Abstract
Objectives:
The susceptibility to smoking index can be improved as it only identifies one third of future adult smokers. Adding curiosity to this index may increase the identification of future smokers and improve the identification of effective prevention messages.
Methods:
Analyses used data from the California Longitudinal Study of Smoking Transitions in Youth, for whom tobacco use behaviors, attitudes, and beliefs were assessed at 3 time points from age 12 through early adulthood. Logistic regressions were used to evaluate whether baseline curiosity about smoking was predictive of smoking during the 6-year follow-up period and whether curiosity about smoking provided evidence of incremental validity over existing measures of susceptibility to smoking.
Results:
Compared to those who were classified as definitely not curious about smoking, teens who were classified as probably not curious (OR adj = 1.90, 95% CI = 1.28–2.81) and those classified as definitely curious (OR adj = 2.38, 95% CI= 1.49–3.79) had an increase in the odds of becoming a young adult smoker. Adding curiosity to the original susceptibility to smoking index increased the sensitivity of the enhanced susceptibility index to 78.9% compared to 62.2% identified by the original susceptibility index. However, a loss of specificity meant there was no improvement in the positive predictive value.
Conclusions:
The enhanced susceptibility index significantly improves identification of teens at risk for becoming young adult smokers. Thus, this enhanced index is preferred for identifying and testing potentially effective prevention messages.
Introduction
Ideas to improve the effectiveness of interventions to prevent initiation of cigarette smoking need to come from studies of those at risk to make this transition.1 Several groups of researchers have demonstrated that the susceptibility to smoking index2 identifies teens with a twofold risk of starting to smoke3–6 and it is now widely used. However, this index could be improved as it categorizes as at risk only one third of nonsmoking teens who become future smokers.3,4 Studies identifying influences that promote or minimize the transition to smoking are much more generalizable when the study population includes a majority of future adult smokers identified while they are still nonsmokers.
Early work on measuring risk for adult smoking focused on a positive intention to smoke, but few teens had such an intention so the measure identified very few future smokers.7,8 The key advance with the susceptibility to smoking index was to classify nonsmokers as “at risk” unless they were strongly committed to remain never-smokers (Pierce, Farkas, Evans, Gilpin9—volume 1 and 2). This index also included further classification of high-risk teens by targeting self-efficacy for refusing cigarettes (ability to resist a best friend’s offer of a cigarette), the situation in which many adult smokers report having their first cigarette.10,11
Efforts to further refine identification of the lowest risk teens suggested inquiring about cognitions that may precede formation of intentions about smoking. When current smokers are asked for reasons they initiated smoking, most report that they were motivated by curiosity,12,13 as people are similarly motivated for many new behaviors.14 Curiosity has long been considered a primary cognitive motivational state underlying pursuit of novel experiences.15 Curiosity has been included as a key mediator in a number of marketing theories promoting novel consumer behavior.16,17 Thus, curiosity could be the first smoking-related cognition that an individual has, with other influences on smoking (e.g., exposure to smokers, receptivity to marketing, etc.) leading an individual to become curious. Recently, curiosity was added to susceptibility in a national study and the enhanced index identified half of never-smokers who later experimented with cigarettes.18 However, the real value of the index must be assessed by its ability to identify never-smokers who go on to become adult smokers, as many who experiment do not progress.19
The aim of this paper is to extend previous research by testing the predictive validity for young adult smoking of an enhanced susceptibility index that includes curiosity measured in a population sample of young adolescents. In this study, we use a large longitudinal study of Californians, for whom tobacco use behaviors, attitudes, and beliefs were assessed at 3 time points from age 12 through early adulthood. We hypothesize that the enhanced susceptibility index measured in the early adolescent years will predict established smoking by the time they reach young adulthood 6 years later.
Methods
Study Participants and Survey Methods
The 1996 California Tobacco Survey used a random digit dialing methodology to identify and complete interviews with a random, representative sample of 39,674 households in California. A full description of the methodology for this survey has been presented.20,21 During an initial screening interview with an adult household member (n = 39,674), the household was enumerated and all identified adolescents aged 12–17 years were scheduled for an extended phone interview. Interviews were completed with 4,287 adolescents aged 12–15 years (cooperation rate= 71.2%). Participants were consented only for the cross-sectional survey although the household did agree to be recontacted. In 1999, with separate funding for the Longitudinal Study of Smoking Transitions in Youth, we attempted to contact all 12–15 year olds who responded to the 1996 survey and consented and re-interviewed 2,825 (66%). In 2002, again with separate funding, we attempted to contact adolescents who completed the 1999 interview and consented and re-interviewed 2,034 (cooperation rate 72%). Thus 47% of a cohort of 12–15 year olds (n = 2,034 of 4,287) originally interviewed in 1996 were assessed at both 1999 and 2002. This report focuses on the 1,577 who were never-smokers in 1996 and who completed the three interviews.
