Abstract
Background and Aims:
Sudden, profound hypotension and bradycardia events (HBEs) have been reported in more than 20% of patients undergoing shoulder arthroscopy in the sitting position. The present study was designed to know whether intravenous (IV) ondansetron (selective 5-hydroxy tryptamine 3-antagonist) can help in reducing the HBEs associated with shoulder arthroscopy performed in sitting position under interscalene brachial plexus block (ISBPB).
Methods:
A total of 100 patients (age 20–50 years) undergoing shoulder arthroscopy performed in the sitting position under ISBPB were assigned randomly to one of the two groups: Group C received 10 ml of normal saline and Group T received 4 mg of ondansetron diluted in 10 ml of normal saline` IV. All patients received ISBPB using levobupivacaine 0.5%. Assessment of motor and sensory blockade, pulse rate, systolic blood pressure, respiration, and side effects were noted every 5 min for first 30 min and every 10 min till the end of surgery. HBEs were recorded in both groups.
Results:
IV injection of ondansetron significantly reduces the incidence of HBEs from 11 (22.44% in Group C) to 3 (6.1% in Group T). The duration of analgesia was significantly longer in Group C (8.1 ± 3.3) in comparison with Group T (6.3 ± 4.2 h).
Conclusion:
We conclude that 4 ml of IV ondansetron can significantly reduce the HBEs during shoulder arthroscopy done in the sitting position under ISBPB.
Keywords: Arthroscopy, bradycardia, hypotension, interscalene brachial block, intravenous ondansetron, sitting position
INTRODUCTION
Shoulder arthroscopy can be performed in either lateral decubitus or sitting position. Although surgeon has a preference for patient positioning, the sitting position has several advantages including the ease of setup, excellent intra-articular visualisation for all types of arthroscopic shoulder procedures, less intra-operative blood loss, a lower incidence of traction neuropathy, and ease of conversion to the open approach if needed.[1] In addition, positioning during shoulder arthroscopy may affect the type of anaesthesia used. Surgeons who prefer the sitting position cite the ability to use general or interscalene brachial plexus block (ISBPB) as an advantage. ISBPB is possible for patients in the sitting position; however, it is poorly tolerated in patients in the lateral decubitus position.
Interscalene brachial plexus block provides effective anaesthesia for most types of shoulder surgeries, including arthroplasty and fracture fixation. When administered by an anaesthesiologist committed to and skilled in the technique, the block has an excellent rate of success and is associated with a relatively low complication rate.[2]
Interscalene brachial plexus block has several advantages for patients undergoing shoulder surgery: Excellent anaesthesia, reduction in both intra-operative and post-operative doses of opiates, delay in the onset of post-operative pain, a shortened post-anaesthesia stay, and increased patient satisfaction.[3] One of the major disadvantages of the sitting position is cardiovascular instability during the shoulder procedure.[4] Sudden, profound hypotension and bradycardia events (HBEs) have been reported in more than 20% of patients undergoing shoulder arthroscopy in the sitting position.[5]
These HBEs may be a form of vasovagal syncope mediated by the Bezold–Jarisch reflex (BJR), which happens when venous pooling and increased sympathetic tone cause a low volume, hyper contractile ventricle.[6] This leads to sudden activation of the parasympathetic nervous system and sympathetic withdrawal, causing bradycardia and hypotension.
Animal studies reported that serotonin (5-hydroxy tryptamine 3 [5-HT3]), may be an important contributing factor to the occurrence of BJR in the settings of decreased blood volume, which can be blocked by antagonising the serotonin at the level of the receptors.[7] One previous study also reported that intravenous (IV) ondansetron attenuated the spinal induced hypotension that might be caused by BJR.[8]
The present work is a prospective, randomised study, which attempts to assess if blocking of the serotonin receptors by ondansetron (a selective 5-HT3 receptor antagonist) can help in reducing the HBEs associated with shoulder arthroscopy done in the sitting position under ISBPB.
