Abstract
Context:
Popliteal synovial cysts, also known as Baker’s cysts, are commonly found in association with intra-articular knee disorders, such as osteoarthritis and meniscus tears. Histologically, the cyst walls resemble synovial tissue with fibrosis evident, and there may be chronic nonspecific inflammation present. Osteocartilaginous loose bodies may also be found within the cyst, even if they are not seen in the knee joint. Baker’s cysts can be a source of posterior knee pain that persists despite surgical treatment of the intra-articular lesion, and they are routinely discovered on magnetic resonance imaging scans of the symptomatic knee. Symptoms related to a popliteal cyst origin are infrequent and may be related to size.
Evidence Acquisition:
A PubMed search was conducted with keywords related to the history, diagnosis, and treatment of Baker’s cysts—namely, Baker’s cyst, popliteal cyst, diagnosis, treatment, formation of popliteal cyst, surgical indications, and complications. Bibliographies from these references were also reviewed to identify related and pertinent literature.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
Baker’s cysts are commonly found associated with intra-articular knee disorders. Proper diagnosis, examination, and treatment are paramount in alleviating the pain and discomfort associated with Baker’s cysts.
Conclusion:
A capsular opening to the semimembranosus–medial head gastrocnemius bursa is a commonly found normal anatomic variant. It is thought that this can lead to the formation of a popliteal cyst in the presence of chronic knee effusions as a result of intra-articular pathology. Management of symptomatic popliteal cysts is conservative. The intra-articular pathology should be first addressed by arthroscopy. If surgical excision later becomes necessary, a limited posteromedial approach is often employed. Other treatments, such as arthroscopic debridement and closure of the valvular mechanism, are not well studied and cannot yet be recommended.
Keywords: popliteal synovial cysts, Baker’s cysts, intra-articular knee disorders
Popliteal synovial cysts, also known as Baker’s cysts, are commonly found in association with intra-articular knee disorders, such as osteoarthritis and meniscus tears. They can be a source of posterior knee pain that persists despite surgical treatment of the intra-articular lesion.
The eponym “Baker’s cyst” honors British surgeon William Morant Baker’s, who wrote a description of 8 cases of popliteal cysts that he had seen.3 The treatment differed from modern standards and included above-knee amputation in 3 patients, cyst aspiration, or introduction of a seton into the cyst. His conclusions were that the cysts were a result of an effusion from osteoarthritis, they directly communicate with the knee joint, and fluid can flow from the joint into the cyst but not in reverse. Despite the eponym, several other surgeons described popliteal cysts before him. Notably, Robert Adams2 in 1840 described an enlargement of the bursa under the medial head of the gastrocnemius that communicated with the knee by a valvular opening. He concluded that it was the result of arthritis. Foucher,12 in 1856, dissected 11 knees with popliteal cysts, and he concluded that they result from distention of a bursa under the inner head of the gastrocnemius. In 1938, Wilson et al41 dissected 30 knees and found a bursa located between the medial head of the gastrocnemius and semimembranosus in 26 knees. Of those with this bursa, 58% had a direct connection with the knee joint.
Popliteal cysts are commonly encountered in orthopaedic practices that treat knee disorders. They are routinely discovered on up to 38% of magnetic resonance imaging scans (MRIs) performed in the symptomatic knee.32 The formation of the popliteal cyst in adults is frequently found in association with an intra-articular disorder, up to 94%.32 Knee pathologies that have been linked to Baker’s cysts include the presence of meniscus tears,23,32,35 size of effusion,23 osteoarthritis,37 chondral lesions,32 inflammatory arthritis, and anterior cruciate ligament tears.32 Of these disorders, meniscus tears are most frequently associated with popliteal cysts.32,35
Pathology
A valvular opening of the posterior capsule, high up on the medial side and deep to the medial head of the gastrocnemius, is present in up to 40% to 54% of healthy adult knees, based on cadaveric studies.26,38 Radiopaque dye has been injected into popliteal cysts, confirming that fluid flow is from the knee joint into the cyst,38 while reverse flow was not possible. It is thought that this 1-way valvular opening allows fluid to pass into the gastrocnemius-semimembranosus bursa.41 As an effusion is often present with intra-articular pathology, it is possible that the Baker’s cyst may provide a protective effect on the knee by decreasing the hydraulic pressure within the knee through the 1-way valve.16 This argument is strengthened by the finding that the volume of the popliteal cysts is associated with the size of the knee effusions.15,23 This valvular opening allows flow during knee flexion, but it is compressed closed during knee extension due to tension in the semimembranosus and the medial head of gastrocnemius.26
Histologically, the cyst walls resemble synovial tissue with fibrosis evident, and there may be chronic nonspecific inflammation present.28 Osteocartilaginous loose bodies may also be found within the cyst, even if they are not seen in the knee joint. The cyst fluid may be thickened by the presence of fibrin.16 Histologic examination of symptomatic and nonsymptomatic cysts did not reveal any difference microscopically in 1 study.28
Although popliteal cysts are most commonly found between the medial head of the gastrocnemius and semimembranosus, they have been reported in other areas. Jensen and Jorgensen17 reported on a lateral presentation of a popliteal cyst, which communicated with the knee joint at the intercondylar fossa and herniated laterally through the iliotibial band. The authors suggested that if a posterolateral cyst is discovered, further evaluation should be performed to rule out a meniscal cyst or soft tissue tumor,3 as lateral presentation of popliteal cysts are unusual.
