Abstract
Background
It is a struggle to identify the most adaptive coping strategies with disease-mediated stress. Here, we hypothesize that intensity of coping strategies, including denial, in patients with end-stage renal disease (ESRD), varies with type of renal replacement therapy (RRT).
Material/Methods
We enrolled 60 in-center hemodialyzed patients (HD) and 55 patients treated with continuous ambulatory peritoneal dialysis (CAPD). We administered the Coping Inventory with Stressful Situation, Profile of Mood States, and Stroop Anxiety Inventory to measure patient coping strategies in the context of their ESRD. Denial defense mechanism was measured via the IBS-R/ED. The Nottingham Health Profile was used to evaluate self-perceived quality of life. Serum potassium, urea, creatinine, phosphorus, calcium, albumin, and hematocrit were utilized as the measurements of adequacy of dialysis.
Results
HD patients had higher self-reported intensity of denial mechanism and avoidance-oriented strategies versus CAPD patients. Because a single strategy is almost never employed, we conducted cluster analysis. We identify 3 patterns of coping strategies using cluster analysis. “Repressors” employed denial and avoidance strategies and were predominant in HD. The second cluster consists of subjects employing predominantly task-oriented strategies with equal distribution among dialyzed patients. The third cluster encompassed a small group of patients who shared higher intensity of both denial and task-oriented strategies. Health-related outcome, anxiety, and mood profile were similar across all patients.
Conclusions
HD patients predominantly used “repressive” strategies. Patients on RRT utilized denial and avoidance-based strategies to achieve satisfactory outcome in terms of perceived quality of life. We conclude that these coping mechanisms that were previously thought to be inferior are beneficial to patient compliance with RRT.
Keywords: Anxiety; Denial (Psychology); Kidney Failure, Chronic; Personality Disorders; Personality Disorders; Renal Replacement Therapy
Background
End-stage renal disease (ESRD) imposes a severe stress on patients [1–3]. Severe diet restriction, extensive drug regimen, and very strict schedule of dialysis are among most significant stressors. Renal replacement therapy (RRT) can be performed in 2 main ways: hemodialysis or continuous ambulatory peritoneal dialysis [4]. Hemodialysis (HD) relies on a patient visiting a specialized center to use an “artificial kidney” 3 times per week for 4–6 hours. During HD, the patient rests while the automated process removes products of metabolism from the blood using a large-bore needle placed in a surgically created arterio-venous fistula. Alternatively, continuous ambulatory peritoneal dialysis (CAPD) can be implemented. CAPD relies on daily fluid dialysis exchanges in the patient’s abdomen via a pre-implanted catheter. Follow-up treatment is done at home by the patient. Even a brief description of these two modalities of RRT suggests that different psychological challenges and outcomes are encountered by patients.
Researchers studying interactions between disease-mediated stress and coping process struggle to identify which coping strategies are most adaptive [3]. Traditionally, strategies oriented at instrumental coping with disease-related stress are perceived most favorably from adaptation to the therapy [5–7]. Conversely, emotional-oriented strategies are considered inferior [5,8,9]. Denial is perceived as the least adaptive strategy to cope with illness-related stress. However, emotion-oriented strategies can be important since anxiety, depression, and hostility significantly affect patients’ self-perceptions, adherence to treatment, and health-related quality of life [10,11]. Avoidance and denial are focused on dealing with negative emotions [12–14]. Some suggest that utilization of emotion-based techniques is inferior because they focus on emotion, not the process of therapy. However, no clear connection between emotional-oriented strategies and somatic outcome has been identified. It is likely that situational context may be responsible for variable outcomes. Emotion-oriented strategies are beneficial in situations where a high intensity of negative emotions is present for short periods of time. Reduction in anxiety, depression, and sense of alienation related to being sick support patient adherence to treatment. Denial-related distortion in perception of health-related issues can affect optimal functioning in RRT [6,9,10]. A very good understanding of their health condition and compliance to a strict medical regiment is paramount for their survival. This is a different context compared to psoriasis, lupus, coronary artery disease, or spinal cord injury [8,11,15,16]. In the case of chronic disease, optimal coping should deal with the emotional aftermath of the illness, allowing patients to fully adhere to treatment. Nevertheless, the negative perception of medical professionals of emotion-oriented, avoidance, and denial-oriented strategies persevere.
Few studies related to denial mechanism in ESRD have been published. Jadoulle et al. showed that denial is related to improved emotional status in HD [17]. Concomitantly, patients with high activation of denial had decreased compliance with treatment. A similar observation was made by Kohli et al. [17,18]. No study has been published comparing denial and other emotion-based strategies in coping with stress between the 2 different modalities of RRT to date.
