Abstract
Context:
Orofacial and dental trauma continues to be a commonly encountered issue for the sports medicine team. All sports have some risk for dental injury, but “contact sports” presumably incur more risk. Immediate evaluation and proper management of the most common injuries to dentition can result in saving or restoration of tooth structure. Despite the growing body of evidence, mouth guard use and dental protection have not paralleled the increase in sports participation.
Evidence Acquisition:
A PubMed search from 1960 through April 2012 was conducted, as well as a review of peer-reviewed online publications.
Results:
Common dental injuries in sports include tooth (crown) fractures; tooth intrusion, extrusion, and avulsion; and temporomandibular joint dislocation. Mouth guards help prevent most injuries and do not significantly affect ventilation or speech if fitted properly.
Conclusion:
A working knowledge of the presentation as well as management of commonly encountered dental trauma in sports is essential to the immediate care of an athlete and returning to play. Mouth guard use should be encouraged for athletes of all ages in those sports that incur significant risk.
Keywords: sports-related dental injury, tooth fracture, tooth avulsion, mouth guard
The interest and participation in exercise and sports is increasing in the United States and worldwide. As an example, the United Kingdom hoped that the 2012 Olympic Games in London would be a catalyst to increase sport participation by 2 million people.8 With this increased participation comes an increase in risk; although statistics vary, dental and orofacial injuries are common in sport. The result of injury may certainly impact the athlete’s contest and career.32,39 More importantly, orofacial and dental trauma may impact the individual’s life outside of sport as well. Fortunately, many injuries are preventable with the proper equipment. When available, a dentist can be a valuable part of the sports medicine team, helping with acute treatment and return-to-play management of these injuries.
Epidemiology
With approximately 30 million children and adolescents involved in sports annually in the United States, the impact of dental injuries can be significant. Greater than 5 million teeth are avulsed in the United States every year, accruing nearly $500 million in cost for care.39 The cost to treat an avulsed tooth over a lifetime is between $5000 and $20,000.32
Dental injury statistics in sport are difficult to obtain. While several studies report dental injury in up to 80% of participants, others suggest that these injuries are relatively rare, especially in high school sports.6,9,13,38
Basketball, football, hockey, martial arts, and boxing carry the highest risk. However, noncontact sports carry risk as well. In intercollegiate athletes, there was a fivefold increase in risk for dental trauma in basketball compared with football, possibly due to mouth guard protection.9 A New Zealand study of insurance claims for sports-related dental trauma showed rugby led all sports (22%-33%), followed by water sports.42 Basketball and hockey represented only 5% each of insurance claims.42
Orofacial injuries vary, but the most common are soft tissue injuries (eg, lacerations).39 The upper lip, maxilla, and central maxillary incisors are involved in up to 90% of all orofacial and dental trauma.13,39 The majority of dental trauma is tooth (crown) fracture, tooth avulsion, or tooth subluxation.14,20
Anatomy
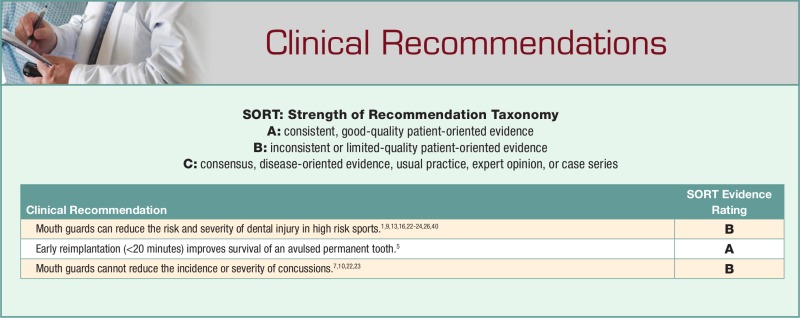
The tooth (Figure 1) is made up of 3 main layers—the enamel, dentin, and pulp. The enamel is the hard outer surface, with the dentin just beneath it and covering the pulp, which contains the neurovascular structures of the tooth. The crown is the portion of the tooth exterior to the gum, while the root is below the gum line. A crown fracture can indicate an injury to the enamel only, the enamel-dentin structures (uncomplicated), or through all 3 layers (complicated fracture) to the pulp. Typically, involvement of the dentin produces temperature and pressure sensitivity, while exposure of the pulp layer will be evident by a bleeding spot. Direct trauma may cause injury to the tooth’s supporting structures, causing instability without displacement (subluxation) or complete displacement of the tooth from its alveolar socket (avulsion). These injuries typically cause bleeding from the gingiva and may cause ankylosis—fusion of the tooth to the alveolar socket secondary to loss (or necrosis) of the periodontal ligament.
