Abstract
Aims and Objectives:
The aim was to study the prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility.
Materials and Methods:
A total of 95 infertile women were investigated for thyroid stimulating hormone (TSH). Infertile women with clinical/subclinical hypothyroidism were given thyroxine ranges from 25 to 150 μg.
Results:
Of 95 infertile women, 53.7% were hypothyroid (TSH > 4.6 μIU/ml). After the treatment with thyroxine, 33.3% of subclinical hypothyroid women conceived within 6 weeks to 2-year period. The mean time to conception was 14.56 ± 4.83 months.
Conclusion:
Thyroid profile should be done in infertility work up. Women with normal TSH levels who are positive for thyroid antibodies should also be treated with levothyroxine.
Keywords: Hypothyroidism, infertile women, response
INTRODUCTION
Infertility is a world health issue affecting approximately 8–10% of couple's worldwide.[1] WHO estimates the overall prevalence of primary infertility in India to be 3.5–16.8%.[2] Thyroid dysfunction is more common (4–5 times) in females than in males. Both hyperthyroidism and hypothyroidism have profound effects on estrogen and androgen metabolism, menstrual function and fertility.[3] They may cause delayed onset of puberty, menstrual abnormalities, anovulatory cycles, miscarriages and infertility.[4,5] If thyroid disease is left untreated, it can be a cause for sub-fertility as well as infertility. Thyroid evaluation should be done in any woman who wants to conceive with family history of thyroid problem or irregular menstrual cycle or had more than two abortions or unable to conceive after 1-year of unprotected intercourse.
Prevalence of hypothyroidism in the reproductive age group ranges from 2% to 4%.[6] Hypothyroidism can be easily detected by assessing serum thyroid stimulating hormone (TSH) levels. A slight increase in TSH levels with normal T3 and T4 indicates subclinical hypothyroidism whereas high TSH levels accompanied by low T3 and T4 levels indicate clinical hypothyroidism. Elevated thyrotropin-releasing hormone levels due to hypothyroidism are often associated with increased prolactin (PRL) levels and a delayed LH response to GnRH.[7] It has been recommended that even in the presence of raised PRL levels, the treatment should be first given to treat hypothyroidism before evaluating other causes of raised PRL levels.
Due to the lack of population-based study on infertile women with subclinical/clinical hypothyroidism in our state, we planned to study the prevalence of hypothyroidism in infertile women as well as to assess their response to drug treatment for hypothyroidism.
MATERIALS AND METHODS
The study was carried out in the Department of Obstetrics and Gynecology in collaboration with Rajiv Gandhi Centre for Diabetes and Endocrinology, Jawaharlal Nehru Medical College and Hospital, A.M.U, Aligarh from March 2013 to August 2014. The subjects were selected from the patients coming to endocrinology outpatient department (OPD) and gynecology OPD. After informed consent, thyroid profile (serum TSH, T3, T4) of all subjects was done at their first visit. As per National Health and Nutrition Examination Survey III[8] 2002, the subjects were divided into three groups.
Group 1 (euthyroid): Infertile women with normal TSH level (0.39–4.6 mIU/ml).
Group 2 (subclinical hypothyroidism): Infertile women with raised TSH level ranging from 4.6–20 mIU/ml and normal free T4 level.
Group 3 (overt hypothyroidism): Infertile women with TSH level > 20 mIU/ml and low free T4 level.
As per WHO guidelines, PRL level > 25 μg/l is considered as hyperprolactinemia.[9]
Methods
Samples were taken for evaluation of serum TSH, T3, T4. These were measured using chemiluminescence assay. The machine used for chemiluminescence was immulite 1000 (this is a test unit that contains an assay specific coated bead which serves as the reaction vessel for sample processing).