Popliteal cysts may also be seen with a failed total knee arthroplasty due to osteolysis or polyethylene debris.8,11 The cysts may be multilobulated8 or gigantic.11 Histologically, macrophage phagocytosed polyethylene particles and particle-induced synovitis are seen.11 Popliteal cysts found in knees with a previous arthroplasty may represent loosening of the components or polyethylene wear.
Examination
Patients commonly present with symptoms of meniscal or chondral pathology. Symptoms related to a popliteal cyst origin are infrequent and may be related to size. Symptoms related to the cysts include posterior or posteromedial fullness and achiness, mass, and stiffness.14,19 Bryan et al4 reported on the common symptoms in 38 patients with a Baker’s cyst. The most common symptoms were popliteal swelling (76%) and posterior aching (32%). Patients may also complain of pain that occurs with terminal knee extension. Functionally, they may develop loss of knee flexion from cysts that are so large that they mechanically block flexion.39 Examination will most commonly reveal knee meniscal or chondral pathology. Palpable posteromedial fullness or tenderness may be present if the cyst is large. If palpable, the cyst often will be firm in full knee extension and soft when the knee is flexed. This finding is commonly known as “Foucher sign” and is due to cyst compression between the medial head of the gastrocnemius and semimembranosus as they approximate each other and the joint capsule during knee extension.6 It is useful for differentiating a Baker’s cyst from other popliteal masses, such as popliteal artery aneurysms, ganglia, adventitial cysts, and tumors, for which the palpation of the mass is unaffected by the knee position.6
Patients may exhibit signs or symptoms of thrombophlebitis, such as calf pain or swelling and a positive Homan sign—a finding known as pseudothrombophlebitis syndrome.20 This condition is most commonly seen with large, dissected, or ruptured popliteal cysts.20
The differential diagnosis of a Baker’s cyst includes popliteal artery aneurysm, soft tissue tumors, meniscal cyst, hematoma, thromboemboli, and seroma.
The imaging workup of knees with suspected popliteal cysts can include plain radiographs, arthrography, ultrasound, and MRI. Plain radiographs such as posteroanterior Rosenberg, lateral, and patellofemoral axial views, though not helpful for detecting popliteal cysts,39 should be obtained early in the evaluation, as they are useful for detecting other conditions commonly found in association with popliteal cysts, such as osteoarthritis, inflammatory arthritis, and loose bodies. In addition, loose bodies may be seen in a Baker’s cyst on plain radiographs.39
Before the advent of MRI, direct arthrography was widely used for detecting popliteal cysts.39 This involved intra-articular injection of the knee with either gas or an iodinated contrast medium, followed by mobilization of the joint to force the contrast (or gas) into the cyst. Spot radiographs or fluoroscopy was then used to detect the presence of the contrast (or gas) in the cysts. Disadvantages of arthrography include the use of ionizing radiation and the use of invasive techniques to inject the contrast.
Ultrasound has largely replaced arthrography as the initial assessment for Baker’s cysts. The advantages include its low cost, noninvasive usage, and absence of radiation. The main disadvantage is the fact that it is user dependent. The ability to detect Baker’s cysts is near 100%, but ultrasound lacks the specificity to differentiate from other conditions, such as meniscal cysts or myxoid tumors.40 Another disadvantage is that it does not adequately visualize other conditions in the knee that are often associated with these cysts, such as meniscal tears. The cysts appear anechoic on ultrasound, indicating that they are fluid filled39 (Figure 1). These extend across the posteromedial aspect of the knee between the medial head of the gastrocnemius and semimembranosus. Echogenic areas, representing loose bodies, may occasionally be seen within a popliteal cyst.
Figure 1.
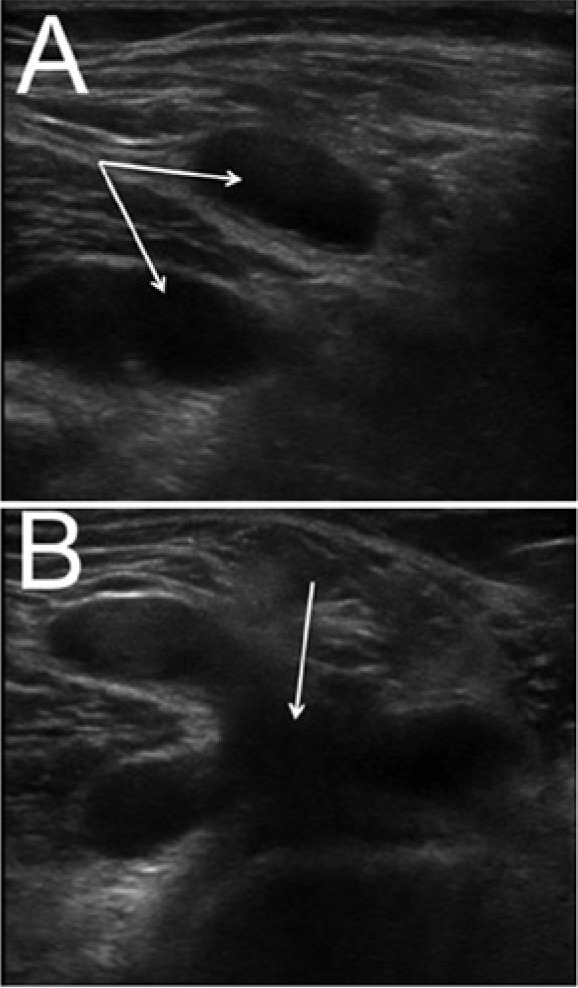
Ultrasound images demonstrating anechoic regions within the popliteal fossa representing a popliteal cyst (arrows). (A) Long axis and (B) short axis of the same multiloculated cyst. Note the medial head gastrocnemius tendon between the loculations on image A.