The overarching aim of the present study was to determine whether emotion-centered strategies in dealing with chronic stress are truly detrimental to patient somatic and psychological well-being. Thus, we specifically explored the role of denial in patients with ESRD, treated with the 2 different modalities of RRT. Both therapies present very different challenges to the patients, necessitating different strategies. We hypothesized that HD will result in more frequent use of denial versus CAPD. Furthermore, we suggest that increased activity of denial and avoidance-oriented strategies should correlate with positive emotional outcome and negative outcome of dialysis compliance and performance, as suggested by prior reports.
Material and Methods
The present study was designed as a cross-sectional cohort study and is a part of the Psychological Assessment of Patients with ESRD program. Our institution’s Ethics Committee approved the study.
The study population consisted of chronic, in-center hemodialyzed patients (HD; n=60), and patients treated with continuous ambulatory peritoneal dialysis (CAPD; n=55) in the Military Medical Institute. All patients were screened by an in-hospital psychologist, independent from the primary investigator, to exclude subjects with cognitive impairment. To ensure that the patients were settled into the routine of RRT, the interviews were performed at least 3 months after the onset of RRT. Patients below the age of 21 years and with history of recent kidney transplantation were excluded from the study. The interviews with CAPD patients took place during routine hospitalization, whereas HD patients were examined while undergoing dialysis. After explaining the aim of the study, the examinee was asked to fill out a series of questionnaires according to the attached instructions. These instructions directed the examinee to keep in mind the ESRD context while answering the questionnaires. A psychologist supervised each subject throughout the study.
Sex, age, level of education, duration of the underlying disease leading to ESRD, and duration of RRT were collected. Serum potassium, urea, creatinine, phosphorus, and calcium were utilized as the measurements of adequacy of dialysis. Total albumin and hematocrit values assessed clinical well-being of the patients [19]. The total change in body weight over 1 week was used as a sensitive measurement of patient compliance with treatment [20]. All laboratory values were collected 1 week before the interview.
The process of coping was assessed with the Coping Inventory with Stressful Situation (CISS). The CISS describes the coping process in 3 dimensions of task-, emotion-, and avoidance-oriented coping [13,14,21,22]. The intensity of denial defense mechanism as described by Spielberger was used in this study [23,24]. Several instruments were used to evaluate psychological outcomes of coping with stress in different modalities of RRT. The State and Trait Anxiety Inventory (STAI) has a similar structure to the CISS, with the first part measuring baseline anxiety and the second part of the questionnaire was modified to assess ESRD-related anxiety [22,25]. The baseline anxiety is a trait of one’s personality [9,12]. Mood, a pervasive emotional state, was evaluated by the Profile of Mood States (POMS) [12,26,27], which is the World Health Organization-recommended questionnaire for study of emotional outcomes of various medical therapies. It describes mood in 6 dimensions: Tension/Anxiety, Depression/Dejection, Anger/Hostility, Vigor/Activity, Fatigue/Inertia, and Confusion/Bewilderment [27]. To measure a layman perception of the health-related quality of life (HRQoL), the Nottingham Health Profile (NHP) was employed [6,28]. NHP appraises 6 dimensions of HRQoL: energy, pain, sleep, emotional reactions, mobility limitations, and social isolation. The psychometric features of the employed psychological tests have been found to be satisfactory in prior investigations [7,26,29,30].
Statistical analysis was done in a step-wise approach. For categorical variables, the Pearson χ2 test was applied. The Shapiro-Wilk W test and distribution plots were used to test normality of distribution for intervals. Parametric variables are expressed as mean ±SD. These variables were compared using the t test or ANOVA with LSD post hoc tests. For non-parametric variables, median (Me) and interquartile ranges (IR) were shown. The Mann-Whitney U test was employed to compare such variables. The r2-Pearson momentum and multiple regression with stepwise forward method were calculated for some analyses. A double-sided p value less than 0.05 was considered statistically significant for all tests. Clustering procedures were done with k-means. Statistical analyses were performed with the Statistica 8.0 software (StatSoft Inc., Tulsa, OK).
Result
Demographic variables
A total of 60 HD and 55 CAPD patients were enrolled in the study. There was no difference between HD ad CAPD groups in employment or gender (Table 1). We recruited a total of 52 males and 63 females to the study. There was no difference in the sex distribution in the studied RRT groups. The CAPD subjects (49.6±13.56 y/o) tended to be slightly younger vs. HD patients (55.3±13.33 y/o). Most of our subjects in both RRT groups were employed (68% in the HD group vs. 76% in the CAPD group). No difference in duration of ESRD, duration of RRT, baseline laboratory values were seen between studied groups (Table 1). The underlying etiology for ESRD was diabetes (46%), hypertension (22%), autoimmune, inherited renal diseases (12%), or others (20%).
