Abstract
Context:
Despite the significant attention directed toward optimizing arthroscopic rotator cuff repair, there has been less focus on rehabilitation after rotator cuff repair surgery.
Objective:
To determine the effect of different rehabilitation protocols on clinical outcomes by comparing early versus late mobilization approaches and continuous passive mobilization (CPM) versus manual therapy after arthroscopic rotator cuff repair.
Data Sources:
PubMed was searched for relevant articles using the keywords rotator cuff, rotator, cuff, tears, lacerations, and rehabilitation to identify articles published from January 1980 to March 2014.
Study Selection:
Inclusion criteria consisted of articles of level 1 or 2 evidence, written in the English language, and with reported outcomes for early versus late mobilization or rehabilitation with CPM versus manual therapy after primary arthroscopic rotator cuff repair. Exclusion criteria consisted of articles of level 3, 4, or 5 evidence, non-English language, and those with significantly different demographic variables between study groups. Included studies were evaluated with the Consolidated Standards of Reporting Trials criteria.
Study Design:
Systematic review.
Level of Evidence:
Level 2.
Data Extraction:
Level of evidence, study type, number of patients enrolled, number of patients at final follow-up, length of follow-up, age, sex, rotator cuff tear size, surgical technique, and concomitant operative procedures were extracted from included articles. Postoperative data included clinical outcome scores, visual analog score for pain, shoulder range of motion, strength, and rotator cuff retear rates.
Results:
A total of 7 studies met all criteria and were included in the final analysis. Five studies compared early and late mobilization. Two studies compared CPM and manual therapy.
Conclusion:
In general, current data do not definitively demonstrate a significant difference between postoperative rotator cuff rehabilitation protocols that stress different timing of mobilization and use of CPM.
Keywords: arthroscopic, rotator cuff, rehabilitation, mobilization timing, continuous passive mobilization, manual therapy
The ultimate goals of rotator cuff tear management are to relieve pain and restore shoulder function. Rehabilitation after surgical management is crucial to realize these goals and improve patient functional outcome, range of motion, and strength.9,14 Although rehabilitation protocols may differ widely among surgeons, there exist 2 central parameters that can differentiate protocols: timing of mobilization and continuous passive mobilization (CPM).
Currently, there is no consensus regarding the optimal timing of mobilization after arthroscopic rotator cuff repair. Some advocate early mobilization to prevent postoperative stiffness and subsequent decreased range of motion and function.16 Others advocate a delay in mobilization to avoid compromise of tendon healing and integrity. Tendon integrity remains a valid concern as the retear rate after arthroscopic rotator cuff repair has been reported to be as high as 94% for massive cuff tears.2,5,11 However, a variety of factors such as patient age and initial tear size are risk factors for recurrent tears.12,15
Additionally, debate exists regarding the use of CPM in rehabilitation protocols after arthroscopic rotator cuff repair. CPM may allow cautious early mobilization, an increase in collagen tissue healing with proper fiber orientation, and better functional outcomes after total knee arthroplasty.10,13 However, there is a lack of consensus regarding its effect on functional outcomes in arthroscopic rotator cuff repair. Furthermore, it is unknown whether CPM offers benefit over manual therapy.
Given the central role of rehabilitation, the authors conducted a qualitative systematic review to investigate the optimal timing of therapy and the use of CPM in rehabilitation after rotator cuff repair. The primary purpose was to review all level 1 and 2 studies that evaluated the clinical outcomes of early versus late mobilization and CPM versus manual therapy after arthroscopic rotator cuff repair to compare the efficacies of these approaches. The authors hypothesized that clinical outcomes between patients that undergo early versus late mobilization and between patients that undergo CPM versus manual therapy are not statistically different.
Methods
Studies were included that met the following criteria: level 1 or 2 evidence, written in English, compared outcomes between patients undergoing early versus late mobilization or compared outcomes between patients undergoing rehabilitation with CPM versus manual therapy after primary arthroscopic rotator cuff repair, and detailed the rehabilitation protocol. Studies were excluded if they: had level 3, 4, or 5 evidence, were non-English articles, or maintained a significant difference between study groups in terms of demographic variables.
