Abstract
Upper extremity stress fractures, which are relatively rare, have become increasingly common, with olecranon stress injuries representing a subset primarily affecting throwing athletes. Olecranon stress fractures have been classified to fit specific radiographic patterns, with most of these injuries typified by a fracture line. Only a handful of olecranon stress injury cases report magnetic resonance imaging findings of osseous edema within the olecranon, as in our case of a 17-year-old competitive overhand baseball pitcher with elbow pain. The patient was treated conservatively and had resolution of pain after 6 weeks of rest, followed by a 6-week throwing progression with full return to pitching.
Keywords: elbow, MRI, olecranon, stress fracture, overuse injury
Olecranon stress fractures can be categorized radiographically, with most of these injuries typified by a fracture line. No fracture line was visualized in this case.
Case Report
A 17-year-old left hand–dominant competitive overhand baseball pitcher presented after 1 week of posterior elbow pain refractory to analgesia and limited rest. Although he suffered no known prior elbow injury, he had been throwing up to 150 pitches a week with a peak velocity of 82 mph and a short rest period prior to onset of symptoms. In addition to pitching, he also had been playing first base and outfield. He complained of pain at the posterior and lateral aspects of the left olecranon, with radiation to his biceps muscle intermittently. The quality of his pain was initially dull but evolved to sharp in nature with throwing. Eventually, the pain became unbearable after fielding a ground ball and throwing to first base, and he ceased pitching at that point. The pain did not improve with ibuprofen.
On examination, there was significant left posterior olecranon process tenderness to palpation without edema or ecchymosis with a normal carrying angle. He had no tenderness of the left medial epicondyle, lateral epicondyle, or radial head. No elbow effusion was noted. Full elbow range of motion in flexion and extension was noted, and there was no deficit in strength testing. Pain was elicited with resisted supination. He had no laxity on valgus or varus stress as well as a negative Milking test.7 Tinel test was negative at both the wrist and cubital tunnel. Vascular and sensory examinations were normal.
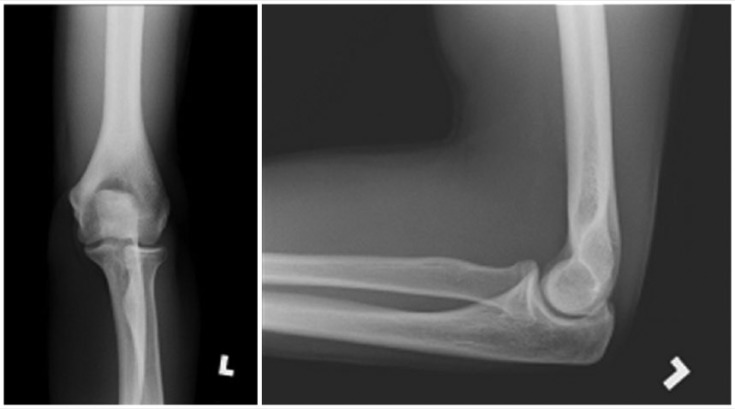
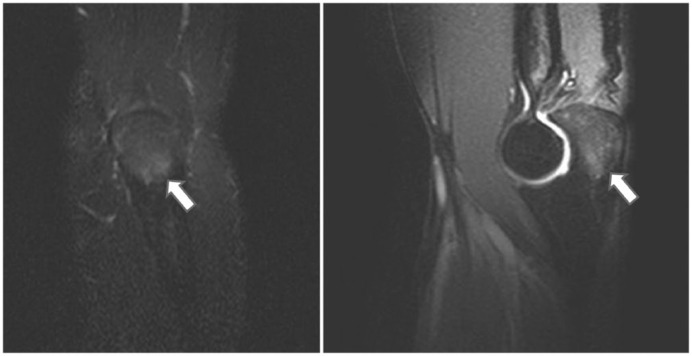
The differential diagnosis included triceps tendonitis, osteochondritis dissecans of the capitellum, chondral defect/injury, and posteromedial elbow impingement. Radiographs of the left elbow (Figure 1) did not reveal a fracture line or other interosseous abnormality, prompting magnetic resonance imaging (MRI). The MRI without contrast (Figure 2) identified a confluent area of edema along the olecranon process, more so medially, without an identifiable fracture line, suggestive of stress-related changes. The diagnosis of an olecranon stress fracture was made, and the patient was immediately notified to cease further pitching or throwing activities.
