.Davis SM, Peterson JC, Helfrich CD, Cunningham-Sabo L. Introduction and conceptual model for utilization of prevention research. Am J Prev Med 2007; 33:S1–5. [DOI] [PubMed] [Google Scholar]
- 45.Mody L, Saint S, Galecki A, et al. Knowledge of evidence-based urinary catheter care practice recommendations among healthcare workers in nursing homes. J Am Geriatr Soc 2010; 58:1532–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McNulty CA, Bowen J, Foy C, et al. Urinary catheterization in care homes for older people: self-reported questionnaire audit of catheter management by care home staff. J Hosp Infect 2006; 62:29–36. [DOI] [PubMed] [Google Scholar]
- 47.Peterson JC, Rogers EM, Cunningham-Sabo L, et al. A framework for research utilization applied to seven case studies. Am J Prev Med. 2007; 33:S21–34. [DOI] [PubMed] [Google Scholar]
- 48.Rogers EM. Diffusion of innovations. 5th ed New York: Free Press, 2003. [Google Scholar]
- 49. Centers for Disease Control and Prevention; Division of Healthcare Quality and Promotion. National Healthcare Safety Network (NHSN) protocol for tracking infections in long-term care facilities. Urinary Tract Infection (UTI) Event for Long-term Care Facilities, 2013. Available at: http://www.cdc.gov/nhsn/PDFs/LTC/LTCF-UTI-protocol_FINAL_8-24-2012.pdf Accessed 6 June 2014. [Google Scholar]
- 50.Loeb M, Bentley DW, Bradley S, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol 2001; 22:120–4. [DOI] [PubMed] [Google Scholar]
- 51.McGeer A, Campbell B, Emori TG, et al. Definitions of infection for surveillance in long-term care facilities. Am J Infect Control 1991; 19:1–7. [DOI] [PubMed] [Google Scholar]
- 52.Stone ND, Ashraf MS, Calder J, et al. Surveillance definitions of infections in long-term care facilities: revisiting the McGeer criteria. Infect Control Hosp Epidemiol 2012; 33:965–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.D'Agata E, Loeb MB, Mitchell SL. Challenges in assessing nursing home residents with advanced dementia for suspected urinary tract infections. J Am Geriatr Soc 2013; 61:62–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


