Abstract
Aim
Alcohol is a known cardiac toxin and heavy consumption can lead to heart failure (HF). However, the relationship between moderate alcohol consumption and risk for HF, in either men or women, remains unclear.
Methods and results
We examined 14 629 participants of the Atherosclerosis Risk in Communities (ARIC) study (54 ± 6 years, 55% women) without prevalent HF at baseline (1987–89) who were followed for 24 ± 1 years. Self-reported alcohol consumption was assessed as the number of drinks/week (1 drink = 14 g of alcohol) at baseline, and updated cumulative average alcohol intake was calculated over 8.9 ± 0.3 years. Using multivariable Cox proportional hazards models, we examined the relation of alcohol intake with incident HF and assessed whether associations were modified by sex. Overall, most participants were abstainers (42%) or former drinkers (19%), with 25% reporting up to 7 drinks per week, 8% reporting ≥7 to 14 drinks per week, and 3% reporting ≥14–21 and ≥21 drinks per week, respectively. Incident HF occurred in 1271 men and 1237 women. Men consuming up to 7 drinks/week had reduced risk of HF relative to abstainers (hazard ratio, HR 0.80, 95% CI 0.68–0.94, P = 0.006); this effect was less robust in women (HR 0.84, 95% CI 0.71–1.00, P = 0.05). In the higher drinking categories, the risk of HF was not significantly different from abstainers, either in men or in women.
Conclusion
In the community, alcohol consumption of up to 7 drinks/week at early-middle age is associated with lower risk for future HF, with a similar but less definite association in women than in men. These findings suggest that despite the dangers of heavy drinking, modest alcohol consumption in early-middle age may be associated with a lower risk for HF.
Keywords: Alcohol consumption; Heart failure; Men, women, general population
See page 897 for the editorial comment on this article (doi:10.1093/eurheartj/ehv021)
Introduction
Heart failure (HF) is a major public health problem, but data on the relationship between community lifestyle factors, such as alcohol consumption and incident HF, are limited. Although heavy alcohol consumption is associated with impairment in left ventricular function and eventual alcoholic cardiomyopathy with symptomatic HF,1 moderate alcohol intake could, conversely, lower the risk for HF.2,3 However, the association between moderate alcohol intake and the risk of HF is still controversial, as some studies did not find an association4,5 and the cardiovascular mechanisms of potential benefit of alcohol consumption in HF are uncertain.3,6
Myocardial damage may occur as a consequence of direct toxic effects of alcohol or its metabolites by ethanol-induced apoptosis;7 associated hypertension,8 coexisting nutritional deficiencies, or, rarely, toxic additives to alcoholic beverages.9 Conversely, the cardiovascular mechanisms of alcohol benefit in HF may involve the risk reduction for coronary artery disease (CAD),10 neurohormonal changes11 or blood pressure lowering.12,13 Importantly, the balance of risks and benefits is likely to differ in different populations and by gender and across race and age groups.2,14 Women are known to develop alcohol-associated cardiomyopathy at a lower lifetime dose of alcohol compared with men,15 and women have a much greater risk of heart disease death for the same amount of alcohol use.16 Nonetheless, sex-related differences on the effects of alcohol consumption and risk of HF remain relatively unexplored. In the current study, we aimed to assess the association between alcohol intake and the risk of developing HF in men and women, in a large biracial community-based cohort.
Methods
Study population
The Atherosclerosis Risk in Communities (ARIC) Study is an ongoing, prospective observational study. Detailed study rationale, design, and procedures have been previously published.17 The original cohort included 15 792 persons aged 45–64 years recruited between 1987 and 1989 (Visit 1), selected from four communities in the United States: Forsyth County, North Carolina; Jackson, Mississippi; Minneapolis, Minnesota; and Washington County, Maryland. Three subsequent follow-up visits occurred at 3-year intervals, with annual telephone interviews ongoing and conducted between visits. Institutional review boards from each site approved the study, and informed consent was obtained from all participants.
We restricted our analyses to self-described black or white participants (44 exclusions by undetermined race) and excluded those with prevalent or missing HF data (n = 1,039) and those with missing data on alcohol consumption at visit 1 (n = 80). A total of 14 629 U.S. adults aged 45–64 followed prospectively through 2011 (mean of 24 ± 1 years) constitute the sample for the present analysis.
Definition of heart failure
Prevalent HF at visit 1 was defined by Stage 3 or manifest HF according to Gothenburg criteria or the use of medications for HF. The Gothenburg criteria are a validated scoring system composed of three components, cardiac, pulmonary, and therapy, in which Stage 3 or manifest HF requires one point from each component.18 Incident HF at follow-up was defined by HF hospitalization or HF death, according to the International Classification of Diseases-Ninth Revision (ICD-9), code 410 in any position, for HF, obtained by ARIC Study retrospective surveillance of hospital discharges.19,20 Deaths were ascertained through linkage with the National Death Index.