Magnetic resonance imaging remains the gold standard for diagnosis of Baker’s cysts and differentiating them from other conditions. It allows assessment of the entire spectrum of related disorders, such as meniscal tears, chondral defects, loose bodies, synovitis, osteoarthritis, and ligament tears. Conditions such as meniscal cysts are more easily differentiated from Baker’s cysts with MRI than ultrasound.40 Its main disadvantage is the high cost; therefore, ultrasound should be considered as a screening modality if evaluation of the intra-articular structures is not necessary. The cysts appear as a water-intensity fluid collection (low signal intensity on T1-weighted images and high signal intensity on T2-weighted images) initiating between the medial head gastrocnemius and semimembranosus23 (Figure 2).
Figure 2.
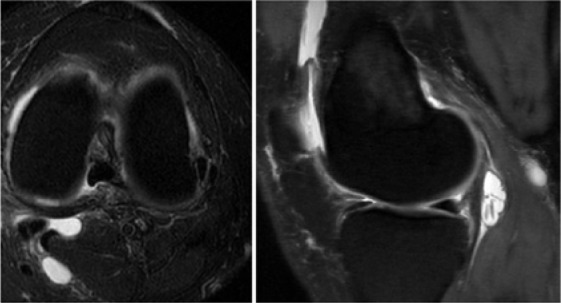
T2-weighted axial and sagittal images of a popliteal cyst. Note the relationship of the medial head gastrocnemius and semitendinosus tendons to the popliteal cyst on the axial image.
Most Baker’s cysts are small and unilocular, but the imaging spectrum is wide. The spectrum includes findings of a septum, multilocularity, size, sites of extension, loose bodies/debris, and rupture. A septum is commonly found in smaller cysts, separating the semimembranosus and gastrocnemius components,32 which are often thin and fragile and may act as a 1-way valve.39 Although most cysts are unilocular, it is not unusual for Baker’s cysts to be multilocular. Though this can cause difficulty in differentiating a Baker’s cyst from other types of popliteal cysts or masses, the key to recognizing them is that the characteristic epicenter is at the location of the medial gastrocnemius-semimembranosus bursa.39 Sometimes these cysts are so large that even identification of the origin of the cyst is difficult to define. Since these cysts are in direct continuity with the intra-articular knee joint, loose bodies such as cartilage, osteochondral bodies, or polyethylene debris can traverse the 1-way valve into the cyst. These bodies will be seen as a heterogenous signal on ultrasound and MRI.
Complications related to the presence of popliteal cysts include infection, rupture, and neurovascular compression. The reports of popliteal cysts by Baker,3 for whom these cysts are named, were associated with infection in most patients. There have been other reports of pyogenic popliteal cysts in association with septic arthritis.8,11 Eichinger et al11 described a rheumatoid patient that had persistent septic knee arthritis despite 2 consecutive knee arthroscopic irrigation and debridements and treatment with appropriate intravenous antibiotics. The patient subsequently underwent open excision of a popliteal cyst through a posteromedial approach. Improvement was noted to be rapid after cyst excision. The authors recommended specialized imaging, such as ultrasound, CT, or MRI, for patients with a septic knee if they have a history of a popliteal cyst, clinical examination findings of a popliteal cyst, or a history of rheumatoid arthritis. In addition, patients that fail to improve after a standard irrigation and debridement for septic arthritis should be imaged to rule out the presence of a popliteal cyst, which could account for a loculated pyogenic infection.
Popliteal cysts can cause compression of local anatomy, resulting in thrombophlebitis, compartment syndrome, and compressive neuropathies. Thrombophlebitis can be difficult to differentiate clinically from a pseudothrombophlebitis that is a result of calf pain from a large cyst.20,34 If there is doubt about the diagnosis or if there is suspicion of deep venous thrombosis (DVT), ultrasonography should be performed.34 Popliteal cyst compression upon the popliteal vein or artery resulting in stenosis or thrombosis has been reported.22,25,36 If vascular compression is present, cyst excision should be performed.
Bleeding following rupture of a popliteal cyst can result in a compartment syndrome.10,33 These patients are often on antithrombotic medications because of an initial suspicion of DVT.10,33 If a ruptured popliteal cyst is thought to be high in the differential diagnosis, further imaging with a venogram or ultrasound should be considered before placement on antithrombotics to potentially avoid this complication. Pain that is out of proportion for a DVT or worsening pain or swelling should heighten the suspicion for compartment syndrome. Pain with passive stretch of the calf muscles (Homan sign) may be positive for both DVT and compartment syndrome; therefore, it may not be useful in differentiating the 2.
