Abstract
Our aim was to characterize the incidence rates and cumulative incidence of anorexia nervosa (AN), bulimia nervosa (BN), and eating disorder not otherwise specified (EDNOS), and examine associations among eating disorder diagnoses, suicide attempts, and mortality. Individuals born in Denmark between 1989 and 2006 were included (N=966,141, 51.3% male). Eating disorders diagnoses (AN, Broad AN, BN, EDNOS) were drawn from the Danish Psychiatric Central Research Register (PCRR) and Danish National Patient Register (NPR). Suicide attempts and deaths were captured in the NPR, the PCRR, and the Danish Civil Registration System (CRS). In females, AN had a peak hazard at approximately age 15 years, BN at 22 years, and EDNOS had an extended peak that spanned 18 years to 22 years. Eating disorder diagnoses predicted a significantly higher hazard for death and suicide attempt compared with the referent of individuals with no eating disorders. In males, peak hazard for diagnosis was earlier than in females. The present study represents one of the largest and longest studies of eating disorder incidence and suicide attempts and death in both females and males. Eating disorders are accompanied by increased hazard of suicide attempts and death even in young adults.
Keywords: eating disorders, anorexia nervosa, bulimia nervosa, incidence, suicide, mortality
Increasingly, eating disorders are recognized as severe, occasionally chronic mental illnesses that are associated with with both disability and elevated mortality (Arcelus, Mitchell, Wales, & Nielsen, 2011; Field et al., 2012; Sullivan, 1995). Describing incidence rates across age strata provides important insight into the developmental course of eating disorders, risk factors for their onset, and timing of clinical referral. Clinically, it assists in allocating funds for health services and ensuring adequate resources for service delivery (Smink, van Hoeken, & Hoek, 2012).
Studies of anorexia nervosa (AN) and bulimia nervosa (BN) have documented a peak age of disorder incidence between 16 and 21 (Favaro, Caregaro, Tenconi, Bosello, & Santonastaso, 2009; Hudson, Hiripi, Pope, & Kessler, 2007; Keski-Rahkonen et al., 2009; van Son, van Hoeken, Bartelds, van Furth, & Hoek, 2006). However, most of our knowledge of eating disorder incidence is based on females and much less is known about the age trends in the incidence of eating disorders in males (Bulik et al., 2006; Hudson et al., 2007; Micali, Hagberg, Petersen, & Treasure, 2013). Moreover, very little is known about the incidence of eating disorder not otherwise specified (EDNOS) or, as it is defined currently in the Diagnostic And Statistical Manual – 5th edition, other specified feeding or eating disorder (OSFED) (American Psychiatric Association, 2013; Micali et al., 2013; Wade, Bergin, Tiggemann, Bulik, & Fairburn, 2006).
The best estimates of eating disorder incidence have been obtained from primary care medical surveillance (Currin, Schmidt, Treasure, & Jick, 2005; Micali et al., 2013; van Son et al., 2006), pediatric medical surveillance (Nicholls, Lynn, & Viner, 2011; Pinhas, Morris, Crosby, & Katzman, 2011), representative community samples (Hudson et al., 2007; Preti et al., 2009; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011), and twin cohorts (Bulik et al., 2006; Keski-Rahkonen et al., 2009; Keski-Rahkonen et al., 2007; Wade et al., 2006). Because of the relatively low incidence rates of eating disorders in the community, medical surveillance through register data offers an invaluable resource to estimate the number of people with eating disorders across sex and age even though it cannot provide community-based estimates or precise age of onset.
Since 1995, the Danish Psychiatric Central Research Register (PCRR) has included medical surveillance of all clinical eating disorders diagnoses using the International Statistical Classification of Diseases and Related Health Problems, 10th edition (ICD-10) in both outpatient and hospital care and, thus, offers a unique opportunity to extend our understanding of age trends in eating disorders diagnoses in both females and males (Mors, Perto, & Mortensen, 2011; Organization, 2005).
Aims of the Study
The overarching aim of the present study was to characterize the incidence rates and cumulative incidence of AN, BN, and EDNOS as detected in outpatient and inpatient care for individuals born in Denmark between 1989 and 2006 (~1 million individuals). We investigated patterns of peak age of risk for eating disorders across sex and associations among eating disorder status, mortality, and suicide attempts across diagnoses.
Methods
The Registers
In 1968, the Danish Civil Registration System (CRS) was established. Since that time, every person living in Denmark or alive at the time the CRS was established has been assigned a CRS number (Pedersen, Gotzsche, Moller, & Mortensen, 2006). The CRS number serves as a unique personal identifier and enables linkage across all national registers. The CRS includes each individual’s CRS number, parental CRS numbers, sex, date of birth, and vital status, and is continuously updated.
The Danish National Patient Register (NPR) was established in 1977 (Lynge, Sandegaard, & Rebolj, 2011). It initially included data on all hospital admissions in Denmark but, in 1995, was expanded to include hospital-based outpatient and emergency room contacts. The PCRR was computerized in 1969 and contains data on all admissions to Danish psychiatric inpatient facilities. Since 1995 the PCRR has also included information on all outpatient and emergency room visits. Both NPR and PCRR contain information on dates of admission and discharge, patient type (inpatient, outpatient, or emergency room visit), reason for contact and main and auxiliary diagnoses (up to 17 diagnoses). PCRR currently includes data on approximately 850,000 persons and 3.9 million admissions since 1969 (Mors et al., 2011). Diagnostic codes in the NPR and PCRR have followed a Danish version of the International Classification of Diseases (ICD). Since 1994, ICD, tenth revision (ICD-10) codes have been used (World Health Organization, 1992).