METHODS
After obtaining Institutional Review Board approval and informed, written consent, 100 American Society of Anesthesiologists’ (ASA) physical status I or II, age of 20–50 years patients who were undergoing shoulder arthroscopy in the sitting position under ISBPB were studied. Sample size calculation was done based on a previous study in which the incidence of HBEs in control group and study group were 24% and 6%, respectively.[9] It was estimated that a minimum of 50 patients in each group would be required to have a 90% power of detecting a 50% difference in the HBEs with 95% confidence interval.
Patients with a history of coronary artery disease, cardiac conduction defects, uncontrolled diabetes and hypertension, asthma, and those receiving clonidine, beta-blocker or calcium channel-blocker therapy were excluded from the study. Patients underwent surgery for a variety of indications including rotator cuff repair, acromioplasty, and labral repair. Patients were randomised using a computer generated random number list. Patients were assigned randomly to one of the two groups. One hundred patients were randomly assigned to one of the two equal groups to receive either of the following: Group C: 10 ml normal saline. Group T: 4 mg ondansetron diluted in 10 ml normal saline. All patients received test drug IV over a period of 5 min before starting ISBPB.
All patients received ISBPB using levobupivacaine 0.5%. A total volume of 35 ml of local anaesthetic was selected to provide the highest rate of success of interscalene block administered using the nerve stimulation technique. After establishing IV access, non-invasive monitoring of blood pressure (BP), oxygen saturation, and electrocardiogram (ECG) were applied to all patients and their baseline vital signs were measured. All patients received supplemental oxygen provided via nasal cannula at 2 L/min. Sedation was provided by IV administration of midazolam 1 mg and fentanyl 30 μg before the block. A nerve stimulation technique with a Stimuplex© needle and a stimulator were used. After the proper location of the nerve, the local anaesthetic solution was injected in incremental 5 ml boluses with intermittent aspiration.
All ISBPB were performed by one anaesthesiologist, and all surgeries were performed by the same group of surgeons. After the ISBPB, non-invasive BP was measured every 5 min with more frequent measurements if needed, and continuous ECG monitoring. Then the patients were placed in the sitting or ‘beach chair’ position, which was achieved by elevating the back of the operating table to 60°–80° and flexing both the knees and hips to 90° with the patients’ feet resting properly on a footboard.
Sensory blockade was evaluated every 5 min by pinprick test and the motor block was tested by asking the patient to raise his arm, to abduct/adduct the thumb, and to flex the forearm on the arm. Intra-operatively, midazolam boluses of 0.02 mg/kg and fentanyl 1 μg/kg boluses were given if the patient complained of pain. The amount of midazolam and fentanyl administered and the degree of sedation were recorded (sedation score: 1 = awake, 2 = awake but sedated, 3 = asleep but responsive to verbal stimuli, and 4 = asleep but responsive to tactile stimuli). All patients were pre-loaded with 500 ml of crystalloid. Heart rate and BP were recorded by an anaesthesiologist blinded to the study drugs.
A HBE was defined as; heart rate decrease of more than 30 bpm in <5 min or any decrease <50 bpm, and/or a systolic BP decrease more than 30 mmHg in <5 min or any decrease to <90 mmHg.[10] A HBE was managed by IV injection of atropine (0.6 mg boluses) or ephedrine (6 mg boluses). Each patient was observed for side effects such as Horner's syndrome (HS), ipsilateral diaphragmatic paralysis, hoarseness of voice, difficulty in swallowing and complications such as pneumothorax, vascular injury (external jugular vein puncture, haematoma formation, intra-arterial injection), epidural or spinal injection, neuropathy/nerve injury.
After the recovery, the pain was tested and recorded by using the verbal numerical rating scale (VNRS: 0 = no pain, 10 = most severe pain imaginable); starting immediately on arrival to the recovery room as 0 h and 1, 3, 6, and 12 h later. When the VNRS was more than 3, IV pethidine 0.5 mg/kg was injected and recorded. Any complications as neurological disabilities, nausea, vomiting or respiratory difficulties were also recorded.