Though unusual, compressive neuropathies have also occurred from large popliteal cysts.9,18 Most are reported to involve compression of the tibial nerve, but the peroneal nerve can also be involved.18 The presenting signs are calf atrophy, numbness, and weakness of the muscles innervated by either of these nerves. Open excision is the preferred technique to treat these compressive cysts to prevent further nerve damage.18
Treatment
The initial treatment for symptomatic popliteal cysts should be nonoperative for at least 6 weeks, unless vascular or neural compression is present. During this time, rehabilitation focusing on maintenance of knee flexibility should be emphasized to avoid stiffness that can develop from pain occurring at terminal flexion and extension. Intra-articular corticosteroid injections have been found to decrease the size and symptoms of the cysts,1 and their use can be considered during conservative management. If the pain fails to resolve with this conservative approach, usually under 2 months, then surgical treatment may be considered directed to the intra-articular cause of the joint fluid production and not at the popliteal cyst unless it is unduly large and highly symptomatic.
Surgical excision of the Baker’s cyst without treatment of any intra-articular lesions has been reported; however, the results have been disappointing because of the high rate of recurrence.7,29 The high rate of reoccurrence is believed to be a result of the continued presence of intra-articular pathology and associated recurrent effusions. Rauschning and Lindgren29 reported on 46 excisions performed: 63% recurred and 33% had experienced wound complications or pseudothrombophlebitis afterward. They and other authors proposed surgical treatment of the intra-articular lesion as the mainstay of treatment for popliteal cysts,19,29 as they are nearly always found in association with an intra-articular lesion. The reports of management of symptomatic popliteal cysts by correction of the intra-articular lesions have been limited. Rupp et al30 evaluated the results of arthroscopic treatment for intra-articular disorders with 16 patients with popliteal cysts. Eleven of the cysts persisted, 9 of which remained unchanged and 2 became larger when imaged with ultrasound at 1 year postoperative. Chondral lesions were the most important prognostic factor. All of the patients with persistent cysts had Outerbridge III or IV lesions. The authors are not aware of any studies comparing this method of treatment against other treatment methods.
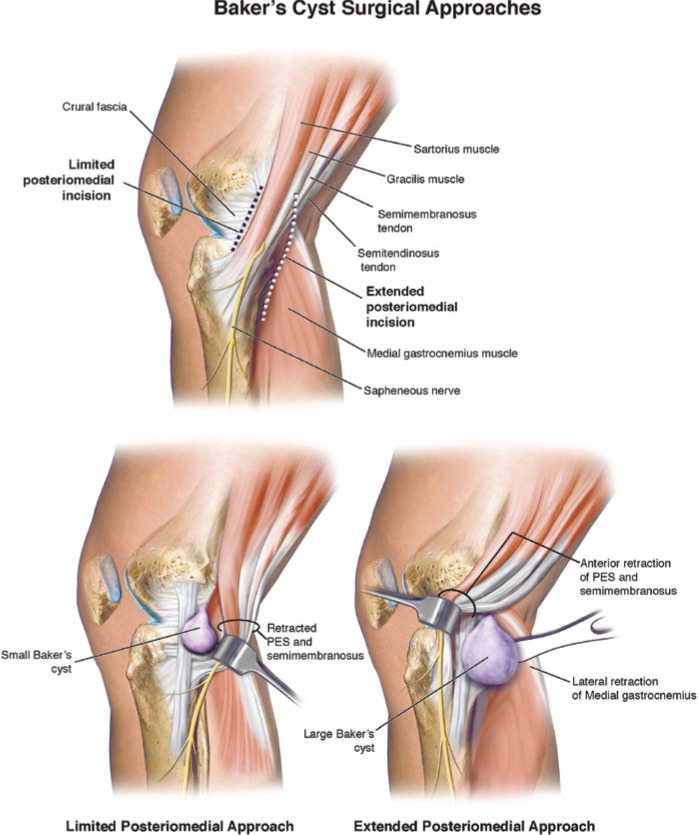
Surgical excision of the medial popliteal cyst, when symptomatic, can be performed through several approaches: limited posteromedial, extended posteromedial, and direct posterior. The direct posterior approach was described by Haggart13 and involves a curvilinear or S-shaped incision over the popliteal fossa at the midflexion crease with the patient in a prone position. The superficial fascia is then incised, and the semimembranosus and medial head of the gastrocnemius are identified. The medial head is retracted to allow exposure of the cyst and communication to the joint.