Figure 1.
Patient’s normal anteroposterior and lateral radiograph of the left elbow. Note the fused olecranon apophysis, suggesting that the patient is skeletally mature.
Figure 2.
Fat-saturated, T2-weighted magnetic resonance image of the left elbow reveals edema (arrows) of the olecranon in the coronal (left image) and sagittal (right image) planes. No triceps tendon or significant ligamentous pathology was identified.
Discussion
Upper extremity stress fractures have been documented with increased frequency, including olecranon stress fractures.14 Olecranon stress fractures, while occurring predominantly in throwing and overhead athletes,12,13 have occurred in gymnasts,5 weight lifters,22 tower-diving swimmers,24 and javelin throwers.10 In an analysis of a panel of 196 patients with stress fractures, Iwamoto and Takeda found olecranon stress fractures to rank as the fourth most common (8.7%) behind the tibia (40.3%), rib (15.8%), and metatarsal bone (9.7%).13 Another study of 70 athletes by Miller and Kaeding17 reported 4 of the 7 athletes with olecranon stress fractures were throwers.
Olecranon stress fractures have been classified in various manners5,18: Transverse fractures and osteochondroses occur in the skeletally immature,16 whereas fractures of the olecranon tip and straight or oblique fractures through the midportion of the olecranon occur in skeletally mature patients, both of which have been seen in throwers.10,19 A classification-based treatment system stratified olecranon stress fractures into 5 types: (1) adolescent olecranon apophyseal line stress injuries, (2) metaphyseal olecranon stress reaction, (3) oblique mid-olecranon stress fracture, (4) transverse proximal olecranon stress fracture, and (5) olecranon tip stress fractures.8(pp249-259) Most recently, a new classification system based on the direction of the fracture line with corresponding mean age was delineated: (1) physeal, 14.1 years; (2) classic, 18.6 years; (3) transitional, 16.9 years; (4) sclerotic, 18.0 years; and (5) distal, 19.6 years. The physeal type, which is most common in adolescents and occurs when delayed closure or nonunion is found along the line of the epiphyseal plate, was the most common in this study and further divided into 4 stages based on severity.9
Unlike the majority of the aforementioned stress injury patterns, this patient’s MRI revealed confluent bone marrow edema without a distinct fracture line or sclerotic borders. Stress reactions are likely an intermediary point on the spectrum between normal physiologic response and stress fractures themselves. Although seldom reported, or perhaps underrecognized, olecranon stress reactions have been identified in throwing athletes.10-13,17-19,25 In a retrospective review series of 7 professional baseball players between the ages of 18 and 29 years, several players had stress reactions without fracture lines, including 1 characterized by bone edema throughout the proximal ulna and another involving the posteromedial superior aspect of the olecranon.23 All 7 players had an intact ulnar collateral ligament. Similarly, in a different case, a 16-year-old pitcher had persistent and painful intraosseous edema due to suspected traction forces on the olecranon.20
Mechanism