All personal information from the registers is anonymized. As the study did not result in any contact with participants, no written informed consent was required. The study was fully approved by the Danish Data Protection Agency.
Study Population
Using the CRS, we identified everyone born in Denmark between January 1, 1989 and December 31, 2006. We included all individuals who were alive and living in Denmark on their 6th birthday and had Danish-born parents (N=966,141, 51.3% male). Members of the cohort were followed from their 6th birthday, until the event of interest, date of death or emigration from Denmark, or December 31, 2012, whichever came first. In total, 4764 individuals emigrated from Denmark during this period and 22 individuals were lost to follow up. Those lost to follow-up were treated as emigrants in these analyses.
Eating Disorder Assessment
In the present study, we examined prevalence and incidence of eating disorders since January 1995. ICD-10 eating disorders codes include AN (F50.0), atypical AN (F50.1), BN (F50.2, F50.3), and EDNOS (F50.9).
The ICD-10 AN diagnoses were collapsed into two separate classifications. In our first classification, broad AN included both AN (F50.0) and atypical AN (F50.1). However, to determine the sensitivity of this classification, we also examined the incidence of the more narrow definition of AN (F50.0), without including the F50.1 cases. The ICD-10 matches Diagnostic and Statistical Manual – 4th Edition (DSM-IV) criteria and requires weight status of <85% of ideal weight and amenorrhea to make a diagnosis of narrow AN (F50.0) (American Psychiatric Association, 2000). The ICD-10 atypical AN (F50.1) criteria includes disorders that fulfill core features of AN (marked weight loss) but in which symptoms, such as amenorrhea or marked fear of fat, can be absent.
The eating disorder diagnosis did not have to be indicated as the main or “action” diagnosis, which led to hospitalization or outpatient treatment in the registry records, and diagnoses were not considered to be mutually exclusive. That is, an individual could be diagnosed with AN at one time point and contribute to incidence rate of AN and be diagnosed with BN at a different time point and contribute to the incidence rate of BN. Onset was defined as the admission date of the first in- or outpatient contact recorded in the NPR or PCRR after the age of 6 years leading to a discharge diagnosis (main or auxiliary) of the eating disorder of interest.
Suicide Attempts and Suicide
Medical contacts in the NPR and PCRR were defined as suicide attempts under the following conditions, either: 1) The reason for medical contact marked as “suicide/suicide attempt;” or 2) The contact had a primary psychiatric diagnosis (ICD-10: F00-F99) and a secondary diagnosis of poisoning (T36-T50, T52-T60); or 3) The contact had a primary psychiatric diagnosis and an auxiliary diagnosis of wound to the lower arm, wrist or hand (S51, S55, S59, S61, S65, S69); or 4) The contact had primary diagnosis of poisoning (T39, T42, T43, T58); or 5) the contact had main or auxiliary diagnosis of intentional self-harm (X60-X84). Suicide attempts were categorized as either violent (e.g., use of a weapon) or nonviolent (e.g., poisoning).
Statistical Analyses
Eating disorders incidence
The age- and sex-specific incidence rates were calculated as the number of new cases occurring at each age category/group in females and males separately and reported per 10,000 person years. Person-years—the sum of years that individuals in the study population have been followed—is commonly used as a denominator in epidemiological studies of incidence rates in order to account for situations in which the amount of observation time differs between individuals (Vandenbroucke & Pearce, 2012).
Cumulative incidences were calculated taking into account the possibility that a person could die before receiving a diagnosis. The cumulative incidence describes, at a given age, the proportion of people (in % or per 100 person) in a population who have received a diagnosis earlier than the given age. Baseline cumulative incidences of each of the eating disorders were calculated and plotted by sex using competing-risks survival regression with death and emigration as competing risks. Smoothed age- and sex-specific hazard functions were estimated and plotted using the estimated hazard contributions and Epanechnikov kernel smoothing (Soltanian & Hossein, 2012).
Rates of Death and Suicide Attempt
Sex-specific hazard ratios (HR) of death and suicide attempt (any, violent, nonviolent) were calculated using Cox proportional hazards regression for each of the eating disorder exposures: broad AN (including broad and narrow diagnoses), narrow AN, BN, and EDNOS. All estimates were adjusted for calendar-time and for age in the nonparametric part of the Cox model. Calendar year and eating disorder status were treated as time-dependent variables, while all other variables were considered time-independent. Calendar years were categorized as 1995-1999, 2000-2004, 2005-2009 and 2010-2012. All statistical analyses were conducted using Stata version 12 (StataCorp, 2011). In keeping Danish Data Protection privacy, we report cells with values from 1-3 as <4 in the tables.
Results
Incidence rate
The incidence rate per 10,000 person-years by age, sex and type of eating disorder is presented in Table 1.
Table 1.
