Summary
Background
In January, 2014, the Same-Sex Marriage Prohibition Act was signed into law in Nigeria, further criminalising same-sex sexual relationships. We aimed to assess the immediate effect of this prohibition act on stigma, discrimination, and engagement in HIV prevention and treatment services in men who have sex with men (MSM) in Nigeria.
Methods
The TRUST cohort study uses respondent-driven sampling to assess the feasibility and effectiveness of engagement of MSM in HIV prevention and treatment services at a clinical site located with a community-based organisation trusted by the MSM community. TRUST is a prospective implementation research cohort of MSM (≥16 years) in Abuja, Nigeria. We compared HIV clinical outcomes and stigma, including fear and avoidance of health care, across baseline and quarterly visits before and after implementation of the the Same-Sex Marriage Prohibition Act. Outcomes assessed were measures of stigma and discrimination, loss to follow-up, antiretroviral therapy status, and viral load. We compared outcomes before and after the legislation with χ2 statistics, and estimated incident stigma-related events and loss to follow-up with Poisson regression.
Findings
Between March 19, 2013, and Aug 7, 2014, 707 MSM participated in baseline study procedures, contributing to 756 before legislation (prelaw) and 420 after legislation (postlaw) visits. Reported history of fear of seeking health care was significantly higher in postlaw visits than in prelaw visits (n=161 [38%] vs n=187 [25%]; p<0.0001), as was avoidance of health care (n=118 [28%] vs n=151 [20%]; p=0.001). In incidence analyses, of 192 MSM with follow-up data and no history of an event at baseline, reported fear of seeking health care was higher in the postlaw than the prelaw period (n=144; incidence rate ratio 2.57, 95% CI 1.29–5.10; p=0.007); loss to follow-up and incident healthcare avoidance were similar across periods. Of the 161 (89%) of 181 HIV-infected MSM with HIV viral loads available, those who had disclosed sexual behaviour with a health-care provider were more often virally suppressed at baseline than those with no previous disclosure (18 [29%] of 62 vs 13 [13%] of 99 men; p=0.013).
Interpretation
These analyses represent individual-level, quantitative, real-time prospective data for the health-related effects resulting from the enactment of legislation further criminalising same-sex practices. The negative effects of HIV treatment and care in MSM reinforce the unintended consequences of such legislation on global goals of HIV eradication. Strategies to reach MSM less likely to engage in HIV testing and care in highly stigmatised environments are needed to reduce time to HIV diagnosis and treatment.
Funding
National Institutes of Health.
Introduction
Worldwide, gay men and other men who have sex with men (MSM) are disproportionately affected by HIV.1,2 In the past few years, data have shown that HIV disparities between MSM and other men observed in the USA and Europe since the start of the pandemic are also present in low-income and middle-income settings.3 In sub-Saharan Africa, HIV prevalence is four times greater in MSM than in other men.1,3 These health inequities have raised awareness among community groups, donors, public health practitioners, researchers, and national AIDS programmes of the urgent need to improve HIV prevention and treatment services for MSM across the continent.4–6 However, alongside increased attention to the needs of MSM is a growing social and political pushback to sexual and gender minority rights in many low-income and middle-income countries.
MSM across many countries in sub-Saharan Africa face stigma and discrimination, and anti-sodomy laws date back to the colonial era.7–10 Targeted hate crimes and new legislation criminalising same-sex practices in several countries continue to undermine the human rights of lesbian, gay, bisexual, and transgender (LGBT) individuals.7 Policies further criminalising same-sex practices or the community groups addressing the health-related needs of these populations might further restrict coverage of HIV prevention, treatment, and care programmes.11–14
In Nigeria, the Same-Sex Marriage Prohibition Act was passed by the Senate in 2011, and then by the House of Representatives in July, 2013.15 The bill was signed into law on Jan 7, 2014.16 Before this legislation, consensual sex between male same-sex couples was already prohibited in Nigeria under anti-sodomy laws enacted in the colonial era, and same-sex marriages were not legally recognised.17 The new law further criminalised same-sex practices, including prohibiting participation in organisations, service provision, or meetings that support gay people, and punishes attempts to enter civil unions or publicly show same-sex amorous relationships.18
Although an environment hostile to the rights of the LGBT community existed before enactment of new legislation, the public announcement of the Same-Sex Marriage Prohibition Act in Nigeria was followed by multiple arrests and reports of torture.19,20 Acts of violence against gay men and other MSM have also been reported in other countries with policies against same-sex intimate behaviours and might result in fear of accessing health services.7 However, few non-ecological data are available, and no prospective data exist assessing the effect of legislation against homosexuality on health outcomes. Furthermore, in Nigeria and other countries criminalizing same-sex relationships, investments in HIV/AIDS funding for programmes intended to reach MSM have been scarce.21 We did this study to assess the immediate effect on stigma, discrimination, and engagement in HIV prevention and treatment services in MSM prospectively followed up before and after the passing of the Same-Sex Marriage Prohibition Act in Nigeria.