Literature Search
PubMed was used to find relevant articles, published between January 1980 and March 2014, on rehabilitation after arthroscopic rotator cuff repair using the keywords rotator cuff, rotator, cuff, tears, lacerations, and rehabilitation. General search terms were used to prevent the inadvertent neglect of potential studies. The references of all included studies were carefully reviewed for studies not identified by our literature search. Two independent reviewers reviewed the abstract of every article to determine the methods and subsequently reviewed all articles that met the aforementioned inclusion and exclusion criteria. The Consolidated Standards of Reporting Trials (CONSORT) 2010 checklist was used by both independent reviewers for quality appraisal of each randomized controlled study eligible for final inclusion.17
Data Extraction
Level of evidence, study type, number of patients enrolled, number of patients at final follow-up, length of follow-up, age, sex, rotator cuff tear size, surgical technique, and concomitant operative procedures were extracted from included articles. Postoperative data included clinical outcome scores, visual analog score for pain, shoulder range of motion, strength, and rotator cuff retear rates (Table 1).
Table 1.
Patient demographics and rotator cuff tear classification
| Study | Level of Evidence | Study Type | Patients Enrolled, n | Patients at Final Follow-up, n | Mean Follow-up, mo | Average Age, y | Men | Women | Small Tear (<1 cm) | Medium Tear (1-3 cm) | Large Tear (3-5 cm) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Arndt et al1 | 1 | Early vs late mobilization | 100 | 92 | 16 | 55 | 34 | 58 | NR | NR | NR |
| Cuff and Pupello3 | 1 | Early vs late mobilization | 68 | 68 | 12 | 63 | 38 | 30 | NR | NR | NR |
| Düzgün et al4 | 1 | Early vs late mobilization | 29 | 29 | 6 | 56 | 3 | 26 | NR | 12 | 17 |
| Garofalo et al6 | 1 | CPM vs manual therapy | 100 | 100 | 12 | 60 | 47 | 53 | NRa | NRa | NRa |
| Keener et al7 | 1 | Early vs late mobilization | 145 | 114 | 24 | 55 | 73b | 51b | NR | NR | NR |
| Kim et al8 | 1 | Early vs late mobilization | 117 | 105 | 12 | 60 | 44 | 61 | NRc | NRc | NR |
| Lee et al9 | 1 | CPM vs manual therapy | 85 | 64 | 25 | 55 | 41 | 23 | 0 | 41 | 23 |
CPM, continuous passive mobilization; NR, not reported.
All had C2-C318 rotator cuff tears (C2, <2 cm; C3, 3-4 cm).
Reflects patients who underwent surgery.
All were small- or medium-sized tears.
Results
Literature Search
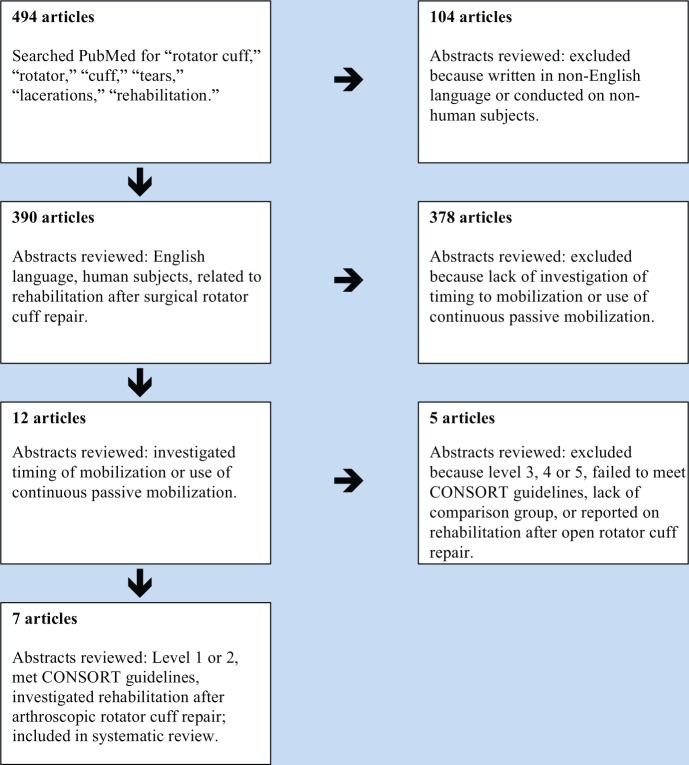
The literature search is detailed in Figure 1.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram.