Sample Weighting and Statistical Analysis
As previously described for the California Tobacco Survey,22 person-level survey weights were developed to account for adolescent selection probabilities at baseline. These were adjusted to account for nonresponse in both the baseline and follow-up interviews (using census totals). The probability of response for the longitudinal sample was adjusted for demographic characteristics, smoking status of parent, and smoking rules in the home. Replicate weights were computed so that jackknifed variance estimates could be used to account for the sampling design and the weighting scheme.23
Survey Measures
Sociodemographics
Demographic characteristics measured at baseline included age, gender, and race/ethnicity. To control for factors known to be associated with smoking, adolescents were asked about academic achievement,24–26 having family members who smoke,27–29 and having peers who smoke.30–32 Following previous work, to assess academic achievement adolescent participants were asked: “How do you do in school?,” with response categories of much better than average, better than average, average, or below average. Exposure to cigarette smokers in the family was determined with an affirmative response to either of the following questions: “Do any of your parents, step-parents or guardians now smoke cigarettes?” or “Do your older brothers or sisters smoke cigarettes? ”. Exposure to smoking among peers was indicated by any response > 0 to either of the following questions: “Of your best friends who are male, how many of them smoke?” and “Of your best friends who are female, how many of them smoke?”. Following earlier work,33 we collapsed exposure into a binary variable for family and another for friends.
Tobacco Use
Tobacco use was assessed at baseline and all follow-up waves using validated standard measures.34,35 Never-smokers at baseline were identified with a negative response to both of the following questions, “Have you ever smoked a cigarette?” and “Have you ever tried or experimented with cigarette smoking, even a few puffs?” Never-smokers at follow-ups were participants who responded “no” to the question, “Have you smoked at least 100 cigarettes in your life?” A positive response to this question during the 1999 or 2002 assessment classified the respondent as having ever established tobacco use. A repeated opportunity to inquire about tobacco use behavior was afforded by these two surveys and enabled capture of tobacco users who may have been established in 1999 but did not report established smoking in 2002 (n = 16). These cases are included given our outcome was the report of established smoking by young adulthood.
Receptivity to Tobacco Advertising
At baseline, receptivity to tobacco advertising was measured with two sets of questions: “If you were given a tee shirt or a bag that had a tobacco industry cigarette brand image on it, would you use it?”; “Think back to the cigarette advertisements you have recently seen. What is the name of the cigarette brand of your favorite cigarette advertisement?” Respondents who did not name a brand were also asked, “Of all the cigarette advertisements you have seen, which do you think attracts your attention the most?” Those who responded “probably yes” or “definitely yes” that they would use an item with a tobacco logo were classified as “highly receptive.” Those not classified as “highly receptive,” but who named a favorite cigarette brand were classified as “moderately receptive.” Remaining respondents were classified as “low receptivity” For the analyses “moderately” or “highly” receptive adolescents we each compared to the “low receptivity” adolescents. This receptivity index has been shown to have predictive validity for future smoking.36
Susceptibility to Smoking
At baseline, susceptibility to smoking2 was assessed with three items: “Do you think that in the future you might experiment with cigarettes?”; “At any time during the next year do you think you will smoke a cigarette?”; and “If one of your best friends were to offer you a cigarette, would you smoke it?” Response options included “definitely not,” “probably not,” “probably yes,” and “definitely yes.” Adolescents reporting “definitely not” to all three questions were classified as “committed never-smokers.” Those reporting “probably yes” or “definitely yes” on at least one question were classified as “highly susceptible” and the remaining respondents who did not endorse “probably yes” or “definitely yes” for any question and failed to report “definitely not” on all questions were classified as “susceptible.” The susceptibility index has been shown to be a valid predictor of future smoking initiation.2
Curiosity
At baseline, curiosity about smoking was assessed using the validated item, “Have you ever been curious about smoking a cigarette?”.37 Response options included, “definitely not,” “probably not,” “probably yes,” and “definitely yes.” Given low response rates to the highest categories, we collapsed “probably yes” and “definitely yes” to yield a three-level index for use in all analyses. This item has been shown to be a valid predictor of smoking initiation.37
Analysis Plan
We used logistic regression to evaluate whether baseline reports of curiosity about smoking were predictive of young adult smoking during the 6-year follow-up period and whether curiosity about smoking provided evidence of incremental validity over existing measures of susceptibility to smoking. The model included 1,525 adolescents after removing 52 cases with missing covariate or outcome indices. These were weighted to account for the survey design using the “survey”38 package and R statistical software.39 All models included sociodemographic, social smoking environment, perceived school performance, and level of receptivity to advertising when evaluating the relationship of curiosity and susceptibility measures with young adult smoking.