Alcohol consumption
Alcohol consumption was ascertained at all visits by means of an interviewer-administered questionnaire. Subjects were asked if they currently drank alcoholic beverages and, if not, whether they had done so in the past. Current drinkers were asked how often they usually drank wine, beer, or hard liquor. In calculating the amount of alcohol consumed (in g/week), it was assumed that 4 ounces (118 mL) of wine contains 10.8 g, 12 ounces (355 mL) of beer contains 13.2 g, and 1.5 ounces (44 mL) of liquor contains 15.1 g of ethanol. Subsequently, grams of ethanol were converted to drinks per week (14 g of alcohol = 1 drink)) and participants were classified into six categories: former drinkers, abstainers, drinkers of up to 7 drinks/week, ≥7 up to 14, ≥14 up to 21, and ≥21 drinks/week, as in prior publications.6 Cumulative average alcohol intake was calculated using data acquired from questionnaire responses at Visit 1, Visit 2, Visit 3, and Visit 4. Subsequently, we estimated time-updated average consumption of alcohol for a mean time exposure of 8.9 ± 0.3 years. For the purpose of the analysis using cumulative average, participants were classified as abstainers if every time recorded zero for current consumption of any alcoholic beverage in all visits. If a participant was missing alcohol consumption for a certain visit, the measurements from the available years were averaged. In addition, participants were divided into groups, according to the kind of beverage consumption. We classified exclusive consumers of wine, beer, or liquor and analysed its association with incident HF, having as reference category the abstainers in each group.
Covariates
Established definitions for hypertension, obesity, diabetes mellitus, CAD, stroke, and smoking status were used as previously described in the ARIC study.21 An index of physical activity was derived from the physical activity questionnaire of Baecke et al., including physical activity at work and during sports.22 Interviews included assessment of educational level and high education level was defined as college or graduate or professional school attendance. All covariates were ascertained at Visit 1.
Statistical methods
We performed analyses for men and women, for the association between alcohol consumption and HF. For the six groups [former drinkers, abstainers, drinkers of up to 7 drinks/week (<7), ≥7 to 14, ≥14 to 21, and ≥21 drinks/week], summary statistics for covariates were calculated as counts and percentages or means and standard deviation for categorical and continuous data, respectively. Comparisons of baseline characteristics between the six groups were made using Pearson χ2 test and analysis of variance. The rates of incident HF were calculated and expressed as events per 100 person-years at risk.
We estimated multivariable hazard ratios for incident HF, baseline alcohol consumption and time-updated cumulative average alcohol intake classification, using time-updated Cox proportional hazards regression models adjusted for age, body mass index (BMI), total cholesterol and score of physical activity, as continuous variables, and diabetes, hypertension, CAD, education level and smoking status, as categories, with incident myocardial infarction as a time-varying covariate, comparing each level of drinking with abstainers. Tests for violation of the proportional hazards assumption were conducted through the introduction of linear interaction between the time variable and the exposure of interest (categories of alcohol consumption).
In addition to the test for linear trend from the categorical analysis, we also tested for a curvilinear association between the continuous measure of alcohol consumption (grams per week) at baseline and incident HF, via an adjusted Cox model using a restricted cubic spline. For the purpose of the spline analysis, former drinkers were excluded, with abstainers (0 g/week) as the reference group. The number of knots used in the cubic spline model was chosen on the basis of maximizing goodness of fit (i.e. minimizing AIC). Tests for interaction were performed using the likelihood ratio test for the cross-product interaction term between sex, race, and the categories of drinking status.
Finally, as a sensitivity analysis, we analysed incident HF while accounting for the competing risk of non-HF mortality, using the sub-distribution hazards model proposed by Fine and Gray.23 From this model, we estimated the 20-year risk of HF in each alcohol category, adjusting for the previously specified baseline covariates. In order to provide context for these HF estimates, we also estimated the adjusted 20-year risk of all-cause mortality and estimated multivariable hazard ratios for all-cause mortality for each alcohol consumption category. Two-sided P-values of <0.05 were considered significant. Analyses were performed using Stata version 13.1 (Stata Corp., College Station, TX, USA).
Results
Population characteristics
The average age of the study population at baseline was 54 ± 6 years, 45% of participants were men, and 74% were white. Approximately 61% of participants reported no alcohol consumption, being 19% former drinkers and 42% abstainers. About 25% participants drank up to 7 drinks/week, 8% ≥7–14 drinks/week, 3% ≥14 up to 21, and 3% ≥ 21 drinks/week, respectively. Table 1 describes the characteristics of the study population according to categories of alcohol consumption. Abstainers of both genders were more likely to have diabetes mellitus and lower HDL cholesterol when compared with alcohol drinkers, and abstaining women had higher mean BMI than drinkers. Heaviest alcohol consumers (≥21 drinks/week) of both genders were more likely to be smokers, hypertensive, to have a lower BMI, lower level of education and higher mean HDL cholesterol compared with abstainers and lower drinkers. Women from the heaviest alcohol consumption category had lower score in sports physical activity. Age and physical activity at work in both genders were similar across the alcohol consumption groups. Former drinkers were more likely to be smokers, to have lower education level, diabetes mellitus, hypertension, and CAD than abstainers (see Supplementary material online, Table S1).
Table 1.