RESULTS
Of the 98 infertile women enrolled for the study, 3 were excluded due to microprolactinoma and endometriosis. Of the remaining 95 women, 51 (53.7%) were hypothyroid while 44 (46.3%) were euthyroid. Of 51 hypothyroid women, 48 (50.5%) had subclinical hypothyroidism and 3 (3.2%) had overt hypothyroidism. Among 48 subclinical hypothyroid infertile women, 16 (33.3%) were conceived after treatment with thyroxine. Of 16 women, 1 (6.3%) conceived within 6 months of therapy, 4 (25%) conceived after 6 months to 1-year of therapy and rest 11 (68.7%) conceived after 1–2 years of therapy. The mean time to conception was 14.56 ± 4.83 months.
None of the overtly hypothyroid women conceived after treatment with levothyroxine. In Group 1b, 50% women conceived after levothyroxine treatment. Of these two women, one had an abortion, and another continued her pregnancy. The mean TSH of pregnant women was 7.27 ± 2.81, and that of nonpregnant women was 11.16 ± 7.32 mIU/L. The difference between these two was found to be statistically significant (P < 0.05).
DISCUSSION
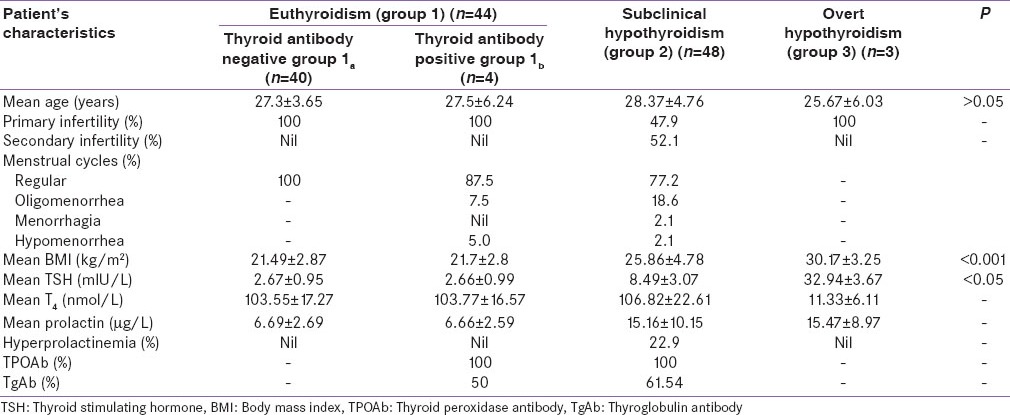
Prevalence of subclinical hypothyroidism (50.5%) was more common than overt hypothyroidism (3.2%) in this study, and the results were consistent with Verma et al.,[10] Biradar et al.[11] and Rijal et al. (2011).[12] There was no significant difference in age among different groups according to thyroid status (P > 0.05). The difference in the body mass index in infertile women with hypothyroidism was highly significant when compared to infertile women with normal thyroid levels (P < 0.001). The result was similar to that of Rahman et al.[13] Most of the study population belonged to primary infertility. Most of the women of all groups had regular cycles [Table 1]. The mean time to conception (14 months approximately) was higher when compared to Raber et al.[7] Higher TSH levels were associated with lower conception rate which was similar to that of Raber et al.[7] and Gerhard et al.[14] The percentage of abortion in hypothyroid infertile women who conceived with the help of levothyroxine was 31.3%, and 80% of those aborted women were positive for thyroid antibodies. Increased number of abortion was noted in this study when compared to Raber et al.[7] and Rahman et al.[13] The association between thyroid antibodies and abortions could not be made out in this study due to small sample size.
Table 1.
Baseline clinical and demographic characteristics of the study population (n=95) has been shown in the following tabulation
The percentage of conception in euthyroid women who were positive for antithyroid antibodies was 50% (2/4) after levothyroxine treatment. Of these, 50% had miscarriage and rest 50% continued with their pregnancy. The result of the present study was not consistent with Negro et al.[15] who reported that the pregnancy rate was not affected either by the presence of antithyroid antibodies or treatment with levothyroxine.