Data were checked, entered, and analysed by using SPSS for Windows version 19 (Armonk, NY: IBM Corp). Data are expressed as mean ± standard deviation for quantitative variables, number, and percentage for categorical variables. Students ‘t’ test and Chi-square (χ2) test used for comparison in between groups. P < 0.05 was considered statistically significant.
RESULTS
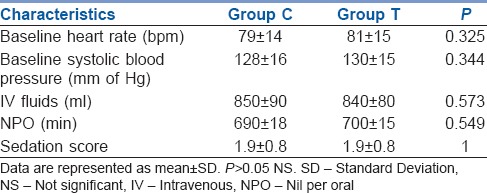
Two patients were excluded from the study due to block failure; one of them was randomised to Group C and the second one was randomised to Group T. The demographic data and surgical characteristics were comparable in both groups [Tables 1 and 2]. The mean age in Group C (33.88 ± 9.39 years) was very much comparable to the mean age in Group T (34.28 ± 8.8 years) (P > 0.05). Side of surgery in both the groups was comparable and non-significant for statistical analysis. To summate, all the demographic characteristics such as age, weight, ASA grade, and side of the shoulder operated were comparable in both the groups and were found to be statistically non-significant (P > 0.05) [Table 1]. Baseline heart rate, BP was comparable in both groups [Table 2]. There was no difference in sedation score, nil per oral status and IV fluids in both the groups; P > 0.05, and statistically not significant [Table 2].
Table 1.
Demographic data
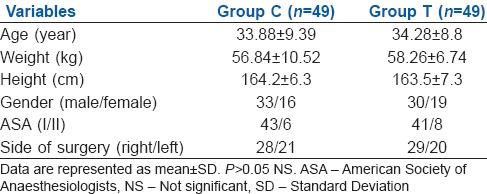
Table 2.
Characteristics of groups
There were no signs and symptoms suggestive of spinal, epidural or stellate ganglion blockade or intra-vascular injection in two groups.
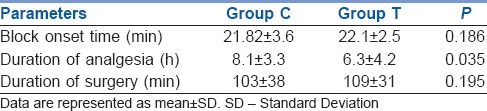
Hypotension and bradycardia events occurred in three patients in Group T (6.1%), and 11 patients in Group C (22.44%) which was significantly higher than in Group C; P - 0.030 [Table 3]. The onset of these HBEs was comparable in the two groups [Table 3]. There was no significant difference in the block onset time in the two groups; (21.82 ± 3.6 min), and (22.1 ± 2.5 min) in Groups C and T, respectively; P - 0.186 [Table 4]. The duration of analgesia was significantly longer in Group C (8.1 ± 3.3 h) in comparison with Group T (6.3 ± 4.2 h); P - 0.035 [Table 4].
Table 3.
Details of Hypotension Bradycardia Events
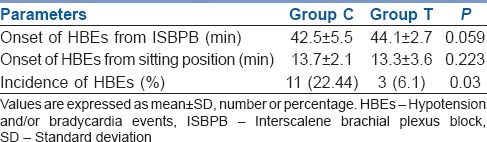
Table 4.
Intra-operative data
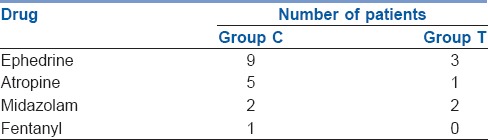
Nine patients in Group C received ephedrine to treat hypotension, which was significantly higher compared to the other group (three patients in Group T) [Table 5]. One patient in Group T and five patients in Group C needed atropine to treat bradycardia [Table 5]. There was no significant difference in the use of intra-operative midazolam or fentanyl [Table 5].
Table 5.