Results
Study Retention
Table 1 reports the 1996 sample characteristics of those who were resurveyed in 2002 compared to those who were not. Adolescents who were older, reported non-White race (Black or Hispanic), lower academic performance, family smoking, peer smoking, or higher receptivity to tobacco advertising were less likely to be followed (ps < .001). The likelihood of a follow up interview was not associated with susceptibility (p = .65) or curiosity (p = .17). Sample weighted base rate of established smoking was 3.3±0.5% in 1999, 14.9±1% in 2002 with 15.4±1% of adolescents reporting established smoking at one of the two surveys.
Table 1.
Comparison of Teens Who Were Followed and Not Followed Across 1996, 1999, and 2002 Surveys
| Variable | Followed to 2002 (n = 1,574) | Not followed (n = 2,077) | p value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age | |||||
| 12 | 490 | 31.13 | 443 | 21.33 | <.001 |
| 13 | 443 | 28.14 | 389 | 18.73 | |
| 14 | 352 | 22.36 | 412 | 19.84 | |
| 15 | 289 | 18.36 | 833 | 40.11 | |
| Missing | 0 | 0 | |||
| Gender | |||||
| Male | 781 | 49.62 | 1,043 | 50.22 | .725 |
| Female | 793 | 50.38 | 1,034 | 49.78 | |
| Missing | 0 | 0 | |||
| Race/ethnicity | |||||
| Non-Hispanic White | 993 | 63.09 | 923 | 44.44 | <.001 |
| Hispanic | 299 | 19.00 | 671 | 32.31 | |
| Black | 67 | 4.26 | 200 | 9.63 | |
| Asian/PI | 160 | 10.17 | 217 | 10.45 | |
| Other | 55 | 3.49 | 66 | 3.18 | |
| Missing | 0 | 0 | |||
| School performance | |||||
| Average and below | 436 | 27.70 | 786 | 37.84 | <.001 |
| Better than average | 627 | 39.83 | 773 | 37.22 | |
| Much better than average | 497 | 31.58 | 500 | 24.07 | |
| Missing | 14 | 0.89 | 18 | 0.87 | |
| Family smoking | |||||
| No | 1,114 | 70.78 | 1,292 | 62.20 | <.001 |
| Yes | 460 | 29.22 | 785 | 37.79 | |
| Missing | 0 | 0 | |||
| Peer smoking | |||||
| None smoke | 976 | 62.01 | 1,105 | 53.20 | <.001 |
| Some smoke | 598 | 37.99 | 972 | 46.80 | |
| Missing | 0 | 0 | |||
| Receptivity to ads | |||||
| Low | 557 | 35.39 | 751 | 36.16 | <.001 |
| Moderate | 769 | 48.86 | 915 | 44.05 | |
| High | 215 | 13.66 | 380 | 18.30 | |
| Missing | 33 | 2.10 | 31 | 1.49 | |
| Susceptibility index | |||||
| Committed never-smoker | 748 | 47.52 | 1,010 | 48.63 | .650 |
| Susceptible never-smoker | 598 | 37.99 | 758 | 36.49 | |
| Highly susceptible never-smoker | 228 | 14.49 | 309 | 14.88 | |
| Missing | 0 | 0 | |||
| Curiosity | |||||
| Definitely not | 816 | 51.84 | 1,117 | 53.78 | .174 |
| Probably not | 402 | 25.54 | 475 | 22.87 | |
| Probably/definitely yes | 356 | 22.62 | 485 | 23.35 | |
Curiosity Among Never Smoking Adolescents
Table 2 describes the baseline curiosity variable by sociodemographics for the 1,574 adolescent never-smokers for whom data were available. Greater levels of curiosity were found among those who were older (χ2 = 3.24, p = .006), male (χ2 = 3.86, p = .02), lived with a smoker (χ2 = 9.23, p = .0002), identified friends who smoked (χ2 = 43.53, p < .0001), reported greater receptivity to tobacco advertising (χ2 = 12.70, p < .0001), and were classified as having a higher susceptibility to smoking (χ2 = 41.29, p < .0001).
Table 2.