Table 1.
Demographic and clinical variables among studied groups.
| HD | CAPD | p | ||
|---|---|---|---|---|
| Sex | Males | 27 | 25 | NS |
| Females | 33 | 30 | ||
| Age | 55.3±13.33 | 49.6±13.56 | 0.017 | |
| Employment | Employed | 41 | 42 | NS |
| Unemployed | 19 | 13 | ||
| Education | Elementary | 10 | 14 | NS |
| High School | 29 | 28 | ||
| Undergraduate and above | 21 | 13 | ||
| Duration of ESRD [years] | 10.4±8.73 | 10.3±7.75 | NS | |
| Duration of RRT [months] | 23.1±25.7 | 25.9±26.01 | NS | |
| Hematocrit [%] | 30.9±3.09 | 30.6±3.52 | NS | |
| Albumin [g/dL] | 3.4±0.57 | 3.2±0.44 | NS | |
| Potassium [mg/dL] | 5.1±0.65 | 4.9±0.81 | NS | |
| Calcium [mg/dL] | 8.8±0.97 | 8.9±1.02 | NS | |
| Phosphorus [mg/dL] | 6.1±1.98 | 6.4±1.86 | NS | |
| Creatinine [mg/dL] | 9.5±1.89 | 10.0±2.94 | NS | |
| Urea [mg/dL] | 140.1±41.09 | 135.6±38.77 | NS | |
| Inerdialytic weight change [kg] | 2.1±0.88 | 2.3±0.96 | NS | |
p – level of statistical significance; NS – not statistically significant comparisons; HD – hemodialysed patients; CAPD – continuos peritoneal dialysis; ESRD – end stage renal disease; RRT – renal replacement therapy.
Intensity of defense mechanisms
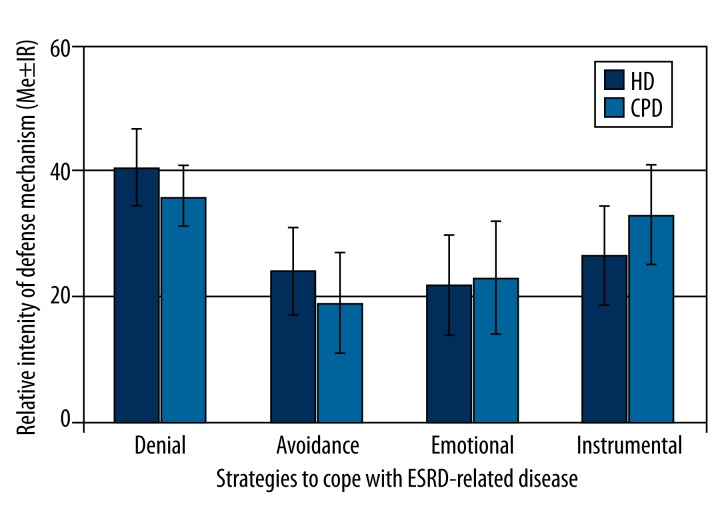
Following the main hypothesis, we studied the coping mechanisms involved in dealing with ESRD-related stress. HD patients had higher self-reported intensity of denial mechanism compared to the CAPD group (Figure 1). Avoidance-oriented strategies were also more pronounced in the HD group, whereas task-oriented strategies where more prevalent in CAPD subjects (Figure 1). Of note, utilization of avoidance-oriented strategies was related to the level of education when univariate general linear model of ANOVA was analyzed (data not shown). Emotion-oriented strategies had similar intensity in both RRT groups. Again, there was significant interaction between modality and education. Subjects with elementary or higher education level had higher intensity of avoidance-oriented strategies in the hemodialyzed group. In contrast, CAPD subjects utilized avoidance-oriented strategy similarly, regardless of their education. Employment of avoidance-oriented strategies was generally less frequent in the CAPD group as compared to HD patients (Figure 1).
Figure 1.
Intensity of defense mechanism in studied populations of ESRD patients.
Intensity of denial did not correlate with intensity of any other strategies to cope with disease when controlled for modality of RRT (data not shown). Interestingly, age correlated positively with higher intensity of denial mechanism (r=0.28;p=0.008). Also, length of RRT was weakly correlated (r=0.21;p<0.05) with intensity of avoidance strategies.