Intra-operative drugs
DISCUSSION
The study was conducted with the aim to test the hypothesis that IV ondansetron would reduce the incidence of HBEs in arthroscopic shoulder surgery in the sitting position after ISBPB. Activation of the BJR is considered one of the proposed mechanisms for the occurrence of HBEs.[6,11] The BJR is an inhibitory reflex that originates in the cardiac sensory receptors with vagal afferents, which are affected by chemical and mechanical stimuli.[12] This reaction may be related to venous pooling (caused by the sitting position and epinephrine-induced beta 2-adrenergic effect) and increased inotropy (alfa-adrenergic effect of epinephrine). Increase in epinephrine levels may result from decreased venous return and carotid baroreceptor stimulation, as well as exogenously from epinephrine administered with the local anaesthetic or in the irrigating solution. A low-volume hypercontractile ventricle causes stimulation of intra-myocardial mechanoreceptors (C fibres), which is followed, in susceptible patients, by an abrupt withdrawal of sympathetic outflow and an increase in vagal tone with resultant bradycardia and hypotension were observed in this setting.
Hypovolaemia not only causes stimulation of cardiac mechanoreceptors in the left ventricle that triggers the BJR and causes reflex bradycardia, vasodilatation and hypotension, but also results in the activation of thrombocytes to release serotonin which triggers chemoreceptors in the wall of the heart.[11,13] Furthermore, stimulation of 5-HT3 receptors, which are G protein-coupled, ligand-gated, fast-ion channels, increases the activity of the vagal nerve.[14]
One previous study in anaesthetised rats reported that BJR induced by serotonin participates in systemic hypotension and bradycardia.[15] This means that BJR can also be directly triggered by the activation of the serotonin 5-HT3 receptors.
Based on these studies, we assumed that preventing the effect of serotonin by blocking 5-HT3 receptors by IV ondansetron can help in reducing the incidence of the HBEs associated with shoulder arthroscopy done in the sitting position under ISBPB.
Our results demonstrated that IV injection of ondansetron 4 mg significantly reduced the incidence of HBEs in our patients from 22.44% in the saline group (Group C) to 6.1% after injection of 4 mg ondansetron (Group T). This 22.44% incidence of HBEs in the saline group is consistent with the previous reports of such events. Many studies show the incidence of 21–27.7% HBEs in the placebo group.[16] The reduction in HBEs in our study after IV ondansetron is similar to a previous study done in rabbits, in which IV administration of granisetron 50 μg/kg was efficacious in reducing bradycardia and hypotension associated with BJR.[17]
In one more study, it was found that granisetron injection reduced the heart rate fluctuation and hypotension during head-up tilt table tests that are likely related to BJR.[18] And this is consistent with Matrinek who concluded that injection of 4 mg ondansetron IV with atropine 0.6 mg could revert asystole during spinal anaesthesia and also with Owczuk et al. who found that 8 mg ondansetron reduced the incidence of bradycardia and hypotension after spinal anaesthesia.[7,8]
The combination of the sitting position, regional anaesthetic technique, an awake patient, and surgical procedure may precipitate vasovagal episodes, which if anticipated are of minor significance, but which in the extreme may lead to cardiac arrest. There are many possible causes of the observed symptomatology. IV uptake of local anaesthetic can be considered, but time from block placement to the onset of symptoms was 42.5 ± 5.5 min and 44.1 ± 2.7 min in Group C and in Group T, respectively. This is significantly longer than that which would be expected for peak local anaesthetic uptake from an interscalene brachial (ISB) which is approximately 30 min for bupivacaine and <20 min for lidocaine with or without epinephrine. Roth et al., using mepivacaine 10 mg/kg and Tetzlaff et al., using the same dose of alkalinised mepivacaine for ISB reported no episodes of toxicity. The central nervous system symptoms of lightheadedness and nausea were unlike those of local anaesthetic toxicity and promptly resolved after the administration of atropine, glycopyrrolate or ephedrine. Extensive spread of local anaesthetic to the epidural or subarachnoid space may cause cardiovascular and respiratory compromise but is rare. None of the patients experienced bilateral HS, contralateral arm weakness, or apnoea.[19]
Previous studies reported interval between positioning and haemodynamic changes ranging between 12 and 24 min but may be delayed to 1 h.[20,21] Our patients had similar sequence of events to those undergoing tilt-table testing and the onset of symptoms was (13.7 ± 2.1 min), (13.3 ± 3.6 min), in Groups C and T, respectively.
