Abstract
Context:
With the ever-increasing number of masters athletes, it is necessary to understand how to best provide medical support to this expanding population using a multidisciplinary approach.
Evidence Acquisition:
Relevant articles published between 2000 and 2013 using the search terms masters athlete and aging and exercise were identified using MEDLINE.
Study Design:
Clinical review.
Level of Evidence:
Level 3.
Results:
Preparticipation screening should assess a variety of medical comorbidities, with emphasis on cardiovascular health in high-risk patients. The masters athlete should partake in moderate aerobic exercise and also incorporate resistance and flexibility training. A basic understanding of physiology and age-related changes in muscle composition and declines in performance are prerequisites for providing appropriate care. Osteoarthritis and joint arthroplasty are not contraindications to exercise, and analgesia has an appropriate role in the setting of acute or chronic injuries. Masters athletes should follow regular training regimens to maximize their potential while minimizing their likelihood of injuries.
Conclusion:
Overall, masters athletes represent a unique population and should be cared for utilizing a multidisciplinary approach. This care should be implemented not only during competitions but also between events when training and injury are more likely to occur.
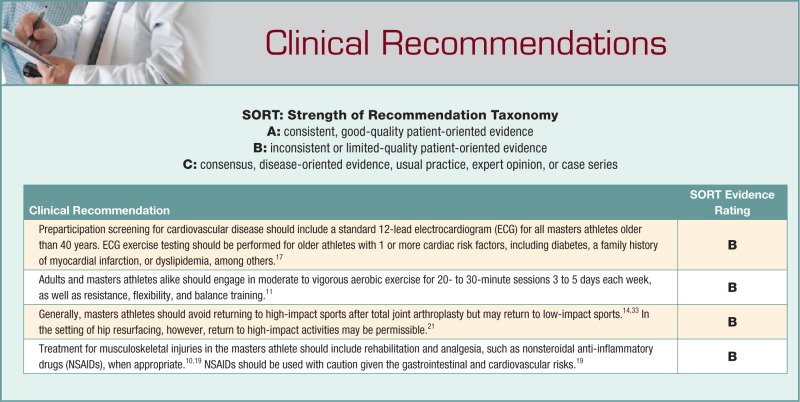
Strength of Recommendation Taxonomy (SORT):
B.
Keywords: masters athlete, exercise, recommendations
A recent increase in the number of masters athletes in the United States can be attributed to a growing population of more than 300 million people, an aging subpopulation of “baby boomers,” and a culture enamored with sports.13,21 To exemplify this increase, in 1987, the first National Senior Games had 2500 participants (all older than 50 years), which more than quadrupled to 10,100 participants in the 2011 games despite more stringent qualifying standards.21 Similarly, the number of athletes older than 50 years in the New York City marathon increased 119% from 1983 to 1999, with significant improvement in completion times as compared with younger age groups.12
The masters athlete is typically defined as older than 35 years (as this is the age at which cardiovascular issues tend to become a greater cause of morbidity) who either trains for or takes part in athletic competitions often specifically designed for older participants.28 Many of these athletes are experienced competitors who continue their athletic pursuits after their sports careers have ended, while others are individuals who return to sport after extended periods of inactivity or simply participate and train sporadically. Ideally, care should be administered using a multidisciplinary team including the primary care provider, physiatrist, therapists, trainers, coaches, and, if necessary, an orthopaedic surgeon. Preventative and management options should be tailored to individual patients.