An individual usually engages in several strategies simultaneously in order to optimally cope with all aspects of stress. Thus, we conducted a cluster analysis in order to distinguish the potential patterns. Three clusters were separated (Table 2). Cluster 1 involved patients with employing predominantly denial as defense mechanism. They also had the highest intensity of avoidance-oriented strategies. Consequently, the individuals from this group were called “repressors”. Cluster 2 consisted of subjects predominantly using task-oriented strategies. Cluster 3 encompassed a small group of patients who shared both higher intensity of denial- and task-oriented strategies.
Table 2.
Clusters of coping styles in studied population.
| Cluster | |||
|---|---|---|---|
| #1 (repressors) | #2 | #3 | |
| Number of subjects (HD & CAPD) | 54 (n=42HD & n=12 CAPD) | 57 (n=18HD & n=39 CAPD) | 4 (only n=4 CAPD) |
| Task-oriented coping with ESRD | 24 | 34 | 37 |
| Emotion-oriented coping with ESRD | 21 | 24 | 24 |
| Avoidance-oriented coping with ESRD | 24 | 19 | 19 |
| Intensity of denial defense mechanism | 39 | 22 | 37 |
| Tension and anxiety | 15.3±6.08 | 14.7±6.96 | 10.8±3.30 |
| Depression and dejection | 18.35±11.34 | 24.7±12.31 | 11.8±6.02 |
| Tension and anxiety | 13.3±9.64 | 15.0±8.25 | 9.5±4.93 |
| Vigor and activity | 15.2±6.72 | 15.2±6.19 | 14.8±3.78 |
| Fatigue and inertia | 11.0±5.15 | 9.3±4.32 | 5.3±1.71 |
| Confusion and bewilderment | 11.1±5.41 | 11.3±5.50 | 9.0±3.46 |
| ESRD – anxiety | 42.2±7.52 | 45.8±11.96 | 51.5±2.52 |
| Duration of ESRD | 11.0±8.62 | 9.9±8.13 | 7.5±1.92 |
| Duration of RRT | 27.3±29.1 | 20.3±19.85 | 43±41.8 |
| Energy | 33.3±39 | 22.4±40 | 16.5±33 |
| Pain | 12.5±31 | 12.5±38 | 18.75±31 |
| Emotional reaction | 11.1±33 | 22.2±33 | 11.1±50 |
| Sleep disturbances | 20±50 | 20±45 | 20±60 |
| Social alienation | 20±20 | 0±15 | 20±20 |
| Movement limitations | 12.5±30 | 12.5±25 | 12.5±25 |
HD – hemodialysed patients; CAPD – continuos peritoneal dialysis; ESRD – end stage renal disease; RRT – renal replacement therapy.
Correlations of psychological outcomes with coping
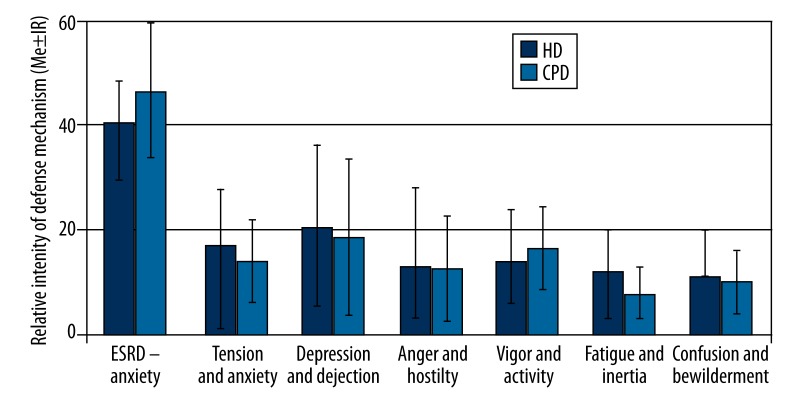
In the next step, emotional profiles were analyzed (Figure 2). HD patients were more anxious when referring to their medical condition, having less Vigor&Activity and more Fatigue&Inertia. There were significant correlations between emotion-oriented coping style and mood of Depression&Dejection (r=0.4) and Confusion&Bewilderment (r=0.3) in HD patients. In contrast, in CAPD patients the intensity of denial correlated with ESRD anxiety (r=−0.35), emotion-oriented coping style with the mood of Anger&Hositlity. No difference in mood profile and level of ESRD-related anxiety was seen between the 3 previously distinguished clusters of disease coping styles.
Figure 2.
Different emotional profiles in CAPD vs. HD patients.