Baseline Participant Characteristics by Past Curiosity About Smoking, N = 1,574
| Variable | Definitely not N (%) | Probably not N (%) | Probably/definitely yes N (%) | p value |
|---|---|---|---|---|
| Overall | 816 (51.7%) | 402 (25.4%) | 356 (22.9%) | |
| Age | ||||
| 12 | 288 (59.0%) | 119 (24.0%) | 83 (17.0%) | .0060 |
| 13 | 230 (52.0%) | 112 (25.0%) | 101 (23.0%) | |
| 14 | 165 (47.0% | 105 (30.0%) | 82 (23.0%) | |
| 15 | 133 (46.0%) | 66 (23.0%) | 90 (31.0%) | |
| Missing | 0 | 0 | 0 | |
| Gender | ||||
| Female | 440 (55.0%) | 197 (25.0%) | 156 (20.0%) | .0244 |
| Male | 376 (48.0%) | 205 (26.0%) | 200 (26.0%) | |
| Missing | 0 | 0 | 0 | |
| Race/ethnicity | ||||
| Non-Hispanic White | 513 (52.0%) | 271 (27.0%) | 209 (21.0%) | .1178 |
| Hispanic | 149 (50.0%) | 71 (24.0%) | 79 (26.0%) | |
| Black | 31 (46.0%) | 13 (19.0%) | 23 (34.0%) | |
| Asian/PI | 89 (55.0%) | 38 (23.0%) | 33 (20.0%) | |
| Other | 34 (62.0%) | 9 (16.0%) | 12 (22.0%) | |
| Missing | 0 | 0 | 0 | |
| School performance | ||||
| Average | 212 (48.0%) | 118 (27.0%) | 106 (24.0%) | .4090 |
| Better than average | 308 (49.0%) | 160 (25.0%) | 159 (25.0%) | |
| Much better than average | 285 (57.0%) | 122 (25.0%) | 90 (18.0%) | |
| Missing | 11 (79.0%) | 2 (14.0%) | 1 (7.0%) | |
| Parental smoking | ||||
| No | 608 (55.0%) | 286 (26.0%) | 220 (20.0%) | .0002 |
| Yes | 208 (45.0%) | 116 (25.0%) | 136 (29.0%) | |
| Missing | 0 | 0 | 0 | |
| Peer smoking none | ||||
| Some | 590 (60.0%) | 251 (26.0%) | 135 (14.0%) | <.0001 |
| Missing | 226 (38.0%) | 151 (25.0%) | 221 (37.0%) | |
| Receptivity to tobacco marketing | ||||
| Low | 355 (64.0%) | 115 (21.0%) | 87 (16.0%) | <.0001 |
| Moderate | 371 (48.0%) | 218 (28.0%) | 180 (23.0%) | |
| High | 70 (32.0%) | 64 (29.0%) | 81 (37.0%) | |
| Missing | 20 (61.0%) | 5 (15.0%) | 8 (24.0%) | |
| Original susceptible index | ||||
| Committed never | 528 (70.0%) | 137 (18.0%) | 86 (11.0%) | <.0001 |
| Moderate | 237 (40.0%) | 214 (36.0%) | 144 (24.0%) | |
| High | 51 (22.0%) | 51 (22.0%) | 126 (55.0%) | |
| Missing | 0 | 0 | 0 | |
Curiosity, Susceptibility, and Young Adult Smoking
At baseline, over half (51.7%; n = 816) of adolescents were categorized as definitely not curious, 25.4% as probably not curious, and 22.9% probably/definitely been curious. Of those who were definitely not curious at baseline, significantly fewer were young adult smokers by 2002 compared to those categorized as either probably not curious or as having been curious (9% vs. 18% and 25%, respectively; χ2 = 51.78, df = 2, p < .001).
Using logistic regression, we evaluated how the original susceptibility index and the curiosity question predicted young adult smoking, first in unadjusted models and then in multivariable models adjusting for variables known to potentially predict later smoking behavior (e.g., age, gender, race/ethnicity, school performance, parental smoking, peer smoking, receptivity to tobacco marketing). In unadjusted models, increasing responses on the susceptibility index were associated with an increase in odds of 1.05 (95% CI = 0.71–1.58, p = .79) and 1.94 (95% CI = 2.87–4.25, p < .001) over adolescents classified as committed never-smokers. In unadjusted models, increasing levels of the curiosity index were associated with an increase in odds of 2.19 (95% CI = 1.49–3.21, p < .001) and 3.22 (95% CI = 2.19–4.75, p < .001) over those definitely not curious. When models were adjusted with all examined variables, again, the only level of the susceptibility index that remained a significant predictor of young adult smoking was the highest level (Table 3 and Supplementary Table 1). When compared to committed never-smokers, highly susceptible teens had 2.42 times higher odds of becoming young adult smokers. However, in adjusted models that included the susceptibility index, each increasing level of curiosity remained independently associated with an increase in the odds of young adult smoking. Compared to those who were definitely not curious about smoking, teens who were probably not curious had a 1.90 (95% CI = 1.28–2.81, p < .001) increase in the odds of becoming a young adult smoker and teens who indicated that they were either probably or definitely curious were 2.38 (95% CI = 1.49–3.79) higher. We examined whether the value of curiosity as a risk factor varied across demographic characteristics. No two-way interaction terms of curiosity with age, gender, or ethnic status was significant statistically (F(8,25) = 1.39, p = .25) suggesting a consistent effect of curiosity on risk for established smoking that was independent of the original susceptibility index.