Figure 1.
Normal tooth anatomy.
Trauma may additionally cause intrusion, displacement of the tooth into the alveolar socket, or extrusion, partial displacement (without removal) of the tooth from the alveolar socket. These usually produce some axial malalignment (retrusion/protrusion).
Case Presentations
Case 1: Avulsed Teeth
A 22-year-old professional hockey player presented after being hit with a hockey stick during a professional game, sustaining 2 avulsed bicuspid teeth in the right maxilla. After a thorough examination,33,34 including radiographs, it was determined that the teeth may be replantable.
Key Points
Primary teeth should never be replanted; only attempt this with intact, permanent teeth.3,5
Every patient must be evaluated immediately for airway obstruction33 and then the injured area washed with sterile water and dabbed with gauze. Care must be taken to avoid injuring the periodontal ligaments further, so do not aggressively cleanse the area.5
Replantation of an avulsed tooth should ideally occur within 5 to 10 minutes. The risk of ankylosis increases with time out of the alveolar socket. Successful replantation is much less likely after 20 minutes of “extraoral dry time” and highly unlikely after 60 minutes.5
If unable to replant, the intact tooth or tooth remnants should be kept in a storage media such as (in order of preference) Hank’s Balanced Salt Solution, cold milk (skim milk preferably), saliva (inside the patient’s cheek), saline, or water. The storage of any remnant of tooth is also extremely beneficial to the success of functional and esthetic replacement.3,13,34
If the intact tooth has debris, then the tooth should be held by its crown, rinsed with water or normal saline, properly oriented by observing the adjacent teeth, and replanted in the socket.3,5,13,34
Once replanted, the tooth may be splinted using a variety of possible materials. If needed, simple tissue adhesive (cyanoacrylate derivatives) has been shown to be useful in holding a splint in place until definitive treatment.5,13,19,37
Systemic antibiotics are recommended following replantation to aid periodontal and pulpal healing, though evidence-based studies do not clearly establish a benefit.5,18
Return to play should be individualized. For completely avulsed teeth with no chance of replantation, the player could return within 48 hours with mouth guard protection if no bone fractures are evident.5
Players who have replantation and splinting of avulsed teeth should wait at least 2 to 4 weeks to return and only with mouth guard and face mask protection.3,5,19
Tetanus status should be determined and consideration given for booster vaccinations if indicated.5
Case 2
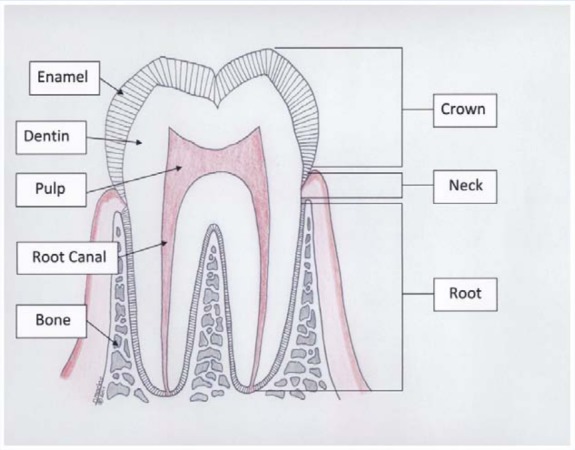
A 21-year-old basketball player suffered a fracture of the maxillary central incisors and a forced displacement of a maxillary lateral incisor tooth after being hit with an elbow during a rebound. After determining that the displaced tooth was not fractured, the tooth was repositioned with finger pressure only to the proper position and verified by having the patient close his teeth (Figure 2).