Incidence rate of eating disorders per 10,000 person-years by age (divided into 5-year epochs), sex and type of eating disorder.
| Females | Males | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Age (years) | Cases (N) | Person- Years | Incidence (95% CI) | Cases (N) | Person-Years | Incidence (95% CI) | Cases (N) | Person-Years | Incidence (95% CI) |
| Broad Anorexia Nervosa
| |||||||||
| 6-10 | 22 | 1679757.3 | 0.13 (0.09, 0.20) | 4 | 1770800.3 | 0.02 (0.01, 0.06) | 26 | 3450557.6 | 0.08 (0.05, 0.11) |
| 11-15 | 929 | 1533786.0 | 6.05 (5.68, 6.46) | 108 | 1619727.6 | 0.67 (0.55, 0.81) | 1037 | 3153513.6 | 3.29 (3.10, 3.50) |
| 16-20 | 1014 | 870339.6 | 11.65 (10.96, 12.39) | 71 | 921606.8 | 0.77 (0.61, 0.97) | 1085 | 1791946.5 | 6.05 (5.71, 6.43) |
| 21-24 | 171 | 206114.3 | 8.30 (7.14, 9.64) | 5 | 218857.9 | 0.23 (0.10, 0.55) | 176 | 424972.3 | 4.14 (3.57, 4.80) |
|
| |||||||||
| Narrow Anorexia Nervosa
| |||||||||
| 6-10 | 11 | 1679770.6 | 0.07 (0.04, 0.12) | <4 | 1770801.9 | 0.02 (0.01, 0.05) | 14 | 3450572.5 | 0.04 (0.02, 0.07) |
| 11-15 | 690 | 1534139.2 | 4.50 (4.17, 4.85) | 73 | 1619791.7 | 0.45 (0.36, 0.57) | 763 | 3153930.9 | 2.42 (2.25,2.60) |
| 16-20 | 683 | 871592.6 | 7.84 (7.27, 8.45) | 42 | 921764.8 | 0.46 (0.34, 0.62) | 725 | 1793357.4 | 4.04 (3.76, 4.35) |
| 21-24 | 92 | 206622.7 | 4.45 (3.63, 5..46) | <4 | 218901.2 | 0.14 (0.04, 0.42) | 95 | 425523.9 | 2.23 (1.83, 2.73) |
|
| |||||||||
| Bulimia Nervosa
| |||||||||
| 6-10 | 0 | 1679781.2 | 0.00 (·, ·) | 0 | 1770804.2 | 0.00 (·, ·) | 0 | 3450585.4 | 0.00 (·, ·) |
| 11-15 | 69 | 1535112.6 | .45 (0.36,0.57) | 0 | 1619923.6 | 0.00 (·, ·) | 69 | 3155036.3 | 0.22 (0.17,0.28) |
| 16-20 | 489 | 873966.3 | 5.60 (5.12, 6.11) | 18 | 922005.0 | 0.19 (0.12, 0.31) | 507 | 1795971.3 | 2.82 (2.59, 3.08) |
| 21-24 | 181 | 206973.8 | 8.75 (7.56, 10.11) | <4 | 218966.1 | 0.09 (0.02, 0.37) | 183 | 425939.9 | 4.30 (3.72, 4.97) |
|
| |||||||||
| Eating Disorder Not Otherwise Specified
| |||||||||
| 6-10 | 21 | 1679752.6 | 0.13 (0.08, 0.19) | 10 | 1770787.6 | 0.06 (0.30, 0.10) | 31 | 3450540.1 | 0.09 (0.06, 0.13) |
| 11-15 | 385 | 1534630.0 | 2.51 (2.27, 2.77) | 50 | 1619803.8 | 0.31 (0.23, 0.41) | 435 | 3154433.8 | 1.38 (1.25, 1.51) |
| 16-20 | 579 | 872855.6 | 6.63 (6.11, 7.20) | 54 | 921778.1 | 0.58 (0.45, 0.76) | 633 | 1794633.7 | 3.53 (3.26, 3.81) |
| 21-24 | 139 | 206908.7 | 6.72 (5.69, 7.93) | <4 | 218898.8 | 0.14 (0.04, 0.42) | 142 | 425807.4 | 3.33 (2.82,3.93) |
Females
In Table 1, when divided into 5-year epochs, the peak age of incidence of diagnosed broad and narrow AN in females was 16-20 years of age [incidence rate = 11.65 (CI: 10.96, 12.39) and 7.84 (CI: 7.27, 8.45) respectively]. Diagnosed BN peaked between the ages of 21-24 years [incidence rate = 8.75 (CI: 7.56, 10.11). EDNOS had dual peak incidence rates at 16-20 years of age and 21-24 years of age [incidence rate = 6.63 (CI: 6.11, 7.20) and 6.72 (CI: 5.69, 7.93), respectively].
Figure 1 presents the smoothed hazard for female eating disorder diagnosis per 10,000 person-years at each age. In these curves, both broad and narrow AN had a peak hazard at approximately age 15 years (15.0 and 14.8 respectively). Diagnosed BN peaked at 22.0 years and EDNOS had a peak hazard at 17.6 years that plateaued until 22 years.
Figure 1.
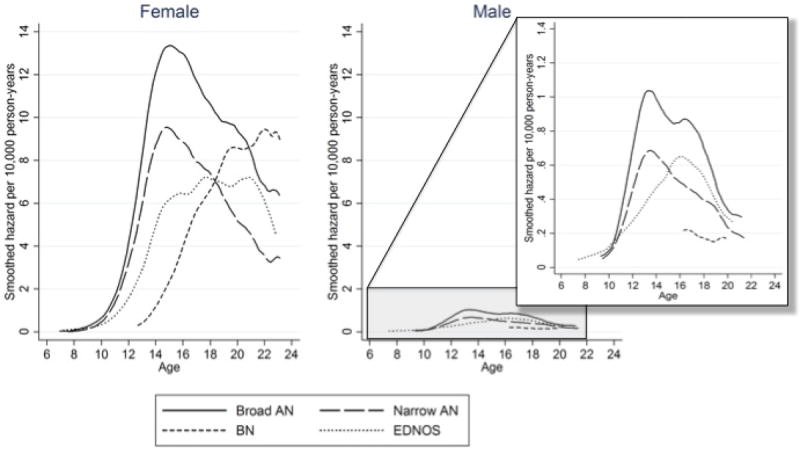
Hazard per 10,000 person-years for broad and narrow anorexia nervosa (AN), bulimia nervosa (BN), and eating disorder not otherwise specified (EDNOS). Male curves are magnified for comparison
Since diagnostic crossover from AN to BN is common and may explain why the peak BN incidence occurs later than AN, we conducted post-hoc analyses to examine the peak age of incidence in those who developed BN without a prior history of AN (Eddy et al., 2008). In females without an AN history, the maximum hazard of BN was 22.1 years of age. In females with BN and an AN history, the maximum hazard of BN was 22.9 years of age (data not shown).