Methods
Study design and participants
MSM in Abuja, Nigeria, were recruited into the TRUST cohort study with respondent-driven sampling. The purpose of the TRUST study is to assess the feasibility and effectiveness of engagement of MSM from Abuja into HIV prevention and treatment services at a clinical site located with a community-based organisation trusted by the MSM community (the TRUST model). Respondent-driven sampling uses peer referral methods to recruit and enrol eligible study participants and has been previously described.22 Briefly, participants termed seeds were purposively selected to ensure that over time various MSM community networks were reached, including MSM of different ages, marital statuses, and religions. After completion of study procedures, seeds were given three coupons to invite other eligible friends to participate, who upon study completion also received three coupons to invite their peers. Eligible individuals were 16 years or older; assigned male sex at birth; had engaged in insertive or receptive anal sex with a man in the past 12 months; spoke English or Hausa; presented with a valid study coupon; and were willing to be followed up for 18 months, including regular HIV testing and clinical monitoring.
Enrolment into the cohort began in March, 2013, and remains open as of June, 2015. At baseline, individuals presenting with a coupon were screened and asked to provide informed consent. Those agreeing to participate completed a behavioural questionnaire at the baseline visit (visit 0) and returned within 2 weeks to complete HIV counselling and testing, testing for sexually transmitted infections (STIs), and clinical and laboratory examination (visit 1). Quarterly visits were scheduled after the baseline visit and included a condensed behavioural questionnaire in addition to HIV counselling and testing or HIV treatment monitoring and STI testing. All MSM living with HIV were offered antiretroviral treatment (ART) independent of CD4 cell count.
The Same-Sex Marriage Prohibition Act was publicly announced as law on Jan 13, 2014, midway through study enrolment and data collection. Distribution of recruitment coupons was temporarily halted on Jan 21, 2014, and efforts were made to reinforce safety of the clinic facility and study records. Follow-up of enrolled participants continued during this period and institutional review board-approved recruitment recommenced on Feb 3, 2014. Because the policy change was not anticipated, these analyses were not planned a priori, but are a secondary analysis of data obtained before and after the law was put into effect.
All study participants provided written informed consent. This study was done in collaboration with the Institute of Human Virology at the University of Maryland, the Institute of Human Virology Nigeria, Johns Hopkins University, the International Center for Advocacy on the Right to Health, and the US. Military HIV Research Program. The study was approved by the Federal Capital Territory Health Research Ethics Committee in Nigeria and the University of Maryland Institutional Review Board.
Exposures and outcomes
Time period is the primary exposure of interest in this analysis. Visits and person-time accrued before the public announcement of the Same-Sex Marriage Prohibition Act were assigned to the prelaw period; visits on or after that date were assigned to the postlaw period.
Outcomes assessed were measures of stigma and discrimination, loss to follow-up, ART status, and viral load. Measures of stigma and discrimination were self-reported and assessed whether participants had ever feared seeking health care because they were MSM, felt they had no safe places to socialise with other MSM, had avoided health care because they were MSM, had been verbally harassed, or had been blackmailed. We assessed history of having had these outcomes at baseline and subsequently every 3 months. In view of the ever versus never nature of the stigma and discrimination outcomes, they were treated as absorbing states, such that once a participant reported having had the outcome, their outcome could not reverse.
We defined loss to follow-up as a patient missing a quarterly visit (90 days after the previous visit) and not returning to care within an additional 90 day window period thereafter despite efforts to contact the participant. ART status was self-reported and confirmed with clinical records for participants previously diagnosed and transferred into HIV care at the TRUST site. HIV testing and assessment of viral load were done at visit 1 and then quarterly. HIV testing was done in accordance with Nigerian national guidelines, with use of a parallel rapid testing algorithm. A viral load less than 50 RNA copies per mL was counted as viral suppression.
Statistical analysis
We compared demographic characteristics of participants enrolled in prelaw and postlaw periods with χ2 statistics. In the initial analyses, reported measures of lifetime stigma and discrimination were illustrated graphically over time, and diff erences between visits in the prelaw and postlaw periods compared with χ2 statistics. To address limitations of the absorbent nature of the outcomes, the potential for confounding, and to account for multiple visits per person, we assessed the incidence of reported stigma and discrimination events. We estimated incidence rate ratios (IRRs) and multivariate adjusted IRRs with Poisson regression with robust variance estimators to account for potential clustering among MSM emanating within the same sexual networks.23 MSM reporting a lifetime history of specific stigma or discrimination events at enrolment were considered prevalent cases and excluded from the corresponding incidence analysis. Thus, the total number of MSM included in the five stigma and discrimination incidence models varied because of differences in the baseline prevalence of the different outcomes. We divided time at risk for an incident event into person-time accrued in the prelaw and postlaw periods. Incident events were assigned to the visit date on which they were first reported. In the multivariate models, we adjusted for factors that differed between participants who were enrolled prelaw and postlaw (baseline age, education, religion, marital status, employment, and ever having tested for HIV).