Although the onset of analgesia was similar in all groups, the duration of analgesia was shorter in Group T in comparison with Group C. This can be explained by antagonising the effect of serotonin in controlling pain. Although potential mechanisms of this observation were not clear, but animal studies have clarified the anti-nociceptive mechanisms of the descending serotoninergic system at the level of the spinal cord. It hyperpolarises the membrane of substantia gelatinosa neurons, inhibits the excitatory transmitter glutamate release of A-delta and C afferent fibres pre-synaptically and increases the inhibitory transmitters release including aminobutyric acid and glycine from the interneurons.[22]
The shortened duration of analgesia observed in our study is consistent with Fassoulaki et al. who reported that IV ondansetron leads to a faster regression of the sensory block after spinal anaesthesia with lidocaine.[23] Furthermore, continuous IV administration of ondansetron decreased the analgesic potency of tramadol infusion for post-operative pain.[24]
CONCLUSION
The combination of sitting position, ISBPB, and surgical procedure may result in HBEs, usually of minor significance if anticipated. In extreme cases, it can lead to profound hypotension and bradycardia. We conclude that IV ondansetron 4 mg can reduce the HBEs during shoulder arthroscopy in the sitting position under ISBPB.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Peruto CM, Ciccotti MG, Cohen SB. Shoulder arthroscopy positioning: Lateral decubitus versus beach chair. Arthroscopy. 2009;25:891–6. doi: 10.1016/j.arthro.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Gelber PE, Reina F, Caceres E, Monllau JC. A comparison of risk between the lateral decubitus and the beach-chair position when establishing an anteroinferior shoulder portal: A cadaveric study. Arthroscopy. 2007;23:522–8. doi: 10.1016/j.arthro.2006.12.034. [DOI] [PubMed] [Google Scholar]
- 3.Fredrickson MJ, Ball CM, Dalgleish AJ. Analgesic effectiveness of a continuous versus single-injection interscalene block for minor arthroscopic shoulder surgery. Reg Anesth Pain Med. 2010;35:28–33. doi: 10.1097/AAP.0b013e3181c771bd. [DOI] [PubMed] [Google Scholar]
- 4.Brull R, McCartney CJ, Sawyer RJ, von Schroeder HP. The indications and applications of interscalene brachial plexus block for surgery about the shoulder. Acute Pain. 2004;6:57–77. [Google Scholar]
- 5.Kahn RL, Hargett MJ. Beta-adrenergic blockers and vasovagal episodes during shoulder surgery in the sitting position under interscalene block. Anesth Analg. 1999;88:378–81. [PubMed] [Google Scholar]
- 6.Sia S, Sarro F, Lepri A, Bartoli M. The effect of exogenous epinephrine on the incidence of hypotensive/bradycardic events during shoulder surgery in the sitting position during interscalene block. Anesth Analg. 2003;97:583–8. doi: 10.1213/01.ANE.0000070232.06352.48. [DOI] [PubMed] [Google Scholar]
- 7.Martinek RM. Witnessed asystole during spinal anesthesia treated with atropine and ondansetron: A case report. Can J Anaesth. 2004;51:226–30. doi: 10.1007/BF03019100. [DOI] [PubMed] [Google Scholar]
- 8.Owczuk R, Wenski W, Polak-Krzeminska A, Twardowski P, Arszulowicz R, Dylczyk-Sommer A, et al. Ondansetron given intravenously attenuates arterial blood pressure drop due to spinal anesthesia: A double-blind, placebo-controlled study. Reg Anesth Pain Med. 2008;33:332–9. doi: 10.1016/j.rapm.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Roch J, Sharrock NE. Hypotension during shoulder arthroscopy in the sitting position under interscalene block. Reg Anesth. 1991;15(Suppl):64. [Google Scholar]