Patient Demographics
Patient demographics are available in Table 1. None of the studies investigating the use of CPM reported the effective follow-up for each study group individually.6,9 Five studies included a study of homogeneity to ensure that comparison groups were not significantly different in terms of baseline characteristics.1,4,7-9 One study6 matched for age and sex and another study3 did not specify whether a study of homogeneity was performed, but showed similar comparison group baseline characteristics in tabular format without mentioning statistical significance.
Rotator Cuff Tear Classification
Tear sizes were classified as small (<1 cm), medium (1-3 cm), large (3-5 cm), and massive (>5 cm). Full- and partial-thickness tears were included in the studies (Table 1).
Surgical Technique and Concomitant Procedures
All included studies involved all-arthroscopic rotator cuff repair, although the exact method varied (Table 2).
Table 2.
Surgical procedures, concomitant procedures, and retear rate
| Study | Arthroscopic Technique | Concomitant Procedures | Retear Rate, % | Modality Used to Determine Retear |
|---|---|---|---|---|
| Arndt et al1 | Single-row fixation (59%), double-row fixation (41%) | Long head of biceps tenotomy (65%), long head of biceps tenodesis (11%), acromioplasty (91%), AC joint ostephyte removal (5%), complete AC resection (15%) | 20 | Arthro–computed tomography |
| Cuff and Pupello3 | Transosseous equivalent suture bridge (100%) | Subacromial decompression (100%) | 12 | Ultrasound |
| Düzgün et al4 | 1 anchor (76%), 2 anchors (24%); Side-to-side technique: 1 (38%), 2 (14%), 3 (3%) | NR | NR | NR |
| Garofalo et al6 | Double-loaded titanium suture anchor (100%) | NR | NR | NR |
| Keener et al7 | Modified double-row transosseus technique (100%) | Subacromial decompression (100%), acromioplasty (100%) | 16 | Ultrasound |
| Kim et al8 | Single-row fixation (16%), double-row fixation (2%), suture bridge (82%) | Subacromial decompression (100%), acromioplasty (100%) | NR | NR |
| Lee et al9 | Single-row fixation (100%); 1 or 2 anchors (64%), 3 or 4 anchors (36%) | Subacromial decompression (100%) | 16 | Magnetic resonance imaging |
AC joint, acromioclavicular joint; NR, not reported.
Rehabilitation Protocol
Tables 3 and 4 outline the rehabilitation protocols used in the included studies.
Table 3.