Males
In Table 1, when divided into 5-year epochs, the peak age of incidence of diagnosed broad AN in males was between 16-20 years of age [incidence rate = 0.77 (CI: 0.61, 0.97)]. Narrow AN had peak incidences at 11-15 years and 16-20 years of age [incidence rate = 0.45 (CI: 0.36, 0.57) and 0.46 (CI: 0.34, 0.62) respectively]. Diagnosed BN peaked between the ages of 16-20 years [incidence rate = 0.19 (CI: 0.12, 0.31) and was younger than in females. EDNOS had a peak incidence rates at 16-20 years of age [0.58 (CI: 0.45, 0.76)].
Figure 1 presents the smoothed hazard for male eating disorder diagnosis per 10,000 person-years at each age. In these curves, both broad and narrow AN in males had a peak hazard at approximately age 13.3 years. Diagnosed BN and EDNOS both peaked at 16 years (16.5 and 16.1 years, respectively). In post-hoc analyses examining males without a history of AN, the peak age of BN incidence was 16.6 years of age (data not shown).
Thus, overall, the eating disorder incidence for females was significantly greater than for males at each age. Upon visual inspection, the peak diagnosed eating disorder incidence for males appeared to be younger than for females. For example, in broad and narrow AN, the peak age of onset was ~13 years for males vs. ~15 years for females in the incidence curves. In both females and males, broad AN was the most commonly diagnosed eating disorder. The peak incidence for broad and narrow AN in the incidence curves also occurred at a younger age than the peak for BN or EDNOS. For females, the peak age of onset of AN was age 15 years vs. age 18-22 years for BN and EDNOS. For males, the peak age of onset for AN was age 13 years vs. 16 years for BN and EDNOS.
Cumulative Incidence
The cumulative incidence per 100 persons by age, sex, and type of eating disorder is presented in Table 2 and represented in Figure 2.
Table 2.
Cumulative incidence at age 24 of eating disorders per 100 persons by age, sex and type of eating disorder.
| Females | Males | Total | ||||
|---|---|---|---|---|---|---|
| Cases (N) | Incidence (95% CI) | Cases (N) | Incidence (95% CI) | Cases (N) | Incidence (95% CI) | |
| Broad Anorexia Nervosa | ||||||
| 2136 | 1.19 (1.12,1.27) | 188 | 0.08 (0.07,0.09) | 2324 | 0.62 (0.58, 0.66) | |
| Narrow Anorexia Nervosa | ||||||
| 1476 | 0.78 (0.72,0.85) | 121 | 0.05 (0.04, 0.06) | 1597 | 0.41 (0.38, 0.44) | |
| Bulimia Nervosa | ||||||
| 739 | 0.69 (0.58,0.83) | 20 | 0.01 (0.01, 0.02) | 759 | 0.34 (0.29,0.41) | |
| Eating Disorder Not Otherwise Specified | ||||||
| 1124 | 0.70 (0.65, 0.76) | 117 | 0.05 (0.04, 0.06) | 1241 | 0.37 (0.34, 0.40) | |
Figure 2.
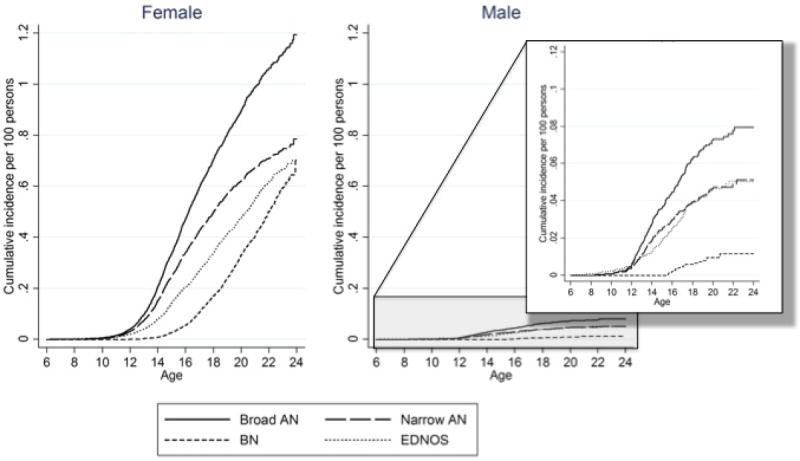
Cumulative incidence (per 100 people) of broad and narrow anorexia nervosa (AN), bulimia nervosa (BN), and eating disorder not otherwise specified (EDNOS). Male curves are magnified for comparison.
Overall in the final cohort of 966,141 individuals in the NPR and PCRR, 2136 females and 188 males had broad AN, 1476 females and 121 males had narrow AN, 739 females and 20 males had BN, 1124 females and 117 males had EDNOS detected before the age of 25. The female to male ratio for cumulative incidence was 15.0:1 for broad AN, 15.3:1 for narrow AN, 60.2:1 for BN and 13.9:1 for EDNOS.