Table 3.
Predictors of Established Smoking by Follow-Up From 1996, 1999, and 2002 Surveys, N = 1,574
| Variable | n | Established % | OR a | 95% CI | p value | AOR b | 95% CI | p value |
|---|---|---|---|---|---|---|---|---|
| Model 1: original susceptible index | ||||||||
| Committed never | 751 | 13% | 1.00 | – | – | 1.00 | – | – |
| Susceptible | 595 | 14% | 1.06 | 0.71–1.57 | .79 | 0.93 | 0.61–1.41 | .746 |
| Highly susceptible | 228 | 32% | 2.87 | 1.94–4.26 | <.001 | 2.42 | 1.64–3.58 | <.001 |
| Model 2: extended susceptibility index | ||||||||
| 0 | 528 | 10% | 1.00 | – | – | 1.00 | – | – |
| 1 | 374 | 10% | 1.25 | 0.78–1.99 | .361 | 1.17 | 0.73–1.87 | .52 |
| 2 | 351 | 19% | 2.23 | 1.38–3.62 | .002 | 2.00 | 1.18–3.42 | .015 |
| 3 | 195 | 21% | 2.23 | 1.38–3.59 | .002 | 1.90 | 1.10–3.26 | .027 |
| 4 | 126 | 39% | 5.42 | 3.18–9.23 | <.001 | 4.51 | 2.50–8.15 | <.001 |
Note. aUnadjusted odds ratio (OR).
bAdjusted odds ratio (AOR) in a model that includes age, gender, race/ethnicity, school performance, household smoking, peer smoking, receptivity to marketing.
Given support for the incremental predictive validity of enhancing the susceptibility index with the curiosity question, we examined the frequency of young adult smoking for each level of curiosity within groups of teens classified as committed never-smokers, susceptible, and highly susceptible to smoking using the original susceptibility index (Figure 1). We did not find support for an interaction between the susceptibility index and levels of curiosity and the set of interaction terms added to the previous multivariable logistic model was not statistically significant (F(4,28) = 0.95, p = .45). This analysis suggests that both the susceptibility index and levels of curiosity provided independent predictive validity and thus may be complementary when assessing the probability of young adult smoking.
Figure 1.
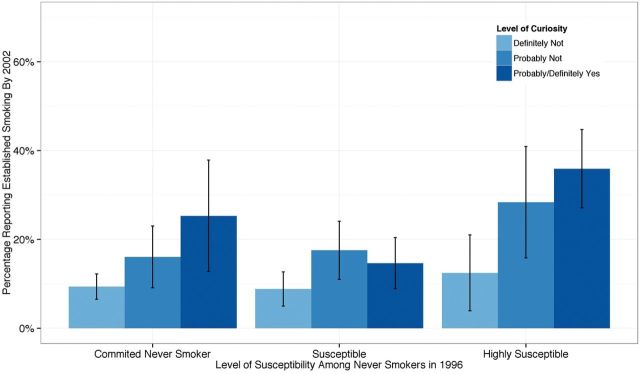
Frequency of reports of adult smoking among committed never-smokers, susceptible, and highly susceptible adolescents with increasing levels of curiosity about smoking. Both susceptibility and curiosity are independently related to adult smoking.
A comparison of the original susceptibility index and the enhanced susceptibility index that included a sum of the three-level susceptibility and three-level curiosity index (scored 0–4) is presented in Table 3 along with the number of teens (unweighted) within levels of each index classified as established smokers at the later surveys. Typically, the susceptibility index is used to make a binary classification of risk and in Table 4, respondents were identified as committed never-smokers with all others being labeled as susceptible. The original index classified almost half (48%) of the 12–15 year old population of California in 1996 as susceptible to smoking and 19% of these became young adult smokers (positive predictive value [PPV]). The sensitivity of this measure (i.e., the identification of those who actually became young adult smokers) was 62% and the specificity (the percent of long term never-smokers identified as committed never-smokers at 12–15 years) was 50%. The enhanced susceptibility index identified two thirds (67%) of this young teenage population as at risk to start smoking and 19% of these became young adult smokers. Thus, the sensitivity of this enhanced measure was 79% (up from 62%) but the specificity was 36% (down from 50%) although the PPV did not change (18.9% vs. 19.0%).
Table 4.
