Abstract
Context:
Dance, gymnastics, figure skating, and competitive cheerleading require a high degree of hip range of motion. Athletes who participate in these sports use their hips in a mechanically complex manner.
Evidence Acquisition:
A search of the entire PubMed database (through December 2013) and additional searches of the reference lists of pertinent articles.
Study Design:
Systematic review.
Level of Evidence:
Level 3.
Results:
Whether innate or acquired, dancers and gymnasts have some hypermobility that allows their hips to be placed in potentially impinging or unstable positions required for their given activity. Such extremes of motion can result in both intra-articular and extra-articular impingement as well as compensatory osseous and muscular pathology. In addition, dancers and gymnasts are susceptible to impingement-induced instability. Dancers with innate generalized hyperlaxity are at increased risk of injury because of their activities and may require longer recovery times to return to play. Both nonoperative and operative treatments (arthroscopic and open) have an important role in returning flexibility athletes to their preoperative levels of sport and dance.
Conclusion:
Because of the extreme hip motion required and the compensatory soft tissue laxity in dancers and gymnasts, these athletes may develop instability, impingement, or combinations of both. This frequently occurs in the setting of subtle pathoanatomy or in patients with normal bony anatomy. With appropriate surgical indications and the correct operative technique, the treating surgeon can anticipate high levels of return to play for the gymnast and dancer with hip pain.
Keywords: hip injury, dance, gymnastics, femoroacetabular impingement, instability, impingement
The dancer, gymnast, figure skater, and cheer athletes generally start at a very early age.23,34,55 As they progress to higher levels, they typically train for multiple hours per day during adolescence.23,67,89 Furthermore, females participate in these sports in much greater numbers than males.67,92 After running and walking, dance is the third most common activity reported by adolescent girls,92 with 35% participating in some form of dance. All these sports have high range of motion (ROM) requirements. Dance, in particular, involves combinations of extreme hip flexion, extension, abduction, and external rotation, which may cause increased labral strain or femoroacetabular subluxation.25,95 These sports all emphasize jumping or leaping, with landing strategies involving hip control and hip flexion.31,38,55,68 Finally, tendinopathy and muscular imbalances can also be problematic, independent of bone structure or secondary to compensatory patterns related to underlying bony anatomy. Both male and female dancers have well-studied strength imbalances with stronger hip abductors and weaker adductors31 and, occasionally, side-to-side strength differences.32,34
Search Criteria
An unrestricted search of the PubMed database was conducted using the initial search phrase hip pain in dancers, which yielded 35 articles. Additional searches with various combinations of hip pain, groin pain, hip dysplasia, hip pathology performing arts, hip gymnastics, hip figure skating, athlete hip pain, femoroacetabular impingement, capsular laxity, intra-articular hip pathology, extra-articular hip pathology, hip arthroscopy, and hip athletic injury were used to expand the pertinent data included in this article. A search of each included article’s reference list was also conducted. All English-language abstracts were initially reviewed. Ultimately, 119 articles were included in our study.
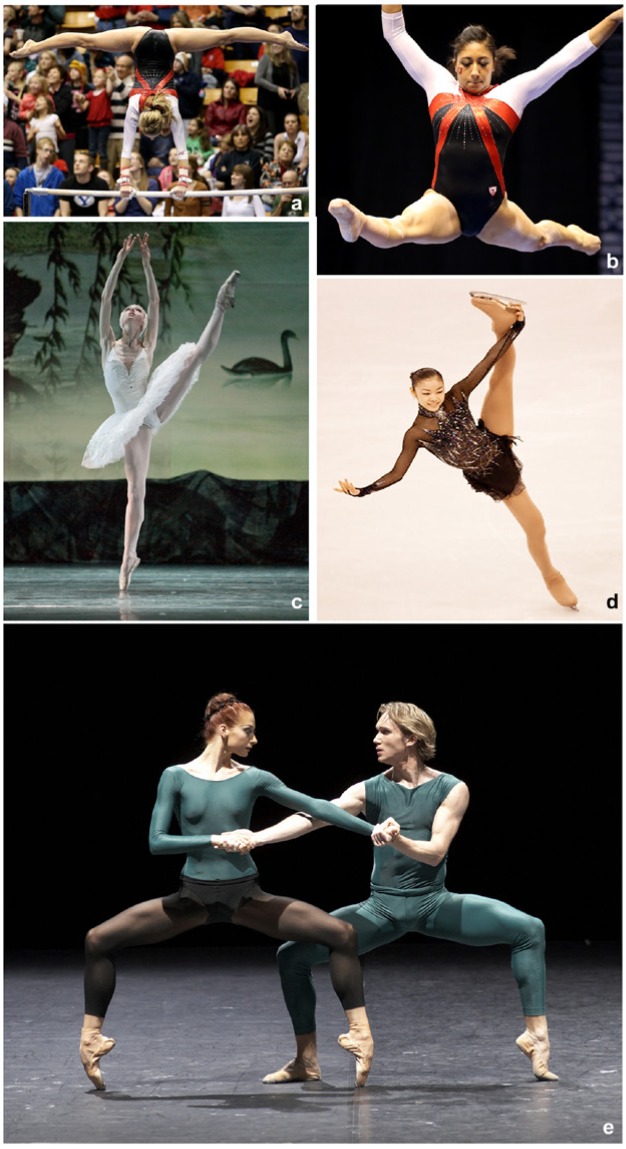
Motion Requirements and Acquired Soft Tissue Laxity
The ROM requirements for these sports causes compensatory soft tissue laxity that develops during training.24,34,45,89 Classical ballet is the most commonly studied in this regard. While the natural pattern over childhood and adolescence is to become less flexible, dancers maintain more ROM than nondancers.89 As a result of training, dancers have increased flexibility throughout the spine, pelvis, and hips and are, as a rule, able to place their palms on the floor and/or knees to their forehead.34,89 When these trained motions are excluded and dancers are evaluated by standard measures of hyperlaxity (eg, elbow hyperextension or genu recurvatum), they tend to be at least as flexible as the general population.34 Ballet also places great emphasis on turnout, which is the lower extremity external rotation achieved with the knees held in extension (Figure 1). The hip is thought to contribute 50% to 70% of this rotation.30,34,42 Not surprisingly, both male and female ballet dancers have increased hip external rotation and decreased hip internal rotation when compared with nondancers.32,34,41,75,89 Female dancers have a slight increase in their overall arc of motion,32,34,41,75,89 whereas male dancers have an average of 10° less total ROM than controls.34,41 The increased hip external rotation likely results from either relative femoral retroversion/less anteversion,90 soft tissue laxity at the anterior hip, or both.33 Dancers also have more hip abduction than do controls,34,89 although this decreases with age89 secondary to the normal ossification and subsequent deepening of the acetabulum.16
Figure 1.
(a) Ballet turnout. Dance places a great deal of emphasis on the turnout, which is the amount of lower extremity external rotation with the knees in extension. The hip is thought to contribute 50% to 70% of the rotation. Reprinted with permission from http://www.shutterstock.com/g/smoxx. (b) Lower extremity external rotation with the knees in extension is common to other flexibility sports as well, as can be seen in this skater. Yuna Kim, 2007 National Sports Festival Winter Games, http://www.flickr.com/photos/queenyuna/5017220486/, used under a Creative Commons Attribution-NonCommercial-NoDerivatives License.