Loss-to-follow-up models were estimated with robust Poisson regression and adjusted for the confounders described above. Participants completing all enrolment procedures (visits 0 and 1) were included in this analysis if their time since enrolment was sufficient to have achieved the lost to follow-up outcome (180 days after enrolment).
We assessed the associations at enrolment between open communication with a health-care provider, ART use, and viral suppression with χ2 statistics; adjustment was not feasible because of the small sample size of MSM living with HIV. We did analyses with Stata (version 12.1).
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between March 19, 2013, and Aug 7, 2014, 707 MSM participated in baseline study procedures at visit 0. MSM enrolled before legislation had lower levels of education, were more likely to be Muslim, were more likely to be married or living with a woman, and were less likely to be unemployed than MSM enrolled after legislation (table 1). MSM in the postlaw period were also less likely to have been previously tested for HIV (table 1). Overall 404 (57%) MSM returned to complete the remaining baseline study procedures at visit 1, including HIV testing. Individuals not returning for visit 1 were more likely to be young (aged <30 years), Muslim, and employed, and were less likely to have previously identified themselves as MSM to a family member or health-care provider or to have previously tested for HIV (data not shown). HIV testing was completed by 336 (58%) of 578 MSM completing baseline assessments in the prelaw period and by 68 (53%) of 129 MSM in the postlaw period (p=0.261). Overall, 181 (49%, 95% CI 39.9–49.7) of 404 MSM completing HIV testing had a positive test result; the proportion of MSM testing positive was similar between the time periods (data not shown).
Table 1. Baseline characteristics.
| Overall (n=707) | Prelaw (n=578) | Postlaw (n=129) | p value | |
|---|---|---|---|---|
| Age (years) | .. | .. | .. | 0.203 |
| <25 | 415 (59%) | 347 (60%) | 68 (53%) | .. |
| 25–34 | 254 (36%) | 203 (35%) | 51 (39%) | .. |
| ≥35 | 38 (5%) | 28 (5%) | 10 (8%) | .. |
|
| ||||
| Highest education attended* | .. | .. | .. | 0.009 |
| Primary or lower | 103/700 (15%) | 73/572 (13%) | 30/128 (24%) | .. |
| Junior school | 100/700 (14%) | 79/572 (14%) | 21/128 (16%) | .. |
| Secondary school | 311/700 (44%) | 265/572 (46%) | 46/128 (36%) | .. |
| Tertiary or higher | 186/700 (27%) | 155/572 (27%) | 31/128 (24%) | .. |
|
| ||||
| Religion | .. | .. | .. | <0.0001 |
| Christian | 413 (58%) | 369 (64%) | 44 (34%) | .. |
| Muslim | 290 (41%) | 205 (35%) | 85 (66%) | .. |
| Other | 4 (1%) | 4 (1%) | 0 | .. |
|
| ||||
| Self-defined sexual orientation | .. | .. | .. | 0.645 |
| Gay | 246 (35%) | 205 (36%) | 41 (32%) | .. |
| Bisexual | 460 (65%) | 372 (64%) | 88 (68%) | .. |
| Does not know | 1 (<1%) | 1 (<1%) | 0 | .. |
|
| ||||
| Marital status | .. | .. | .. | 0.001 |
| Never married or living with a man | 606 (86%) | 505 (87%) | 101 (78%) | .. |
| Married or living with a woman | 79 (11%) | 53 (9%) | 26 (20%) | .. |
| Divorced, separated, or widowed | 22 (3%) | 20 (4%) | 2 (2%) | .. |
|
| ||||
| Employment | .. | .. | .. | <0.0001 |
| Unemployed | 154 (22%) | 147 (25%) | 7 (5%) | .. |
| Self or formally employed | 396 (56%) | 293 (51%) | 103 (80%) | .. |
| Student | 157 (22%) | 138 (24%) | 19 (15%) | .. |
|
| ||||
| Ever had an HIV test† | .. | .. | .. | 0.019 |
| Yes | 410/706 (58%) | 347/577 (60%) | 63/129 (49%) | .. |
| No | 296/706 (42%) | 230/577 (40%) | 66/129 (51%) | .. |
|
| ||||
| HIV infected at enrolment testing‡ | .. | .. | .. | 0.510 |
| Yes | 181/404 (45%) | 153/336 (46%) | 28/68 (41%) | .. |
| No | 223/404 (55%) | 183/336 (54%) | 40/68 (59%) | .. |
Data are n (%) or n/N, unless otherwise specified.
Data missing for seven individuals.
Data missing for one individual.
404 of the 707 men who participated in the baseline respondent-driven sampling study returned to complete HIV testing and enrolment into the cohort study.