Comparison of Original and Enhanced Susceptibility Indices
| Baseline | % Identified as at risk | Sensitivitya | Specificityb | PPVc |
|---|---|---|---|---|
| Original susceptibility index | 47.7% | 62.2% | 49.6% | 18.9% |
| Enhanced susceptibility index | 66.5% | 78.9% | 35.9% | 19.0% |
Note. aSensitivity: percent of adult smokers identified as “at risk” at age 12–15.
bSpecificity: percent of adult never-smokers identified as “committed never-smokers” at age 12–15 years.
cPositive predictive value (PPV): percent identified as “at risk” who became adult smokers.
Discussion
In this six year follow-up study, adolescents who reported being curious about smoking were much more likely to become young adult smokers. Adding curiosity to the original susceptibility index resulted in one third more adult established smokers (79%) being identified as at risk while they were still never smoking adolescents. However, this desired increase in sensitivity with the enhanced index came at the cost of its specificity, so that there was little change in the low positive predicted value. However, the high sensitivity of the enhanced index does allow opportunities to use these at risk adolescents to develop more effective prevention messages.
A recent paper on favorite advertising for and against cigarettes highlighted this point.40 The identification of favorite antismoking messages varied for teen never-smokers depending on their receptive to tobacco industry advertising, a known influence on susceptibility and curiosity.37 Those who were more likely to have been labeled as at risk by the enhanced index were much less likely to identify health consequences messages as their favorite antismoking messages than those who were more likely to be committed never-smokers. Choosing a message that is highly salient to those with little risk to become a smoker will probably be much less effective in preventing initiation than one that was salient to those who would become smokers. Thus, when developing effective interventions is the goal, it is the sensitivity of the index that is important with little downside if the measure has a lower specificity.
The sensitivity of the enhanced measure was much higher than expected from the earlier paper18 and this may be an artifact of the timing of this study. The baseline measure occurred in 1996 which was the height of expenditures on the Tobacco Industry’s teen marketing campaign that included R.J. Reynolds “Joe Camel” campaign as well as the promotional programs (Marlboro Miles, Camel Cash etc.).22 Both of these are expected to reduce the number of committed never-smokers. The baseline year in this study was also the peak in smoking prevalence among high school seniors.41 The Master Settlement Agreement of 1998 between the State Attorneys’ General and the Tobacco Industry was designed to remove many of the marketing approaches that could impact teens and resulted in a major shift in the Industry’s advertising and promotional expenditures.42 Additionally, many states strengthened their enforcement of sales to minors laws. In California, the combination of these two issues along with the conduct of a comprehensive tobacco control program was associated with a major decline in teen experimentation to smoke from 1996 through 2002.43 Thus, these findings should be replicated in future studies to determine if the enhanced susceptibility measure performs as well in predicting young adult smoking within the context of currently evolving smoking laws and social norms in the United States.
Another limitation of these results is that participants were only followed until young adulthood (age 18–21), when it is known that the window for smoking initiation extends through age 24 years.19 Thus, it is likely that our study will underestimate those who will become adult established smokers. Future studies should replicate these findings in adolescents who are followed further into adulthood.
Although this was a representative sample of Californians, these findings may not be generalizable to the rest of the United States as California has a much lower prevalence than the rest of the country.44 In addition, participants were not enrolled in a longitudinal study, but were separately consented for each follow-up. Loss to follow-up in such studies is related to participant relocation, biasing against those with lower socioeconomic status and from minority population groups who have less stable housing situations. While data were weighted to adjust for this under-representation, this does not completely remove the bias.
Conclusions
The enhanced susceptibility index that includes a measure of curiosity significantly improves identification of teens at risk for becoming young adult smokers. With this increase in sensitivity, the enhanced index will serve as a more comprehensive early warning of future smoking behaviors and could be used to develop more targeted interventions. Future research should examine the enhanced index in distinct environments and population groups. The upcoming longitudinal nationally-representative Population Assessment of Tobacco and Health Study will help to further explore the enhanced susceptibility index and its relevance in today’s complex tobacco landscape.
Supplementary Material
Supplementary Table 1 can be found online at http://www.ntr.oxfordjournals.org
Funding
This work was supported by the California Department of Health Services (contract number 95-23211) and by a grant from the Robert Wood Johnson Foundation (grant number 044244) Funding for this analysis and manuscript preparation has been funded with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the Food and Drug Administration, Department of Health and Human Services. (contract number HHSN271201100027C), and Tobacco Related Disease Research Program (grant numbers 21RT-01335, 21XT-0076). The views and opinions expressed in this article are those of the authors only and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
Declaration of Interests
None declared.