Death and Suicide Outcomes
In a Cox regression model, hazard ratios greater than 1 indicate a higher probability of the outcome compared to the general population whereas ratios less than 1 indicate a lower probability of outcome. In this case, we estimated the hazard of death, suicide attempt, non-violent suicide attempt, and violent suicide attempt by eating disorder status (Table 3).
Table 3.
Results (hazard ratios and 95% confidence intervals) from Cox regression hazards models predicting death, suicide attempt, non-violent suicide attempt, and violent suicide attempt from broad anorexia nervosa, narrow anorexia nervosa, bulimia nervosa, and eating disorder not otherwise specified.
| Females (N=470,499) | Males (N=495,642) | |||
|---|---|---|---|---|
|
| ||||
| Outcome | n/N (%) | Hazard Ratio (95% CI) | n/N (%) | Hazard Ratio (95% CI) |
| Broad Anorexia Nervosa
| ||||
| Death | 4/2136 | 3.1* (1.1, 8.2) | 0/188 | ne |
| Suicide Attempt | 145/2046 | 4.8*** (4.1, 5.7) | <4/187 | 2.1 (0.7, 6.6) |
| Non-violent Attempt | 142/2054 | 4.9*** (4.1, 5.7) | <4/187 | 2.2(0.7, 6.9) |
| Violent Attempt | 22/2124 | 8.6*** (5.6, 13.1) | 0/188 | ne |
|
| ||||
| Narrow Anorexia Nervosa
| ||||
| Death | <4/1476 | 1.0 (0.1, 7.4) | 0/121 | ne |
| Suicide Attempt | 109/1421 | 4.9*** (4.0, 5.9) | <4/121 | 1.1 (0.2, 7.8) |
| Non-violent Attempt | 105/1425 | 4.9*** (4.0, 5.9) | <4/121 | 1.1 (0.2, 8.1) |
| Violent Attempt | 14/1471 | 7.3*** (4.3,12.4) | 0/121 | ne |
|
| ||||
| Bulimia Nervosa
| ||||
| Death | <4/739 | 5.0* (1.2, 20.3) | 0/20 | ne |
| Suicide Attempt | 57/642 | 8.7*** (6.7, 11.2) | <4/19 | 7.4* (1.1, 52.7) |
| Non-violent Attempt | 56/652 | 8.7*** (6.7, 11.3) | <4/20 | 7.4* (1.0, 52.9) |
| Violent Attempt | 9/722 | 13.9*** (7.1, 26.9) | 0/19 | ne |
|
| ||||
| Eating Disorder Not Otherwise Specified
| ||||
| Death | 0/1124 | ne | <4/117 | 6.5 (0.9, 46.6) |
| Suicide Attempt | 101/995 | 7.9*** (6.5, 9.6) | 4/116 | 4.6** (1.7, 12.3) |
| Non-violent Attempt | 98/1002 | 7.9*** (6.5, 9.7) | 4/117 | 4.8** (1.8, 12.7) |
| Violent Attempt | 16/1106 | 13.3*** (8.1, 21.9) | 0/116 | ne |
p<0.05
p<0.01
p<0.0001
ne=not able to be estimated
Cells with fewer than 1-3 cases are identified as <4
Significant hazard ratio statistics (p < .05) are highlighted in bold.
Females
In females, any eating disorder predicted a significantly higher hazard for death, suicide attempt, and both non-violent suicide attempt and violent suicide attempt compared with referents with no eating disorders. The only exceptions to this general pattern were the hazard ratios for death in those with narrow AN and with EDNOS which could not be estimated due to sparse counts. The risk of violent suicide attempt was particularly elevated in females with broad AN (8.6 times greater hazard), narrow AN (7.3 times greater hazard), BN (13.9 times greater hazard) and EDNOS (13.3 times greater hazard) compared with the referent females with no eating disorders.
Males
In males, BN and EDNOS predicted a higher hazard for suicide attempt overall (7.4 and 4.6 higher hazard, respectively) and non-violent suicide attempt (7.4 and 4.8 higher hazard, respectively) compared with referent males with no eating disorders. However, a number of the hazard ratios could not be estimated due to zero instances of the outcome. Moreover, there was no significant association between AN, broad or narrow, and suicide attempts in males.
Discussion
With a total sample of 966,141 and a follow-up period of 15 years, the present study represents one of the largest and longest studies of eating disorder incidence and mortality in adolescence and young adulthood.
Eating Disorders in Females
The incidence rates of narrow AN, BN, and EDNOS in females were directly comparable to medical surveillance estimates reported in other northern European countries (Smink et al., 2012; van Son et al., 2006). However, when the diagnostic criteria were relaxed for broad AN to include individuals with atypical AN (not including <85% of ideal weight and amenorrhea as criteria), the incidence rates were appreciably higher (6.05-11.65 per 10,000 person years vs. 4.5-7.8).
Eating Disorders in Males
The incidence rate of AN in males in Denmark was also directly comparable to estimates in the Netherlands with fewer than 1 per 10,000 person years, regardless of whether the diagnostic criteria used were narrow or broad. Given that amenorrhea is not a criterion for males, broadening the AN criteria led to few additional cases being captured. Other studies that have examined the incidence of BN and EDNOS in males use a different metric reporting incidence per 100,000 persons rather than person-years, rendering direct comparison impossible across these studies (Currin et al., 2005; Micali et al., 2013).