Baseline characteristics of the 14 629 Atherosclerosis Risk in Communities participants according to alcohol consumption, by sex
| Characteristics | Number of drinks per week |
||||||
|---|---|---|---|---|---|---|---|
| Former drinkers | Abstainers | <7 | ≥7–14 | ≥14–21 | ≥21 | P-value | |
| Men (n, %) | 1464 (22) | 1708 (26) | 1876 (28) | 834 (13) | 339 (5) | 410 (6) | |
| Women (n, %) | 1254 (16) | 4470 (56) | 1752 (22) | 377 (5) | 103 (1) | 42 (0.5) | |
| Total (n, %) | 2718 (19) | 6178 (42) | 3628 (25) | 1,211 (8) | 442 (3) | 452 (3) | |
| Mean drinks/week | |||||||
| M | 0.0 ± 0.0 | 0.0 ± 0.0 | 3.2 ± 1.8 | 10.0 ± 1.9 | 17.0 ± 1.9 | 32.0 ± 14.5 | |
| W | 0.0 ± 0.0 | 0.0 ± 0.0 | 2.8 ± 1.7 | 9.8 ± 1.9 | 16.4 ± 1.8 | 27.5 ± 7.6 | |
| Age (years) | |||||||
| M | 55.1 ± 5.7 | 54.7 ± 5.8 | 54.2 ± 5.8 | 54.3 ± 5.7 | 54.0 ± 5.7 | 54.0 ± 5.8 | <0.001 |
| W | 53.9 ± 5.6 | 53.9 ± 5.7 | 53.0 ± 5.6 | 53.1 ± 5.8 | 53.9 ± 5.7 | 53.4 ± 5.3 | <0.001 |
| Black (%) | |||||||
| M | 418 (29) | 410 (24) | 351 (19) | 159 (19) | 69 (20) | 96 (23) | <0.001 |
| W | 461(37) | 1520 (34) | 289 (17) | 53 (14) | 10 (10) | 8 (19) | <0.001 |
| BMI (kg/m2) | |||||||
| M | 27.6 ± 4.5 | 27.6 ± 4.1 | 27.4 ± 3.9 | 27.2 ± 4.1 | 27.4 ± 4.3 | 26.6 ± 4.3 | <0.001 |
| W | 28.82 ± 6.52 | 28.2 ± 6.1 | 26.1 ± 5.1 | 25.2 ± 4.9 | 24.5 ± 4.3 | 25.7 ± 4.5 | <0.001 |
| Currently smoker (%) | |||||||
| M | 440 (30) | 308 (18) | 470 (25) | 260 (31) | 138 (41) | 208 (51) | <0.001 |
| W | 378 (30) | 817 (18) | 518 (30) | 170 (45) | 53 (52) | 27 (64) | <0.001 |
| Hypertension (%) | |||||||
| M | 497 (34) | 569 (33) | 544 (29) | 273 (33) | 127 (38) | 159 (39) | <0.001 |
| W | 470 (38) | 1551 (35) | 434 (25) | 109 (29) | 27 (27) | 17 (41) | <0.001 |
| DM (%) | |||||||
| M | 237 (16) | 206 (12) | 176 (9) | 75 (9) | 26 (8) | 31 (8) | <0.001 |
| W | 205 (17) | 536 (12) | 92 (5) | 17 (5) | 6 (6) | 3 (7) | <0.001 |
| CAD (%) | |||||||
| M | 151 (10) | 111 (7) | 117 (6) | 43 (5) | 22 (7) | 22 (5) | <0.001 |
| W | 35 (3) | 72 (2) | 13 (0.7) | 7 (2) | 1 (1) | 1 (3) | 0.001 |
| Total cholesterol (mg/dL) | |||||||
| M | 209 ± 40 | 209 ± 39 | 211 ± 39 | 214 ± 41 | 217 ± 42 | 214 ± 40 | 0.001 |
| W | 220 ± 43 | 218 ± 44 | 215 ± 40 | 222 ± 45 | 228 ± 46 | 218 ± 44 | <0.001 |
| HDL cholesterol (mg/dL) | |||||||
| M | 42 ± 12 | 42 ± 12 | 44 ± 13 | 49 ± 16 | 50 ± 15 | 54 ± 19 | <0.001 |
| W | 55 ± 15 | 56 ± 16 | 62 ± 18 | 68 ± 21 | 68 ± 19 | 73 ± 25 | < 0.001 |
| Work physical activity score | |||||||
| M | 2.4 ± 0.9 | 2.4 ± 0.9 | 2.3 ± 0.8 | 2.4 ± 0.8 | 2.4 ± 0.9 | 2.3 ± 0.9 | 0.090 |
| W | 2.1 ± 1.0 | 2.1 ± 0.9 | 2.1 ± 0.9 | 2.0 ± 0.9 | 2.0 ± 0.9 | 2.0 ± 0.9 | 0.445 |
| Sports physical activity score | |||||||
| M | 2.5 ± 0.8 | 2.5 ± 0.8 | 2.7 ± 0.8 | 2.7 ± 0.8 | 2.7 ± 0.8 | 2.4 ± 0.9 | <0.001 |
| W | 2.3 ± 0.8 | 2.3 ± 0.7 | 2.5 ± 0.8 | 2.4 ± 0.8 | 2.4 ± 0.8 | 1.9 ± 0.7 | < 0.001 |
| High education level (%) | |||||||
| M | 371 (25) | 687 (40) | 918 (49) | 385 (46) | 156 (46) | 147 (36) | <0.001 |
| W | 288 (23) | 1339 (30) | 760 (43) | 156 (41) | 156 (41) | 11 (26) | <0.001 |
Data represent mean ± SD or n (%).