Hormonal influences also play a role in female soft tissue laxity. The prevalence of hyperlaxity increases in females after puberty.73 This is expected since high hormone levels during ovulation of the menstrual cycle and during pregnancy facilitate loosening of the pelvic ligaments.56 Dancers with “joint hypermobility syndrome” or “generalized joint hypermobility” have a Beighton score of ≥4.13,18,39,81 In cohort studies of the dance community, authors have suggested that somewhere between 20% and 66% of the professional dance community is classified as having hypermobility.18,78,81 It may be that the innate or acquired hyperlaxity allows these athletes to achieve professional status; however, cross-sectional studies have also documented that hyperlaxity leads to increased risk of injury and longer rehabilitation periods prior to return to participation.18,34,46,69,81
Dysplasia and Instability
Acetabular dysplasia is much more common in females,22,37,61 and, depending on the degree of dysplasia and acetabular version, can be associated with increased hip ROM.54 As dancers advance, there may be a selection bias for those with increased hip ROM, which may also be a result of underlying dysplasia or soft tissue laxity.89 In general, acetabular coverage and version are predictive of hip internal rotation, with increased acetabular coverage or acetabular retroversion associated with less internal rotation.8,90 The prevalence of hyperlaxity in normal children ranges from 1% to 7%,20,96 whereas the prevalence of laxity is greater in children with congenital hip dislocation and may affect 33% to 75% of this population.20 Dancers with both hyperlaxity and dysplasia have sustained low-energy hip dislocations during dance.26,88 Soft tissue laxity may exacerbate structural instability due to dysplasia.1,57,96 Correspondingly, in a series of professional dancers undergoing hip arthroscopy for labral pathology, 55% had evidence of dysplasia (Hammoud et al, 2011, AAOS Annual Meeting, San Diego, California). In addition to acetabular-sided pathology, excessive femoral anteversion may cause symptomatic hip instability.2,90 In a younger or nonprofessional dancer, excessive anteversion may be more common and become symptomatic because of the additive effect of anterior hip soft tissue laxity in these athletes.15,24 This is uncommon in the high-level or professional dancer because increased hip external rotation requirements do not favor those with excessive femoral anteversion.9,24,33
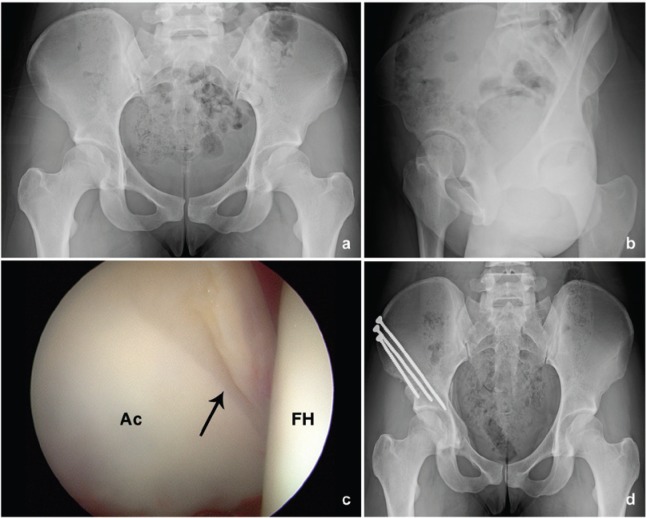
Regardless of the etiology of hip instability in these athletes, the labrum and ligamentum teres tend to have characteristic pathology (Figure 2).43,54,59,77 The labrum is often hypertrophic, with intrasubstance ganglion cyst formation and labral tears.43,54,77 Inflammation, hypertrophy, or tears of the ligamentum teres are considered markers of instability or excessive abduction and internal and external rotation activities59 rather than the cause of instability. In a series of patients undergoing combined arthroscopy and periacetabular osteotomy (PAO), 30% had partial or complete ligamentum tears.77
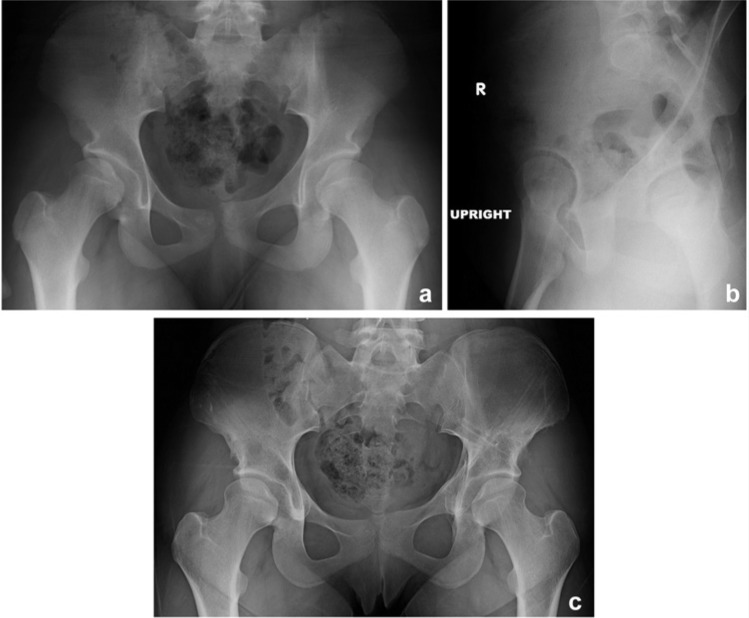
Figure 2.
Preoperative (a) anterior-posterior pelvis and (b) false-profile radiographs from an adolescent dancer with hip pain preventing her from dancing. These show acetabular dysplasia with (a) retroversion and (b) limited anterior coverage. (c) She underwent arthroscopy and periacetabular osteotomy to evaluate the status of her labrum, improve the lateral acetabular coverage, and correct the version. Intraoperatively, the labrum was hypertrophic and degenerative (arrow), which was consistent with her diagnosis of mild dysplasia and instability. (d) The postoperative radiograph shows improved lateral coverage and neutral acetabular version. Ac, acetabulum; FH, femoral head.