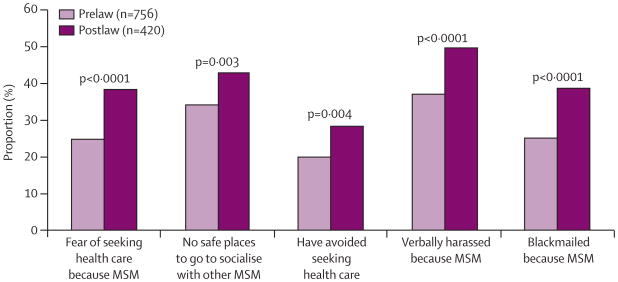
Overall, the 707 participants contributed to 756 prelaw and 420 postlaw visits. At enrolment, 142 (20%) participants reported ever having feared seeking healthcare services and 101 (14%) reported ever having avoided health care because they were MSM. Lifetime reported history of having had each of the five stigma and discrimination indicators was significantly greater in postlaw visits than in prelaw visits (figure 1). In a sensitivity analysis restricted to the first study visit (visit 0), we recorded no differences in reported lifetime stigma and discrimination events between participants enrolled in the prelaw and postlaw periods (data not shown), although slightly fewer individuals enrolled in the postlaw period reported past avoidance of health care (n=89 [15%] vs n=12 [9%]; p=0.074).
Figure 1. Reporting of discrimination and stigma during study visits in the prelaw and postlaw periods.
MSM=men who have sex with men.
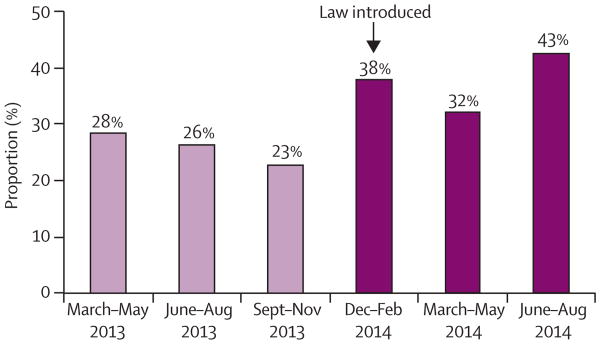
We further assessed the reporting of stigma and discrimination events over quarterly visit periods. The cumulative lifetime experience of reported fear of seeking health-care services across study visits was stable or gradually declined in 2013 (declines are possible because of open enrolment), and increased substantially after the Same-Sex Marriage Prohibition Act was signed into law (figure 2). We noted similar increases in each of the four other stigma and discrimination outcomes in the postlaw period (appendix).
Figure 2. Cumulative lifetime experiences of reported fear of seeking healthcare services across study visits (n=1175 visits).
Overall, 192 participants completed baseline and at least one follow-up visit and were included in the analyses of incident stigma and discrimination outcomes (table 2). After exclusion of individuals who had reported a prevalent event at baseline, the number of participants eligible for each of the five outcome models ranged from 121 to 154 MSM. In the crude Poisson regression models, incidence of fear of seeking health care was 2.57 times greater in the postlaw period than in the prelaw period (table 2). This association was maintained in the multivariate adjusted model (table 2), which accounted for age and variables associated with enrolment in the prelaw and postlaw periods. Risk of reporting no safe spaces to socialise with other MSM also increased significantly in the postlaw period (table 2). Incidence of avoidance of health care did not increase in the postlaw period in participants retained in care, nor did experiences of verbal harassment or blackmail (table 2).
Table 2. Risk of incident stigma and discrimination events in the prelaw and postlaw periods.
| Person-months at risk | Number of events | IRR (95% CI) | p value | Adjusted IRR (95% CI) | p value | |
|---|---|---|---|---|---|---|
| Fear of seeking health care (n=144) | 1153.3 | 32 | 2.57 (1.29–5.10) | 0.007 | 2.92 (1.46–5.84) | 0.002 |
| Prelaw | 735.0 | 13 | .. | .. | .. | .. |
| Postlaw | 418.3 | 19 | .. | .. | .. | .. |
|
| ||||||
| Avoidance of health care (n=154) | 1258.7 | 22 | 1.16 (0.50–2.68) | 0.725 | 1.20 (0.51–2.82) | 0.681 |
| Prelaw | 788.6 | 13 | .. | .. | .. | .. |
| Postlaw | 470.1 | 9 | .. | .. | .. | .. |
|
| ||||||
| No safe spaces to be with other MSM (n=124) | 928.5 | 63 | 2.30 (1.44–3.68) | 0.001 | 3.26 (1.94–5.48) | <0.0001 |
| Prelaw | 665.5 | 33 | .. | .. | .. | .. |
| Postlaw | 263.0 | 30 | .. | .. | .. | .. |
|
| ||||||
| Verbally harassed (n=121) | 920.3 | 27 | 1.33 (0.63-2.78) | 0.453 | 1.41 (0.68-2.92) | 0.351 |
| Prelaw | 574.2 | 15 | .. | .. | .. | .. |
| Postlaw | 346.1 | 12 | .. | .. | .. | .. |
|
| ||||||
| Blackmailed (n=142) | 1138.2 | 31 | 0.95 (0.46–1.92) | 0.877 | 0.99 (0.48–2.05) | 0.988 |
| Prelaw | 719.6 | 20 | .. | .. | .. | .. |
| Postlaw | 418.6 | 11 | .. | .. | .. | .. |
We estimated all IRRs with robust Poisson regression. Adjusted IRRs account for baseline age, education, religion, marital status, employment, and having ever tested for HIV at enrolment. Both crude and adjusted models were run for each outcome (fear, avoidance, absence of safe space, verbal harassment and blackmail). Models have different numbers of individuals present across outcomes because individuals reporting ever having had the relevant outcome were excluded for a given analysis because they were prevalent cases. IRR=incidence rate ratio.