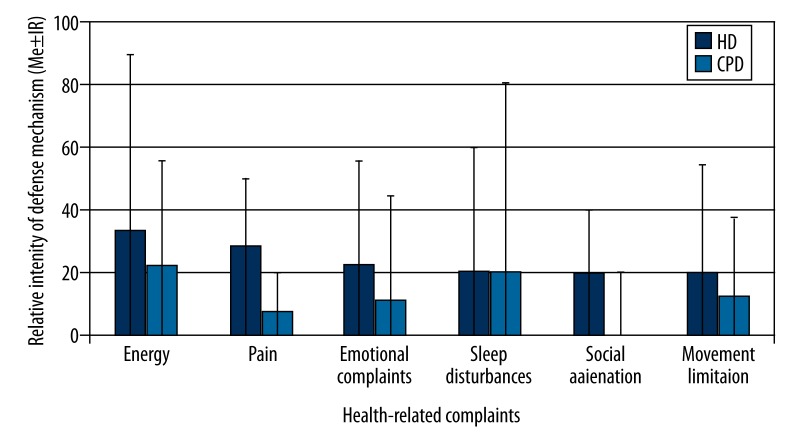
Health-related quality of life was significantly less favorable in HD vs. CAPD patients in the area of energy, pain, sleep disturbances, and social alienation (Figure 3). Only emotional-oriented style of coping with ESRD-related stress correlated with emotional disturbances (r=0.34) in HD patients, whereas no correlations were seen between patients in the CAPD group. No difference was seen between clusters of coping styles in intensity of health-related problems.
Figure 3.
A comparison of HRQoL among studied subjects.
Relationship between somatic measures and coping styles
In the last analysis we decided to test the hypothesis that different styles of coping are related to worse somatic outcome of treatment. There was a weak correlation between intensity of denial and serum creatinine levels in HD patients (r=0.25). There was a significant correlation between ESRD anxiety and serum level of creatinine (r=0.33), urea (r=0.26), phosphorus (r=0.49), and interdialytic weight gain (r=0.41). There was no correlation between denial, styles of coping with ESRD-related stress, and serum markers of adherence (potassium, urea, creatinine, or interdialytic weight gain). When patients were analyzed according to the cluster models, significantly higher levels of serum potassium were found in the repressor cluster vs. other clusters. Other measures of somatic well-being were not different between the studied groups (Table 1).
Discussion
In the present study we investigated the coping mechanisms of ESRD-related stress with a special emphasis on denial and emotional-related strategies in 2 different modalities of RRT. We found that in HD patients, denial and avoidance strategies are more pronounced than in CAPD patients. Moreover, CAPD patients self-reported employing task-oriented strategies more frequently.
We showed that patients can be clustered depending on the spectrum of coping strategies they use to deal with ESRD stress. Denial is a very important part of the coping process [3,12,23,24,31]. Relatively high use of the avoidance strategies in HD patients has been described before, but our study showed that patients use this strategy in conjunction with denial [17,18]. HD patients may prefer to choose emotion-based strategies since they may be more suited for overall well-being [3,4]. In contrast, the nature of CAPD treatment promotes problem-oriented coping strategies. The other explanation for more frequent use of denial and avoidance in the HD group is perception of the locus of control [3,12,17,18]. It is likely that internal locus of control is related to more frequent use of emotional strategies vs. external locus of control, which may be related to problem solving. This is consistent with study by Kohli et al. showing that most HD patients had an internal source of control compared to healthy subjects [18]. No study involving CAPD patients is available.
Our study results need to be interpreted carefully because of inherited selection bias. CAPD patients are frequently selected before admission to the program based on their ability and willingness to perform in-home treatment. This may be a point at which only patients with certain psychological make-up are selected. The remaining patients are transferred into hemodialysis programs. This decision is made by the psychologist and medical team. Also, patients with maladaptive strategies have higher mortality because low compliance with CAPD results in complications like peritonitis [7,17,18,24,31]. These are sources of bias that are frequently overlooked and very difficult to control. The patients we studied were all well into their dialysis programs, yet we were able to discern patients who were “repressors”.