BMI, body mass index; DM, diabetes mellitus; CAD, coronary artery disease.
Alcohol intake and risk of incident heart failure
Participants were followed from 1987 to 1989 through 31 December 2011, with a mean of 24 ± 1 years of follow-up. Incident HF occurred in 1271 men and 1237 women. Table 2 shows unadjusted incidence rates of HF according to categories of alcohol consumption. The lowest rate of events occurred among participants consuming up to 7 drinks/week (0.77 in men and 0.53 in women per 100 person-years of follow-up) and the highest was observed among former drinkers. After adjustment for confounders (age, diabetes, hypertension, CAD, BMI, total cholesterol, physical activity, education level, smoking status, and incident myocardial infarction as a time-varying covariate) men consuming up to 7 drinks/week had significantly reduced risk of HF relative to abstainers (HR 0.80, 95% CI 0.68–0.94, P = 0.006) while women from the same category had a similar, but marginally significant, reduction by baseline alcohol intake (HR 0.84, 95% CI 0.71–1.00, P = 0.05) and a significantly reduced risk of HF when considering cumulative average consumption (HR 0.78, 95% CI 0.62–0.98, P = 0.033) (Table 3). Former drinkers had the highest risk of HF, whereas among participants from the higher drinking categories the risk of HF was not significantly different from abstainers, either in men or in women. The only violation of the proportional hazards assumption was found regarding the risk of HF among women who were former drinkers. For these women, the risk of HF relative to abstainers is estimated to be highest at the time of visit 1 (HR = 1.78, 95% CI 1.27–2.49, P = 0.001) and declines by ∼3% per year thereafter (P = 0.008 for interaction between exposure and follow-up time).
Table 2.
Rate of incident heart failure by baseline alcohol consumption category, by sex
| Incident heart failure | Number of events |
Rates of HF per 100 person-years |
||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Former drinkers | 376 | 266 | 1.50 (1.36–1.66) | 1.12 (0.99–1.26) |
| Abstainers | 333 | 717 | 1.02 (0.92–1.14) | 0.79 (0.74–0.85) |
| No of drinks per week | ||||
| <7 | 281 | 191 | 0.77 (0.69–0.87) | 0.53 (0.46–0.61) |
| ≥7–14 | 144 | 44 | 0.91 (0.78–1.06) | 0.57 (0.42–0.77) |
| ≥14–21 | 62 | 14 | 0.95 (0.74–1.22) | 0.71 (0.42–1.19) |
| ≥21 | 75 | 5 | 1.07 (0.85–1.34) | 0.64 (0.27–1.55) |
Table 3.
Adjusted hazard ratio of incident heart failure, by alcohol consumption categories, at baseline and from time-updated cumulative average alcohol intake, by sex
| Incident heart failure | Hazard ratio (HR 95% CI) |
P–value | Hazard ratio (HR 95% CI) |
P-value |
|---|---|---|---|---|
| Men |
Women |
|||
| Baseline alcohol consumption classification | ||||
| Abstainers | – | – | ||
| Former drinkers | 1.19 (1.02–1.39) | 0.024 | 1.17 (1.01–1.36) | 0.032 |
| No of drinks per week | ||||
| <7 | 0.80 (0.68–0.94) | 0.006 | 0.84 (0.71–1.00) | 0.050 |
| ≥7–14 | 0.92 (0.75–1.13) | 0.426 | 0.93 (0.68–1.27) | 0.637 |
| ≥14–21 | 0.86 (0.65–1.13) | 0.282 | 1.24 (0.72–2.12) | 0.435 |
| ≥21 | 0.98 (0.75–1.28) | 0.878 | 0.78 (0.29–2.09) | 0.616 |
| Cumulative drinking classification | ||||
| Abstainers | – | – | ||
| Former drinkers | 0.91 (0.77–1.08) | 0.277 | 1.02 (0.90–1.17) | 0.726 |
| No of drinks per week | ||||
| <7 | 0.79 (0.63–0.97) | 0.027 | 0.78 (0.62–0.98) | 0.033 |
| ≥7–14 | 0.84 (0.67–1.06) | 0.150 | 1.00 (0.72–1.40) | 0.995 |
| ≥14–21 | 0.81 (0.60–1.11) | 0.191 | 0.78 (0.32–1.89) | 0.581 |
| ≥21 | 0.86 (0.62–1.18) | 0.347 | 1.01 (0.32–3.16) | 0.988 |
Models are adjusted for age, diabetes, hypertension, CAD, BMI, total cholesterol, physical activity, education level, smoking status, and incident myocardial infarction as time-varying covariate.