MSM who had ever tested for HIV before study enrolment were 55% less likely to be lost to follow-up than those with no previous testing history (IRR 0.45, 95% CI 0.33–0.62; p<0.0001). Furthermore, MSM testing HIV negative were more than three times as likely to be lost to follow-up as HIV-infected MSM (IRR 3.19, 95% CI 2.29–4.44; p<0.0001). Whereas in unadjusted analysis loss to follow-up decreased in the postlaw period compared with the prelaw period (IRR 0.70, 95% CI 0.50–0.98; p=0.035), after adjustment for age, HIV status, and factors associated with enrolment in the prelaw and postlaw periods (education, marital status, religion, and HIV testing history), there was no association between loss to follow-up and the postlaw period (0.93, 0.64–1.34; p=0.688). In the multivariate analysis, HIV-negative men and those with no previous testing history were more likely to be lost to follow-up than were HIV-infected men and those with previous testing history (data not shown). We recorded an interaction (p=0.053) between the postlaw period and HIV testing history, such that participants who had never tested at baseline were more likely to be lost to follow-up in the postlaw period, but not the prelaw period (data not shown).
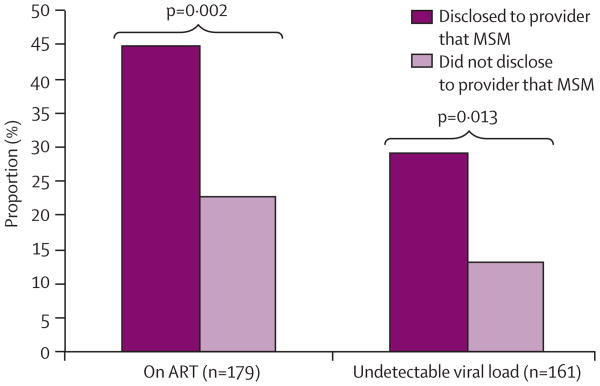
At baseline 144 (21%) of 701 MSM (n=6 had missing data) reported ever having discussed their sexual orientation or relationships with other men with a health-care provider. Among HIV-infected MSM (n=181), data for ART engagement were available for 179 (99%) and viral load suppression for 161 (89%) men. MSM who had previously disclosed to a health-care provider that they had engaged in sexual relationships with other men were significantly more likely to be on ART than were those reporting no previous disclosure (n=31 [45%] vs n=25 [23%]) and were more likely to be virally suppressed at enrolment (n=18 [29%] vs n=13 [13%]; figure 3).
Figure 3. Baseline ART and viral suppression status in HIV-infected MSM and communication with health-care providers.
Two individuals had missing data for ART and 20 individuals had missing data for viral load. MSM=men who have sex with men. ART=antiretroviral treatment.
Discussion
Gay men and MSM in Abuja, Nigeria, experienced increased stigma and discrimination in the period immediately after the signing of the Same-Sex Marriage Prohibition Act. Reports of fear of seeking health care, avoidance of health care, absence of safe spaces to socialise with other MSM, blackmail, and verbal harassment remained steady in the months of enrolment and follow-up before the law, then immediately increased in the post-law period. When limited to participants with available follow-up data and no history of the reported stigma events at baseline, incidence of both fear of seeking health care and absence of safe spaces were significantly greater postlaw than prelaw. Although reports of specific human-rights abuses were not obtained from study participants, findings of increased stigma and discrimination are consistent with reports of violence and persecution of members of the LGBT community in Nigeria in the early months after the law went into effect.24,25
Supportive policy environments and prioritised HIV prevention programmes for marginalised populations are vital to optimise health outcomes in key populations at high risk for HIV acquisition and transmission.26 In this study, MSM who had previously discussed their sexual behaviour with a health-care provider at baseline were more likely to be on ART and virally suppressed than were those who had not engaged in these discussions. Furthermore, even in the context of the study, which provided a safe clinical space in a shared space with a trusted community group, loss to follow-up in MSM was high, particularly in HIV-uninfected MSM who might not perceive that the benefits of continued engagement in HIV prevention programming outweigh the risks of disclosure of sexual practices. The finding that loss to follow-up did not increase after the law went into effect despite increases in fear of seeking health care emphasises the usefulness and success of implementation of the TRUST model (service delivery at a so-called safe haven community venue) for HIV-infected MSM in need of treatment. However, improvement of engagement in services in HIV-negative MSM in Abuja, who have high rates of loss to follow-up and are at substantial HIV acquisition risk, is an unmet challenge. An improved understanding of barriers and incentives for retention in services in HIV-uninfected MSM is needed to identify the most promising combinations of HIV prevention interventions for this population, such as pre-exposure prophylaxis and home-based testing.9