CONCLUSION
Hypothyroidism is an important emerging cause of female infertility and thus, the decision to initiate treatment with levothyroxine in subclinical hypothyroidism at an early stage is justifiable in infertile women. Our data also suggests that women with normal TSH levels who are positive for thyroid antibodies should be treated with levothyroxine. Women who want to conceive should be screened for serum TSH, T3, T4 and thyroid antibodies particularly thyroid peroxidase antibody and thyroglobulin antibodies in their infertility work up. Further studies with larger sample size and long-term follow-up are recommended for better understanding and management of infertility with hypothyroidism.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
REFERENCES
- 1.Inhorn MC. Global infertility and the globalization of new reproductive technologies: Illustrations from Egypt. Soc Sci Med. 2003;56:1837–51. doi: 10.1016/s0277-9536(02)00208-3. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Calverton, Maryland, USA: ORC Marco and World Health Organization; 2004. Infecundity, Infertility and Childlessness in Developing Countries. DHS Comparative Reports No. 9. [Google Scholar]
- 3.Talwar PP. Handbook of Managing Infertility. 1st ed. New Delhi; India: Jaypee Brothers Medical Publishers; 2012. Prevalence of infertility in different population groups in India and its determinants 1986 in establishing an ART in low resource setting-page 55. [Google Scholar]
- 4.Unisa S. Childlessness in Andhra Pradesh, India. Reprod Health Matters. 1999;7:54–64. [Google Scholar]
- 5.Zargar AH, Wani AI, Masoodi SR, Laway BA, Salahuddin M. Epidemiologic and etiologic aspects of primary infertility in the Kashmir region of India. Fertil Steril. 1997;68:637–43. doi: 10.1016/s0015-0282(97)00269-0. [DOI] [PubMed] [Google Scholar]
- 6.Lincoln SR, Ke RW, Kutteh WH. Screening for hypothyroidism in infertile women. J Reprod Med. 1999;44:455–7. [PubMed] [Google Scholar]
- 7.Raber W, Nowotny P, Vytiska-Binstorfer E, Vierhapper H. Thyroxine treatment modified in infertile women according to thyroxine-releasing hormone testing: 5 year follow-up of 283 women referred after exclusion of absolute causes of infertility. Hum Reprod. 2003;18:707–14. doi: 10.1093/humrep/deg142. [DOI] [PubMed] [Google Scholar]
- 8.Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18:988–1028. doi: 10.4158/EP12280.GL. [DOI] [PubMed] [Google Scholar]
- 9.Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:273–88. doi: 10.1210/jc.2010-1692. [DOI] [PubMed] [Google Scholar]
- 10.Verma I, Sood R, Juneja S, Kaur S. Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. Int J Appl Basic Med Res. 2012;2:17–9. doi: 10.4103/2229-516X.96795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biradar SM, Poornima RT, Sonagra AD, Murthy DS. Thyroid dysfunction in infertile women. Int J Pharma Bio Sci. 2012;2:53–8. [Google Scholar]
- 12.Rijal B, Shrestha R, Jha B. Association of thyroid dysfunction among infertile women visiting infertility center of Om Hospital, Kathmandu, Nepal. Nepal Med Coll J. 2011;13:247–9. [PubMed] [Google Scholar]
- 13.Rahman D, Fatima P, Banu J. Thyroid disorders in female subfertility. J Chittagong Med Coll Teach Assoc. 2008;19:46–50. [Google Scholar]
- 14.Gerhard I, Becker T, Eggert-Kruse W, Klinga K, Runnebaum B. Thyroid and ovarian function in infertile women. Hum Reprod. 1991;6:338–45. doi: 10.1093/oxfordjournals.humrep.a137335. [DOI] [PubMed] [Google Scholar]
- 15.Negro R, Mangieri T, Coppola L, Presicce G, Casavola EC, Gismondi R, et al. Levothyroxine treatment in thyroid peroxidase antibody-positive women undergoing assisted reproduction technologies: A prospective study. Hum Reprod. 2005;20:1529–33. doi: 10.1093/humrep/deh843. [DOI] [PubMed] [Google Scholar]