The association between the continuous measure of alcohol consumption at baseline and incident HF demonstrated a J-shaped association between mild alcohol consumption and risk of HF both in men and in women. However, the curve showed more pronounced reduction of HF risk for men than for women, and only among men were mild drinkers found to have a significantly lower risk of HF compared with abstainers (Figure 1). Nevertheless, there was no significant interaction between sex and alcohol intake with respect to risk of HF (P-value = 0.474). Similarly, when analysing differences between white and black participants, there was no significant interaction between race and incident HF (P-value = 0.535).
Figure 1.
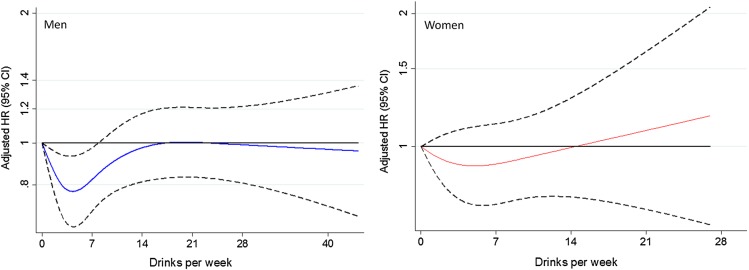
Multivariate analysis of relative risk of incident heart failure as a function of alcohol intake at baseline, by sex, fitted by a restricted cubic spline Cox proportional hazards model. The 95% confidence intervals are indicated by the dash lines. Models are adjusted for age, diabetes, hypertension, CAD, BMI, total cholesterol, physical activity, education level, smoking status, and incident myocardial infarction as time-varying covariate.
When assessing the association between exclusive wine, beer, or liquor drinking and the risk of HF, there were no significant differences between drinkers and abstainers (see Supplementary material online, Table S2). Though, the number of participants exclusively drinking one type of alcohol was limited, precluding additional interpretation by type of drink.
Sensitivity analyses
There was an increased risk for all-cause mortality among men (HR 1.47, 95% CI 1.23–1.75) and women (HR 1.89, 95% CI 1.18–2.99) reporting alcohol intake of ≥21 drinks/week at baseline, and an increase in all-cause mortality among women with a cumulative average intake of ≥14–21 drinks/week (HR 1.87, 95% CI 1.22–2.86) (see Supplementary material online, Table S3). However, the risk of incident HF by alcohol consumption, accounting for the competing risk of non-HF mortality, is similar to the results from the primary analysis (Table 4). Adjusted cumulative incidence curves of incident HF and all-cause mortality for baseline alcohol consumption, by sex, are presented in the Supplementary material online, Figure S1.
Table 4.
Twenty-year risk of incident heart failure and death by alcohol consumption category, by sex
| 20-year risk HF (%) | Number of drinks per week |
|||||
|---|---|---|---|---|---|---|
| Former drinkers | Abstainers | <7 | ≥7–14 | ≥14–21 | ≥21 | |
| Men | ||||||
| HF (primary results)a | 0.17 (0.14, 0.19) | 0.14 (ref) | 0.12 (0.10, 0.14) | 0.13 (0.11, 0.16) | 0.13 (0.10, 0.16) | 0.14 (0.11, 0.18) |
| HF (competing riskb) | 0.14 (0.12, 0.16) | 0.13 (ref) | 0.11 (0.09, 0.12) | 0.12 (0.10, 0.15) | 0.12 (0.09, 0.16) | 0.12 (0.09, 0.15) |
| Death | 0.29 (0.27, 0.32) | 0.24 (ref) | 0.23 (0.21, 0.26) | 0.26 (0.23, 0.29) | 0.23 (0.19, 0.27) | 0.31 (0.27, 0.36) |
| Women | ||||||
| HF (primary results)a | 0.12 (0.10, 0.14) | 0.10 (ref) | 0.09 (0.07, 0.10) | 0.09 (0.07, 0.13) | 0.12 (0.07, 0.20) | 0.07 (0.03, 0.19) |
| HF (competing riskb) | 0.11 (0.10, 0.13) | 0.10 (ref) | 0.08 (0.07, 0.10) | 0.08 (0.06, 0.11) | 0.11 (0.06, 0.17) | 0.06 (0.02, 0.15) |
| Death | 0.17 (0.16, 0.19) | 0.15 (ref) | 0.16 (0.14, 0.17) | 0.17 (0.14, 0.20) | 0.19 (0.13, 0.26) | 0.26 (0.17, 0.38) |
aCensoring patient follow-up at time of death.
bAccounting for the competing risk of non-HF death.
Discussion
In this prospective study of 14 629 adults aged 45–64, we observed that participants who consumed up to 7 drinks/week of alcohol had a lower risk of incident HF compared with abstainers, with a less pronounced association in women than in men. No level of alcohol intake was associated with increased risk for HF, but heavy alcohol intake, which was low in this cohort, increased the risk of all-cause mortality among men and women. Participants classified as former drinkers at baseline had higher risk of incident HF and all-cause mortality compared with abstainers.