The limited posteromedial and extended posteromedial approaches were described and advocated for popliteal cyst excision by Rauschning27 and Medvecky and Noyes.24 The patient is placed supine with the foot of the table lowered to allow access to the posteromedial aspect of the knee. The access should be confirmed before draping. A headlight is worn to enhance visualization. For smaller cysts, the limited posteromedial approach may be used (Figure 3). For larger cysts or those that are multiloculated, an extended posteromedial approach is used (Figure 4). The limited posteromedial approach uses the same interval for a medial meniscus inside-out repair. After palpating bony landmarks, a 4- to 5-cm incision is made posterior to the superficial medial collateral ligament. Careful dissection is performed down to the sartorial fascia to avoid injury to the saphenous nerve and vein. An incision is made anterior to the sartorius, and the pes tendons are retracted posteriorly. The interval among the posteromedial joint capsule anteriorly, semimembranosus posteroinferior, and the medial head of the gastrocnemius posterosuperior is now developed. Larger cysts that extend beyond and around the semimembranosus may also be excised with the limited posteromedial approach. The extended posteromedial approach for major popliteal cysts uses the same interval for tibial-inlay posterior cruciate ligament reconstruction. A longitudinal incision beginning 2 cm above the joint and extending distally for 6 to 8 cm is performed along the posterior border of the semimembranosus. The saphenous nerve and its branches should be preserved during superficial dissection. The sartorial fascia is incised along the posterior border, and the pes tendons are retracted anteriorly. The semimembranosus is retracted posteriorly to identify the cyst, although it may occasionally need to be retracted anteriorly to expose multiloculated portions of the cyst. As a surgical point, it is not necessary, in our opinion, to remove all of the cyst, which increases surgical exposure and dissection. The goal is to remove sufficient cyst wall (50% to 75%) to decompress the cyst and diminish recurrence.
Figure 3.
The limited posteromedial approach may be used for excising small popliteal cysts. This interval is bound by the capsule anteriorly, semimembranosus posteroinferior, and medial head of the gastrocnemius posterosuperior. The extended posteromedial approach is used for excising larger and/or multiloculated popliteal cysts. The dissection proceeds along the posterior border of the sartorial fascia; therefore, the saphenous nerve and its branches should be preserved during superficial dissection. After the sartorial fascia is incised, the pes tendons are retracted anteriorly. Semimembranosus is retracted posteriorly to identify the cyst, although it may occasionally need to be retracted anteriorly to expose multiloculated portions of the cyst.
Figure 4.
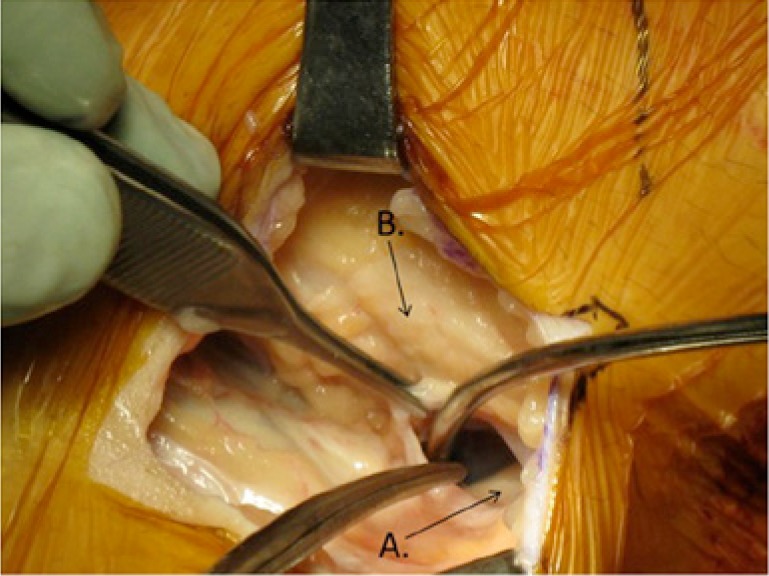
Extended posteromedial approach. The tip of the suction device is within the cavity of the popliteal cyst. The wall of the cyst is being grasped with the forceps while the cyst is being dissected free from surrounding soft tissues. (A) Tendon of medial head of the gastrocnemius. (B) Pes anserine tendon group.
Most authors also advocate closure of the communication to the joint, and Rauschning27 advocated the use of a patch or pedicle graft from the tendon of the medial head of the gastrocnemius to augment the closure (Figure 5). He compared cyst excisions with or without the use of a pedicle graft from the tendon of the medial head of the gastrocnemius. He found that 3 of 7 cysts recurred if a pedicle was not used, and none recurred in the 8 for which a pedicle graft was used.
Figure 5.
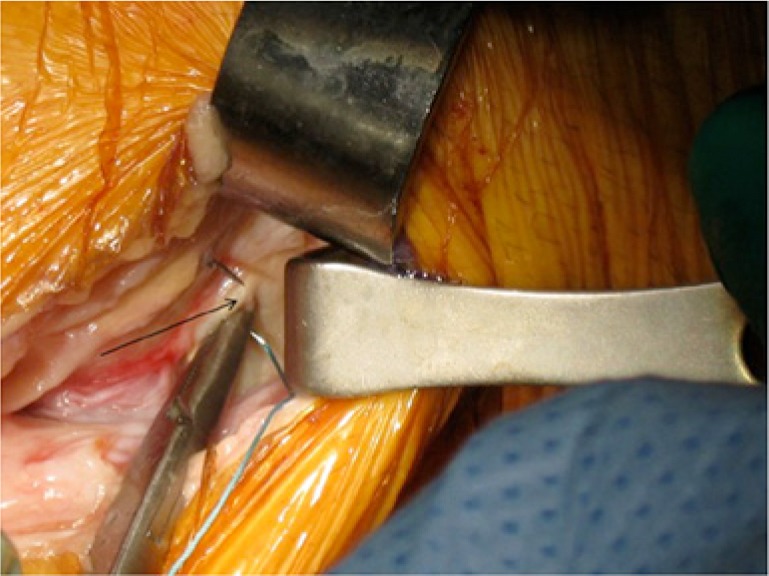
Gastrocnemius tendon used as a patch when sutured over the orifice in the posteromedial capsule after excision of a popliteal cyst. Arrow, tendon.