Supplementary Material
References
- 1.Biglan A, Brennan PA, Foster SL, Holder HD. Helping Adolescents At Risk: Prevention of Multiple Problem Behaviors. New York, NY: Guilford Press; 2004. [Google Scholar]
- 2. Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15:355–361. [DOI] [PubMed] [Google Scholar]
- 3. Choi WS, Gilpin EA, Farkas AJ, Pierce JP. Determining the probability of future smoking among adolescents. Addiction. 2001;96:313–323. [DOI] [PubMed] [Google Scholar]
- 4. Gritz ER, Prokhorov AV, Hudmon KS, et al. Predictors of susceptibility to smoking and ever smoking: a longitudinal study in a triethnic sample of adolescents. Nicotine Tob Res. 2003;5:493–506. [DOI] [PubMed] [Google Scholar]
- 5. Jackson C. Cognitive susceptibility to smoking and initiation of smoking during childhood: a longitudinal study. Prev Med. 1998;27:129–134. [DOI] [PubMed] [Google Scholar]
- 6. Unger JB, Johnson CA, Stoddard JL, Nezami E, Chou CP. Identification of adolescents at risk for smoking initiation: validation of a measure of susceptibility. Addict Behav. 1997;22:81–91. [DOI] [PubMed] [Google Scholar]
- 7. Best JA, Flay BR, Towson SMJ, et al. Smoking prevention and the concept of risk. J Appl Soc Psychol. 1984;14:257–273. [Google Scholar]
- 8. Chassin L, Presson CC, Bensenberg M, Corty E, Olshavsky RW, Sherman SJ. Predicting adolescents’ intentions to smoke cigarettes. J Health Soc Behav. 1981;22:445–455. [PubMed] [Google Scholar]
- 9. Pierce JP, Farkas AJ, Evans N, Gilpin EA. An improved surveillance measure for adolescent smoking? Tob Control. 1995;4(suppl 1):9. [Google Scholar]
- 10. Bauman KE, Fisher LA, Bryan ES, Chenoweth RL. Antecedents, subjective expected utility, and behavior: a panel study of adolescent cigarette smoking. Addict Behav. 1984;9:121–136. [DOI] [PubMed] [Google Scholar]
- 11. Leventhal H, Cleary PD. The smoking problem: a review of the research and theory in behavioral risk modification. Psychol Bull. 1980;88:370–405. [DOI] [PubMed] [Google Scholar]
- 12. Cronan TA, Conway TL, Kaszas SL. Starting to smoke in the Navy: when, where and why. Soc Sci Med. 1991;33:1349–1353. [DOI] [PubMed] [Google Scholar]
- 13. Guo Q, Unger JB, Palmer PH, Chou CP, Johnson CA. The role of cognitive attributions for smoking in subsequent smoking progression and regression among adolescents in China. Addict Behav. 2013;38:1493–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Opdal P. Curiosity, wonder and education seen as perspective development. Stud Philos Educ. 2001;20:13. [Google Scholar]
- 15. Loewenstein G. The psychology of curiosity: a review and reinterpretation. Psychol Bull. 1994;116:23. [Google Scholar]
- 16. Ray ML. Advertising and Communication Management. Englewood Cliffs, NJ: Prentice Hall; 1982. [Google Scholar]
- 17. Smith RE, Swinyard WR. Cognitive responses to advertising and trial: belief strength, belief confidence and product curiosity. J Advertising. 1988;17:3–14. [Google Scholar]
- 18.Nodora J, Hartman SJ, Strong DR, et al. Curiosity predicts smoking experimentation independent of susceptibility in a US national sample. Addict Behav 2014;39:1696–1700. doi:10.1016/j.addbeh.2014.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Surgeon-General’s report. 2012.