Use of the coping strategies based on denial and avoidance is more prevalent in the HD patients with lower education. This is related to the fact that patients with higher education usually have a broader spectrum of coping strategies [9,31]. Avoidance and denial are relatively primitive and immature mechanisms for ego defence in contrast to humor, focusing on the task, or positive reappraisal [15,23]. Again, it is commonly believed that using these emotional strategies is detrimental to patient health [11,15,16]. This seemingly logical way of thinking stemmed from the perception that patients must comply with treatment. At the same time, this way of thinking neglects the fact that patients have to cope with the emotional burden of disease. If such a burden exceeds the capacity of the patient to cope, the anxiety overwhelms the patient and prohibits effective medical therapy [10,17,18]. Studies in other clinical situations show that denial is an effective and desirable way to go through life with disease. Rehabilitation of male cardiac patients is related to high employment of denial as compared to female cardiac patients [32]. Despite higher incidence of denial, the outcomes were better in males than in females. This finding is attributed to the fact that cultural norms force both genders to fulfil certain roles while sick. Using denial is an optimal way to cope with stress related to disease, rehabilitation, and cultural expectations. Similar finding were seen in spouses of patient with myocardial infarction [33]. However, this is not a uniform finding, as shown in a meta-analysis [34]. Oncology patients frequently use denial. Again, the perception is that it is detrimental to individual health, yet not all data support this idea [35,36]. Our study shows that health-related quality of life, emotional status, and somatic measures of well-being were not dramatically different between studied groups. The lack of differences in outcome is in contrast to sharp differences in use of denial. One of the purposes of our study was to challenge the existing idea that denial is a negative and undesirable coping mechanism. One has to realize that the denial mechanism can also be detrimental to individual well-being. Schizophrenic patients have a variety of issues, but denial is an important mechanism in preventing them from adequately assessing their level of perception [37,38]. Also, in some other clinical scenarios, use of avoidance and denial has undesirable effect on patient outcomes.
Use of certain coping strategies was linked to a specific emotional profile, but our study does not allow concluding whether employment of certain coping strategies is a result or a product of the coping process. Coping strategies are preferential ways of dealing with stress in general by the individual. These coping strategies are chosen to best suit the patient’s personality and psychosomatic background in which the patient is immersed [31]. The ultimate outcome is reduction in anxiety and satisfactory heath-related measures; all our patients achieved that, regardless the type of RTT. This suggests that patients reach an equilibrium or optimal point while negotiating several aspects of their illness. This “equilibrium point” is perhaps best for the patient but it may seem suboptimal to the medical staff, leading to the conclusion that denial is maladaptive [38–40]. There is also an interesting notion that denial is an “organic” process related to the processing of information and emotion by the left hemisphere of the brain [41]. This would shed new light on the origin of the denial process as a feature of the individual. Therefore, medical therapy should tailored accordingly.
Conclusions
In context of our study, denial and avoidance mechanism are not seen as maladaptive. The purpose of RRT is extension of patient life and to provide maximal health-related quality of life. Denial and avoidance strategies are beneficial for some individuals, especially if they are unable to employ more mature coping strategies. This strategy is especially beneficial if the patient is unable to control the situation or if the patient perceives an external locus of control.
This conclusion is corroborated by an observation of Kohli et al. [18]. Others have observed this phenomenon in other patient populations, including heart attack, oncology, and psychiatric disorders [33–35,40]. The ability of the individual to cope with the whole spectrum of illness (somatic, psychological, and social) should determine the optimal ways to cope with disease. If denial is the optimal way to achieve this, it should not be stigmatized as a suboptimal way to cope with illness.