Arthroscopic debridement and closure of the cyst valvular opening have been reported (Figure 6). Calvisi et al5 described his technique used for 22 patients with symptomatic popliteal cysts. The posteromedial compartment is viewed through the anterolateral portal with a 30° or 70° arthroscope, as necessary for orifices that far proximal or medial. A posteromedial portal is then established outside-in with a needle for localization. After placement of an 8-mm cannula, the valves are debrided with a motorized shaver to create a bleeding surface. Sutures are shuttled through both walls of the orifice with a 45° curved cannulated hook (Linvatec, Largo, Florida) and tied with an all-inside arthroscopic knot technique. After placement of 2 to 4 sutures, depending on the transverse extension, knot stability is tested by extending and flexing the knee several times. The results of this technique were examined with MRI at 2 years postoperative. The cyst had disappeared in 64% of cases, reduced in size in 27%, and persisted in size in 9%. Patients’ clinical improvement was related to the postoperative cyst condition. There were no neurovascular complications reported.
Figure 6.

View of the posteromedial compartment during arthroscopic popliteal cyst valvular debridement and closure. An arthroscopic shaver is used to debride the valvular opening through a posteromedial portal. The valve is closed by placing sutures via an arthroscopic curved cannulated suture shuttle (Linvatec, Largo, Florida) through the capsule and medial head gastrocnemius tendon.
Debridement of the valvular mechanism with concurrent treatment of intra-articular processes (Figure 7) has resulted in good short-term results. Sansone and De Ponti31 reported that 29 of 30 cysts decreased in size or disappeared with their technique, based on 1-year postoperative ultrasounds. They placed a motorized shaver from the anteromedial portal into the cyst valvular mechanism by traversing a defect in the medial meniscus that was discovered after partial meniscectomy. Ko and Ahn21 reported on cystoscopic excision and valvular debridement in 14 patients. All patients had no limitations in range of motion and absence of pain and swelling at 1 year postoperative. This technique used 2 portals within the cyst wall while the patient was in the lateral decubitus position. A subtotal or total cyst wall excision was performed while avoiding injury to the neurovascular bundle. The valvular opening was then debrided through a posteromedial arthroscopic portal. The only reported complication was a calf hematoma.
Figure 7.
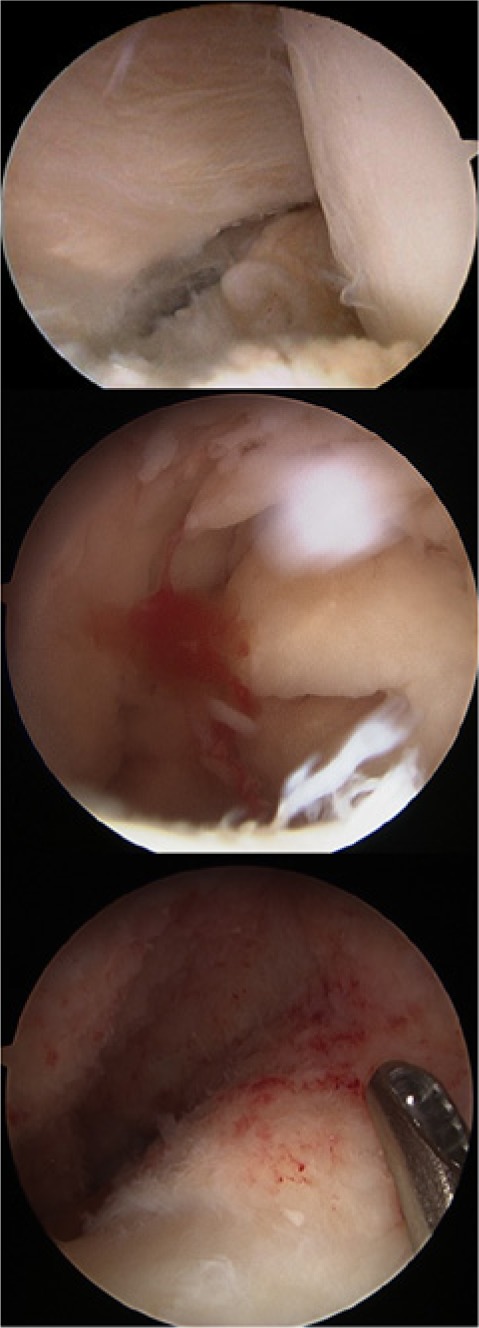
Arthroscopic debridement of popliteal cyst. The top image shows the valve orifice viewed through the notch from an anterolateral portal. The middle image was taken with a 30° arthroscope while visualizing into the cyst from an anterolateral portal through the notch. Note the debris in the cyst. The lower image shows the cyst after debridement with a motorized shaver through a posteromedial accessory portal.