Figure 2.
Mechanism of injury for a displaced tooth.
The fractured tooth showed exposed pulp. The exposed pulp was covered with a calcium hydroxide resin from a dental emergency kit. After radiographs the next day, the player was stabilized for the return trip home.
Key Points
The displaced tooth should be evaluated and moved to its normal position, especially if it is interfering with bite.3,33
If the pulp is exposed, the tooth may have blood at the fracture site and will be sensitive to temperature and pressure. Capping the pulp with a readily available calcium hydroxide is recommended until definitive dental care is achieved.3,11,33
In the case of a displaced tooth with successful treatment, the player may return to play with mouth guard protection within 24 to 48 hours (there are no firmly established return-to-play guidelines).
Case 3
An 18-year-old high school football player was involved in an open-field tackle, hitting his jaw, and was unable to put his teeth together afterward. On the sideline, bimanual examination of his mandible revealed definite dislocation of the right temporomandibular joint (TMJ) and severe pain on palpation. Prompt emergent referral to a dentist resulted in a successful reduction of his TMJ under sedation.
Key Points
TMJ dislocation involves displacement of the mandibular condyle from the articular joint in the temporal bone. It can be unilateral or bilateral.
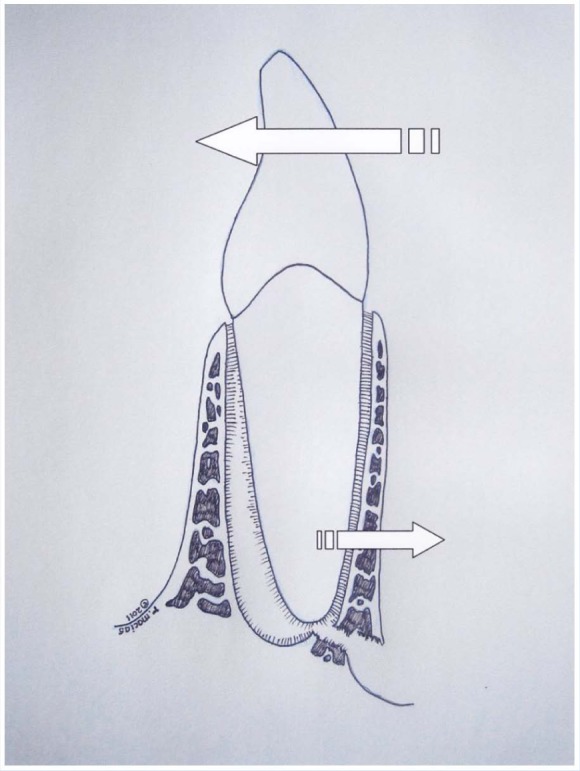
TMJ dislocation can be difficult to differentiate from a displaced mandibular jaw fracture. Both present with malocclusion (Figure 3).25
To differentiate a fracture from a TMJ dislocation, place index fingers on the interior border of the mandible and press outward. If there is a fracture, pain and movement of the fractured segment should be evident.35 If only pain in and around the TMJ is present, then the TMJ may be dislocated (Figure 4).
Moving the jaw laterally back and forth may reduce the dislocation. Urgent referral to a dentist or oral surgeon should be made if reduction does not occur. Swelling or muscle trismus may occur with delay.25,27
With a TMJ dislocation, the player may return with protection (mouth guard and/or face mask) between 2 and 4 weeks, depending on the severity. The risk of another dislocation may be increased with a previous dislocation.
Figure 3.

Malocclusion seen in a temporomandibular joint (TMJ) dislocation.
Figure 4.