It has been suggested that moderate alcohol consumption reduces overall mortality,24,25 mainly by reducing the risk reduction of cardiovascular outcomes, particularly those related to CAD.25–28 However, the epidemiological data on the relationship between moderate drinking and the risk of HF are limited,3 as well as the understanding of underlying physiologic mechanisms and sex-related differences.10 In this study, we demonstrated that alcohol consumption of up to 7 drinks/week at early-middle age was inversely associated with the risk for incident HF, independently of demographic factors, socioeconomic indicators, smoking status, BMI, serum total cholesterol plus diabetes and hypertension. Thus, alcohol-induced effects on blood pressure parameters and diabetes should not account substantially for our results. The benefits of moderate drinking on HF might be mediated by preventing CAD and myocardial infarction,3 but our results show that alcohol consumption of up to 7 drinks/week is associated with lower risk of incident HF independently of CAD and incident myocardial infarction. These findings are consistent with the previously published data from the Framingham Heart Study2 and The Cardiovascular Health Study,6 indicating that a reduction in the risk of CAD does not entirely explain the protective association between moderate alcohol consumption and the risk of incident HF. The physiological mechanisms are complex and are not fully understood, but previous studies have demonstrated beneficial effects of alcohol on HDL cholesterol,29 on insulin sensitivity,30 and endothelial function,31 besides others have described a positive association between alcohol consumption and atrial natriuretic peptide, which might prevent clinical onset of HF.32
Sex-related differences on the effects of moderate alcohol consumption on the risk of HF are not well established. However, women seem to be more sensitive than men to the toxic effects of alcohol on cardiac function.15,16,33 In this study, we found a marginally ‘protective’ association between baseline low alcohol consumption and incident HF among women. Similarly, in The Framingham Heart Study, the risk of HF was significantly lower at all levels of alcohol consumption among men, compared with non-drinkers. However, in women, after adjusting for multiple confounders, the relationship was no longer significant.2 Likewise, in The Nurses' Health Study, light-to-moderate alcohol consumption was associated with lower mortality in women, but this apparent benefit seemed largely confined to women at greater risk for CAD.34 Interestingly, we found a protective association among women reporting a cumulative average intake of up to 7 drinks/week, which might be potentially explained by the role of a stable drinking pattern or by a different biological effect of alcohol in older middle aged women. In fact, there are a number of different mechanisms by which the effects of alcohol on the heart may differ by sex. Women have a higher proportion of body fat and absorb and metabolize alcohol differently than men,35 attaining higher blood alcohol concentrations for a given amount of alcohol consumed.35 In addition, women might be susceptible to alcohol-mediated ventricular dysfunction at relatively lower levels of alcohol intake; mitigating the potentially protective effects of alcohol with respect to HF.
In contrast, excessive alcohol consumption is known as a known cause of cardiomyopathy.36 In our sample, 11.3% of men consumed >14 drinks/week and 6.5% of women consumed >7 drinks/week, levels of alcohol intake, considered as heavy drinking by the National Institute of Alcohol Abuse and Alcoholism.37 However, we observed no increased risk for incident HF compared with abstainers. It is plausible that alcohol-mediated cardiomyopathy occurs at prolonged and higher levels of alcohol intake and it may require coincident genetic predisposition. Nevertheless, it is worth noting that heaviest drinkers (men drinking ≥ 21 drinks/week; women ≥ 14 drinks/week) had an increased risk of all-cause mortality, possibly explained by cirrhosis, cancer, and violence.24,38 Besides, in this population, we did not find that moderate alcohol consumption was associated with lower all-cause mortality. However, the analysis of the association of alcohol with specific causes of death was not a scope of this study.
Additionally, contrasting findings on cardiovascular effects of alcohol in white and black men have been formerly reported.14 Fuchs et al. described an increased risk of hypertension among black men consuming low to moderate amounts of alcohol, as well as a positive association between alcohol consumption and incident CAD for black men, along with an inverse association for white.12 Nevertheless, in the same cohort, HDL cholesterol, known as a potential pathway of alcohol benefit on CAD, increased with alcohol consumption, regardless of race.29 In this study, we did not find significant differences between white and black men and women in the risk of HF by alcohol consumption. However, once men and women were stratified by race, the number of cases was relatively small in each category of alcohol intake, limiting our ability to detect small differences by race.
A number of limitations of this analysis should be noted. This is an observational study and alcohol consumption was self-reported in a questionnaire administered by an interviewer, thus participants may have underreported their consumption level. However, this is unlikely because we observed a positive association between alcohol intake and HDL levels, a biological marker of alcohol consumption,29 supporting the rank-order validity of self-reported alcohol intake. In addition, young adults are not represented, as our population only includes participants older than 44 years old, and we were unable to assess the role of binge drinking on the risk of incident HF and all-cause mortality. We excluded participants with HF at baseline, but alcoholic cardiomyopathy may occur at a relatively young age, thus heaviest drinkers may have developed HF before initiating this study. In this cohort, most participants drank more than one kind of drink, precluding additional interpretation on the association between alcohol intake and HF by type of drink. Moreover, there was a low prevalence of heavy drinking, particularly in women limiting the power to estimate the potential hazards in the heaviest drinking category. In addition, this is an observational study; thus, even with the greatest efforts of statistical adjustment to avoid confounding, potential confounding by unmeasured factors can contribute to biased estimates, and the associations observed between alcohol consumption and incident HF and all-cause mortality may not reflect cause and effect.