Popliteal cysts are also frequently found in association with osteoarthritis at the time of total knee arthroplasty. The orifice can be identified when the posterior joint is exposed with a lamina spreader for removal of femoral condylar osteophytes. This orifice can then be dilated with the use of a curved curette to promote 2-way flow, followed by electrocautery of the valve mechanism to prevent recurrence of the valve effect. This technique has not been studied but is routinely used during total knee arthroplasty.
Conclusion
A capsular opening to the semimembranosus–medial head gastrocnemius bursa is a commonly found normal anatomic variant. It is thought that this can lead to formation of a popliteal cyst in the presence of chronic knee effusions as a result of intra-articular pathology. Management of symptomatic popliteal cysts is conservative. The intra-articular pathology should be first addressed by arthroscopy. If surgical excision later becomes necessary, a limited posteromedial approach is often employed. Other treatments, such as arthroscopic debridement or closure of the valvular mechanism, are not well studied and cannot yet be recommended.
Footnotes
The following author declared potential conflicts of interest: Frank R. Noyes, MD, receives fellowship support from DJO Global, Inc and Arthrex, Inc.
References
- 1. Acebes JC, Sanchez-Pernaute O, Diaz-Oca A, Herrero-Beaumont G. Ultrasonographic assessment of Baker’s cysts after intra-articular corticosteroid injection in knee osteoarthritis. J Clin Ultrasound. 2006;34:113-117. [DOI] [PubMed] [Google Scholar]
- 2. Adams R. Chronic rheumatic arthritis of the knee joint. Dublin J Med Sci. 1840;17:520-522. [Google Scholar]
- 3. Baker WM. On the formation of synovial cysts in the leg in connection with disease of the knee joint. 1877. Clin Orthop Relat Res. 1994;299:2-10. [PubMed] [Google Scholar]
- 4. Bryan RS, DiMichele JD, Ford GL., Jr. Popliteal cysts. Arthrography as an aid to diagnosis and treatment. Clin Orthop Relat Res. 1967;50:203-208. [PubMed] [Google Scholar]
- 5. Calvisi V, Lupparelli S, Giuliani P. Arthroscopic all-inside suture of symptomatic Baker’s cysts: a technical option for surgical treatment in adults. Knee Surg Sports Traumatol Arthrosc. 2007;15:1452-1460. [DOI] [PubMed] [Google Scholar]
- 6. Canoso JJ, Goldsmith MR, Gerzof SG, Wohlgethan JR. Foucher’s sign of the Baker’s cyst. Ann Rheum Dis. 1987;46:228-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Childress HM. Popliteal cysts associated with undiagnosed posterior lesions of the medial meniscus. The significance of age in diagnosis and treatment. J Bone Joint Surg Am. 1970;52:1487-1492. [PubMed] [Google Scholar]
- 8. Corten K, Vandenneucker H, Reynders P, Nijs S, Pittevils T, Bellemans J. A pyogenic, ruptured Baker’s cyst induced by arthroscopic pressure pump irrigation. Knee Surg Sports Traumatol Arthrosc. 2009;17:266-269. [DOI] [PubMed] [Google Scholar]
- 9. DiRisio D, Lazaro R, Popp AJ. Nerve entrapment and calf atrophy caused by a Baker’s cyst: case report. Neurosurgery. 1994;35:333-334. [DOI] [PubMed] [Google Scholar]
- 10. Dunlop D, Parker PJ, Keating JF. Ruptured Baker’s cyst causing posterior compartment syndrome. Injury. 1997;28:561-562. [DOI] [PubMed] [Google Scholar]
- 11. Eichinger JK, Bluman EM, Sides SD, Arrington ED. Surgical management of septic arthritis of the knee with a coexistent popliteal cyst. Arthroscopy. 2009;25:696-700. [DOI] [PubMed] [Google Scholar]
- 12. Foucher E. Memoire sur les kystes de la region poplitee. Arch Gen Med. 1856;2:313. [Google Scholar]
- 13. Haggart GE. Synovial cysts of the popliteal space: clinical significance and treatment. Ann Surg. 1943;118:438-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Handy JR. Popliteal cysts in adults: a review. Semin Arthritis Rheum. 2001;31:108-118. [DOI] [PubMed] [Google Scholar]
- 15. Hill CL, Gale DG, Chaisson CE, et al. Knee effusions, popliteal cysts, and synovial thickening: association with knee pain in osteoarthritis. J Rheumatol. 2001;28:1330-1337. [PubMed] [Google Scholar]
- 16. Jayson MI, Dixon AS. Valvular mechanisms in juxta-articular cysts. Ann Rheum Dis. 1970;29:415-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jensen KH, Jorgensen U. Lateral presentation of a Baker’s cyst. Clin Orthop Relat Res. 1993;287:202-203. [PubMed] [Google Scholar]