Developmental Trends in Eating Disorder Incidence in Females and Males
As in previous studies, the incidence of eating disorders in Denmark increased sharply during adolescence (Hudson et al., 2007). Psychiatric disorders commonly emerge during adolescence, a time of life marked by intense physiological and psychological change (Kessler et al., 2005). Relevant to eating disorders, the physiological changes associated with puberty including elevated body fat may lead to increased body dissatisfaction in cultures that promote a thin-ideal (Stice, 2002). In turn, initiation of dieting behavior increases risk for eating psychopathology (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). In addition, pubertal hormones have an organizational effect on symptoms of anxiety, depression, eating behavior, and weight (Zehr, Culbert, Sisk, & Klump, 2007). Although there are nominal genetic effects for disordered eating in pre-pubertal twins, there are significant genetic effects for female pubertal and young adult twins (Culbert, Burt, McGue, Iacono, & Klump, 2009). In females, ovarian hormones, particularly estradiol, and the consequent increase in body fat and weight during the pubertal transition trigger heightened weight and shape concerns and disordered eating behaviors (Culbert, Racine, & Klump, 2011). The contribution of ovarian hormones could also explain the consistently reported high ratio of females to males for eating disorders.
Reported anxiety reaches its lifetime peak in adolescence and intense and frequent negative affect also increases abruptly during this period (Abe & Suzuki, 1986; Steinberg, 2005). Neurobiological research suggests that adolescents experience an imbalance in the coupling of their subcortical emotional systems and cortical control regions, which can lead to heightened emotional reactivity especially in those with heightened genetic risk (Casey et al., 2010). Since both anxiety and negative affect have been found to be prospective risk factors for eating disorder behaviors, these developmental changes in brain function may trigger eating disorders in those with higher genetic liability (Allen, Byrne, Forbes, & Oddy, 2009; Stice, 2002).
However, it is unclear why the peak age of eating disorder incidence appears to be younger in males than in females (13 vs. 16 years for AN; 16 vs. 18-22 years for BN). Similar age patterns have also been detected in the Swedish registers (Javaras et al., submitted). Male eating disorders may be detected earlier by parents and medical professionals because rapid weight loss and disordered eating behaviors are more infrequent and aberrant in adolescent males and therefore, more likely to be brought to the attention of the medical system. Body fat in adolescent males is also lower than in adolescent females, so weight loss could be more precipitous and worrying (Goodwin et al., 2013). Alternatively, the psychological, hormonal, and neurobiological triggers for male eating disorder behaviors may be distinct from those for females. Although estradiol does increase in males during the pubertal transition, the levels in girls are higher and it may be overshadowed by increases in other hormones (i.e., testosterone) that have more salient effects (Courant et al., 2010). The nature of weight and shape concerns also differs between males and females (e.g., increased concern with muscularity and leanness rather than an endorsement of the thin ideal) (Murray, Rieger, Karlov, & Touyz, 2013). Given the low incidence rates of eating disorders in males, the use of large national registers such as the Danish register provides an invaluable resource for more fully understanding their development.
In addition, these results also shed light on the incidence of early-onset pre-pubertal eating disorders, as this study one of only a few to examine eating disorder presentations in mid-childhood (Madden, Morris, Zurynski, Kohn, & Elliot, 2009; Nicholls et al., 2011; Pinhas et al., 2011). In girls and boys, incidence rates of broad AN and EDNOS were directly comparable to rates cited in previous medical surveillance studies of restrictive eating and early-onset eating disorders in childhood (Madden et al., 2009; Nicholls et al., 2011; Pinhas et al., 2011). Thus, it provides additional evidence that children in middle childhood present with clinically significant AN and EDNOS diagnoses, which require medical treatment.
Risk for Death and Suicide Attempt
Suicide represents the fourth leading cause of death in adolescence and eating disorders have consistently predicted an increase risk for suicide attempts and deaths (Eaton et al., 2008; Pisetsky, Thornton, Lichtenstein, Pedersen, & Bulik, 2013). In this sample, there was a significantly higher hazard for suicide attempt in all eating disorder groups. Notably, for females in the broad AN category (including both atypical AN and AN) there was an equal risk for suicide attempt. Including atypical AN in a broad AN diagnosis does not attenuate the risk for suicide attempt in adolescent girls and young adult women. Moreover, EDNOS significantly predicted a higher hazard of suicide attempts and conferred just as much risk as a diagnosis of BN, consistent with an emerging perspective on EDNOS as a severe disorder associated with considerable risk for adverse outcomes (Crow et al., 2009; Crow, Swanson, le Grange, Feig, & Merikangas, 2014; Field et al., 2012).
Public Health
In total, these results suggest that a staggered approach to primary prevention may be necessary to prevent eating disorders in both girls and boys. In girls, prevention may need to begin by early adolescence (14-15 years of age) in order to capture the largest number of cases before the peak age of onset of AN, BN, and EDNOS. However, in boys, primary prevention of AN may need to begin even earlier (11-12 years of age), prior to the incidence rate peak at 13 years of age. For secondary prevention, pediatricians and primary care physicians should be vigilant about screening for eating disorders, particularly during adolescence. In addition, programs to educate parents about the early signs and symptoms of eating disorders during adolescence could also divert illness trajectories and ensure adequate early diagnosis and treatment.
Limitations
Since no private psychiatric hospitals exist in Denmark and in contrast to private care, hospital-based treatment is free of charge, the nationwide registration of severe mental disorders is almost complete. However in 2010, 184 specialists in psychiatry and 2115 psychologists were working in private practice, mostly treating anxiety, affective, and personality disorders and possibly treat up to 20% of the cases referred to psychiatric treatment in Denmark. These patients may not be registered in the PCRR.