The present analyses provide a unique perspective on the negative effect of the continuing push-back in many countries in sub-Saharan Africa against same-sex practices. Our results emphasise the negative public health effect this legislation can cause via its restrictions on uptake of HIV prevention, treatment, and care services in those most at risk for HIV transmission. We provide unique real-time estimates of the potential harm that such legislation has on health, and potentially preventable outcomes such as onward HIV transmission. These prospective data support cross-sectional studies that have consistently shown that building of trust in the HIV treatment and prevention delivery system is essential to improve health outcomes in MSM.27–30 Moreover, these quantitative results reinforce qualitative findings that criminalisation of same-sex behaviour only adds to the HIV burden by driving MSM away from the benefits of HIV treatment and prevention services.12,31 Although causality cannot be directly established because of the uniform nature of the experience of the exposure in our population, our individual-level prospective data provide more robust evidence than have previous ecological analyses21 and cross-sectional data showing reduced uptake of HIV testing in countries criminalising same-sex practices, and have the added benefit of providing more precise estimates for the drivers of this negative outcome.10
Our analyses have some limitations. Stigma and discrimination outcomes were cumulative absorbent-state measures and when exactly incident events were experienced is unknown. We assigned events to the day that they were reported. If stigma and discrimination events were randomly distributed between study visits, this approach would overestimate the effect of the law. However, if the law did have an effect and events were not distributed at random, the effect would be underestimated because additional exposure time would have been accrued after the outcome had been experienced. Although, theoretically, the events could have been randomly distributed across time periods, we believe that this scenario is less plausible, especially because reported events remained stable until visits after the law went into effect. Additionally, noise and misclassification around the exposure are probable. We used the date of the public announcement of the law's enactment because this is the date most likely to affect stigma and discrimination outcomes. Corresponding media coverage and arrests further support this cutoff; however, concerns within the community were undoubtedly present beforehand and there is probably noise around the exposure cutoff s, which would underestimate the negative effect of the law. Furthermore, informative censoring in the cohort could have biased results to underestimate the effect of the law on avoidance of health care. Specifically, if MSM most likely to report avoidance of health care are self-censored, they would not be available to report this outcome. Future studies to further characterise this frailty bias and drivers of high loss to follow-up, including the roles of stigma and discrimination and lack of confidence in the TRUST model, are needed to develop strategies for engagement of this hard-to-reach population at high risk for HIV acquisition and transmission. The high rate of early loss to follow-up in HIV-negative MSM reinforces this need. We recorded similar trends in loss to follow-up between the first and second visits, suggesting that individuals who are not openly identified as part of the MSM community are less likely to engage in MSM-friendly health services and HIV testing, potentially because of fear of public disclosure of their sexual behaviour. Finally, we noted differences in MSM enrolled before and after the law, although these differences were probably related to the nature of the respondent-driven sampling study and diff erences in individuals reached in deeper recruitment waves.32
Despite these limitations, the present analyses provide the first quantitative, client-level data obtained during the enactment of laws further criminalising same-sex practices, and thus provide the most compelling data so far about the negative consequences of discriminatory legislation. Overall, these results emphasise concerns about the mounting environment of fear, including fear of seeking health-care services, faced by MSM in settings that criminalise same-sex practices and freedom of assembly. Strategies to reach MSM less likely to engage in HIV testing and care in highly stigmatised environments are necessary to reduce time to HIV diagnosis and treatment, which are needed to meaningfully address the high burden of HIV in MSM.33
Supplementary Material
Research in context.
Evidence before this study
A systematic review about structural determinants of HIV-related risk emphasised the scarcity of evidence linking the criminalisation of same-sex practices with health-seeking behaviour and HIV-related health outcomes in men who have sex with men (MSM) worldwide. Ecological analyses have emphasised a link between the criminalisation of same-sex practices and insufficient investment in HIV-related surveillance and programming for MSM, together with some cross-sectional assessments of the association. Specifically, a cross-sectional, multicountry, internet-based survey reported a negative association between individual uptake of HIV testing and HIV prevention strategies and residence in countries with laws criminalising same-sex practices. Two other analyses have qualitatively documented the effect of criminalising policies on engagement in health care, including HIV services in MSM, in addition to concerns from health-care providers in these settings about the risks they take in providing services to MSM. Because of the challenges of data collection in the most stigmatising environments, quantitative data documenting the prospective effect of criminalising policies on HIV-related health outcomes for MSM are not available.