Impingement
Large structural anomalies causing femoroacetabular impingement (FAI) may be less common in higher-level female dancers because of the motion limitations caused by severe acetabular overcoverage or cam pathoanatomy. Conversely, dancers who do have FAI may become symptomatic earlier than nondancers do. In a series of professional dancers undergoing hip arthroscopy, 25% had cam pathoanatomy (Hammoud et al, 2011, AAOS Annual Meeting, San Diego, California). In adolescent female dancers treated for FAI, pincer-type FAI was more common than cam-type.85 Cam-type FAI may be more common in male dancers and consistent with male dancers having less internal rotation than nondancers.34 In addition, dancers often have cam deformities that are localized within the acetabulum more posterolaterally or superiorly than the general athletic population. This may be a physeal response to repetitive external rotation and abduction with posterior-superior femoroacetabular contact observed in dancers.21 Eleven- to 14-year-old dancers who train for more than 6 hours a day often have relative femoral retroversion.9,24,33 When relative femoral retroversion is present, it can exacerbate impingement in flexion or internal rotation.8,40
Athletes in these sports with normal osseous hip morphology may develop symptomatic FAI secondary to the repetitive training and compensatory soft tissue laxity (Figure 3). This can produce impingement and impingement-induced subluxation at the posterior-superior aspect of the hip,21,24 which correlates with the location of cartilage thinning and labral pathology often seen on hip magnetic resonance imaging of asymptomatic dancers. Cadaveric studies provide additional evidence, with combinations of hip abduction and external rotation in both flexion and extension causing increased labral strain25 and anterior femoral head subluxation.25,95 A cadaveric study of hips without osseous FAI examined the effects of dancer- or gymnast-like flexibility and found that extremes of hyperextension and external rotation could generate femoroacetabular contact at the posterior-superior acetabulum.83
Figure 3.
Both (a) side splits and (b) front splits are common in flexibility sports and dance. In ballet, these positions are called grand écart facial and grand écart lateral, respectively. These 2 positions as well as the développé à la seconde (c, in ballet; d, in a skater) and the (e) grand plié have been found to cause impingement at the posterior-superior aspect of the acetabulum in morphologically normal hips. Figure (c) reproduced with permission, http://www.shutterstock.com/g/df028. Figure (d) Yuna Kim 2009 World Figure Skating Championships, Los Angeles, California, http://www.flickr.com/photos/queenyuna/6368356397, used under a Creative Commons Attribution-NonCommercial-NoDerivatives License. Figure (e) reproduced with permission, Sergey Petrov, http://www.shutterstock.com/g/irtish.
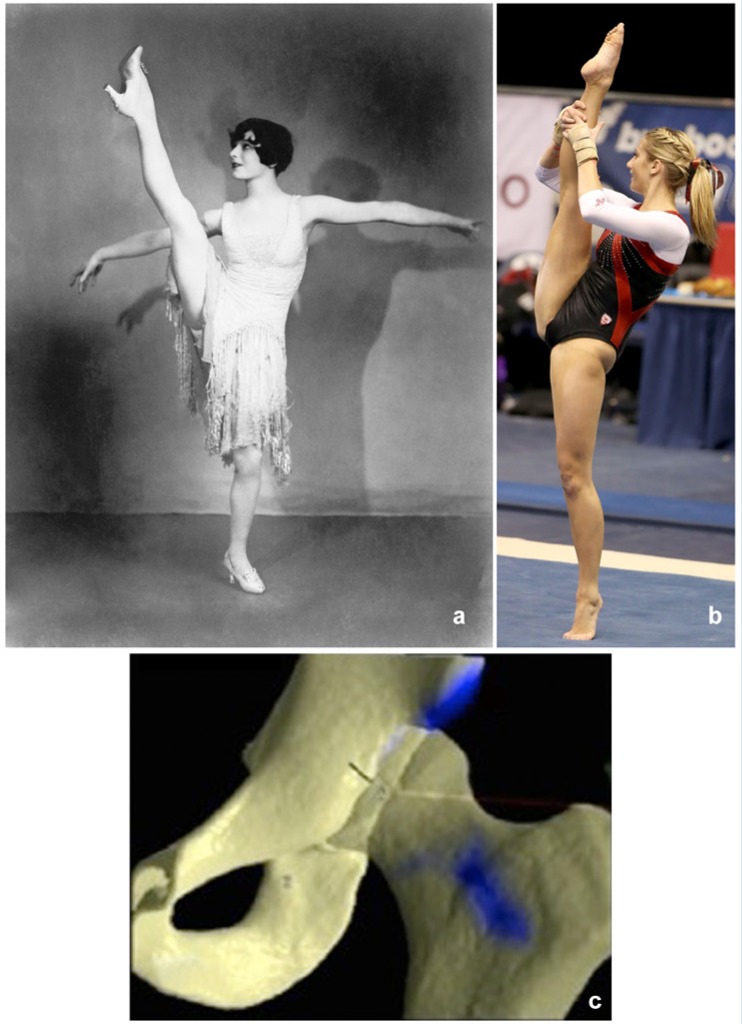
In addition to intra-articular FAI, extra-articular bony impingement can occur in dancing and gymnastic athletes. Extremes of motion with high flexion angles in either neutral rotation or abduction (high-kick dance), similar positions in ballet, and extreme hip flexion in gymnastics can cause impingement between the anterior inferior iliac spine (AIIS) and distal femoral neck (subspinous impingement) (Figures 4 and 5).51 A 3-dimensional computerized simulation of hip motion provided some confirmatory evidence of collisions between the AIIS and the anteromedial femoral neck even in normal hips at high flexion angles.8 Extra-articular FAI or trochanteric-pelvic impingement is a pain generator in the young, active athlete with hip pain, including dancers and gymnasts.8,12,37,51,86 Although not directly studied in the dancer or gymnast, the evaluating clinician should be aware of ischiofemoral impingement.4,5,87,91 This type of extra-articular impingement is caused by abnormal contact between the lesser trochanter and the ischium in positions of hip extension, adduction, and external rotation (ie, turnout). Symptoms of ischiofemoral impingement may be gradual in onset with groin pain and/or buttock pain and may mimic iliopsoas tendonitis or a hamstring strain.86
Figure 4.
In (a) high-kick dance, (b) gymnastics, and some ballet positions, impingement occurs between the anterior-inferior iliac spine (AIIS) and distal femoral neck, as can be seen in this (c) 3-dimensional computer simulation of high-flexion impingement. Figure (a) reprinted with permission, http://www.shutterstock.com. Figure (c) reprinted with permission from Larson et al.58
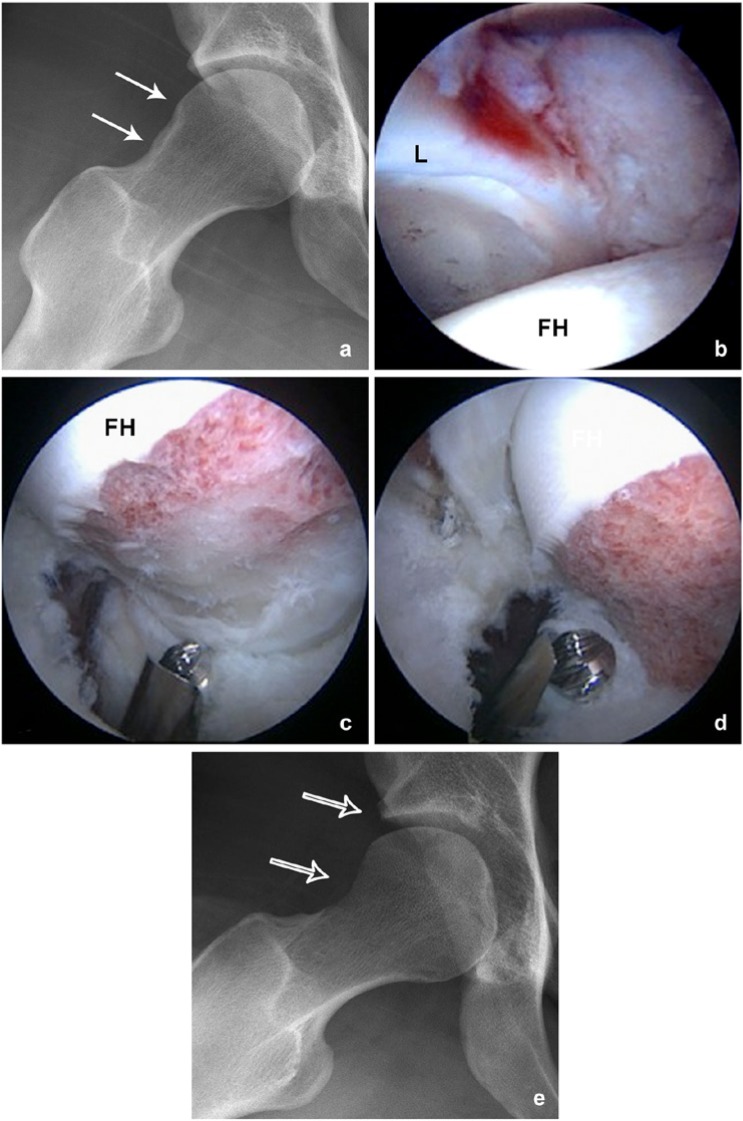
Figure 5.