The strengths of this study include its large size, the long time of follow-up, the ability to analyse sex-specific differences and to control for cardiovascular risk factors, demographic factors, education level, as a rough indicator of socioeconomic status, and incident myocardial infarction as time-varying covariate, determining the association between alcohol consumption and incident HF without interceding myocardial infarction. Moreover, we used baseline and alcohol consumption over time, showing the effects of alcohol intake in early-middle age and from long-term exposure. In addition, we had the capability to classify independently former drinkers and abstainers, minimizing the potential bias due to drinking cessation because of illness, and we demonstrated the risk of incident HF by alcohol consumption while accounting for the competing risk of non-HF mortality.
In summary, in this community-based sample, mild alcohol consumption was associated with lower risk of incident HF, with a similar but less definite association in women than in men. Higher amounts of alcohol intake were not associated with the risk of HF, but heavy alcohol intake increased the risk of all-cause mortality among men and women from this cohort. These findings suggest that despite the dangers of heavy drinking, mild alcohol consumption in early-middle age may be associated with lower the risk of HF.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). The authors thank the staff and participants of the ARIC study for their important contributions. This work was also supported NHLBI cooperative agreement NHLBI-HC-11-08 (S.D.S.), grants R00-HL-107642 (S.C.) and K08-HL-116792 (A.M.S.), and a grant from the Ellison Foundation (S.C.). This work was supported by the Portuguese Foundation for Science and Technology Grant HMSP-ICS/007/2012.
Conflict of interest: none declared.
References
- 1.Mathews EC, Jr, Gardin JM, Henry WL, Del Negro AA, Fletcher RD, Snow JA, Epstein SE. Echocardiographic abnormalities in chronic alcoholics with and without overt congestive heart failure. Am J Cardiol 1981;47:570–578. [DOI] [PubMed] [Google Scholar]
- 2.Walsh CR, Larson MG, Evans JC, Djousse L, Ellison RC, Vasan RS, Levy D. Alcohol consumption and risk for congestive heart failure in the Framingham Heart Study. Ann Intern Med 2002;136:181–191. [DOI] [PubMed] [Google Scholar]
- 3.Djousse L, Gaziano JM. Alcohol consumption and risk of heart failure in the Physicians’ Health Study I. Circulation 2007;115:34–39. [DOI] [PubMed] [Google Scholar]
- 4.Mukamal KJ, Muller JE, Maclure M, Sherwood JB, Mittleman MA. Lack of effect of recent alcohol consumption on the course of acute myocardial infarction. Am Heart J 1999;138:926–933. [DOI] [PubMed] [Google Scholar]
- 5.Aguilar D, Skali H, Moye LA, Lewis EF, Gaziano JM, Rutherford JD, Hartley LH, Randall OS, Geltman EM, Lamas GA, Rouleau JL, Pfeffer MA, Solomon SD. Alcohol consumption and prognosis in patients with left ventricular systolic dysfunction after a myocardial infarction. J Am Coll Cardiol 2004;43:2015–2021. [DOI] [PubMed] [Google Scholar]
- 6.Bryson CL, Mukamal KJ, Mittleman MA, Fried LP, Hirsch CH, Kitzman DW, Siscovick DS. The association of alcohol consumption and incident heart failure: the Cardiovascular Health Study. J Am Coll Cardiol 2006;48:305–311. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Sola J, Fatjo F, Sacanella E, Estruch R, Bosch X, Urbano-Marquez A, Nicolas JM. Evidence of apoptosis in alcoholic cardiomyopathy. Hum Pathol 2006;37:1100–1110. [DOI] [PubMed] [Google Scholar]
- 8.Cheng CP, Cheng HJ, Cunningham C, Shihabi ZK, Sane DC, Wannenburg T, Little WC. Angiotensin II type 1 receptor blockade prevents alcoholic cardiomyopathy. Circulation 2006;114:226–236. [DOI] [PubMed] [Google Scholar]
- 9.Alexander CS. Cobalt-beer cardiomyopathy. A clinical and pathologic study of twenty-eight cases. Am J Med 1972;53:395–417. [DOI] [PubMed] [Google Scholar]
- 10.Rimm EB, Giovannucci EL, Willett WC, Colditz GA, Ascherio A, Rosner B, Stampfer MJ. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 1991;338:464–468. [DOI] [PubMed] [Google Scholar]
- 11.Gianoulakis C, Guillaume P, Thavundayil J, Gutkowska J. Increased plasma atrial natriuretic peptide after ingestion of low doses of ethanol in humans. Alcohol Clin Exp Res 1997;21:162–170. [PubMed] [Google Scholar]
- 12.Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G. Alcohol consumption and the incidence of hypertension: the Atherosclerosis Risk in Communities Study. Hypertension 2001;37:1242–1250. [DOI] [PubMed] [Google Scholar]
- 13.Jackson R, Stewart A, Beaglehole R, Scragg R. Alcohol consumption and blood pressure. Am J Epidemiol 1985;122:1037–1044. [DOI] [PubMed] [Google Scholar]