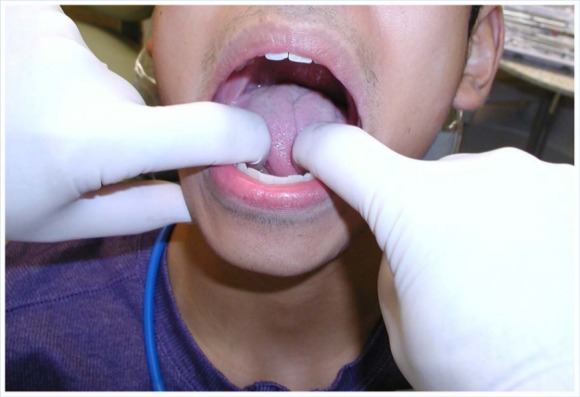
Mandibular examination is performed with palpation in and outside the mouth.
Mouth Guards and Injury Prevention
Most studies show a reduction in dental injuries when mouth guards are worn.1,9,13,16,22-24,26,40 In a meta-analysis, the overall risk of an orofacial injury was 1.6 to 1.9 times higher when a mouth guard was not worn.23 Mouth guard use in high school and college football players significantly reduced dental injury rates.17 Not only do mouth guards help prevent orofacial trauma, they reduce the cost of these injuries significantly.9,24
The mouth guard has several purposes:
restructure and absorb shock to reduce or prevent fractures in teeth and jaws,
provide soft tissue protection to decrease oral and lip lacerations,
give support by filling in missing teeth spaces.
Additionally, some biomechanical studies suggest a reduction of forces and a repositioning of the jaw that could potentially reduce the incidence and severity of concussion; however, current evidence does not support this theory.7,10,22,23
In the early twentieth century, boxing became the first organized sport to realize a need for mouth protection. Fighters used various materials stuffed around their teeth in attempts to better withstand punishment before an approved mouth guard was designed.26,36 Football players began using mouth guards a few decades later, and in 1962, the National Collegiate Athletic Association (NCAA) made them mandatory.4,26 Today, several sports sanctioned by the NCAA require mouth guards, including women’s and men’s lacrosse, field hockey, and ice hockey.22 The American Dental Association and the International Academy of Sports Dentistry recommend using mouth protection for 30 activities.26
Although some studies cite low incidence of dental injuries,6,20 baseball and basketball have frequent orofacial trauma, but few participants wear mouth guards.9 In basketball, dental trauma often occurs from contact with other players, whereas orofacial injury in baseball is usually the result of contact with the ball.21 Mouth protection may reduce the high numbers of injuries to the maxillary central incisor and lip.30 Some athletes claim mouth guards are uncomfortable and affect breathing and communication.1,9,16,21,41 There is no conclusive evidence that breathing or adequate oxygen levels are compromised, even during strenuous physical activity.16,21
Three types of mouth guards have proven beneficial in preventing several common injuries1,22,43:
The stock mouth guard is generic or readymade. It comes in different sizes but is not form-fitted and will not contour to an individual’s mouth. Biting down keeps it in place. It is the least expensive and can be worn immediately.
The “boil-and-bite” mouth guard is the mouth-formed guard. It is economical and is more popular among athletes.1,29 Boiling softens the device temporarily; biting down molds an imprint. Decreasing the thickness can decrease protection (Figure 5).30
The custom-fitted mouth guard is formed by a pressure or vacuum method. They are the most expensive but offer the most comfortable, exact fit.1
Figure 5.

Custom-fitted mouth guard.
Medical or dental professionals can determine the ideal mouth guard fit for a patient by obtaining a complete dental history, knowing the sport and position, and conducting a thorough oral examination, including structures.23,29
Conclusion
While contact sports pose a relatively high risk for dental and orofacial trauma, proper treatment can improve outcomes. Prompt referral for complicated crown fractures and temporomandibular joint dislocations is paramount. A tooth-saving kit is useful on the sideline. If not available, an avulsed tooth can be transported in milk or saliva. Mouth guards can reduce or eliminate dental injury in most cases.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. ADA Council on Access, Prevention and Interprofessional Relations; ADA Council on Scientific Affairs. Using mouth guards to reduce the incidence and severity of sports-related oral injuries. JADA. 2006;137:1712-1720. [DOI] [PubMed] [Google Scholar]
- 2. Akinbimi BO. Evaluation of the mechanism and principles of management of temporomandibular joint dislocation. Systematic review of literature and a proposed new classification of temporomandibular joint dislocation. Head Face Med. 2011;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Academy of Pediatric Dentistry. Guideline on Management of Acute Dental Trauma. http://www.aapd.org/media/policies_guidelines/g_trauma.pdf. Accessed February 12, 2012.