The pathophysiology of stress fractures has not been fully elucidated, although there have been several proposed mechanisms. One hypothesis is that repetitive loading of the structures results in repetitive microdamage that outpaces bone remodeling, culminating in a stress fracture at the area of focal weakness, namely the cement lines between the concentric rings of collagen fibers known as Haversian systems.14,21 The other hypothesis is that accelerated bone remodeling, either general or localized, puts the affected area in a weakened state susceptible to microdamage and subsequent stress fracture.4 Regardless of the etiology, olecranon stress disorders ultimately derive from individual or a combination of directed biomechanical forces arising from altered throwing mechanics and/or overuse. The mechanism of injury is thought to stem from impingement of the olecranon in the olecranon fossa or by excessive tensile force of the triceps brachii muscle on the olecranon during the acceleration phase of throwing.6,25 King et al15 used high-speed motion photography to analyze joint function in baseball players and did not find any evidence of impingement by the surrounding structures in the region of the fossa at the termination of the throwing motion in pitchers without flexion contractures; this ostensibly applies to the adolescent pitcher because of lack of olecranon process hypertrophy. In contrast, resisting valgus stress at the elbow against the medial aspect of the trochlear groove and the olecranon fossa subsequently leads to osteophyte formation at the posterior and posteromedial aspects of the olecranon tip and can cause chondromalacia and loose body formation,26 commonly referred to as valgus extension overload syndrome (“pitcher’s elbow”). In addition, there is evidence substantiating a link between valgus extension overload and olecranon stress fracture due to the repetitive abutment of the olecranon into the olecranon fossa combined with valgus torque, resulting in impaction and shearing forces along the posteromedial olecranon,1 whereas in weight lifters and gymnasts, the stress injury is caused by impaction force due to triceps traction force and overextension.10,16 The type of sport and distinct mechanics involved are not the only directing factors. The athlete’s age and skeletal maturity, specifically the state of closure of the epiphyseal plate of the olecranon, have implications on pattern of injury as well as potential consequences on severity of injury in throwing athletes.9 This patient’s epiphyseal plate was closed, ostensibly decreasing a predisposition to a physeal-type stress injury (see Figure 1).
Furushima et al9 showed that the different patterns of olecranon stress fractures in throwing athletes arose from the articular surface, whereas tensile force from the triceps should result in a dorsal origin. In a study of 200 baseball players with olecranon stress fractures, there was an associated ulnar collateral ligament injury and/or medial epicondyle avulsion fracture diagnosed in 71% to 95% of cases; an ulnar collateral ligament insufficiency alters the contact area and pressure between the posteromedial trochlea and olecranon articular surface.2
Follow-up
This patient was “shut down” from all throwing activity for a period of 6 weeks, followed by physical therapy for a standardized interval throwing progression. Elbow injuries occur more commonly in players with poor sporting technique (52%) than in players with proper technique (6%).3 The patient sustained no setbacks or return of pain during his 6-week course of therapy and has since completed a home exercise program during his sport’s offseason, with future plans to participate in a pitching showcase.
Conclusion
The early detection of this injury prompted the cessation of pitching before any visible fracture line or injury progression could become evident. This case highlights several salient points on olecranon stress fractures: (1) the implication of type of sport as well as the athlete’s age on injury type and severity, (2) the need for a higher index of clinical suspicion in high-volume throwing athletes, (3) the role for using MRI early on, and (4) the importance of monitoring pitch counts and evaluating pitching mechanics in young baseball athletes.
Acknowledgments
The authors thank Kristopher Fayock, MD (Christiana Care Health System).