- 10.Liguori GA, Kahn RL, Gordon J, Gordon MA, Urban MK. The use of metoprolol and glycopyrrolate to prevent hypotensive/bradycardic events during shoulder arthroscopy in the sitting position under interscalene block. Anesth Analg. 1998;87:1320–5. doi: 10.1097/00000539-199812000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: Relationship to vasovagal syncope and the Bezold-Jarisch reflex. Br J Anaesth. 2001;86:859–68. doi: 10.1093/bja/86.6.859. [DOI] [PubMed] [Google Scholar]
- 12.Campagna JA, Carter C. Clinical relevance of the Bezold-Jarisch reflex. Anesthesiology. 2003;98:1250–60. doi: 10.1097/00000542-200305000-00030. [DOI] [PubMed] [Google Scholar]
- 13.Seo KC, Park JS, Roh WS. Factors contributing to episodes of bradycardia hypotension during shoulder arthroscopic surgery in the sitting position after interscalene block. Korean J Anesthesiol. 2010;58:38–44. doi: 10.4097/kjae.2010.58.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aviado DM, Aviado GD. The Bezold-Jarisch reflex. A historical perspective of cardiopulmonary reflexes. AnnNY Acad Sci. 2001;940:48–58. [PubMed] [Google Scholar]
- 15.Yamano M, Kamato T, Nishida A. Serotonin (5-HT) 3-receptor antagonism of 4, 5, 6, 7-tetrahydrobenzimidazole derivatives against 5-HT - Induced bradycardia in anaesthetized rats. Jpn J Anaesth. 2003;47:178–80. doi: 10.1254/jjp.65.241. [DOI] [PubMed] [Google Scholar]
- 16.D’Alessio JG, Weller RS, Rosenblum M. Activation of the Bezold-Jarisch reflex in the sitting position for shoulder arthroscopy using interscalene block. Anesth Analg. 1995;80:1158–62. doi: 10.1097/00000539-199506000-00016. [DOI] [PubMed] [Google Scholar]
- 17.White CM, Chow MS, Fan C, Kluger J, Bazunga M. Efficacy of intravenous granisetron in suppressing the bradycardia and hypotension associated with a rabbit model of the Bezold-Jarisch reflex. J Clin Pharmacol. 1998;38:172–7. doi: 10.1002/j.1552-4604.1998.tb04407.x. [DOI] [PubMed] [Google Scholar]
- 18.Tsikouris JP, Kluger J, Chow MS, White CM. Usefulness of intravenous granisetron for prevention of neurally mediated hypotension upon head upright tilt testing. Am J Cardiol. 2000;85:1262–4. doi: 10.1016/s0002-9149(00)00743-8. [DOI] [PubMed] [Google Scholar]
- 19.Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone J, et al. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am. 2005;87:974–9. doi: 10.2106/JBJS.D.02003. [DOI] [PubMed] [Google Scholar]
- 20.Kwak HJ, Lee JS, Lee DC, Kim HS, Kim JY. The effect of a sequential compression device on hemodynamics in arthroscopic shoulder surgery using beach-chair position. Arthroscopy. 2010;26:729–33. doi: 10.1016/j.arthro.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Grubb BP. Clinical practice. Neurocardiogenic syncope. N Engl J Med. 2005;352:1004–10. doi: 10.1056/NEJMcp042601. [DOI] [PubMed] [Google Scholar]
- 22.Yoshimura M, Furue H. Mechanisms for the anti-nociceptive actions of the descending noradrenergic and serotonergic systems in the spinal cord. J Pharmacol Sci. 2006;101:107–17. doi: 10.1254/jphs.crj06008x. [DOI] [PubMed] [Google Scholar]
- 23.Fassoulaki A, Melemeni A, Zotou M, Sarantopoulos C. Systemic ondansetron antagonizes the sensory block produced by intrathecal lidocaine. Anesth Analg. 2005;100:1817–21. doi: 10.1213/01.ANE.0000152616.57107.F6. [DOI] [PubMed] [Google Scholar]
- 24.Arcioni R, della Rocca M, Romanò S, Romano R, Pietropaoli P, Gasparetto A. Ondansetron inhibits the analgesic effects of tramadol: A possible 5-HT(3) spinal receptor involvement in acute pain in humans. Anesth Analg. 2002;94:1553–7. doi: 10.1097/00000539-200206000-00033. [DOI] [PubMed] [Google Scholar]