- 20. Pierce JP, Berry CC, Gilpin EA, Rosbrook B, White MM. Technical Report on Analytic Methods and Approaches Used in the 1996 California Tobacco Survey Analysis. Vol 1: Data Collection Methodology. La Jolla, CA: Unviersity of California, San Diego; 1998. http://libraries.ucsd.edu/locations/sshl/data-gov-info-gis/ssds/guides/tobacco-surveys.html. Accessed March 15, 2013. [Google Scholar]
- 21. Pierce JP, Berry CC, Gilpin EA, Rosbrook B, White MM. Technical Report on Analytic Methods and Approaches Used in the 1996 California Tobacco Survey Analysis. Vol 2: Statistical Methodology, Public Use Data File Documentation, Individual Item Responses. La Jolla, CA: Unviersity of California, San Diego; 1998. http://libraries.ucsd.edu/locations/sshl/data-gov-info-gis/ssds/guides/tobacco-surveys.html. Accessed March 15, 2013. [Google Scholar]
- 22. Gilpin EA, White MM, Messer K, Pierce JP. Receptivity to tobacco advertising and promotions among young adolescents as a predictor of established smoking in young adulthood. Am J Public Health. 2007;97:1489–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Efron B. The Jacknife, the Bootstrap and Other Resampling Plans. Philadelphia, PA: Society for Industrial and Applied Mathematics; 1982. [Google Scholar]
- 24. Dornbusch SM, Ritter PL, Leiderman PH, Roberts DF, Fraleigh MJ. The relation of parenting style to adolescent school performance. Child Dev. 1987;58:1244–1257. [DOI] [PubMed] [Google Scholar]
- 25. Morin AJ, Rodriguez D, Fallu JS, Maïano C, Janosz M. Academic achievement and smoking initiation in adolescence: a general growth mixture analysis. Addiction. 2012;107:819–828. [DOI] [PubMed] [Google Scholar]
- 26. Steinberg L, Lamborn SD, Dornbusch SM, Darling N. Impact of parenting practices on adolescent achievement: authoritative parenting, school involvement, and encouragement to succeed. Child Dev. 1992;63:1266–1281. [DOI] [PubMed] [Google Scholar]
- 27. Cox RG, Zhang L, Johnson WD, Bender DR. Academic performance and substance use: findings from a state survey of public high school students. J Sch Health. 2007;77:109–115. [DOI] [PubMed] [Google Scholar]
- 28. Diego MA, Field TM, Sanders CE. Academic performance, popularity, and depression predict adolescent substance use. Adolescence. 2003;38:35–42. [PubMed] [Google Scholar]
- 29. Tucker JS, Ellickson PL, Klein DJ. Growing up in a permissive household: what deters at-risk adolescents from heavy drinking? J Stud Alcohol Drugs. 2008;69:528–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hu FB, Flay BR, Hedeker D, Siddiqui O, Day LE. The influences of friends’ and parental smoking on adolescent smoking behavior: the effects of time and prior smoking. J Appl Soc Psychol. 1995;25:2018–2047. [Google Scholar]
- 31. Killen JD, Robinson TN, Haydel KF, et al. Prospective study of risk factors for the initiation of cigarette smoking. J Consult Clin Psychol. 1997;65:1011–1016. [DOI] [PubMed] [Google Scholar]
- 32. Urberg KA, Değirmencioğlu SM, Pilgrim C. Close friend and group influence on adolescent cigarette smoking and alcohol use. Dev Psychol. 1997;33:834–844. [DOI] [PubMed] [Google Scholar]
- 33. Pierce JP, Distefan JM, Jackson C, White MM, Gilpin EA. Does tobacco marketing undermine the influence of recommended parenting in discouraging adolescents from smoking? Am J Prev Med. 2002;23:73–81. [DOI] [PubMed] [Google Scholar]
- 34. Gilpin EA, Emery S, Farkas A, Distefan JM, White MM, Pierce JP. The California Tobacco Control Program: A Decade of Progress. Results from the California Tobacco Survey, 1990–1999. La Jolla, CA: Univeristy of California, San Diego; 2001. http://libraries.ucsd.edu/locations/sshl/data-gov-info-gis/ssds/guides/tobacco-surveys.html Accessed March 15, 2013. [Google Scholar]
- 35. U. S. Department of Health Human Services. Guidelines for school health programs to prevent tobacco use and addiction. MMWR. 1994;43:1–18. [PubMed] [Google Scholar]
- 36. Gilpin EA, Pierce JP, Farkas AJ. Duration of smoking abstinence and success in quitting. J Natl Cancer Inst. 1997;89:572–576. [DOI] [PubMed] [Google Scholar]
- 37. Pierce JP, Distefan JM, Kaplan RM, Gilpin EA. The role of curiosity in smoking initiation. Addict Behav. 2005;30:685–696. [DOI] [PubMed] [Google Scholar]
- 38.Lumley T. (2012). Survey: Analysis of Complex Survey Samples. R package version 2.15. [Google Scholar]
- 39. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. http://www.R-project.org. Accessed March 15, 2013. [Google Scholar]
- 40.Emory KT, Messer K, Vera L, et al. Receptivity to cigarette and tobacco control messages and adolescent smoking initiation. Tob Control. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Johnson LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Drug Use: 2012 Overview, Key Findings on Adolescent Drug Use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2013. http://www.monitoringthefuture.org/pubs.html Accessed March 15, 2013. [Google Scholar]
- 42. Pierce JP, Distefan JM. Adolescent Smoking. Tobacco and Public Health: Science and Policy. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- 43.Messer K, Pierce JP. Changes in age trajectories of smoking experimentation during the California Tobacco Control Program. Am J Pub Health. 2010;100:1298–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pierce JP, Messer K, White MM, Kealey S, Cowling DW. Forty years of faster decline in cigarette smoking in California explains current lower lung cancer rates. Cancer Epidemiol Biomarkers Prev. 2010; 19:2801–2810. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