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Ahmad CS, ElAttrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004;23:665-676. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad CS, Park MC, ElAttrache NS. Elbow medial ulnar collateral ligament insufficiency alters posteromedial olecranon contact. Am J Sports Med. 2004;32:1607-1612. [DOI] [PubMed] [Google Scholar]
- 3. Albright JA, Jokl P, Shaw R, Albright JP. Clinical study of baseball pitchers: correlation of injury to the throwing arm with method of delivery. Am J Sports Med. 1978;6:15-21. [DOI] [PubMed] [Google Scholar]
- 4. Bennell KL, Malcolm SA, Wark JD, Brukner PD. Models for the pathogenesis of stress fractures in athletes. Br J Sports Med. 1996;30:200-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brukner P. Stress fractures of the upper limb. Sports Med. 1998;26:415-424. [DOI] [PubMed] [Google Scholar]
- 6. Cain EL, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31:621-635. [DOI] [PubMed] [Google Scholar]
- 7. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9:99-113. [DOI] [PubMed] [Google Scholar]
- 8. Dines JS, Altchek DW, Andrews J, ElAttrache NS, Wilk KE, Yocum LA, eds. Sports Medicine of Baseball. 1st ed Philadelphia, PA: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 9. Furushima K, Itoh Y, Iwabu S, Yamamoto Y, Koga R, Shimizu M. Classification of olecranon stress fractures in baseball players. Am J Sports Med. 2014;42:1343-1351. [DOI] [PubMed] [Google Scholar]
- 10. Hulkko A, Orava S, Nikula P. Stress fractures of the olecranon in javelin throwers. Int J Sports Med. 1986;7:210-213. [DOI] [PubMed] [Google Scholar]
- 11. Hulkko A, Orava S. Stress fractures in athletes. Int J Sports Med. 1987;8:221-226. [DOI] [PubMed] [Google Scholar]
- 12. Iwamoto J, Sato Y, Takeda T, Matsumoto H. Analysis of stress fractures in athletes based on our clinical experience. World J Orthop. 2011;2:7-12. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 13. Iwamoto J, Takeda T. Stress fractures in athletes: review of 196 cases. J Orthop Sci. 2003;8:273-278. [DOI] [PubMed] [Google Scholar]
- 14. Jones GL. Upper extremity stress fractures. Clin Sports Med. 2006;25:159-174. [DOI] [PubMed] [Google Scholar]
- 15. King JW, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res. 1969;67:116-123. [PubMed] [Google Scholar]
- 16. Maffulli N, Chan D, Aldridge MJ. Overuse injuries of the olecranon in young gymnasts. J Bone Joint Surg Br. 1992;74:305-308. [DOI] [PubMed] [Google Scholar]
- 17. Miller TL, Kaeding CC. Upper-extremity stress fractures: distribution and causative activities in 70 patients. Orthopedics. 2012;35:789-793. [DOI] [PubMed] [Google Scholar]
- 18. Nakaji N, Fujioka H, Tanaka J, et al. Stress fracture of the olecranon in an adult baseball player. Knee Surg Sports Traumatol Arthrosc. 2006;14:390-393. [DOI] [PubMed] [Google Scholar]
- 19. Nuber GW, Diment MT. Olecranon stress fractures in throwers. A report of two cases and a review of the literature. Clin Orthop Relat Res. 1992;(278):58-61. [PubMed] [Google Scholar]
- 20. Parr TJ, Burns TC. Overuse injuries of the olecranon in adolescents. Orthopedics. 2003;26:1143-1146. [DOI] [PubMed] [Google Scholar]
- 21. Pegrum J, Crisp T, Padhiar N. Diagnosis and management of bone stress injuries of the lower limb in athletes. BMJ. 2012;344:e2511. [DOI] [PubMed] [Google Scholar]
- 22. Rao PS, Rao SK, Navadgi BC. Olecranon stress fracture in a weight lifter: a case report. Br J Sports Med. 2001;35:72-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schickendantz MS, Ho CP, Koh J. Stress injury of the proximal ulna in professional baseball players. Am J Sports Med. 2002;30:737-741. [DOI] [PubMed] [Google Scholar]
- 24. Shinozaki T, Kondo T, Takagishi K. Olecranon stress fracture in a young tower-diving swimmer. Orthopedics. 2006;29:693-694. [DOI] [PubMed] [Google Scholar]
- 25. Slocum DB. Classification of elbow injuries from baseball pitching. Tex Med. 1968;64(3):48-53. [PubMed] [Google Scholar]
- 26. Wilson FD, Andrews JR, Blackburn TA, McCluskey G. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83-88. [DOI] [PubMed] [Google Scholar]