Added value of this study
We did these analyses as part of a prospective implementation study of MSM in Nigeria, which began 10 months before introduction of the Same-Sex Marriage Prohibition Act. This is the first study to assess quantitative outcomes related to engagement in HIV prevention, treatment, and care services in a cohort of MSM before and after anti-same-sex legislation was enacted, allowing for a natural examination of the immediate effect of this policy in MSM. We believe that these data are the most compelling reported so far, with characterisation of the negative effects of punitive legislation, including increased reported fear of seeking health services and lower retention in HIV prevention services in HIV-negative than HIV-infected MSM.
Implications of all the available evidence
Combined with results from previous ecological and cross-sectional studies, our findings reinforce the negative HIV-related health effects of anti-homosexuality legislation in young MSM with a high HIV prevalence and incidence. Urgent efforts to characterise safe and trusted HIV prevention and treatment services are needed, particularly in countries with discriminatory legal environments, to minimise the risks of HIV acquisition and transmission and finally achieve an AIDS-free generation.
Acknowledgments
We thank the men who participated in this study, despite the stigma and discrimination they have experienced, and the study staff who have remained dedicated to the mission of TRUST throughout. The TRUST study is supported by the US National Institutes of Health under award number R01MH099001-01. Additional support has been provided by the US Military HIV Research Program (grant number W81XWH-07-2-0067), Fogarty AIDS International Training and Research (D43TW01041), and the President's Emergency Plan for AIDS Relief through cooperative agreement U2G IPS000651 from the Centers for Disease Control and Prevention, part of the Department of Health and Human Services, and the Global AIDS Program with the Institute of Human Virology Nigeria. The content is solely the responsibility of the authors and does not represent the official views of the Department of Defense, National Institutes of Health, or other funders.
Footnotes
Contributors: WAB, MEC, SDB, BK, JA, and ON designed the study. SK, RGN, IO, and MEC collected and managed data. SRS, WAB, MEC, SDB, and IO conceived the analyses. SRS analysed data with input from RGN, MEC, and SDB. SRS, SDB, RGN, WAB, and MEC drafted the manuscript and IO, BK, BK, SK, and ON provided critical review and editing. All authors have seen and approved the paper.
Declaration of interests: We declare no competing interests.
See Online for appendix
Contributor Information
Sheree R Schwartz, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Rebecca G Nowak, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, USA.
Ifeanyi Orazulike, International Centre for Advocacy for the Right to Health, Abuja, Nigeria.
Babajide Keshinro, US Military HIV Research Program, Silver Spring, MD, USA.
Julie Ake, US Military HIV Research Program, Silver Spring, MD, USA.
Sara Kennedy, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, USA.
Ogbonnaya Njoku, US Military HIV Research Program, Silver Spring, MD, USA.
William A Blattner, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, USA.
Manhattan E Charurat, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, USA.
Stefan D Baral, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
References
- 1.Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–77. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyrer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS. 2013;27:2665–78. doi: 10.1097/01.aids.0000432449.30239.fe. [DOI] [PubMed] [Google Scholar]
- 3.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4:e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trapence G, Collins C, Avrett S, et al. From personal survival to public health: community leadership by men who have sex with men in the response to HIV. Lancet. 2012;380:400–10. doi: 10.1016/S0140-6736(12)60834-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dramé FM, Peitzmeier S, Lopes M, et al. Gay men and other men who have sex with men in West Africa: evidence from the field. Cult Health Sex. 2013;15(suppl):7–21. doi: 10.1080/13691058.2012.748935. [DOI] [PubMed] [Google Scholar]
- 6.Beyrer C, Sullivan PS, Sanchez J, et al. A call to action for comprehensive HIV services for men who have sex with men. Lancet. 2012;380:424–38. doi: 10.1016/S0140-6736(12)61022-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beyrer C. Pushback: the current wave of anti-homosexuality laws and impacts on health. PLoS Med. 2014;11:e1001658. doi: 10.1371/journal.pmed.1001658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Risher K, Adams D, Sithole B, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16(3 suppl 2):18715. doi: 10.7448/IAS.16.3.18715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fay H, Baral SD, Trapence G, et al. Stigma, health care access, and HIV knowledge among men who have sex with men in Malawi, Namibia, and Botswana. AIDS Behav. 2011;15:1088–97. doi: 10.1007/s10461-010-9861-2. [DOI] [PubMed] [Google Scholar]
- 10.Arreola S, Santos GM, Beck J, et al. Sexual stigma, criminalization, investment, and access to HIV services among men who have sex with men worldwide. AIDS and Behav. 2015;19:227–34. doi: 10.1007/s10461-014-0869-x. [DOI] [PubMed] [Google Scholar]
- 11.Semugoma P, Beyrer C, Baral S. Assessing the effects of anti-homosexuality legislation in Uganda on HIV prevention, treatment, and care services. SAHARA J. 2012;9:173–76. doi: 10.1080/17290376.2012.744177. [DOI] [PubMed] [Google Scholar]
- 12.Poteat T, Diouf D, Drame FM, et al. HIV risk among MSM in Senegal: a qualitative rapid assessment of the impact of enforcing laws that criminalize same sex practices. PloS One. 2011;6:e28760. doi: 10.1371/journal.pone.0028760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baral S, Holland CE, Shannon K, et al. Enhancing benefits or increasing harms: community responses for HIV among men who have sex with men, transgender women, female sex workers, and people who inject drugs. J Acquir Immune Defic Syndr. 2014;66(suppl 3):S319–28. doi: 10.1097/QAI.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 14.Gruskin S, Ferguson L, Alfven T, Rugg D, Peersman G. Identifying structural barriers to an effective HIV response: using the National Composite Policy Index data to evaluate the human rights, legal and policy environment. J Int AIDS Soc. 2013;16:18000. doi: 10.7448/IAS.16.1.18000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goitom H. Nigeria: bill prohibiting same-sex marriage moves forward. [accessed Nov 29, 2014];2013 Dec 26; http://www.loc.gov/lawweb/servlet/lloc_news?disp3_l205403807_text.