- 18. Ji JH, Shafi M, Kim WY, Park SH, Cheon JO. Compressive neuropathy of the tibial nerve and peroneal nerve by a Baker’s cyst: case report. Knee. 2007;14:249-252. [DOI] [PubMed] [Google Scholar]
- 19. Johnson LL, van Dyk GE, Johnson CA, Bays BM, Gully SM. The popliteal bursa (Baker’s cyst): an arthroscopic perspective and the epidemiology. Arthroscopy. 1997;13:66-72. [DOI] [PubMed] [Google Scholar]
- 20. Katz RS, Zizic TM, Arnold WP. The pseudothrombophlebitis syndrome. Medicine. 1977;56:151. [DOI] [PubMed] [Google Scholar]
- 21. Ko S, Ahn J. Popliteal cystoscopic excisional debridement and removal of capsular fold of valvular mechanism of large recurrent popliteal cyst. Arthroscopy. 2004;20:37-44. [DOI] [PubMed] [Google Scholar]
- 22. Langsfeld M, Matteson B, Johnson W, Wascher D, Goodnough J, Weinstein E. Baker’s cysts mimicking the symptoms of deep venous thrombosis: diagnosis with venous duplex scanning. J Vasc Surg. 1997;25:658-662. [DOI] [PubMed] [Google Scholar]
- 23. Marti-Bonmati L, Molla E, Dosda R, Casillas C, Ferrer P. MR imaging of Baker cysts: prevalence and relation to internal derangements of the knee. MAGMA. 2000;10:205-210. [DOI] [PubMed] [Google Scholar]
- 24. Medvecky MJ, Noyes FR. Surgical approaches to the posteromedial and posterolateral aspects of the knee. J Am Acad Orthop Surg. 2005;13:121-128. [DOI] [PubMed] [Google Scholar]
- 25. Olcott C, Mehigan JT. Popliteal artery stenosis caused by a Baker’s cyst. J Vasc Surg. 1986;4:403-405. [PubMed] [Google Scholar]
- 26. Rauschning W. Anatomy and function of the communication between the knee joint and popliteal bursae. Ann Rheum Dis. 1980;39:354-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rauschning W. Popliteal cysts (Baker’s cyst) in adults: II. Capsuloplasty with and without a pedicle graft. Acta Orthop Scand. 1980;51:547-555. [DOI] [PubMed] [Google Scholar]
- 28. Rauschning W, Fredriksson BA, Wilander E. Histomorphology of idiopathic and symptomatic popliteal cysts. Clin Orthop Relat Res. 1982;164:306-311. [PubMed] [Google Scholar]
- 29. Rauschning W, Lindgren PG. Popliteal cysts (Baker’s cysts) in adults: I. Clinical and roentgenological results of operative excision. Acta Orthop Scand. 1979;50:583-591. [DOI] [PubMed] [Google Scholar]
- 30. Rupp S, Seil R, Jochum P, Kohn D. Popliteal cysts in adults: prevalence, associated intraarticular lesions, and results after arthroscopic treatment. Am J Sports Med. 2002;30:112-115. [DOI] [PubMed] [Google Scholar]
- 31. Sansone V, De Ponti A. Arthroscopic treatment of popliteal cyst and associated intra-articular knee disorders in adults. Arthroscopy. 1999;15:368-372. [DOI] [PubMed] [Google Scholar]
- 32. Sansone V, De Ponti A, Minio Paluello G, Del Maschio A. Popliteal cysts and associated disorders of the knee: critical review with MR imaging. Int Orthop. 1995;19:275-279. [DOI] [PubMed] [Google Scholar]
- 33. Schimizzi AL, Jamali AA, Herbst KD, Pedowitz RA. Acute compartment syndrome due to ruptured Baker cyst after nonsurgical management of an anterior cruciate ligament tear. Am J Sports Med. 2006;34:657-660. [DOI] [PubMed] [Google Scholar]
- 34. Shuckett R, Fam AG. Pseudothrombophlebitis syndrome in pyogenic arthritis. Can Med Assoc J. 1983;128:294-295. [PMC free article] [PubMed] [Google Scholar]
- 35. Stone KR, Stoller D, De Carli A, Day R, Richnak J. The frequency of Baker’s cysts associated with meniscal tears. Am J Sports Med. 1996;24:670-671. [DOI] [PubMed] [Google Scholar]
- 36. Takano Y, Oida K, Kohri Y, et al. Is Baker’s cyst a risk factor for pulmonary embolus? Intern Med. 1996;35:886-889. [DOI] [PubMed] [Google Scholar]
- 37. Tarhan S, Unlu Z. Magnetic resonance imaging and ultrasonographic evaluation of the patients with knee osteoarthritis: a comparative study. Clin Rheumatol. 2003;22:181-188. [DOI] [PubMed] [Google Scholar]
- 38. Taylor AR, Rana NA. A valve: an explanation of the formation of popliteal cysts. Ann Rheum Dis. 1973;32:419-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Torreggiani WC, Al-Ismail K, Munk PL, et al. The imaging spectrum of Baker’s (popliteal) cysts. Clin Radiol. 2002;57:681-691. [DOI] [PubMed] [Google Scholar]
- 40. Ward EE, Jacobson JA, Fessell DP, Hayes CW, van Holsbeeck M. Sonographic detection of Baker’s cysts: comparison with MR Imaging. AJR Am J Roentgenol. 2001;176:373-380. [DOI] [PubMed] [Google Scholar]
- 41. Wilson PD, Eyre-Brook AL, Francis JD. A clinical and anatomical study of the semimembranosus bursa in relation to popliteal cyst. J Bone Joint Surg Am. 1938;20:963-984. [Google Scholar]