Abstract
We present a low-birth weight newborn who presented with bilious vomit and had a “double bubble” sign on plain abdominal X-ray. Intraoperatively, we found annular pancreas with malrotation and type I choledochal cyst. To the best of our knowledge, this is the first reported case with a combination of these anomalies.
KEY WORDS: Annular pancreas, malrotation, type I choledochal cyst
INTRODUCTION
Bilious vomit in neonates is almost always pathological and malrotation of the gut is one of the often encountered entities on exploration of such a case. The incidence of malrotation has been estimated to be 1 in 6000 live births. An increased incidence of 0.2% has been found in barium swallow studies,[1] whereas autopsy studies estimate that the true incidence may be as high as 1% of the total population.[2] Various associations are known along with malrotation. We report a very rare case of annular pancreas with malrotation associated with choledochal cyst. To the best of our knowledge, this is the first case in which such a combination of anomalies is reported.
CASE REPORT
A full-term male neonate weighing 1900 g was born by lower segment caesarian section (LSCS) to a 24-year-old mother. The child was second in the birth order. Antenatal ultrasound performed in the third trimester showed polyhydramnios and single gastric bubble. The child became symptomatic with bilious vomit from Day 2 of life and was transferred to our center. On admission, the child was found to be lethargic and icteric. Laboratory parameters were normal except total bilirubin, which was 12 mg%. His abdomen was distended, especially the epigastric region, with visible peristalsis from left to right. Abdominal X-ray erect revealed the classical “double bubble” sign [Figure 1]. Ultrasonography of the abdomen and color Doppler showed reversed relationship of superior mesenteric artery/superior mesenteric vein (SMA/SMV), distended stomach and duodenum, spleen centrally located and suspicion of an space occupying lesion (SOL) in the liver. The child was stabilized for one day and then he underwent laparotomy. Intraoperatively, we found a distended stomach, annular pancreas, type I Alonso–Lej choledochal cyst, evidence of incomplete rotation with DJ flexure on the right of the spine, loose lax floating appendix and ileocecum [Figure 2]. The child underwent Kimura's duodenoduodenostomy + cholecystectomy and excision of choledochal cyst + Roux-en-Y hepaticojejunostomy + Ladds procedure. The operative time was 150 min, with blood loss of 15 mL. Oral feeds were gradually started on the 9th post-operative day and the child was weaned off parenteral nutrition by the 14th post-operative day. Fourteen months after the operation, the child is thriving well with normal liver function tests and normal ultrasound of the hepatobiliary system.
Figure 1.

Double bubble sign on plain abdominal film
Figure 2.
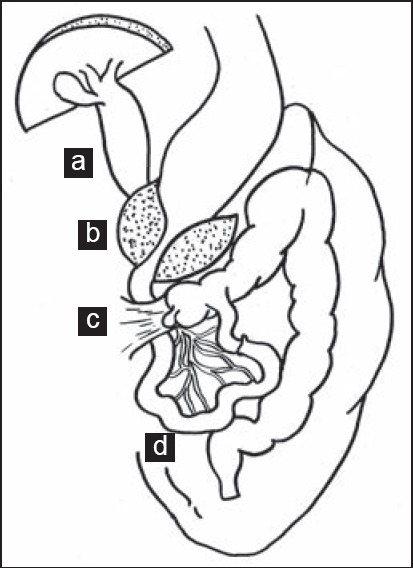
Operative findings: (a)Type I choledochal cyst (b) annular pancreas (c) Ladds bands and (d) malrotated small bowel
DISCUSSION
Associated anomalies are generally the norm in neonates with surgical abnormalities. Malrotation of the gut has been associated with a number of anomalies like intestinal atresias, imperforate anus, cardiac anomalies, duodenal web and Meckels diverticulum.[3] The literature search revealed reports of malrotation with annular pancreas,[4] malrotation with choledochal cyst[5] and choledochal cyst with annular pancreas.[6] However, a combination of malrotation with annular pancreas and choledochal cyst is yet unreported to our knowledge. The abdomen being a “Pandoras box,” the surgeon about to operate on a newborn should be aware of the various possible coexisting pathologies, look for them and surgically address them to avoid post-operative complications and undue embarrassment of a missed diagnosis. Definitive surgical single stage procedure of multiples anomalies in neonates can be safely performed in pediatric surgical centers with adequate pediatric anesthesia and neonatal intensive care facilities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kantor JL. Anomalies of the colon: Their roentgen diagnosis and clinical significance: Resume of 10 years study. Radiology. 1934;23:651–62. [Google Scholar]
- 2.Spigland N, Brandt ML, Yazbeck S. Malrotation presenting beyond the neonatal period. J Pediatr Surg. 1990;25:1139–42. doi: 10.1016/0022-3468(90)90749-y. [DOI] [PubMed] [Google Scholar]
- 3.Warner BW. Malrotation. In: Oldham KT, Colombani PM, Foglia RP, editors. Surgery of Infantsand Children: Scientific Principles and Practice. Philadelphia: Lippincott-Raven; 1997. pp. 1229–40. [Google Scholar]
- 4.Miranda J, Rocha G, Soares P, Morgado H, Baptista MJ, Azevedo I, et al. A novel mutation in FOXF 1 gene associated with alveolar capillary dysplasia with misalignment of pulmonary veins, intestinalmalrotationandannular pancreas. Neonatology. 2013;103:241–5. doi: 10.1159/000346062. [DOI] [PubMed] [Google Scholar]
- 5.Arbell D, Orkin B, Naveh Y, Gur I, Udassin R. Duodenojejunal atresia with absent dorsal mesentery, choledochal cystandmalrotationin a premature newborn — a case report. J Pediatr Surg. 2006;41:e11–3. doi: 10.1016/j.jpedsurg.2006.02.032. [DOI] [PubMed] [Google Scholar]
- 6.Iwai A, Hamada Y, Takada K, Inagaki N, Nakatake R, Yanai H, et al. Choledochal cyst associated with duodenal atresia: Case report and review of the literature. Pediatr Surg Int. 2009;25:995–8. doi: 10.1007/s00383-009-2462-3. [DOI] [PubMed] [Google Scholar]