Preparticipation
Preparticipation screening should include a general evaluation of the patient’s overall health, evaluating for vision loss, diabetes, and hypertension, among other relevant risk factors. Routine Snellen testing,16 basic metabolic profile, glycated hemoglobin (HbA1C), complete blood counts to assess for anemia, and blood pressure readings all aid in screening.31,32
Screening may identify occult cardiovascular disease. A 12-lead electrocardiogram (ECG) should be part of a routine evaluation for all masters athletes older than 40 years, as well as implementation of the American Heart Association 12-element screening with a focused history assessing for exertional symptoms and a physical examination emphasizing the cardiovascular system.16 The 12-lead ECG is often of limited value in identifying active disease in asymptomatic masters patients, regardless of activity level.16 However, it is useful in detecting evidence of a previous myocardial infarction and uncommon forms of heart disease, such as Wolff-Parkinson-White syndrome and hypertrophic cardiomyopathy. Consequently, ECG exercise testing is recommended for all men and women older than 40 or 50 years, respectively, who have at least 1 cardiac risk factor, regardless of activity level.16 These include recent cigarette smoking, diabetes mellitus, or a first-degree relative with a history of myocardial infarction before the age of 60 years. Additional risk factors include dyslipidemia, such as low-density lipoprotein levels more than 130 mg/dL, high-density lipoprotein less than 40 mg/dL, and total cholesterol more than 200 mg/dL, as well as hypertension (>140 mm Hg systolic or >90 mm Hg diastolic pressures). Large trials, such as the Multiple Risk Factor Intervention Trial (MRFIT) and the Seattle Heart Watch Study, have demonstrated that asymptomatic at-risk patients have a profoundly increased risk of future cardiac events, thereby supporting the use of ECG exercise screening in this population.16 Furthermore, while diagnostic echocardiography may be indicated in the setting of a positive ECG exercise test, ventilatory gas analysis to assess oxygen consumption is typically not recommended as it does not yield more relevant information than ECG testing.16
Decisions regarding athletes with cardiac conditions and return to play are based on the underlying cardiac condition, as well as whether a specific treatment can reduce the risk of sudden cardiac death or diminish it substantially. Conditions that warrant high-intensity activity restriction include atherosclerotic coronary artery disease (with more than 50% luminal narrowing), particularly in patients with an ejection fraction less than 50% or evidence of exercise-induced myocardial ischemia.16 Moderate to severe systemic hypertension (>160 mm Hg systolic or >100 mm Hg diastolic pressures) should preclude participation until blood pressure is controlled.16 On returning to training or sports, these athletes should undergo blood pressure monitoring every 2 months.16 Dilated cardiomyopathy also warrants activity restriction, while patients with myocarditis should be limited to low-intensity exercise until there is no evidence of active infection (eg, absence of arrhythmias on ECG) for a period of approximately 6 months.16 In addition, inpatient or outpatient cardiac rehabilitation is recommended for those masters athletes who have had a recent cardiac event.32 Resistance exercise in a cardiac rehabilitation program may be a preferable alternative to aerobic exercise alone.1 These resistance programs can significantly reduce perceived exertion of patients performing at submaximal power outputs, while also mitigating cardiovascular disease risk factors such as hypertension, dyslipidemia, and insulin sensitivity. Resistance exercises, which typically entail lower loads and higher repetitions, are not recommended in patients who are clinically unstable, have a functional capacity of less than 5 metabolic equivalents (METs), or have symptoms of myocardial ischemia induced by exercise.1
Physiology
Muscular atrophy may be the result of sarcopenia due to age-related atrophy and a decrease in the number of muscle fibers.28 These changes have been attributed to a decrease in anabolic agents such as testosterone and growth hormone, confounding the incorporation of amino acids into skeletal muscle, while an increase in catabolic factors such as interleukin-6 enhances muscle wasting.28 There is evidence, however, that physical activity, regardless of age, helps maintain muscle fiber composition.28 Muscle appears to adapt in a manner reflecting training load.28 Resistance training should be continued as athletes age, rather than significantly minimizing such training because of the assumption that older individuals are intrinsically “frail.”1,28 Training may not only improve athletic performance, but it may also enable them to safely perform activities of daily living and minimize their susceptibility to falls.1