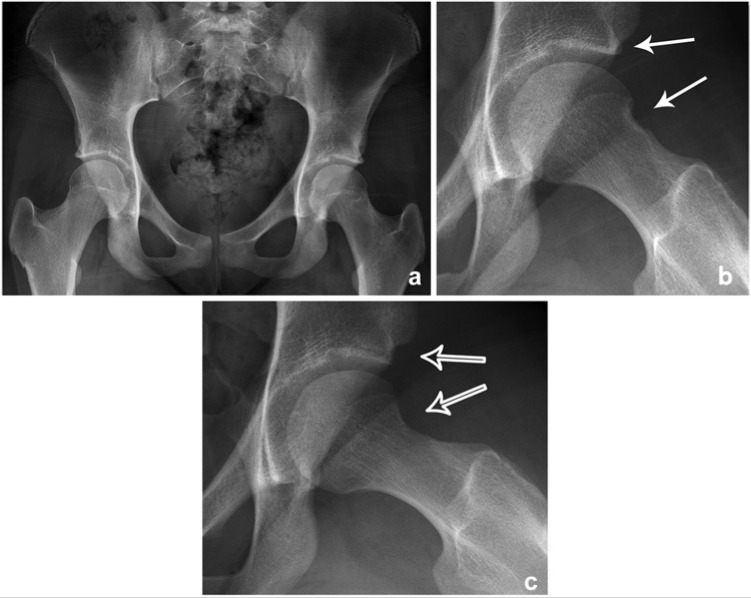
Radiographs and intraoperative images from a 30-year-old former high-level studio dancer with right anterior hip pain and pain with straight flexion typical of impingement between the anterior-inferior iliac spine (AIIS) and distal femoral neck. Hip range of motion was 105° in straight flexion, 15° of internal rotation, and 60° of external rotation in flexion. (a) The preoperative Dunn lateral view shows sclerosis on the distal femoral neck (solid arrows). (b) Intraoperatively, she had focal bruising and synovitis around the AIIS with (c) cortical sclerosis distal on the femoral neck, consistent with high range of motion impingement. (d) She underwent rim osteoplasty around the AIIS and femoral neck osteoplasty extending distally on the neck to eliminate the impingement. (e) The postoperative Dunn lateral radiograph demonstrates the AIIS and femoral neck osteoplasties (open arrows). FH, femoral head; L, labrum.
Combined Instability and Impingement
Combinations of instability and impingement may also be common in athletes who achieve extremes of hip flexibility, such as dancers and gymnasts. The retroverted dysplastic acetabulum with posterior deficiency is increasingly recognized as a source of both instability and impingement.2,29 This type of dysplasia results in anterior impingement but posterior-superior instability.2,29 Posterior-superior instability may be especially problematic for a dancer because the force on an abducted and externally rotated hip is also posterior and superior. These patients have a radiographic “cross-over sign” with deficient posterior-superior coverage and, importantly, also have a posterior wall sign, where the posterior acetabular wall is significantly medial to the center of the femoral head (Figure 6).29 Impingement-induced instability was described initially in contact athletes with an anterior cam deformity that caused the femur to lever posteriorly and, in some cases, dislocate.47,48 In dancers and flexibility athletes, impingement-induced instability results from the femoral neck levering on the lateral acetabular rim (extreme abduction) or the AIIS (extreme flexion), causing anteroinferior and posteroinferior subluxation, respectively (Figure 7). Evidence for this mechanism is found on computed tomography scans of impingement patients where the direction of subluxation was dependent on the location of the cam deformity.95
Figure 6.
This patient has bilateral dysplasia with acetabular retroversion. (a) The sourcils are short, the posterior acetabular walls are both medial to the center of rotation of the femoral head, and the anterior acetabular wall crosses in front of the posterior acetabular wall. (b) The false-profile radiograph of the right hip demonstrates deficient anterior coverage. (c) The patient underwent bilateral periacetabular osteotomy with subsequent hardware removal once the osteotomies had healed. The postoperative radiograph shows improved coverage and correction of acetabular version on both hips.
Figure 7.
Radiographs and intraoperative images from a 15-year-old female ballet and studio dancer with left anterior groin pain provoked by dance. (a) Anterior-posterior pelvis radiograph reveals normal acetabular coverage and version. (b) A Dunn lateral radiograph demonstrates a pincer groove at the anterior femoral neck with otherwise normal head-neck offset and a slightly prominent anterior-inferior iliac spine (AIIS; solid arrows). She underwent acetabular rim osteoplasty under the AIIS and femoral neck osteoplasty to eliminate the impingement and resultant levering between the AIIS and femur. (c) The postoperative Dunn lateral radiograph demonstrates the acetabular and femoral neck osteoplasties (open arrows).
Evaluation of the Flexibility Athlete with Hip or Groin Pain
The examination of the dancer or gymnast with hip or groin pain is no different than any other athlete. The objective of the physical examination is to narrow the differential diagnosis by localizing the pain generators. The physical examination should be performed in the same stepwise fashion each time and should include 5 examination positions: standing, seated, supine, lateral, and prone.58 Specific physical examination findings in dancers and gymnasts may include lateral or posterior symptoms due to abductor fatigue, whereas pain in terminal flexion (which can be common for both dysplasia and FAI) often indicates anterior labral pathology and/or subspine impingement.6,18,79 When the gymnast’s or dancer’s athletic demands on the hip are greater than the functional ROM, compensatory stresses and subsequent pain may develop in the adjacent structures. The sequelae of compensatory injury can occur in the lumbar spine, the pubic symphysis, the sacroiliac joints, and the posterior acetabulum.6,10,18,79 The compensatory stress also places demands on the periarticular musculature, which may also lead to muscle injury of the adductor longus, proximal hamstrings, abductors, iliopsoas, and hip flexors.35,52,63
When is Surgery Indicated and What Should be Done?