Rehabilitation protocols in studies comparing early versus late mobilization
| Early Group | Late Group | |
|---|---|---|
| Arndt et al1 | 3-5 physical therapy sessions per week starting on day after operation (stressing pendulum exercise, manual passive ROM, and CPM) | Sling immobilization for 6 weeks postoperatively |
| Identical progressive active ROM rehabilitation protocol started at 6 weeks postoperatively | ||
| Cuff and Pupello3 | 3 physical therapy sessions per week starting on postoperative day 2 (stressing pendulum exercise and graduated passive ROM) for 6 weeks | Sling immobilization for 6 weeks postoperatively, but pendulum exercises (3 times daily for 5 min/session) during this time period |
| Active assisted ROM at weeks 6-10Active ROM to tolerance at weeks 10-12Rotator cuff muscle strengthening at week 12 | Passive ROM at week 6; then started same protocol that “Early Group” started at week 6 | |
| Düzgün et al4 | Identical protocols consisting of progressive increases in active ROM and exercise intensity | |
| Reached final stage (active ROM against resistance and rotator cuff muscle strengthening) at week 7 | Reached final stage at week 18 | |
| Keener et al7 | Initial 6 weeks of passive ROM, progressive active ROM in subsequent 6 weeks, and rotator cuff strengthening 3-4 months postoperatively | |
| Protocol started at first postoperative visit (10-14 days) | Protocol started 6 weeks postoperatively | |
| Kim et al8 | Passive shoulder ROM initiated on postoperative day 1 | Shoulders immobilized for 4 or 5 weeks postoperatively (based on tear size) |
| At 4-5 weeks postoperatively, identical progressive increases in active ROM and rotator cuff muscle strengthening at 9-12 weeks postoperatively | ||
CPM, continuous passive mobilization; ROM, range of motion.
Table 4.
Rehabilitation protocols in studies comparing manual therapy versus CPM
| Manual Therapy Group | CPM Group | |
|---|---|---|
| Garofalo et al6 | Shoulders immobilized 4 weeks in both groups | |
| Progressive pendulum and passive ROM exercises for the next 4 weeks | CPM regimen in addition to progressive pendulum and passive ROM exercises for the next 4 weeks | |
| Starting at 8 weeks postoperatively, both groups stress identical increases in passive and active ROM | ||
| Lee et al9 | Starting on day of surgery, pendulum and progressive passive ROM ×6 weeks | Starting on day of surgery, CPM machine with stretching limited to 90° ×3 weeksProgressive increases in passive ROM for next 3 weeks |
| In both groups, active ROM started at 6 weeks postoperatively | ||
CPM, continuous passive mobilization; ROM, range of motion.
Functional Scores
All studies investigating early versus late mobilization reported functional outcome scores (Table 5). Only 1 of 2 studies evaluating CPM versus manual therapy reported functional scores (Table 6).
Table 5.
Early versus late mobilization: functional and pain scores
| Mean Follow-up, mo | Constant Score | ASES Score | VAS Pain Score at Rest | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | Early | Late | P Value | Early | Late | P Value | Early | Late | P Value | |
| Arndt et al1 | 16 | 77.6 ± 12.4 | 69.7 ± 18.0 | 0.045 | NR | NR | NR | NR | NR | NR |
| Cuff and Pupello3 | 12 | NR | NR | NR | 91.1 | 92.8 | <0.0049a | NR | NR | NR |
| Düzgün et al4 | 6 | NR | NR | NR | NR | NR | NR | —b | —b | NR |
| Keener et al7 | 24 | 83.2 ± 11.5 | 84.3 ± 10.8 | 0.5 | 91.0 ± 15.3 | 93.3 ± 10.6 | 0.75 | 0.9 ± 1.7 | 0.6 ± 1.1 | 0.26 |
| Kim et al8 | 12 | 69.81 | 69.83 | 0.854 | 73.29 | 82.90 | 0.216 | 2.8 | 1.8 | 0.34 |
ASES, American Shoulder and Elbow Surgeons score; NR, not reported; VAS, visual analog scale.
Preoperative ASES scores were significantly different between groups.
No numerical data reported; data reported in graphical format.
Table 6.
CPM versus manual therapy: functional and pain scores
| Mean Follow-up, mo | UCLA Score | VAS Pain Score at Rest | |||||
|---|---|---|---|---|---|---|---|
| Study | CPM | Manual | P Value | CPM | Manual | P Value | |
| Garofalo et al6 | 12 | NR | NR | NR | 0.2 ± 0.1 | 0.2 ± 0.2 | >0.05 |
| Lee et al9 | 12 | 31.8 | 32.3 | 0.341 | 0.15 | 0.23 | 0.382 |
CPM, continuous passive mobilization; NR, not reported; UCLA, University of California Los Angeles; VAS, visual analog scale.