The muscles of the masters athlete reach the same level of fatigue as the younger athlete; however, they are slower to recover.5 Strength-dependent events show the greatest rates of decline with age, whereas walking and jumping manifest the slowest declines.2 The decrease in overall performance correlates with a loss of type 2 muscle fiber units and a resultant loss of power.2 The decline in muscle performance begins in the early-to-late 30s, prior to the loss of fiber units and muscular atrophy, and has been attributed to subtle changes in fine motor control.7 Exercise training alone may be insufficient to prevent age-related declines in skeletal muscle mass, but it leads to increased exercise capacity, lower levels of body fat, and greater survival rates.4 The masters athlete is likely to experience a decrease in endurance with advancing age.2 Men’s endurance decreases to 75% of their peak performance by the seventh decade in sprinting events and by the middle of the sixth decade in longer distances.2 Women’s endurance decreases at similar rates but approximately 3 to 8 years before that of the men, depending on the athletic event.2 A key mechanism associated with the decrease in age-related endurance is a reduction in maximal aerobic capacity.25 An individual can maintain their peak endurance performance until approximately 35 years of age.2,25 After, a dramatic decline is primarily because of a progressive reduction in maximal oxygen consumption.25 Masters athletes with a vigorous and frequent training regimen have smaller declines in maximal aerobic capacity compared with those athletes who do not.25,26
Recommendations for Exercise
The American College of Sports Medicine (ACSM) position on the quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, as well as the ACSM stance on flexibility and balance in older adults, includes several recommendations (Table 1).10 Light activity, including walking, is recommended for deconditioned patients or those with significant chronic diseases as it may reduce the rate of age-associated deterioration in numerous physiologic functions. Moderate- to vigorous-intensity aerobic exercise, however, is required to elicit changes in the cardiovascular system and is recommended for most adults and masters athletes. Specifically, the ACSM recommends at least 30 minutes of moderate-intensity exercise 5 days per week, at least 20 minutes of vigorous aerobic exercise 3 days per week, or some combination of moderate and vigorous exercises at least 3 days per week. The activity (eg, running, cycling, or cross-country skiing) should involve large muscle groups, be rhythmic in nature, and be performed either in a single continuous session or several sessions each more than 10 minutes in duration per day. With increasing muscle strength, increased levels of spontaneous activity have been seen in both healthy, free-living older individuals and very old and frail men and women.10,23 Neuromotor and proprioceptive exercises involving balance and coordination should be performed for 20 to 30 minutes per day at least 2 days each week for older patients.10
Table 1.
Exercise recommendations in healthy adultsa
| Type of Training | Frequency | Quality |
|---|---|---|
| Aerobic | 3-5 days per week for 20-60 minutes per session | 55% to 95% of maximum heart rate for moderate to vigorous intensity; light intensity for deconditioned adults or those with chronic diseases |
| Resistance | 2-3 days per week | 2-4 sets of 8-20 repetitions incorporating all major muscle groups |
| Flexibility | Minimum 2-3 days per week | Incorporated into existing routine, repeat stretch 2-4 times for total of 60 seconds per stretch |
| Balance | 2-3 days per week | 20-30 minutes per neuromotor or proprioceptive exercise session |
From American College of Sports Medicine position stand on the recommended quantity/frequency and quality of exercise for developing and maintaining cardiorespiratory, muscular fitness, flexibility, and balance in healthy adults.10
In addition to basic weight training, plyometrics can be performed.29 Although not specifically for the masters athlete, plyometrics, in addition to weight training, have been shown to increase strength and power.29 Surveys given to the strength and conditioning coaches of the National Basketball Association and Major League Baseball revealed that 94% to 100% use plyometrics in their respective training regimens.6,24 The muscle fibers of older athletes may be susceptible to contraction-induced injury, and plyometric training may similarly increase strength and power to help prevent subsequent injury.29 A plyometric training regimen for the masters athlete would involve alternating between high- and low-intensity upper and lower extremity exercises every 2 days to allow for adequate recovery. Upper extremity exercises include chest passes, inclined push-ups, and vertical ball tosses, while lower extremity regimens include straight-leg jogging, stride drills, and forward lunges. The intensity and frequency of the program should start with low to moderate volumes (eg, 80 contacts per session) and be modified based on the athlete’s baseline functional level, progress, and recovery after each session. Plyometrics, however, should be limited or avoided in older patients with moderate to severe arthritis, clinically impaired proprioception, or severe osteoporosis.29
Risks of Exercise
Sports-related injuries are commonly classified as either acute traumatic or chronic overuse. Injuries common to the masters athlete include rotator cuff injuries, Achilles tendinopathies, and meniscal tears in the knee.9 Although variable in duration depending on the multiplicity and severity of the injury, 60% of masters athletes abstain from activity for at least 1 week after a sports-related injury, with one third remaining out for more than 1 month.9 Additionally, in patients older than 70 years, 20% note persistent pain or symptoms for more than 1 year after a sports-related injury.