The decision for surgery can be difficult in this population because the patient’s expectations for returning to the preinjury level of activity may exceed what can be delivered with surgical management. Nonetheless, there are a few relatively clear indications. Surgery can be considered for patients with identifiable structural pathoanatomy who have continued symptoms with activities of daily living despite a reasonable attempt at nonoperative management or who require pain medication to perform or are unable to perform because of pain. Other clear indications include proximal hamstring avulsions with retraction, tension-sided femoral neck stress fractures, and patients with recurrent low-energy hip dislocations or loose bodies.
For patients with labral tears and intra-articular pathology, the bony morphology on radiographs and computed tomography scans should be used to guide surgical decision making. Arthroscopy cannot correct dysplasia or instability due to excessive femoral anteversion; thus, acetabular reorientation or, less frequently, femoral derotational osteotomy may be necessary to correct the structural pathoanatomy causing labral tears in these patients.17,70 Patients who have cam- or pincer-type FAI can be treated arthroscopically in the majority of cases, and, where indicated, femoral/acetabular osteoplasties can address these deformities. Of note, cam deformities can be subtle in females when compared with males36 but may be more likely to be symptomatic. For patients with suspected impingement between the AIIS and distal femoral neck, a careful neck-reshaping osteoplasty can significantly improve clearance and reduce any levering effect/subluxation (Figures 5 and 7).53
For small amounts of labral fraying, selective arthroscopic labral debridement or suture anchor refixation can be used to stabilize the labrum.44 For larger labral tears, comparative cohorts of labral debridement and refixation patients have shown better outcomes for labral refixation.27,47,50,82 Thus, in these cases, the labrum should be repaired if it is technically possible. Patients who have ligamentum teres inflammation or tearing can have mechanical symptoms; thus, judicious debridement of the ligamentum can help improve these symptoms.19,49,97 Labral reconstruction and ligamentum reconstruction is not well supported by the literature and consists entirely of level 4 case series with small numbers, short-term follow-up, and may or may not have included dancers or other hypermobility athletes.71,72,84,94 Thus, the role of these reconstructions for treatment is currently unclear.
Although dancers and gymnasts frequently have psoas pain and tendinopathy, psoas tenotomy should be avoided. A psoas tenotomy in dancers can lead to hip flexor weakness and further destabilize the anterior hip, resulting in a career-ending situation for these athletes.28,53 The high-kick or dance-line dancer who loses hip flexor strength cannot regain his or her kick, and ballet dancers who undergo psoas tenotomy cannot regain extension—the ability to flex their hip high with the knee extended (à la seconde position). As previously stated, the psoas may also be functioning as a dynamic stabilizer for patients with subtle anterior instability,28 with the extreme example of this being dislocation with the hip in abduction and external rotation after an arthroscopy and psoas tenotomy.80
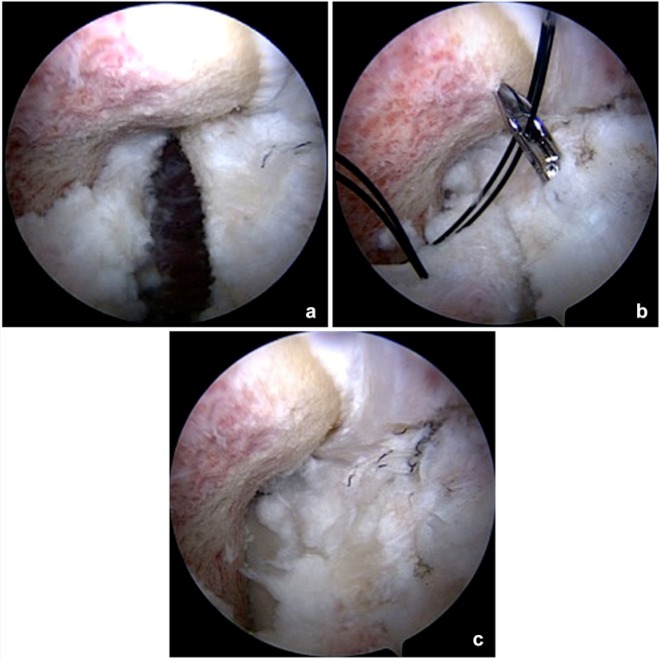
Capsular management during arthroscopy is also important for the flexibility athlete. The iliofemoral ligament is the primary stabilizer for external rotation and anterior translation,62 which are key motions for dance. While subtle capsular laxity or increased microinstability may impair return to sport, there have also been case reports of subluxation and dislocation in the setting of ligamentous laxity, an unrepaired capsule, and/or dysplasia (both mild and iatrogenic).14,60,74,80 Thus, capsular repair with or without plication11 (Figure 8) or avoiding a capsular T-cut altogether is imperative in this population. When repairing the capsule, care should be taken not to overtighten the capsule, as this can result in loss of hip external rotation, which, in dancers, is a critical component of lower extremity turnout.
Figure 8.
Arthroscopic photos of capsular repair. (a) Prior to repair, the interportal capsulotomy (mid-anterior to anterolateral portals) is visible along the femoral neck. The capsule is repaired with a suture passing instrument that allows the edges of the capsule to be (b) opposed or plicated. (c) After the repair, the interportal capsulotomy has been closed.
Patients with acetabular dysplasia and instability should be managed with a PAO, particularly if standing pain is a primary component of their symptoms. Arthroscopy can be considered as an adjunct at the time of the PAO to repair intra-articular labral tears or debride ligamentum tears, particularly if the patient has mechanical symptoms (see Figure 2).77 PAO definitively corrects dysplasia and has a 90% survivorship at 10 years with optimal acetabular positioning and establishment of appropriate head-neck offset.3 There is a growing awareness that patients with dysplasia often have decreased head-neck offset that, after PAO, may result in symptomatic impingement. In the general population, femoral neck osteoplasty may improve the survivorship of the PAO3 and decrease the rates of reoperation for impingement after PAO.64 For the ROM requirements inherent to these sports, dancers and other flexibility athletes may require femoral neck osteoplasty at the time of the PAO to restore the ROM after acetabular correction.3,64 Although there are no published studies, restoration of preoperative ROM is likely to be important for returning to sports or dance after a PAO.