Incidence rate and prevalence estimates are higher in community samples than primary care and medical records (Milos et al., 2004; van Son et al., 2006). Therefore, cases captured in this study are likely to be an underestimate of community incidence rates and prevalence. Epidemiological studies using hospital-based medical records including psychiatric or outpatient case registers may underestimate eating disorder incidence and prevalence because patients could hide their illness or avoid medical providers (Smink et al., 2012). In addition, incidence rates using medical surveillance capture the age at referral to medical care, which is likely to be later than the age at disorder onset. In European samples, only 25% to 50% of adult patients with eating disorders access treatment (Keski-Rahkonen et al., 2009; Keski-Rahkonen et al., 2007; Preti et al., 2009). Moreover, previous studies have suggested that only a minority of women with BN are detected by primary care or specialized mental health care (Hoek & van Hoeken, 2003). All of the above could result in a bias towards underestimating incidence rates and detecting patients with more severe illness in the present study. In addition, although we were unable to examine incidence rates in individuals older than 24 years of age using the Danish Registers, incident cases of eating disorders do appear after 24 years of age and the period of incident risk can extend throughout the lifespan.
Summary
In sum, the present study represents one of the largest and longest studies of eating disorder incidence and mortality in adolescence and young adulthood. The Danish registers provide insight into the developmental course of eating disorders and additional evidence that eating disorders are severe mental illnesses associated with increased risk for suicide and death.
Highlights.
Adolescence represents a high-risk period for the onset of eating disorders.
For AN, the peak age of risk was earlier for males than females (13 vs. 15 years).
Broadening AN criteria leads to increased rates of incidence for AN in females.
Broadening AN criteria does not attenuate morbidity and mortality.
Eating disorders significantly increase the hazard for suicide attempts and deaths.
Acknowledgments
Dr. Zerwas is supported by a NIMH training grant (K01MH100435). This research was supported by the Anorexia Nervosa Genetics Initiative (ANGI), an initiative of the Klarman Family Foundation.
Role of the funding source
This research was supported by the Anorexia Nervosa Genetics Initiative (ANGI), an initiative of the Klarman Family Foundation. Dr. Zerwas was supported by Dr. Zerwas is supported by a NIMH training grant (K01MH100435). The authors had sole responsibility for the study design, data analysis, data interpretation, writing of the report, and decision to submit the article for publication. Data were collected by the Danish Psychiatric Central Research Register (PCRR) and Danish National Patient Register (NPR).
Footnotes
Conflict of interests
Dr. Bulik is a consultant for Shire Pharmaceuticals.
References
- Abe K, Suzuki T. Prevalence of some symptoms in adolescence and maturity: social phobias, anxiety symptoms, episodic illusions and idea of reference. Psychopathology. 1986;19(4):200–205. doi: 10.1159/000284448. [DOI] [PubMed] [Google Scholar]
- Allen KL, Byrne SM, Forbes D, Oddy WH. Risk factors for full- and partial-syndrome early adolescent eating disorders: a population-based pregnancy cohort study. J Am Acad Child Adolesc Psychiatry. 2009;48(8):800–809. doi: 10.1097/CHI.0b013e3181a8136d. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Press; 2000. Text Revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. Washington, DC: American Psychiatric Press; 2013. Text Revision. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry. 2006;63(3):305–312. doi: 10.1001/archpsyc.63.3.305. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Levita L, Libby V, Pattwell SS, Ruberry EJ, Somerville LH, et al. The storm and stress of adolescence: insights from human imaging and mouse genetics. Dev Psychobiol. 2010;52(3):225–235. doi: 10.1002/dev.20447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courant F, Aksglaede L, Antignac JP, Monteau F, Sorensen K, Andersson AM, Bizec BL, et al. Assessment of circulating sex steroid levels in prepubertal and pubertal boys and girls by a novel ultrasensitive gas chromatography-tandem mass spectrometry method. J Clin Endocrinol Metab. 2010;95(1):82–92. doi: 10.1210/jc.2009-1140. [DOI] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry. 2009;166(12):1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Crow SJ, Swanson SA, le Grange D, Feig EH, Merikangas KR. Suicidal behavior in adolescents and adults with bulimia nervosa. Compr Psychiatry. 2014 doi: 10.1016/j.comppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Culbert KM, Burt SA, McGue M, Iacono WG, Klump KL. Puberty and the genetic diathesis of disordered eating attitudes and behaviors. J Abnorm Psychol. 2009;118(4):788–796. doi: 10.1037/a0017207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Racine SE, Klump KL. The influence of gender and puberty on the heritability of disordered eating symptoms. Curr Top Behav Neurosci. 2011;6:177–185. doi: 10.1007/7854_2010_80. [DOI] [PubMed] [Google Scholar]
- Currin L, Schmidt U, Treasure J, Jick H. Time trends in eating disorder incidence. Br J Psychiatry. 2005;186:132–135. doi: 10.1192/bjp.186.2.132. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Prevention. Youth risk behavior surveillance--United States, 2007. MMWR Surveill Summ. 2008;57(4):1–131. [PubMed] [Google Scholar]
- Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB. Diagnostic crossover in anorexia nervosa and bulimia nervosa: implications for DSM-V. Am J Psychiatry. 2008;165(2):245–250. doi: 10.1176/appi.ajp.2007.07060951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favaro A, Caregaro L, Tenconi E, Bosello R, Santonastaso P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J Clin Psychiatry. 2009;70(12):1715–1721. doi: 10.4088/JCP.09m05176blu. [DOI] [PubMed] [Google Scholar]
- Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, Horton NJ, et al. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012;130(2):e289–295. doi: 10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin K, Syme C, Abrahamowicz M, Leonard GT, Richer L, Perron M, Pausova Z, et al. Routine clinical measures of adiposity as predictors of visceral fat in adolescence: a population-based magnetic resonance imaging study. PloS one. 2013;8(11):e79896. doi: 10.1371/journal.pone.0079896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34:383–396. doi: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javaras KN, Runfola CD, Thornton LM, Agerbo E, Birgegård A, Yao S, Bulik CM, et al. Incidence of Healthcare-Detected Eating Disorders in Sweden: A Total Population Study. submitted. [Google Scholar]
- Keski-Rahkonen A, Hoek HW, Linna MS, Raevuori A, Sihvola E, Bulik CM, Kaprio J, et al. Incidence and outcomes of bulimia nervosa: a nationwide population-based study. Psychol Med. 2009;39(5):823–831. doi: 10.1017/S0033291708003942. [DOI] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Hoek HW, Susser ES, Linna MS, Sihvola E, Raevuori A, Rissanen A, et al. Epidemiology and course of anorexia nervosa in the community. Am J Psychiatry. 2007;164(8):1259–1265. doi: 10.1176/appi.ajp.2007.06081388. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- Madden S, Morris A, Zurynski YA, Kohn M, Elliot EJ. Burden of eating disorders in 5-13-year-old children in Australia. Med J Aust. 2009;190(8):410–414. doi: 10.5694/j.1326-5377.2009.tb02487.x. [DOI] [PubMed] [Google Scholar]
- Micali N, Hagberg KW, Petersen I, Treasure JL. The incidence of eating disorders in the UK in 2000-2009: findings from the General Practice Research Database. BMJ Open. 2013;3(5) doi: 10.1136/bmjopen-2013-002646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milos G, Spindler A, Schnyder U, Martz J, Hoek HW, Willi J. Incidence of severe anorexia nervosa in Switzerland: 40 years of development. International Journal of Eating Disorders. 2004;36:118–119. doi: 10.1002/eat.20052. [DOI] [PubMed] [Google Scholar]
- Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7 Suppl):54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- Murray SB, Rieger E, Karlov L, Touyz SW. Masculinity and femininity in the divergence of male body image concerns. J Eat Disord. 2013;1:11. doi: 10.1186/2050-2974-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. J Am Diet Assoc. 2011;111(7):1004–1011. doi: 10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls DE, Lynn R, Viner RM. Childhood eating disorders: British national surveillance study. Br J Psychiatry. 2011;198(4):295–301. doi: 10.1192/bjp.bp.110.081356. [DOI] [PubMed] [Google Scholar]
- Organization, World Health. International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2. Geneva: World Health Organization; 2005. [Google Scholar]
- Pedersen CB, Gotzsche H, Moller JO, Mortensen PB. The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull. 2006;53(4):441–449. [PubMed] [Google Scholar]
- Pinhas L, Morris A, Crosby RD, Katzman DK. Incidence and age-specific presentation of restrictive eating disorders in children: a Canadian Paediatric Surveillance Program study. Arch Pediatr Adolesc Med. 2011;165(10):895–899. doi: 10.1001/archpediatrics.2011.145. [DOI] [PubMed] [Google Scholar]
- Pisetsky EM, Thornton LM, Lichtenstein P, Pedersen NL, Bulik CM. Suicide attempts in women with eating disorders. J Abnorm Psychol. 2013;122(4):1042–1056. doi: 10.1037/a0034902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti A, Girolamo Gd, Vilagut G, Alonso J, Graaf Rd, Bruffaerts R, et al. Investigators, E. SEMeD-WMH. The epidemiology of eating disorders in six European countries: results of the ESEMeD-WMH project. J Psychiatr Res. 2009;43(14):1125–1132. doi: 10.1016/j.jpsychires.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14(4):406–414. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltanian AR, Hossein M. A non-parametric method for hazard rate estimation in acute myocardial infarction patients: kernel smoothing approach. J Res Health Sci. 2012;12(1):19–24. [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Steinberg L. Cognitive and affective development in adolescence. Trends Cogn Sci. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Sullivan PF. Mortality in anorexia nervosa. Am J Psychiatry. 1995;152(7):1073–1074. doi: 10.1176/ajp.152.7.1073. [DOI] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68(7):714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Son GE, van Hoeken D, Bartelds AI, van Furth EF, Hoek HW. Time trends in the incidence of eating disorders: a primary care study in the Netherlands. Int J Eat Disord. 2006;39(7):565–569. doi: 10.1002/eat.20316. [DOI] [PubMed] [Google Scholar]
- Vandenbroucke JP, Pearce N. Incidence rates in dynamic populations. Int J Epidemiol. 2012;41(5):1472–1479. doi: 10.1093/ije/dys142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TD, Bergin JL, Tiggemann M, Bulik CM, Fairburn CG. Prevalence and long-term course of lifetime eating disorders in an adult Australian twin cohort. Aust N Z J Psychiatry. 2006;40(2):121–128. doi: 10.1080/j.1440-1614.2006.01758.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International Classification of Diseases 10th revised. Geneva: 1992. [Google Scholar]
- Zehr JL, Culbert KM, Sisk CL, Klump KL. An association of early puberty with disordered eating and anxiety in a population of undergraduate women and men. Horm Behav. 2007;52(4):427–435. doi: 10.1016/j.yhbeh.2007.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


