Abstract
Context:
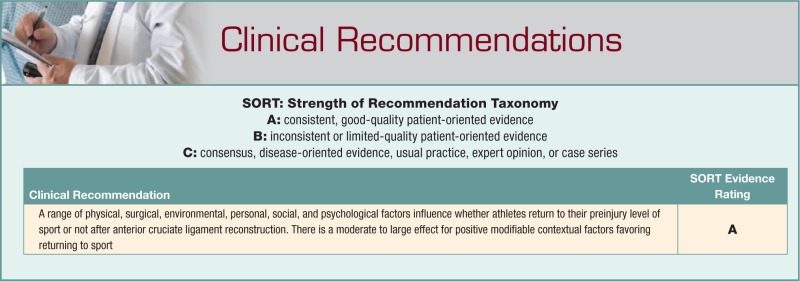
A recently updated meta-analysis of return-to-sport rates after anterior cruciate ligament (ACL) reconstruction demonstrated that 65% of athletes returned to their preinjury level of sport after surgery. The aim of this clinical review was to explore contextual factors associated with returning or not returning to the preinjury level after ACL reconstruction.
Evidence Acquisition:
Data were obtained from peer-reviewed literature via a search of the electronic databases Medline, Embase, CINAHL, and SPORTDiscus from database inception to January 2015. The keywords anterior cruciate ligament and return to sport were used. Additional literature was identified via hand-searching of the reference lists of relevant articles and the ePublication lists of key scientific journals. Random effects meta-analyses were used to pool the results of modifiable contextual factors and to examine their association with returning or not returning to the preinjury level of sport after surgery.
Study Design:
Clinical review.
Level of Evidence:
Level 2.
Results:
Lower fear of reinjury (standardized mean difference, 0.7), greater psychological readiness to return to sport (standardized mean difference, 1.0), and a more positive subjective assessment of knee function (standardized mean difference, 0.9) favored return to the preinjury level after surgery.
Conclusion:
Returning or not returning to the preinjury level after ACL reconstruction is complex and multifactorial. Screening for potentially modifiable contextual factors, particularly psychological factors, early after ACL injury may help clinicians identify athletes who could be at risk of not returning to the preinjury level of sport and institute interventions that could improve returning to sport.
Keywords: knee, ligament, sport psychology, sport reentry, anterior cruciate ligament
Anterior cruciate ligament (ACL) rupture is one of the most common sports-related injuries to the knee.39 Patients are typically young, active, and otherwise healthy individuals who are often devastated to receive their diagnosis. Before the adoption of modern surgical and rehabilitation techniques, ACL rupture was often considered a career-ending injury for athletes.22,46,62 Surgery was performed to stabilize the injured and dysfunctional knee joint to eliminate giving way episodes in patients with recurrent instability. With the shift to less invasive surgical techniques and accelerated rehabilitation protocols55 in the late 1980s, surgical and functional outcomes steadily improved, and ACL reconstruction was increasingly performed to restore stability and facilitate return to sport. At the same time, it was hoped that early intervention could reduce the individual’s risk of developing posttraumatic osteoarthritis. In contemporary orthopaedics, the desire to return to the preinjury level of sports participation is one of the main reasons athletes choose surgical treatment,20,26 and a key indication for clinicians to advise ACL reconstruction, particularly if the individual wishes to return to pivoting sports.41,50
While returning to participation in sport is often the most important outcome for patients after ACL reconstruction, research has been primarily focused on evaluating impairment-based outcomes as a measure of the success of surgery. Postoperative impairment-based outcomes such as knee laxity and muscle strength have been excellent,9 but in a previous systematic review, participation—particularly in competitive sport—was disappointingly low.6 The ability to return to participation at the preinjury level was recently considered by experts as a key milestone in successful outcome after ACL reconstruction.38
Evaluating impairment-based outcomes after ACL reconstruction is justified. Recovery of physical impairments after surgery is important because the individual requires the physical capabilities, such as sufficient muscle strength about the knee, and neuromuscular control to safely cope with the physical requirements of playing sport.1,60 However, the recovery of physical capabilities alone is not enough to ensure a return to sport.9 It is acknowledged that both physical and psychological readiness is important for successful return to sport, but these states do not always coincide.5,7,48 In support of this, in a previous meta-analysis, a range of physical and contextual factors were found to be associated with returning to the preinjury level of sport after surgery.6
The aim of the current clinical review was to explore the contextual factors associated with returning or not returning to sport after ACL reconstruction by synthesizing additional data not included in the previous meta-analysis. Studies were identified via a search of the electronic databases Medline, Embase, CINAHL, and SPORTDiscus from inception to January 31, 2015, and hand-searching of the reference lists and ePublication lists of relevant articles and scientific journals. Empirical data from studies comparing modifiable contextual factors between people who had and had not returned to their preinjury level of sport after primary ACL reconstruction (or where at least 80% of participants had primary surgery) were extracted. RevMan 5.1 (The Cochrane Collaboration) was used to calculate pooled standardized mean differences (also known as effect sizes) using a random-effects model where clinically homogenous data were available. The random effects model was chosen based on anticipated statistical heterogeneity. Cohen guidelines14 were used when interpreting the pooled standardized mean differences. Heterogeneity was assessed statistically using Higgins I2,27 which measures the amount of inconsistency in effects across studies included in a meta-analysis, and Cochran Q.