In some cases, patients with FAI should be managed with an open osteoplasty and corrections via surgical hip dislocation.17 This may be indicated for the patient with a cam deformity that is primarily posterior or for the uncommon patient with global acetabular overcoverage secondary to protrusion. Patients who have normal radiographic anatomy but suspected trochanteric-pelvic impingement should also undergo treatment via a surgical hip dislocation because this allows the trochanter to be translated posteriorly or reshaped to eliminate extra-articular impingement. Some surgeons also believe that there may also be a role for the open approach in a very hypermobile patient because the open capsular repair incites a more vigorous healing response and is technically less demanding than that with an arthroscopic approach.53,65,76,98
Return to Sport After Hip Preservation Surgery
Although dancers and other flexibility athletes are frequently referred for therapy, there are no studies on the rate of return to sport after nonoperative management. There is 1 systematic review specifically examining return to sport after surgery for FAI.7 In general, 92% of patients are able to return to sports, with 88% returning to the same level of play as before surgery.7 When professional athletes were considered, 92% returned to sport at the same level as before surgery.7 In a study of isolated arthroscopic labral debridement in dancers, modified Harris hip scores improved from 52.7 to 91.5, and overall pain levels decreased from 7.5 to 2.5 postoperatively.44 Patients required an average of 8 months to return to dance at their preoperative levels. The study was limited in that follow-up ranged from 5 months to 5 years, and only 57% reached their preoperative levels of dance.44 Another study of dancers undergoing hip arthroscopy found that return to professional dance was less likely for older dancers, dancers with dysplasia, and for professional ballerinas (Hammoud et al, 2011, AAOS Annual Meeting, San Diego, California). Considering that treatments may not have addressed the structural pathoanatomy (eg, dysplasia or pincer-type FAI), the rates of return for dancers to high-level or professional dance after hip preservation surgery has the potential to be higher than was observed in this series. Although no studies have been done for flexibility athletes undergoing PAO, general activity level increases after PAO, particularly in younger patients or patients who were more active preoperatively.66,93 In a recent series of PAO patients, all patients who participated in gymnastics, yoga, or dance prior to surgery were able to return to these same sports, although their level of participation was unknown.66
Summary and Conclusion
Dancers, gymnasts, and flexibility athletes with hip pain are a challenging population because of the extreme ROM requirements for their sports and compensatory soft tissue laxity. As a result, they are able to place their hips in impinging positions even in the setting of normal osseous anatomy and often have combinations of impingement and instability. These hips are complex, and decision making is challenging; however, if these athletes are appropriately evaluated and treated, return to play at a high frequency can be expected.
Footnotes
The following authors declared potential conflicts of interest: Asheesh Bedi, MD, is a paid consultant for A3 Surgical and Smith & Nephew; Christopher M. Larson, MD, is a paid consultant for A3 Surgical and Smith & Nephew, and holds stock/stock options from A3 Surgical.
References
- 1. Adib N, Davies K, Grahame R, Woo P, Murray KJ. Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology (Oxford). 2005;44:744-750. [DOI] [PubMed] [Google Scholar]
- 2. Akiyama M, Nakashima Y, Fujii M, et al. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol. 2012;41:1411-1418. [DOI] [PubMed] [Google Scholar]
- 3. Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ali AM, Teh J, Whitwell D, Ostlere S. Ischiofemoral impingement: a retrospective analysis of cases in a specialist orthopaedic centre over a four-year period. Hip Int. 2013;23:263-268. [DOI] [PubMed] [Google Scholar]
- 5. Ali AM, Whitwell D, Ostlere SJ. Case report: imaging and surgical treatment of a snapping hip due to ischiofemoral impingement. Skeletal Radiol. 2011;40:653-656. [DOI] [PubMed] [Google Scholar]
- 6. Allen N, Nevill A, Brooks J, Koutedakis Y, Wyon M. Ballet injuries: injury incidence and severity over 1 year. J Orthop Sports Phys Ther. 2012;42:781-790. [DOI] [PubMed] [Google Scholar]
- 7. Alradwan H, Phillippon MJ, Farrokhyar F, et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy. 2012;28:1567-1576. [DOI] [PubMed] [Google Scholar]
- 8. Audenaert EA, Peeters I, Vigneron L, Baelde N, Pattyn C. Hip morphological characteristics and range of internal rotation in femoroacetabular impingement. Am J Sports Med. 2012;40:1329-1336. [DOI] [PubMed] [Google Scholar]
- 9. Bauman PA, Singson R, Hamilton WB. Femoral neck anteversion in ballerinas. Clin Orthop Relat Res. 1994;(302):57-63. [PubMed] [Google Scholar]
- 10. Bedi A, Dolan M, Leunig M, Kelly BT. Static and dynamic mechanical causes of hip pain. Arthroscopy. 2011;27:235-251. [DOI] [PubMed] [Google Scholar]
- 11. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011;27:1720-1731. [DOI] [PubMed] [Google Scholar]
- 12. Bedi A, Kelly BT, Khanduja V. Arthroscopic hip preservation surgery: current concepts and perspective. Bone Joint J. 2013;95-B:10-19. [DOI] [PubMed] [Google Scholar]
- 13. Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32:413-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Benali Y, Katthagen BD. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405-407. [DOI] [PubMed] [Google Scholar]
- 15. Bennell KL, Khan KM, Matthews BL, Singleton C. Changes in hip and ankle range of motion and hip muscle strength in 8-11 year old novice female ballet dancers and controls: a 12 month follow up study. Br J Sports Med. 2001;35:54-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Birkenmaier C, Jorysz G, Jansson V, Heimkes B. Normal development of the hip: a geometrical analysis based on planimetric radiography. J Pediatr Orthop B. 2010;12:1-8. [DOI] [PubMed] [Google Scholar]
- 17. Bogunovic L, Gottlieb M, Pashos G, Baca G, Clohisy JC. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res. 2013;471:2523-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Briggs J, McCormack M, Hakim AJ, Grahame R. Injury and joint hypermobility syndrome in ballet dancers—a 5-year follow-up. Rheumatology. 2009;48:1613-1614. [DOI] [PubMed] [Google Scholar]
- 19. Byrd JW, Jones KS. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2004;20:385-391. [DOI] [PubMed] [Google Scholar]
- 20. Carter C, Wilkinson J. Persistent joint laxity and congenital dislocation of the hip. J Bone Joint Surg Br. 1964;46-B:40-45. [PubMed] [Google Scholar]