Given similar training regimens, however, age may not have significant effects on the rates of all types of injury. For example, age is not an independent risk factor for Achilles tendinopathy or patellar tendinopathy in the masters track and field athlete.14,15 Sudden cardiac arrest during a marathon, however, is more common in masters athletes (mean age, 50 years) than the younger cohort.31 In general, one third of running masters athlete’s medical visits may relate to running-related injuries, but runners seek medical services less often (which may unduly lower reported injury rates in this population), and have less physical disability, better cardiovascular fitness, and reduced weight compared with age-matched control subjects.31 Nonetheless, in those injuries whose rates do not appear to be related to age, masters athletes typically require longer recovery times.14,31
Regardless of the prevalence of injuries in the masters athlete population, when treating injuries, it is advisable to treat the masters athlete as one would a younger athlete. Certain patient factors and conditions may render exercise inadvisable. These include acute febrile illness, acute unstable chest pain, uncontrolled diabetes, hypertension, asthma, congestive heart failure, severe aortic stenosis, new falls, and, in some cases, musculoskeletal pain.31 Osteoarthritis (OA) is not a contraindication to general exercise.8,33 Masters athletes, unlike their younger counterparts, are more likely to present with several of the aforementioned conditions. A more thorough medical evaluation and longer rehabilitation period may be necessary for this older population.
Exercise for Osteoarthritis
Although no specific consensus exists as to what impact activity has on arthritis of the lower extremity, it is believed that participation in high joint loading and high-impact sports may lead to a higher risk of OA, whereas moderate amounts of exercise do not appear to increase an athlete’s risk for OA.33 A common condition in older patients, knee OA is affected by mechanical differences in knee joint loading, as well as differences in gait due to increases in the peak knee adduction moment and the knee adduction angular impulse.27 An increased association between elite participation in weightbearing sports and radiographic OA has been shown, but the overall impact on the athlete’s disability when taking into consideration comorbidities, overall fitness, and ability to participate is undetermined.33 The increased risk of OA due to participation in sports is the result of joint injuries manifesting as single-impact insults or repetitive microtrauma, and not regular intense physical activity.33 Also, maintaining joint motion and muscle mass with regular physical activity has minimal impact on one’s risk for OA.3
A Cochrane review published in 2009 analyzing 32 randomized controlled trials with data on 3616 participants with knee pain investigated exercise specifically for knee OA.8 Simple quadriceps strengthening programs achieved a significance for decreased pain and increased physical function. According to these data, strengthening programs could be performed in individual treatments or class- or home-based programs. Fewer than 12 supervised sessions were necessary for notable benefits, including decreased pain and increased physical function, but those who received more than 12 supervised sessions demonstrated greater effect sizes for improvements in pain. The advantages of group-based exercise programs include social interaction as well as possible cost minimization.8
Joint Arthroplasty
The progression of OA and the persistence of symptomatic degenerative changes within the joint may ultimately necessitate surgical intervention. This occurs much more commonly in highly active older athletes, as older athletic men and women have relative risks of 4.5 and 2.3, respectively, of developing hip OA requiring hip arthroplasty compared with their low activity counterparts.33 When the severity of joint degeneration warrants arthroplasty, however, the surgery does not need to halt the activities of the masters athlete, although activity modification may be warranted. In general, after arthroplasty, athletes should avoid returning to high-impact sports but may return to low-impact sports.33 This recommendation, based on small retrospective studies and expert opinion, is related to the perception that return to high-impact sports may lead to implant loosening, fracture, and overall worse prosthesis survival.11 In certain situations, however, given select patient factors including comorbidities, athletic experience, and type of prosthesis, returning to high-impact sports may be acceptable, such as after hip resurfacing.13,20 Nonetheless, participation in high-impact sports typically decreases after hip resurfacing, perhaps in part because of patient anxiety regarding their implants, while participation in low-impact sports does not decrease.20
With regard to exercise after total joint arthroplasty, a balance likely exists between those who have decreased bone density from little activity and those who have increased wear and late loosening of the prosthesis after much exercise. Low-impact activities, such as cycling or swimming, are ideal for those who have had joint arthroplasty, and high-impact sports should be avoided on a regular basis.13 If continued recreationally, joint load–reducing measures such as skiing on flatter slopes and avoiding icy conditions, or participation in doubles as opposed to singles tennis, are recommended.13 Regarding return to sport after unicompartmental knee arthroplasty, some recommend waiting until there are no symptoms or pain.19 Low- to mid-impact activities are specifically recommended, and return to activity is advised after restoration of quadriceps and hamstring strength.19 Moreover, more than 75% of athletes who receive a shoulder replacement return to those sports in which they had previously participated, such as swimming, golf, and tennis, and spend more than twice as much time doing them as they had prior to surgery.17 Conversely, researchers found that less than 50% of those athletes who had participated in weight lifting, bowling, and softball prior to surgery returned to their presurgery sports.17 This has been attributed to the increased stress that these sports place on the shoulder. In general, the masters athlete’s ability to participate in sports may return after surgery; however, the frequency and intensity with which they participate may vary.