- 4. American Dental Association Bureau of Dental Health Education and Bureau of Economic Research and Statistics. Mouth protectors: 1962 and the future. JADA. 1963;66:539-543. [Google Scholar]
- 5. Andersson L, Andreasen JO, Day P, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2012;28:88-96. [DOI] [PubMed] [Google Scholar]
- 6. Beachy G. Dental injuries in intermediate and high school athletes: a 15-year study at Punahou School. J Athl Train. 2004;39:310-315. [PMC free article] [PubMed] [Google Scholar]
- 7. Benson BW, Hamilton GM, Meeuwisse WH, McCrory P, Dvorak J. Is protective equipment useful in preventing concussion? A systematic review of the literature. Br J Sports Med. 2009;43(suppl 1):i56-57. [DOI] [PubMed] [Google Scholar]
- 8. Coalter F. London 2012: a sustainable sporting legacy? http://www.nolondon2012.org/SportingLegacyPaper.pdf. Accessed November 1, 2011.
- 9. Cohenca N, Roges RA, Roges R. The incidence and severity of dental trauma in intercollegiate athletes. J Am Dent Assoc. 2007;138:1121-1126. [DOI] [PubMed] [Google Scholar]
- 10. Daneshvar DH, Baugh CM, Nowinski CJ, McKee AC, Stern RA, Cantu RC. Helmets and mouth guards: the role of personal equipment in preventing sport-related concussions. Clin Sports Med. 2011;30:145-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Diangelis AJ, Andreasen JO, Ebeleseder KA, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:2-12. [DOI] [PubMed] [Google Scholar]
- 12. Emergency treatment of athletic dental injuries. http://academyforsportsdentistry.org/Resources/TreatmentCards/tabid/70/Default.aspx. Published 2010. Accessed November 1, 2011.
- 13. Emerich K, Kaczmarek J. First aid for dental trauma caused by sporting activities. Sports Med. 2010;40:361-366. [DOI] [PubMed] [Google Scholar]
- 14. Fairiniuk LF, Souza MH, Westphalen VP, et al. Evaluation of care of dentoalveolar trauma. J Appl Oral Sci. 2010;18:343-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gebauer DP, Williamson RA, Wallman KE, Dawson BT. The effect of mouth guard design on respiratory function in athletes. Clin J Sport Med. 2011;21:95-100. [DOI] [PubMed] [Google Scholar]
- 16. Heintz WD. Mouth protectors: a progress report. Bureau of Dental Health Education. J Am Dent Assoc. 1986;77:632-636. [DOI] [PubMed] [Google Scholar]
- 17. Hinckfuss SE, Messer LB. An evidenced-based assessment of the clinical guidelines for replanted avulsed teeth. Part II: prescription of systemic antibiotics. Dent Traumatol. 2009;25:158-164. [DOI] [PubMed] [Google Scholar]
- 18. Hinckfuss SE, Messer LB. Splinting duration and periodontal outcomes for replanted avulsed teeth: a systematic review. Dent Traumatol. 2009;25:150-157. [DOI] [PubMed] [Google Scholar]
- 19. Huffman EA, Yard EE, Fields SK, et al. Epidemiology of rare injuries and conditions among United States high school athletes during the 2005-2006 and 2006-2007 school years. J Athl Train. 2008;43:624-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kececi AD, Cetin C, Eroglu E, Baydar ML. Do custom-made mouth guards have negative effects on aerobic performance capacity of athletes? Dent Traumatol. 2005;21: 276-280. [DOI] [PubMed] [Google Scholar]