- 21. Charbonnier C, Kolo FC, Duthon VB, et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39:557-566. [DOI] [PubMed] [Google Scholar]
- 22. Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy. A systematic literature review. Clin Orthop Relat Res. 2009;467:2041-2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dubravcic-Simunjak S, Pecina M, Kuipers H, Moran J, Haspl M. The incidence of injuries in elite junior figure skaters. Am J Sports Med. 2003;31:511-517. [DOI] [PubMed] [Google Scholar]
- 24. Duthon VB, Charbonnier C, Kolo FC, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29:411-419. [DOI] [PubMed] [Google Scholar]
- 25. Dy CJ, Thompson MT, Crawford MJ, Alexander JW, McCarthy JC, Noble PC. Tensile strain in the anterior part of the acetabular labrum during provocative maneuvering of the normal hip. J Bone Joint Surg Am. 2008;90:1464-1472. [DOI] [PubMed] [Google Scholar]
- 26. Epstein DM, Rose DJ, Philippon MJ. Arthroscopic management of recurrent low-energy anterior hip dislocation in a dancer: a case report and review of literature. Am J Sports Med. 2010;38:1250-1254. [DOI] [PubMed] [Google Scholar]
- 27. Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925-935. [DOI] [PubMed] [Google Scholar]
- 28. Fabricant PD, Bedi A, dela Torre K, Kelly BT. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy. 2012;28:965-971. [DOI] [PubMed] [Google Scholar]
- 29. Fujii M, Nakashima Y, Yamamoto T, et al. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895-903. [DOI] [PubMed] [Google Scholar]
- 30. Gilbert CB, Gross MT, Klug KB. Relationship between hip external rotation and turnout angle for the five classical ballet positions. J Orthop Sports Phys Ther. 1998;27:339-347. [DOI] [PubMed] [Google Scholar]
- 31. Gittoes MJR, Irwin G, Kerwin D. Kinematic landing strategy transference in backward rotating gymnastics dismounts. J Appl Biomech. 2013;29:253-260. [DOI] [PubMed] [Google Scholar]
- 32. Gupta A, Fernihough B, Bailey G, Bombeck P, Clarke A, Hopper D. An evaluation of differences in hip external rotation strength and range of motion between female dancers and non-dancers. Br J Sports Med. 2004;38:778-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hamilton D, Aronsen P, Løken JH, et al. Dance training intensity at 11-14 years is associated with femoral torsion in classical ballet dancers. Br J Sports Med. 2006;40:299-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hamilton WG, Hamilton LH, Marshall P, Molnar M. A profile of the musculoskeletal characteristics of elite professional ballet dancers. Am J Sports Med. 1992;20:267-273. [DOI] [PubMed] [Google Scholar]
- 35. Hammoud S, Bedi A, Magennis E, Meyers WC, Kelly BT. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy. 2012;28:1388-1395. [DOI] [PubMed] [Google Scholar]
- 36. Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy. 2013;29:54-63. [DOI] [PubMed] [Google Scholar]
- 37. Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644-1653. [DOI] [PubMed] [Google Scholar]
- 38. Jaworski CA, Ballantine-Talmadge S. On thin ice: Preparing and caring for the ice skater during competition. Curr Sports Med Rep. 2008;7:133-137. [DOI] [PubMed] [Google Scholar]
- 39. Juul-Kristensen B, Røgind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford). 2007;46:1835-1841. [DOI] [PubMed] [Google Scholar]
- 40. Kelly BT, Bedi A, Robertson CM, Dela Torre K, Giveans MR, Larson CM. Alterations in internal rotation and alpha angles are associated with arthroscopic cam decompression in the hip. Am J Sports Med. 2012;40:1107-1112. [DOI] [PubMed] [Google Scholar]
- 41. Khan K, Roberts P, Nattrass C, et al. Hip and ankle range of motion in elite classical ballet dancers and controls. Clin J Sports Med. 1997;7:174-179. [DOI] [PubMed] [Google Scholar]
- 42. Khoo-Summers LC, Prather H, Hunt DM, Van Dillen LR. Predictors of first position turnout in collegiate dancers. Am J Phys Med Rehabil. 2013;92:136-142. [DOI] [PubMed] [Google Scholar]
- 43. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-429. [DOI] [PubMed] [Google Scholar]
- 44. Kocher MS, Solomon R, Lee BM, Micheli LJ, Solomon J, Stubbs A. Arthroscopic debridement of hip labral tears in dancers. J Dance Med Sci. 2006;10:99-105. [Google Scholar]
- 45. Kolo FC, Charbonnier C, Pfirrmann CW, et al. Extreme hip motion in professional ballet dancers: dynamic and morphologic evaluation based on magnetic resonance imaging. Skeletal Radiol. 2013;42:689-698. [DOI] [PubMed] [Google Scholar]
- 46. Konopinski MD, Jones GJ, Johnson MI. The effect of hypermobility on the incidence of injuries in elite-level professional soccer players: a cohort study. Am J Sports Med. 2012;40:763-769. [DOI] [PubMed] [Google Scholar]
- 47. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29:46-53. [DOI] [PubMed] [Google Scholar]
- 48. Krych AJ, Thompson M, Larson CM, Byrd JW, Kelly BT. Is posterior hip instability associated with cam and pincer deformity? Clin Orthop Relat Res. 2012;470:3390-3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kusma M, Jung J, Dienst M, Goedde S, Kohn D, Seil R. Arthroscopic treatment of an avulsion fracture of the ligamentum teres of the hip in an 18-year-old horse rider. Arthroscopy. 2004;20(suppl 1):64-66. [DOI] [PubMed] [Google Scholar]
- 50. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015-1021. [DOI] [PubMed] [Google Scholar]
- 51. Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011;27:1732-1737. [DOI] [PubMed] [Google Scholar]
- 52. Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27:768-775. [DOI] [PubMed] [Google Scholar]
- 53. Larson CM, Stone RM. Current concepts and trends for operative treatment of FAI: hip arthroscopy. Curr Rev Musculoskelet Med. 2013;6:242-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;(418):74-80. [DOI] [PubMed] [Google Scholar]
- 55. Lockwood KL, Gervais PJ, McCreary DR. Landing for success: a biomechanical and perceptual analysis of on-ice jumps in figure skating. Sports Biomech. 2006;5:231-241. [DOI] [PubMed] [Google Scholar]
- 56. MacLennan AH. Relaxin—a review. Aust N Z J Obstet Gynaecol. 1981;21:195-202. [DOI] [PubMed] [Google Scholar]
- 57. Mangat G, Dieppe P. Hypermobility, arthritis and congenital hip dislocation. Br J Rheumatol. 1990;29:77. [DOI] [PubMed] [Google Scholar]
- 58. Martin HD, Kelly BT, Leunig M, et al. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26:161-172. [DOI] [PubMed] [Google Scholar]
- 59. Martin RL, Kivlan BR, Clemente FR. A cadaveric model for ligamentum teres function: a pilot study. Knee Surg Sports Traumatol Arthrosc. 2013;21:1689-1693. [DOI] [PubMed] [Google Scholar]
- 60. Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400-404. [DOI] [PubMed] [Google Scholar]
- 61. Mladenov K, Dora C, Wicart P, Seringe R. Natural history of hips with borderline acetabular index and acetabular dysplasia in infants. J Pediatr Orthop. 2002;22:607-612. [PubMed] [Google Scholar]
- 62. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability. Am J Sports Med. 2011;39(suppl 1):85S-91S. [DOI] [PubMed] [Google Scholar]