Pain
Pain data are summarized in Tables 5 and 6 for early versus late mobilization and CPM versus manual therapy, respectively.
Range of Motion
Range of motion data are summarized in Tables 7 and 8 for early versus late mobilization and CPM versus manual therapy, respectively.
Table 7.
Early versus late mobilization: range of motion (in degrees unless noted otherwise)
| Mean Follow-up, mo | Forward Flexion | External Rotation | External Rotation With Abduction to 90° | Internal Rotation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Early | Late | P Value | Early | Late | P Value | Early | Late | P Value | Early | Late | P Value | |
| Arndt et al1 | 16 | 172.4 ± 13.0 | 163.3 ± 25.1 | 0.094 | 58.7 ± 12.9 | 49.1 ± 18.0 | 0.011 | NR | NR | NR | NR | NR | NR |
| Cuff and Pupello3 | 12 | 174 | NR | 0.063 | 46 | 45 | 0.668 | NR | NR | NR | 94a | 91a | 0.99 |
| Düzgün et al4 | 6 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Keener et al7 | 24 | 164 ± 13.4 | 163 ± 15.8 | 0.85 | 62.0 ± 16.4 | 66.2 ± 14.0 | 0.15 | 90.0 ± 10.3 | 87.7 ± 11.9 | 0.27 | NR | NR | NR |
| Kim et al8 | 12 | 159.75 | 153.67 | 0.206 | 78.50 | 81.33 | 0.623 | NR | NR | NR | T 10.0 | T 9.9 | 0.854 |
NR, not reported.
Percentage of patients achieving full internal rotation.
Table 8a.
CPM versus manual therapy: range of motion (in degrees)
| Mean Follow-up, mo | Forward Flexion | External Rotation | |||||
|---|---|---|---|---|---|---|---|
| Study | CPM | Manual | P Value | CPM | Manual | P Value | |
| Garofalo et al6 | 12 | 165.2 ± 8 | 158 ± 10.1 | >0.05 | 86 ± 4 | 85 ± 4.2 | >0.05 |
| Lee et al9 | 12 | 153.0 ± 12.2 | 155.3 ± 13.0 | 0.729 | 48.1 ± 13.9 | 53.0 ± 11.6 | 0.078 |
CPM, continuous passive mobilization.
Table 8b.
CPM versus manual therapy: range of motion (in degrees)
| External Rotation at 90° of Abduction | Internal Rotation at 90° of Abduction | Abduction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | CPM | Manual | P Value | CPM | Manual Therapy | P Value | CPM | Manual Therapy | P Value |
| Garofalo et al6 | NR | NR | NR | NR | NR | NR | 90 ± 2.5 | 88 ± 1.8 | >0.5 |
| Lee et al9 | 77.7 ± 11.6 | 76.3 ± 12.1 | 0.778 | 54.9 ± 21.5 | 65.7 ± 13.3 | 0.057 | 161.8 ± 27.3 | 167.8 ± 12.8 | 0.884 |
CPM, continuous passive mobilization, NR, not reported.
Strength
Strength data are summarized in Tables 7 and 8 for early versus late mobilization and CPM versus manual therapy, respectively.
Tendon Retear Rate
For studies comparing early and late mobilization, 2 studies used ultrasound3,7 and 1 study used arthro–computed tomography1 to evaluate tendon retear rates. All 3 studies found a higher tendon retear rate in the early mobilization group relative to the late mobilization group, but none of the differences were statistically significant (Table 9).
Table 9.