- 21. Klossner D. 2011-2012. NCAA sports medicine handbook. National Collegiate Athletic Association; http://www.NCAA.org/health-safety. Accessed November 1, 2011. [Google Scholar]
- 22. Knapik JJ, Marshall SW, Lee RB, et al. Mouthguards in sport activities: history, physical properties and injury prevention effectiveness. Sports Med. 2007;37:117-144. [DOI] [PubMed] [Google Scholar]
- 23. Labella CR, Smith BW, Sigurdsson A. Effect of mouth guards on dental injuries and concussions in college basketball. Med Sci Sports Exerc. 2002;34:41-44. [DOI] [PubMed] [Google Scholar]
- 24. Luyk NH, Larsen PE. The diagnosis and treatment of the dislocated mandible. Am J Emerg Med. 1989;7:329-335. [DOI] [PubMed] [Google Scholar]
- 25. Mihalik JP, McCaffrey MA, Rivera EM, et al. Effectiveness of mouth guards in reducing neurocognitive deficits following sports-related cerebral concussion. Dent Traumatol. 2007;23:14-20. [DOI] [PubMed] [Google Scholar]
- 26. Muhtarogullari M, Demiralp B, Ertan A. Non-surgical treatment of sports-related temporomandibular joint disorders in basketball players. Dent Traumatol. 2004;20:338-343. [DOI] [PubMed] [Google Scholar]
- 27. Padilla R, Dorney B, Balikov S. Prevention of oral injuries. J Calif Dent Assoc. 1996;24:30-36. [PubMed] [Google Scholar]
- 28. Park JB, Shaull KL, Overton B, Donly KJ. Improving mouth guards. J Prosthet Dent. 1994;72:378-380. [DOI] [PubMed] [Google Scholar]
- 29. Policy on prevention of sports-related orofacial injuries. Pediatr Dent. 2008-2009;30(suppl 7):58-60. [PubMed] [Google Scholar]
- 30. Ranalli DN, Demas PN. Orofacial injuries from sport. Sports Med. 2002;32:409-418. [DOI] [PubMed] [Google Scholar]
- 31. Ranalli DN. Dental injuries in sports. Curr Sport Med Rep. 2005;4:12-17. [DOI] [PubMed] [Google Scholar]
- 32. Ranalli DN. Prevention of craniofacial injuries in football. Dent Clin North Am. 1991;35:627-645. [PubMed] [Google Scholar]
- 33. Reed RV., Jr. Origin and early history of the dental mouthpiece. Br Dent J. 1994;176:478-480. [DOI] [PubMed] [Google Scholar]
- 34. Rosenberg H, Rosenberg H, Hickey M. Emergency management of a traumatic tooth avulsion. Ann Emerg Med. 2011;57:375-377. [DOI] [PubMed] [Google Scholar]
- 35. Shirani G, Kalantar Motamedi MH, Ashuri A, Eshkevari PS. Prevalence and patterns of combat sport related maxillofacial injuries. J Emerg Trauma Shock. 2010;3:314-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Smith WS, Kracher CM. Sports-related dental injuries and sports dentistry. Crest Oral-B Continuing Education Course, March 2011. http://dentalcare.com/media/en-US/education/ce127/ce127.pdf. Accessed November 1, 2011.
- 37. Spinas E, Savasta A. Prevention of traumatic dental lesions: cognitive research on the role of mouth guards during sport activities in paediatric age. Eur J Paediatr Dent. 2007;8:193-198. [PubMed] [Google Scholar]
- 38. Tulunoglu I, Ozbek M. Oral trauma, mouth guard awareness, and use in two contact sports in Turkey. Dent Traumatol. 2006;22:242-246. [DOI] [PubMed] [Google Scholar]
- 39. Welch CL, Thomson WM, Kennedy R. ACC claims for sports-related dental trauma from 1999 to 2008: a retrospective analysis. N Z Dent J. 2010;106:137-142. [PubMed] [Google Scholar]
- 40. Woodmansey KF. Athletic mouth guards prevent orofacial injuries: a review. Gen Dent. 1999;47:64-69. [PubMed] [Google Scholar]