Analgesia
Nonoperative management for soft tissue injuries such as muscle strains, ligament sprains, or contusion commonly includes rest, ice, elevation, and pain control. In addition, analgesia combined with stretching, strengthening, and reconditioning should be included in the rehabilitation protocol. Nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit nonspecific cyclooxygenase and mitigate prostaglandin production, are often indicated for the soft tissue injuries that the masters athlete may endure. A short course of NSAIDs is likely to offer analgesic effects as well as relief related to soreness when the athlete is in the early stages of a new exercise regimen. NSAIDs, however, are also associated with a variety of adverse side effects that should be carefully monitored in the masters athlete population, as these individuals may be at increased risk compared with younger athletes. More specifically, they may have gastrointestinal, such as gastritis and dyspepsia, and renal insults that may have detrimental effects on muscle and ligament healing.18 Additionally, long-term NSAID use may increase the risk of cardiovascular insults, including hypertension, myocardial infarction, congestive heart failure, and stroke.18 These risks are notably increased in patients with a prior history of myocardial infarction or underlying cardiovascular disease and can be mitigated with short-term use. Furthermore, NSAIDs may interfere with the antiplatelet activity of aspirin in those masters athletes taking this medication daily for cardiovascular event prophylaxis. In the setting of concurrent NSAID and aspirin use, patients can minimize this risk by taking their daily aspirin at least 30 minutes prior to, or at least 8 hours after, any NSAID ingestion.18 When considering soft tissue injuries and subsequent analgesic recommendations, chronic and acute injuries must be differentiated (Table 2). In general, NSAID use is recommended for impingement syndromes, tenosynovitis, and inflammatory arthropathies, but NSAIDs may inhibit healing with regard to chronic tendinopathies.18,22
Table 2.
Nonsteroidal anti-inflammatory drug (NSAID) recommendationsa
| Scenario | Condition(s) | Comments |
|---|---|---|
| Conditions in which NSAID will tend to be most useful (but should be avoided if patient is at high risk of side effects) | Impingement conditions (nerve or soft tissue impingement), tenosynovitis, inflammatory arthropathy | For analgesic use, but no improvement in tendon healing |
| Conditions in which NSAID use might be considered based on clinical findings | Ligament and joint sprains, osteoarthritis, and other degenerative joint conditions, hematomas | Reduces pain and allows for faster return to recovery |
| The value of NSAID remains controversial and should be used with caution | Muscle strains/injury | Likely helpful, useful with pain reduction |
| Conditions in which NSAID use is not generally indicated because they may compromise healing | Isolated chronic tendinopathies (without impingement), fractures | Probably harmful and unlikely to be helpful, particularly with long-term use |
When managing chronic pain, such as that associated with OA, NSAIDs, given orally or topically, will likely offer relief. Not without adverse effects of their own, alternatives such as COX-2 inhibitors or medications such as acetaminophen are an effective initial analgesic. In part because of the aforementioned adverse effects of certain medications, alternative supplements such as glucosamine or chondroitin have gained popularity. Studies examining the effects of these supplements have failed to find significant adverse effects, and there remains a potentially limited role for use with moderate to severe knee pain.30