- 16.Gladstone R. Nigerian President signs ban on same-sex relationships. [accessed Nov 29, 2014];2014 Jan 13; http://www.nytimes.com/2014/01/14/world/africa/nigerian-president-signs-ban-on-same-sex-relationships.html.
- 17.Itaborahy LP, Zhu J. A world survey of laws: criminalisation, protection and recognition of same-sex love. Geneva: International Lesbian Gay Bisexual Trans and Intersex Association; 2014. [Google Scholar]
- 18.National Assembly of the Federal Republic of Nigeria. Same Sex Marriage (Prohibition) Act, 2013. [accessed May 21, 2015];2014 http://www.nassnig.org/nass/acts.php.
- 19.Faul M. Nigerian gay men arrested in dozens after new law passes. [accessed April 3, 2015];2014 Jan 14; http://www.huffingtonpost.com/2014/01/14/nigeria-gay-arrests_n_4595124.html.
- 20.BBC News. Nigeria Islamic court tries gay suspects in Bauchi. [accessed April 3, 2015];2014 Jan 15; http://www.bbc.co.uk/news/world-africa-25749308.
- 21.The Foundation for AIDS Research and Johns Hopkins Bloomberg School of Public Health. Achieving an AIDS-free generation for gay men and other MSM: financing and implementation of HIV programs targeting MSM. New York: AMFAR; 2012. [Google Scholar]
- 22.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- 23.Frome EL, Checkoway H. Epidemiologic programs for computers and calculators. Use of Poisson regression models in estimating incidence rates and ratios. Am J Epidemiol. 1985;121:309–23. doi: 10.1093/oxfordjournals.aje.a114001. [DOI] [PubMed] [Google Scholar]
- 24.Nossiter A. Nigeria tries to ‘sanitize’ itself of gays. [accessed Nov 29, 2015];2014 Feb 8; http://www.nytimes.com/2014/02/09/world/africa/nigeria-uses-law-and-whip-to-sanitize-gays.html.
- 25.Frizell S. Mob attacks gays In Nigerian capital. [accessed Nov 29, 2015];2014 Feb 15; http://world.time.com/2014/02/15/nigeria-mob-attack-abuja/
- 26.UN Development Programme. Global Commission on HIV and the law: risks, rights and health. New York: UNDP; 2012. [Google Scholar]
- 27.Charurat ME, Emmanuel B, Akolo C, et al. Uptake of treatment as prevention for HIV and continuum of care among hiv-positive men who have sex with men in Nigeria. J Acquir Immune Defic Syndr. 2015;68(suppl 2):S114–23. doi: 10.1097/QAI.0000000000000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernstein KT, Liu KL, Begier EM, Koblin B, Karpati A, Murrill C. Same-sex attraction disclosure to health care providers among New York City men who have sex with men: implications for HIV testing approaches. Arch Intern Med. 2008;168:1458–64. doi: 10.1001/archinte.168.13.1458. [DOI] [PubMed] [Google Scholar]
- 29.Durso LE, Meyer IH. Patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbians, gay men, and bisexuals. Sex Res Social Policy. 2013;10:35–42. doi: 10.1007/s13178-012-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baral S, Trapence G, Motimedi F, et al. HIV prevalence, risks for HIV infection, and human rights among men who have sex with men (MSM) in Malawi, Namibia, and Botswana. PloS One. 2009;4:e4997. doi: 10.1371/journal.pone.0004997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wirtz AL, Kamba D, Jumbe V, et al. A qualitative assessment of health seeking practices among and provision practices for men who have sex with men in Malawi. BMC Int Health Hum Rights. 2014;14:20. doi: 10.1186/1472-698X-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baral SD, Ketende S, Schwartz S, et al. Evaluating respondent-driven sampling as an implementation tool for universal coverage of antiretroviral studies among men who have sex with men living with HIV. J Acquir Immune Defic Syndr. 2015;68(suppl 2):S107–13. doi: 10.1097/QAI.0000000000000438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sullivan PS, Carballo-Dieguez A, Coates T, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380:388–99. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.