Early versus late mobilization: tendon retear rate (%)
| Study | Mean Follow-up, mo | Early | Late | P Value |
|---|---|---|---|---|
| Arndt et al1 | 16 | 23.3 | 15.4 | 0.269 |
| Cuff and Pupello3 | 12 | 15 | 9 | 0.47 |
| Düzgün et al4 | 6 | NR | NR | NR |
| Keener et al7 | 24 | 10 | 6 | 0.46 |
| Kim et al8 | 12 | NR | NR | NR |
NR, not reported.
Lee et al,9 using magnetic resonance imaging, found a statistically nonsignificant higher tendon retear rate in the manual therapy group relative to the CPM group at final 24-month follow-up (Table 10).
Table 10.
CPM versus manual therapy: strength (in kg unless noted otherwise)
| Mean Follow-up, mo | Forward Flexion | External Rotation | Internal Rotation | Tendon Retear Rate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | CPM | Manual | P value | CPM | Manual | P value | CPM | Manual | P value | CPM | Manual Therapy | P value | |
| Garofalo et al6 | 12 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Lee et al9 | 12 | 7.33 | 7.76 | 0.227 | 7.62 | 7.94 | 0.542 | 8.44 | 8.90 | 0.450 | 8.8% | 23.3% | 0.106 |
CPM, continuous passive mobilization; NR, not reported.
Discussion
Published data do not definitively demonstrate a significant clinical difference between patients who undergo early versus late mobilization and between patients who undergo CPM versus manual therapy.
Although all 5 studies that investigated early versus late mobilization reported functional scores, there was considerable study heterogeneity. In general, there exists a possible benefit from early mobilization at early follow-up, but results are equivocal at later follow-up.
Regarding pain, the literature generally shows no significant difference between early and late rehabilitation in terms of pain as measured by visual analog scale (VAS) pain scores. Only 1 study found a lower VAS pain score in the early mobilization group at 5- and 16-week follow-up, but not at final 6-month follow-up.4
Similarly, the literature generally does not demonstrate a significant difference between early and delayed mobilization in terms of range of motion. Three studies found significantly greater forward flexion and external rotation range of motion in the early mobilization group relative to the late mobilization group, but only at early follow-up (6 months or less).1,3,7 Only 1 study reported consistently better external range of motion at each follow-up for the early mobilization group.1 Similar to the functional outcome score results, range of motion results showed a possible improved outcome at early follow-up with early mobilization and equivocal results at later follow-up.
Only 1 article comparing early versus late mobilization reported strength as an outcome and did not find a significant difference.7
The authors consistently found a statistically nonsignificant trend of higher retear rates among patients undergoing early mobilization relative to those undergoing late mobilization. The higher rate of rotator cuff retears among patients undergoing early mobilization may still be clinically significant, especially as these studies were not powered to detect a significant difference between study groups in terms of retear rates. However, the true clinical significance of postoperative rotator cuff retears is unclear. Studies have implicated male sex, older age, and larger initial tear size as risk factors for recurrent rotator cuff tears.12,15
The paucity of studies comparing CPM versus manual therapy precludes the ability to draw any meaningful conclusion regarding the efficacy of CPM. The literature shows superior results in terms of functional scores, at early 3-month follow-up only, for the manual therapy group relative to the CPM group.9 However, patients undergoing CPM had lower pain levels at early 2.5-month follow-up only,6 and a nonsignificant higher retear rate was observed in the manual therapy group.9 The clinical significance of these differences at early follow-up only is unclear.
The strengths of this systematic review include the adherence to strict inclusion and exclusion criteria, the analysis of level 1 studies only, and the high number of patients (572) included in the final analysis. In addition, the authors used 2 independent reviewers and the CONSORT 2010 checklist17 to ensure the inclusion of high-quality data.
There are several limitations to this study. First, there was heterogeneity among the included studies in terms of patient demographics, tear characteristics, rehabilitation program protocols, outcome assessment tools, and imaging modalities used to determine retear rates. This heterogeneity among individual study designs precludes data analysis through meta-analysis. The final analysis only included 7 studies identified through a single database, which may not be generalizable to current clinical practice.