Rehabilitation is also an important component of the musculoskeletal injury recovery process in masters athletes. Although similar to younger adults, rehabilitation programs differ for older patients by necessitating longer recovery periods between exercises as well as longer warm-up and cool-down sessions.16 Inactivity after an injury should be avoided to better facilitate a return to preinjury activity levels, particularly in older athletes as they may experience more rapid deconditioning than their younger counterparts.28 Alternative conditioning therapies, such as water running or water aerobics exercises, can help prevent this deconditioning.9
Conclusion
Overall, masters athletes represent a unique population and should be cared for using a multidisciplinary approach. The masters athlete should first receive medical clearance in part to determine if there is an underlying cardiac condition that precludes athletic participation or if such a condition can be modified to optimize the individual for play. Preparticipation screening for cardiovascular disease should include a 12-lead ECG for all masters athletes older than 40 years. ECG exercise testing should be performed for older athletes with 1 or more cardiac risk factor, including diabetes, a family history of myocardial infarction, or dyslipidemia, among others.16 In general, athletes should follow regular training regimens so as to slow the natural decline in performance and minimize the likelihood of injury. Per recommendations from the ACSM, adults and masters athletes alike should engage in moderate to vigorous aerobic exercise for 20- to 30-minute sessions 3 to 5 days each week, as well as resistance, flexibility, and balance training.10 OA, or previous joint replacement, should not preclude the masters athlete from participating in athletic events. When treating soft tissue injuries such as sprains or strains, rest, ice, elevation, and emphasis on rehabilitation should be the first line of treatment. NSAIDs can be considered but must be carefully monitored for gastrointestinal and cardiovascular effects.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Adams J, Cline M, Reed M, Masters A, Ehlke K, Hartman J. Importance of resistance training for patients after a cardiac event. Proc (Bayl Univ Med Cent). 2006;19:246-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baker AB, Tang YQ, Turner MJ. Percentage decline in masters superathlete track and field performance with aging. Exp Aging Res. 2003;29:47-65. [DOI] [PubMed] [Google Scholar]
- 3. Buckwalter JA. Sports, joint injury, and posttraumatic osteoarthritis. J Orthop Sports Phys Ther. 2003;33:578-588. [DOI] [PubMed] [Google Scholar]
- 4. Ciolac EG. Exercise training as a preventive tool for age-related disorders: a brief review. Clinics (Sao Paulo). 2013;68:710-717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Easthope CS, Hausswirth C, Louis J, Lepers R, Vercruyssen F, Brisswalter J. Effects of a trail running competition on muscular performance and efficiency in well-trained young and master athletes. Eur J Appl Physiol. 2010;110:1107-1116. [DOI] [PubMed] [Google Scholar]
- 6. Ebben WP, Hintz MJ, Simenz CJ. Strength and conditioning practices of Major League Baseball strength and conditioning coaches. J Strength Cond Res. 2005;19:538-546. [DOI] [PubMed] [Google Scholar]
- 7. Faulkner JA, Davis CS, Mendias CL, Brooks SV. The aging of elite male athletes: age-related changes in performance and skeletal muscle structure and function. Clin J Sport Med. 2008;18:501-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2009;(3):CD007912. [DOI] [PubMed] [Google Scholar]
- 9. Galloway MT, Jokl P. Aging successfully: the importance of physical activity in maintaining health and function. J Am Acad Orthop Surg. 2000;8:37-44. [DOI] [PubMed] [Google Scholar]
- 10. Garber CE, Blissmer B, Deschenes MR, et al. ; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334-1359. [DOI] [PubMed] [Google Scholar]
- 11. Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90:2245-2252. [DOI] [PubMed] [Google Scholar]
- 12. Jokl P, Sethi PM, Cooper AJ. Master’s performance in the New York City Marathon 1983-1999. Br J Sports Med. 2004;38:408-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kuster MS. Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Sports Med. 2002;32:433-445. [DOI] [PubMed] [Google Scholar]