- 63. Nassif NA, Pekmezci M, Pashos G, Schoenecker PL, Clohisy JC. Osseous remodeling after femoral head-neck junction osteochondroplasty. Clin Orthop Relat Res. 2010;468:511-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Nassif NA, Schoenecker PL, Thorsness R, Clohisy JC. Periacetabular osteotomy and combined femoral head-neck junction osteochondroplasty. A minimum two-year follow-up cohort study. J Bone Joint Surg Am. 2012;94:1959-1966. [DOI] [PubMed] [Google Scholar]
- 65. Nepple JJ, Byrd JW, Siebenrock KA, Prather H, Clohisy JC. Overview of treatment options, clinical results, and controversies in the management of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(suppl 1):S53-S58. [DOI] [PubMed] [Google Scholar]
- 66. Novais EN, Heyworth B, Murray K, Johnson VM, Kim YJ, Millis MB. Physical activity level improves after periacetabular osteotomy for the treatment of symptomatic hip dysplasia. Clin Orthop Relat Res. 2013;471:981-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. O’Kane JW, Levy MR, Pietila KE, Caine DJ, Schiff MA. Survey of injuries in Seattle area Levels 4 to 10 female club gymnasts. Clin J Sports Med. 2011;21:486-492. [DOI] [PubMed] [Google Scholar]
- 68. Orishimo KF, Kremenic IJ, Pappas E, Hagins M, Liederbach M. Comparison of landing biomechanics between male and female professional dancers. Am J Sports Med. 2009;37:2187-2193. [DOI] [PubMed] [Google Scholar]
- 69. Pacey V, Nicholson LL, Adams RD, Munn J, Munns CF. Generalized joint hypermobility and risk of lower limb injury during sport: a systematic review with meta-analysis. Am J Sports Med. 2010;38:1487-1497. [DOI] [PubMed] [Google Scholar]
- 70. Parvizi J, Bican O, Bender B, et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24(6 suppl):110-113. [DOI] [PubMed] [Google Scholar]
- 71. Philippon MJ, Briggs KK, Hay CJ, Kuppersmith DA, Dewing CB, Huang MJ. Arthroscopoic labral reconstruction in the hip using iliotibial band autograft: technique and early outcomes. Arthroscopy. 2010;26:750-756. [DOI] [PubMed] [Google Scholar]
- 72. Philippon MJ, Pennock A, Gaskill TR. Arthroscopic reconstruction of the ligamentum teres. Technique and early outcomes. J Bone Joint Surg Br. 2012;94:1494-1498. [DOI] [PubMed] [Google Scholar]
- 73. Quatman CE, Ford KR, Myer GD, Paterno MV, Hewett TE. The effects of gender and pubertal status on generalized joint laxity in young athletes. J Sci Med Sport. 2008;11:257-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. J Bone Jont Surg Am. 2009;91:192-197. [DOI] [PubMed] [Google Scholar]
- 75. Reid DC, Burnham RS, Saboe LA, Kushner SF. Lower extremity flexibility patterns in classical ballet dancers and their correlation to lateral hip and knee injuries. Am J Sports Med. 1987;15:347-352. [DOI] [PubMed] [Google Scholar]
- 76. Ross JR, Schoenecker PL, Clohisy JC. Surgical dislocation of the hip: evolving indications. HSS J. 2013;9:60-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39(suppl 1):72S-78S. [DOI] [PubMed] [Google Scholar]
- 78. Roussel NA, Nijs J, Mottram S, Van Moorsel A, Truijen S, Stassijns G. Altered lumbopelvic movement control but not generalized joint hypermobility is associated with increased injury in dancers. A prospective study. Manual Ther. 2009;14:630-635. [DOI] [PubMed] [Google Scholar]
- 79. Sands WA, Shultz BB, Newman AP. Women’s gymnastics injuries: a 5-year study. Am J Sports Med. 1993;21:271-276. [DOI] [PubMed] [Google Scholar]
- 80. Sansone M, Ahldén M, Jónasson P, Swärd L, Eriksson T, Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21:420-423. [DOI] [PubMed] [Google Scholar]
- 81. Scheper MC, deVries JE, deVos R, Verbunt J, Nollet F, Englebert RH. Generalized joint hypermobility in professional dancers: a sign of talent or vulnerability? Rheumatology (Oxford). 2013;52:651-658. [DOI] [PubMed] [Google Scholar]
- 82. Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement. A comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93:1027-1032. [DOI] [PubMed] [Google Scholar]
- 83. Signorelli C, Lopomo N, Bonanzinga T, et al. Relationship between femoroacetabular contact areas and hip position in the normal joint: an in vitro evaluation. Knee Surg Sports Traumatol Arthrosc. 2013;21:408-414. [DOI] [PubMed] [Google Scholar]
- 84. Simpson JM, Field R, Villar RN. Arthroscopic reconstruction of the ligamentum teres. Arthroscopy. 2011;27:436-441. [DOI] [PubMed] [Google Scholar]
- 85. Sink EL, Gralla J, Ryba A, Dayton M. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop. 2008;28:806-811. [DOI] [PubMed] [Google Scholar]
- 86. Skendzel JG, Weber AE, Ross JR, et al. The approach to the evaluation and surgical treatment of mechanical hip pain in the young patient: AAOS exhibit selection. J Bone Joint Surg Am. 2013;95:e133. [DOI] [PubMed] [Google Scholar]
- 87. Stafford GH, Villar RN. Ischiofemoral impingement. J Bone Joint Surg Br. 2011;93:1300-1302. [DOI] [PubMed] [Google Scholar]
- 88. Stein DA, Polatsch DB, Gidumal R, Rose DJ. Low-energy anterior hip dislocation in a dancer. Am J Orthop. 2002;31:591-594. [PubMed] [Google Scholar]
- 89. Steinberg N, Hershkovitz I, Peleg S, et al. Range of joint movement in female dancers and nondancers aged 8 to 16 years. Am J Sports Med. 2006;34:814-823. [DOI] [PubMed] [Google Scholar]
- 90. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747-1770. [DOI] [PubMed] [Google Scholar]
- 91. Tosun O, Cay N, Bozkurt M, Arslan H. Ischiofemoral impingement in an 11-year-old girl. Diagn Interv Radiol. 2012;18:571-573. [DOI] [PubMed] [Google Scholar]
- 92. US Census Bureau. Statistical Abstract of the United States 2012 (131st edition): Arts, Recreation and Travel. Washington, DC: US Census Bureau; 2011. http://www.census.gov/compendia/statab. Accessed February 8, 2013. [Google Scholar]
- 93. van Bergayk AB, Garbuz DS. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br. 2002;84:339-343. [DOI] [PubMed] [Google Scholar]
- 94. Walker JA, Pagnotto M, Trousdale RT, Sierra RJ. Preliminary pain and function after labral reconstruction during femoroacetabular impingement surgery. Clin Orthop Relat Res. 2012;470:3414-3420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Wassilew GI, Janz V, Heller MO, et al. Real time visualization of femoroacetabular impingement and subluxation using 320-slice computed tomography. J Orthop Res. 2013;31:275-281. [DOI] [PubMed] [Google Scholar]
- 96. Wynne-Davies R. Acetabular dysplasia and familial joint laxity: two etiological factors in congenital dislocation of the hip. J Bone Joint Surg Br. 1970;52:704-716. [PubMed] [Google Scholar]
- 97. Yamamoto Y, Usui I. Arthroscopic surgery for degenerative rupture of the ligamentum teres femoris. Arthroscopy. 2006;22:689.e1-689.e3. [DOI] [PubMed] [Google Scholar]
- 98. Zaltz I, Kelly BT, Larson CM, Leunig M, Bedi A. Surgical treatment of femoroacetabular impingement: what are the limits of hip arthroscopy? Arthroscopy. 2014;30:99-110. [DOI] [PubMed] [Google Scholar]