Conclusion
Based on the current literature, timing of mobilization and the use of CPM after arthroscopic rotator cuff repair do not significantly affect clinical outcomes at early to midterm follow-up.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Arndt J, Clavert P, Mielcarek P, Bouchaib J, Meyer N, Kempf JF. Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: a prospective randomized study. Orthop Traumatol Surg Res. 2012;98(6 suppl):S131-S138. [DOI] [PubMed] [Google Scholar]
- 2. Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290-299. [DOI] [PubMed] [Google Scholar]
- 3. Cuff DJ, Pupello DR. Prospective randomized study of arthroscopic rotator cuff repair using an early versus delayed postoperative physical therapy protocol. J Shoulder Elbow Surg. 2012;21:1450-1455. [DOI] [PubMed] [Google Scholar]
- 4. Düzgün I, Baltacı G, Atay OA. Comparison of slow and accelerated rehabilitation protocol after arthroscopic rotator cuff repair: pain and functional activity. Acta Orthop Traumatol Turc. 2011;45:23-33. [DOI] [PubMed] [Google Scholar]
- 5. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219-224. [DOI] [PubMed] [Google Scholar]
- 6. Garofalo R, Conti M, Notarnicola A, Maradei L, Giardella A, Castagna A. Effects of one-month continuous passive motion after arthroscopic rotator cuff repair: results at 1-year follow-up of a prospective randomized study. Musculoskelet Surg. 2010;94(suppl 1):S79-S83. [DOI] [PubMed] [Google Scholar]
- 7. Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014;96:11-19. [DOI] [PubMed] [Google Scholar]
- 8. Kim Y-S, Chung SW, Kim JY, Ok J-H, Park I, Oh JH. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am J Sports Med. 2012;40:815-821. [DOI] [PubMed] [Google Scholar]
- 9. Lee BG, Cho NS, Rhee YG. Effect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: aggressive versus limited early passive exercises. Arthroscopy. 2012;28:34-42. [DOI] [PubMed] [Google Scholar]
- 10. Lenssen TA, van Steyn MJ, Crijns YH, et al. Effectiveness of prolonged use of continuous passive motion (CPM), as an adjunct to physiotherapy, after total knee arthroplasty. BMC Musculoskelet Disord. 2008;9:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liem D, Bartl C, Lichtenberg S, Magosch P, Habermeyer P. Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy. 2007;23:514-521. [DOI] [PubMed] [Google Scholar]
- 12. McElvany M, McGoldrick E, Gee A, Neradilek M, Matse F., 3rd Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sport Med. 2015;43:491-500. [DOI] [PubMed] [Google Scholar]
- 13. Pope RO, Corcoran S, McCaul K, Howie DW. Continuous passive motion after primary total knee arthroplasty. Does it offer any benefits? J Bone Joint Br. 1997;79:914-917. [DOI] [PubMed] [Google Scholar]
- 14. Raab MG, Rzeszutko D, O’Connor W, Greatting MD. Early results of continuous passive motion after rotator cuff repair: a prospective, randomized, blinded, controlled study. Am J Orthop (Belle Mead NJ). 1996;25:214-220. [PubMed] [Google Scholar]
- 15. Robinson P, Wilson J, Dalal S, Parker R, Norburn P, Roy B. Rotator cuff repair in patients over 70 years of age: early outcomes and risk factors. Bone Joint J. 2013;95:199-205. [DOI] [PubMed] [Google Scholar]
- 16. Sarver JJ, Peltz CD, Dourte L, Reddy S, Williams GR, Soslowsky LJ. After rotator cuff repair, stiffness-but not the loss in range of motion-increased transiently for immobilized shoulders in a rat model. J Shoulder Elbow Surg. 2008;17(1 suppl):108S-113S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9:672-677. [DOI] [PubMed] [Google Scholar]
- 18. Snyder S. Shoulder Arthroscopy. New York, NY: Lippincott Williams & Wilkins; 2003:207-210. [Google Scholar]