- 14. Longo UG, Rittweger J, Garau G, et al. No influence of age, gender, weight, height, and impact profile in achilles tendinopathy in masters track and field athletes. Am J Sports Med. 2009;37:1400-1405. [DOI] [PubMed] [Google Scholar]
- 15. Longo UG, Rittweger J, Garau G, et al. Patellar tendinopathy in master track and field athletes: influence of impact profile, weight, height, age and gender. Knee Surg Sports Traumatol Arthrosc. 2011;19:508-512. [DOI] [PubMed] [Google Scholar]
- 16. Maron BJ, Araujo CG, Thompson PD, et al. Recommendations for preparticipation screening and the assessment of cardiovascular disease in masters athletes: an advisory for healthcare professionals from the working groups of the World Heart Federation, the International Federation of Sports Medicine, and the American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2001;103:327-334. [DOI] [PubMed] [Google Scholar]
- 17. McCarty EC, Marx RG, Maerz D, Altchek D, Warren RF. Sports participation after shoulder replacement surgery. Am J Sports Med. 2008;36:1577-1581. [DOI] [PubMed] [Google Scholar]
- 18. Mehallo CJ, Drezner JA, Bytomski JR. Practical management: nonsteroidal antiinflammatory drug (NSAID) use in athletic injuries. Clin J Sport Med. 2006;16:170-174. [DOI] [PubMed] [Google Scholar]
- 19. Naal FD, Fischer M, Preuss A, et al. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35:1688-1695. [DOI] [PubMed] [Google Scholar]
- 20. Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705-711. [DOI] [PubMed] [Google Scholar]
- 21. National Senior Games Association. 2013 National Senior Games Association Web Site. http://www.nsga.com. Accessed August 21, 2013.
- 22. Paoloni JA, Milne C, Orchard J, Hamilton B. Non-steroidal anti-inflammatory drugs in sports medicine: guidelines for practical but sensible use. Br J Sports Med. 2009;43:863-865. [DOI] [PubMed] [Google Scholar]
- 23. Pollock ML, Mengelkoch LJ, Graves JE, et al. Twenty-year follow-up of aerobic power and body composition of older track athletes. J Appl Physiol (1985). 1997;82:1508-1516. [DOI] [PubMed] [Google Scholar]
- 24. Simenz CJ, Dugan CA, Ebben WP. Strength and conditioning practices of National Basketball Association strength and conditioning coaches. J Strength Cond Res. 2005;19:495-504. [DOI] [PubMed] [Google Scholar]
- 25. Tanaka H, Seals DR. Endurance exercise performance in Masters athletes: age-associated changes and underlying physiological mechanisms. J Physiol. 2008;586:55-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tanaka H, Seals DR. Invited review: dynamic exercise performance in masters athletes: insight into the effects of primary human aging on physiological functional capacity. J Appl Physiol (1985). 2003;95:2152-2162. [DOI] [PubMed] [Google Scholar]
- 27. Thorp LE, Sumner DR, Block JA, Moisio KC, Shott S, Wimmer MA. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis Rheum. 2006;54:3842-3849. [DOI] [PubMed] [Google Scholar]
- 28. Trappe S. Master athletes. Int J Sport Nutr Exerc Metab. 2001;11(suppl):S196-S207. [DOI] [PubMed] [Google Scholar]
- 29. Vossen JE, Kramer JE, Burke DG, Vossen DP. Comparison of dynamic push-up training and plyometric push-up training on upper-body power and strength. J Strength Cond Res. 2000;14:248-253. [Google Scholar]
- 30. Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341:c4675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Webner D, DuPrey KM, Drezner JA, Cronholm P, Roberts WO. Sudden cardiac arrest and death in United States marathons. Med Sci Sports Exerc. 2012;44:1843-1845. [DOI] [PubMed] [Google Scholar]
- 32. Whiteson JH, Bartels MN, Kim H, Alba AS. Coronary artery disease in masters-level athletes. Arch Phys Med Rehabil. 2006;87(3 suppl 1):S79-S81. [DOI] [PubMed] [Google Scholar]
- 33. Wolf BR, Amendola A. Impact of osteoarthritis on sports careers. Clin Sports Med. 2005;24:187-198. [DOI] [PubMed] [Google Scholar]