Acknowledgments
Authors of this manuscript would like to thank Kazimierz Wrześniewski for help in creating this study.
Footnotes
Source of support: Departmental sources
References
- 1.Avramovic M, Stefanovic V. Health-related quality of life in different stages of renal failure. Artif Organs. 2012;36(7):581–89. doi: 10.1111/j.1525-1594.2011.01429.x. [DOI] [PubMed] [Google Scholar]
- 2.Wu AW, Fink NE, Marsh-Manzi JV, et al. Changes in quality of life during hemodialysis and peritoneal dialysis treatment: generic and disease specific measures. J Am Soc Nephrol. 2004;15(3):743–53. doi: 10.1097/01.asn.0000113315.81448.ca. [DOI] [PubMed] [Google Scholar]
- 3.Griva K, Jayasena D, Davenport A, et al. Illness and treatment cognitions and health related quality of life in end stage renal disease. Br J Health Psychol. 2009;14(Pt 1):17–34. doi: 10.1348/135910708X292355. [DOI] [PubMed] [Google Scholar]
- 4.Laudanski K, Nowak Z, Wankowicz Z. Psychological aspects of dialysis: does cognitive appraisal determine the overall outcome. Pol Arch Med Wewn. 2010;120(1–2):49–52. [PubMed] [Google Scholar]
- 5.Pucheu S, Consoli SM, D’Auzac C, et al. Do health causal attributions and coping strategies act as moderators of quality of life in peritoneal dialysis patients? J Psychosom Res. 2004;56(3):317–22. doi: 10.1016/S0022-3999(03)00080-1. [DOI] [PubMed] [Google Scholar]
- 6.Valderrabano F, Jofre R, Lopez-Gomez JM. Quality of life in end-stage renal disease patients. Am J Kidney Dis. 2001;38(3):443–64. doi: 10.1053/ajkd.2001.26824. [DOI] [PubMed] [Google Scholar]
- 7.Wrzesniewski K, Wlodarczyk D. The role of cognitive appraisal in coping with myocardial infarction: selected theoretical and practical models. Pol Psych Journal. 2001;32(2):18–26. [Google Scholar]
- 8.Mackay J, Charles ST, Kemp B, Heckhausen J. Goal striving and maladaptive coping in adults living with spinal cord injury: associations with affective well-being. J Aging Health. 2011;23(1):158–76. doi: 10.1177/0898264310382039. [DOI] [PubMed] [Google Scholar]
- 9.Austenfeld JL, Stanton AL. Coping through emotional approach: a new look at emotion, coping, and health-related outcomes. J Pers. 2004;72(6):1335–63. doi: 10.1111/j.1467-6494.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- 10.Cukor D, Coplan J, Brown C, et al. Anxiety disorders in adults treated by hemodialysis: a single-center study. Am J Kidney Dis. 2008;52(1):128–36. doi: 10.1053/j.ajkd.2008.02.300. [DOI] [PubMed] [Google Scholar]
- 11.Bricou O, Taieb O, Baubet T, et al. Stress and coping strategies in systemic lupus erythematosus: a review. Neuroimmunomodulation. 2006;13(5–6):283–93. doi: 10.1159/000104856. [DOI] [PubMed] [Google Scholar]
- 12.Ekman P, Davidson RJ. The nature of emotion: fundamental questions. New York: Oxford University Press; 1994. [Google Scholar]
- 13.Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990;58(5):844–54. doi: 10.1037//0022-3514.58.5.844. [DOI] [PubMed] [Google Scholar]
- 14.Endler NS, Parker JD, Butcher JN. A factor analytic study of coping styles and the MMPI-2 content scales. J Clin Psychol. 1993;49(4):523–27. doi: 10.1002/1097-4679(199307)49:4<523::aid-jclp2270490409>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 15.Awadalla FC, Yentzer B, Balkrishnan R, Feldman SR. A role for denial in poor adherence to psoriasis treatment. J Dermatolog Treat. 2007;18(6):324–25. doi: 10.1080/09546630701731131. [DOI] [PubMed] [Google Scholar]
- 16.Folks DG, Freeman AM, III, Sokol RS, Thurstin AH. Denial: predictor of outcome following coronary bypass surgery. Int J Psychiatry Med. 1988;18(1):57–66. doi: 10.2190/8dc9-n2en-69qb-7gtn. [DOI] [PubMed] [Google Scholar]
- 17.Jadoulle V, Hoyois P, Jadoul M. Anxiety and depression in chronic hemodialysis: some somatopsychic determinants. Clin Nephrol. 2005;63(2):113–18. doi: 10.5414/cnp63113. [DOI] [PubMed] [Google Scholar]
- 18.Kohli S, Batra P, Aggarwal HK. Anxiety, locus of control, and coping strategies among end-stage renal disease patients undergoing maintenance hemodialysis. Indian J Nephrol. 2011;21(3):177–81. doi: 10.4103/0971-4065.83729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones CH, Newstead CG, Wills EJ, Davison AM. Serum albumin and survival in CAPD patients: the implications of concentration trends over time. Nephrol Dial Transplant. 1997;12(3):554–58. doi: 10.1093/ndt/12.3.554. [DOI] [PubMed] [Google Scholar]