- 14.Fuchs FD, Chambless LE, Folsom AR, Eigenbrodt ML, Duncan BB, Gilbert A, Szklo M. Association between alcoholic beverage consumption and incidence of coronary heart disease in whites and blacks: the Atherosclerosis Risk in Communities Study. Am J Epidemiol 2004;160:466–474. [DOI] [PubMed] [Google Scholar]
- 15.Fernandez-Sola J, Estruch R, Nicolas JM, Pare JC, Sacanella E, Antunez E, Urbano-Marquez A. Comparison of alcoholic cardiomyopathy in women versus men. Am J Cardiol 1997;80:481–485. [DOI] [PubMed] [Google Scholar]
- 16.Ikehara S, Iso H, Toyoshima H, Date C, Yamamoto A, Kikuchi S, Kondo T, Watanabe Y, Koizumi A, Wada Y, Inaba Y, Tamakoshi A, Japan Collaborative Cohort Study G. Alcohol consumption and mortality from stroke and coronary heart disease among Japanese men and women: the Japan collaborative cohort study. Stroke 2008;39:2936–2942. [DOI] [PubMed] [Google Scholar]
- 17.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol 1989;129:687–702. [PubMed] [Google Scholar]
- 18.Wilhelmsen L, Eriksson H, Svardsudd K, Caidahl K. Improving the detection and diagnosis of congestive heart failure. Eur Heart J 1989;10(Suppl. C):13–18. [DOI] [PubMed] [Google Scholar]
- 19.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study). Am J Cardiol 2008;101:1016–1022. [DOI] [PubMed] [Google Scholar]
- 20.Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, Deswal A, Heiss G, Chambless LE. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail 2012;5:152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Folsom AR, Yamagishi K, Hozawa A, Chambless LE, Atherosclerosis Risk in Communities Study I. Absolute and attributable risks of heart failure incidence in relation to optimal risk factors. Circ Heart Fail 2009;2:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 1982;36:936–942. [DOI] [PubMed] [Google Scholar]
- 23.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509. [Google Scholar]
- 24.Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW, Jr., Doll R. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med 1997;337:1705–1714. [DOI] [PubMed] [Google Scholar]
- 25.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 2006;166:2437–2445. [DOI] [PubMed] [Google Scholar]
- 26.Jackson R, Scragg R, Beaglehole R. Alcohol consumption and risk of coronary heart disease. BMJ 1991;303:211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chiuve SE, Rimm EB, Mukamal KJ, Rexrode KM, Stampfer MJ, Manson JE, Albert CM. Light-to-moderate alcohol consumption and risk of sudden cardiac death in women. Heart Rhythm 2010;7:1374–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abramson JL, Williams SA, Krumholz HM, Vaccarino V. Moderate alcohol consumption and risk of heart failure among older persons. JAMA 2001;285:1971–1977. [DOI] [PubMed] [Google Scholar]
- 29.Volcik KA, Ballantyne CM, Fuchs FD, Sharrett AR, Boerwinkle E. Relationship of alcohol consumption and type of alcoholic beverage consumed with plasma lipid levels: differences between Whites and African Americans of the ARIC study. Ann Epidemiol 2008;18:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenfield JR, Samaras K, Hayward CS, Chisholm DJ, Campbell LV. Beneficial postprandial effect of a small amount of alcohol on diabetes and cardiovascular risk factors: modification by insulin resistance. J Clin Endocrinol Metab 2005;90:661–672. [DOI] [PubMed] [Google Scholar]
- 31.Shai I, Rimm EB, Schulze MB, Rifai N, Stampfer MJ, Hu FB. Moderate alcohol intake and markers of inflammation and endothelial dysfunction among diabetic men. Diabetologia 2004;47:1760–1767. [DOI] [PubMed] [Google Scholar]
- 32.Djousse L, Hunt SC, Eckfeldt JH, Arnett DK, Province MA, Ellison RC. Alcohol consumption and plasma atrial natriuretic peptide (from the HyperGEN study). Am J Cardiol 2006;98:628–632. [DOI] [PubMed] [Google Scholar]
- 33.Urbano-Marquez A, Estruch R, Fernandez-Sola J, Nicolas JM, Pare JC, Rubin E. The greater risk of alcoholic cardiomyopathy and myopathy in women compared with men. JAMA 1995;274:149–154. [DOI] [PubMed] [Google Scholar]
- 34.Fuchs CS, Stampfer MJ, Colditz GA, Giovannucci EL, Manson JE, Kawachi I, Hunter DJ, Hankinson SE, Hennekens CH, Rosner B. Alcohol consumption and mortality among women. N Engl J Med 1995;332:1245–1250. [DOI] [PubMed] [Google Scholar]
- 35.Frezza M, di Padova C, Pozzato G, Terpin M, Baraona E, Lieber CS. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med 1990;322:95–99. [DOI] [PubMed] [Google Scholar]
- 36.Djousse L, Gaziano JM. Alcohol consumption and heart failure: a systematic review. Curr Atheroscler Rep 2008;10:117–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alcoholism NIAA. Overview of Alcohol Consumption.
- 38.Gaziano JM, Gaziano TA, Glynn RJ, Sesso HD, Ajani UA, Stampfer MJ, Manson JE, Hennekens CH, Buring JE. Light-to-moderate alcohol consumption and mortality in the Physicians’ Health Study enrollment cohort. J Am Coll Cardiol 2000;35:96–105. [DOI] [PubMed] [Google Scholar]