- 20.Lopez-Gomez JM, Villaverde M, Jofre R, et al. Interdialytic weight gain as a marker of blood pressure, nutrition, and survival in hemodialysis patients. Kidney Int Suppl. 2005;(93):S63–68. doi: 10.1111/j.1523-1755.2005.09314.x. [DOI] [PubMed] [Google Scholar]
- 21.Zeidner M, Endler NS. Handbook of coping: theory, research, applications. New York: Wiley; 1996. [Google Scholar]
- 22.Endler NS, Kocovski NL. State and trait anxiety revisited. J Anxiety Disord. 2001;15(3):231–45. doi: 10.1016/s0887-6185(01)00060-3. [DOI] [PubMed] [Google Scholar]
- 23.Swan GE, Carmelli D, Dame A, et al. The Rationality/Emotional Defensiveness Scale – I. Internal structure and stability. J Psychosom Res. 1991;35(4–5):545–54. doi: 10.1016/0022-3999(91)90049-t. [DOI] [PubMed] [Google Scholar]
- 24.Swan GE, Carmelli D, Dame A, et al. The Rationality/Emotional Defensiveness Scale – II. Convergent and discriminant correlational analysis in males and females with and without cancer. J Psychosom Res. 1992;36(4):349–59. doi: 10.1016/0022-3999(92)90071-9. [DOI] [PubMed] [Google Scholar]
- 25.Spielberger CD, Vagg PR. Test anxiety: theory, assessment, and treatment. Washington, DC: Taylor & Francis; 1995. [Google Scholar]
- 26.Dudek B, Koniarek J. Polish Adaptation of POMS. Przegl Psych. 1987;30:753–61. [Google Scholar]
- 27.McNair DM, Lorr M, Droppleman LF. Profile of mood states manual. San Diego, CA: Educational & Industrial Testing Service; 1992. [Google Scholar]
- 28.Coons SJ, Rao S, Keininger DL, Hays RD. A comparative review of generic quality-of-life instruments. Pharmacoeconomics. 2000;17(1):13–35. doi: 10.2165/00019053-200017010-00002. [DOI] [PubMed] [Google Scholar]
- 29.Wrzesniewski K. Polish Adaptation of Nothingham Health Profile. In: Karski JB, Kirschner H, editors. Current options for health measurment. Warsaw: IGP; 1997. pp. 37–42. [Google Scholar]
- 30.Szczepaniak P, Strelau J, Wrzesniewski K. Investigation of coping style using CISS questionnaire. Przegl Psych. 1996;1996(39):1. [Google Scholar]
- 31.Carver CS, Connor-Smith J. Personality and coping. Annu Rev Psychol. 2010;61:679–704. doi: 10.1146/annurev.psych.093008.100352. [DOI] [PubMed] [Google Scholar]
- 32.Modica M, Ferratini M, Spezzaferri R, et al. Gender differences in illness behavior after cardiac surgery. J Cardiopulm Rehabil Prev. 2014;34(2):123–29. doi: 10.1097/HCR.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 33.Salminen-Tuomaala M, Astedt-Kurki P, Rekiaro M, Paavilainen E. Spouses’ coping alongside myocardial infarction patients. Eur J Cardiovasc Nurs. 2013;12(3):242–51. doi: 10.1177/1474515111435603. [DOI] [PubMed] [Google Scholar]
- 34.Covino JM, Stern TW, Stern TA. Denial of cardiac illness: consequences and management. Prim Care Companion CNS Disord. 2011;13(5) doi: 10.4088/PCC.11f01166. pii: PCC.11f01166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keeling M, Bambrough J, Simpson J. Depression, anxiety and positive affect in people diagnosed with low-grade tumours: the role of illness perceptions. Psychooncology. 2013;22(6):1421–27. doi: 10.1002/pon.3158. [DOI] [PubMed] [Google Scholar]
- 36.Arran N, Craufurd D, Simpson J. Illness perceptions, coping styles and psychological distress in adults with Huntington’s disease. Psychol Health Med. 2014;19(2):169–79. doi: 10.1080/13548506.2013.802355. [DOI] [PubMed] [Google Scholar]
- 37.Kruck CL, Flashman LA, Roth RM, et al. Lack of relationship between psychological denial and unawareness of illness in schizophrenia-spectrum disorders. Psychiatry Res. 2009;169(1):33–38. doi: 10.1016/j.psychres.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bedford NJ, David AS. Denial of illness in schizophrenia as a disturbance of self-reflection, self-perception and insight. Schizophr Res. 2014;152(1):89–96. doi: 10.1016/j.schres.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 39.Saks ER. Some thoughts on denial of mental illness. Am J Psychiatry. 2009;166(9):972–73. doi: 10.1176/appi.ajp.2009.09030409. [DOI] [PubMed] [Google Scholar]
- 40.Fortune DG, Smith JV, Garvey K. Perceptions of psychosis, coping, appraisals, and psychological distress in the relatives of patients with schizophrenia: an exploration using self-regulation theory. Br J Clin Psychol. 2005;44(Pt 3):319–31. doi: 10.1348/014466505X29198. [DOI] [PubMed] [Google Scholar]
- 41.Gerretsen P, Menon M, Chakravarty MM, et al. Illness denial in schizophrenia spectrum disorders: A function of left hemisphere dominance. Hum Brain Mapp. 2015;36(1):213–25. doi: 10.1002/hbm.22624. [DOI] [PMC free article] [PubMed] [Google Scholar]