When is it Safe to Return to Sport?
Athletes are typically permitted to return to sport between 6 and 12 months after ACL reconstruction,44,46 with the clinical assumption that return to sport will be achieved by 1 year after surgery.7 Before clearance to return to sport, it is recommended that athletes have no knee effusion, symmetrical muscle strength, and adequate neuromuscular control to manage the specific physical demands of their sport,11,60 although it has yet to be determined whether these factors are predictive of returning to sport.19 Nevertheless, important considerations for clinicians when preparing an athlete to return to sport are to ensure adequate graft healing, minimize the risk for subsequent injury, and prevent the development of osteoarthritis19,60; and evidence-based rehabilitation guidelines are broadly structured around these considerations.2,33
How Many People Return to Sport After ACL Reconstruction?
When reviewing the literature regarding return-to-sport outcomes, wide variation in return-to-sport rates can be seen—from 100% in some studies12,18,40,42 to as low as 20% in others.7,52,54,56 The results of the most recent meta-analysis of return-to-sport rates (based on data from 69 articles and 7556 participants) illustrated the importance of reporting the level of participation when evaluating returning to sport.6 The analysis demonstrated that 81% of individuals returned to some form of sport after ACL reconstruction6—an acceptable result, one might contend. However, when the level of participation was taken into account, it was found that only 65% returned to their preinjury level of sport and 55% returned to competitive sport. This means that 1 in 3 individuals did not return to his or her previous level of sports participation, and 1 in 2 did not return to competitive sport after surgery.6
Physical Recovery Alone is Not Enough to Ensure a Return to Sport
A central tenant of postoperative rehabilitation is to assist athletes to regain physical capacity so that that they may participate safely and at their desired performance level. The results of impairment-based studies demonstrate that most athletes recover knee function to a level that contemporary clinical guidelines would contend is sufficient to cope with the demands of sport.9,31 This suggests that surgery and postoperative rehabilitation programs do address knee function impairments, but it is also possible that current outcome measures may lack sensitivity to detect impairments that could impact function.35,60 Many athletes with apparently good knee function do not return to their preinjury level of sport,9 and the discrepancy between recovery of impairments and returning to sport is in agreement with other studies demonstrating a lack of association between impairments and participation in patients with musculoskeletal disorders.23,49 Clearly, there are factors in addition to physical function that are important. Some of the factors that impact returning may be modifiable with appropriate intervention, while others may be nonmodifiable.
Why Don’t Athletes Return to Sport After ACL Reconstruction?
The World Health Organization’s International Classification of Functioning, Disability, and Health65 (ICF; Figure 1) has been used as a framework for evaluating outcomes after ACL reconstruction.6,9,38 The ICF considers impairments of body structure and function, activity limitations, and participation restrictions arising from a particular health state. It also views all aspects of an individual’s functioning as occurring within a context and emphasizes that the impact of contextual factors must be considered when evaluating health-related outcomes. When applied to participation in sport after ACL reconstruction, the reasons for not returning to sport could be related to physical factors (body structure and function impairments and activity limitations) and to modifiable and nonmodifiable contextual factors (including surgical, personal, environmental, social, and psychological factors). It is possible that poor or inadequate recovery and rehabilitation may impact an athlete’s physical capabilities to participate in sport, yet as previously discussed, there is a discrepancy between physical recovery and returning to sport. On the other hand, it is possible that subtle impairments in physical function, not adequately measured with existing outcome measures, may impact the high-level functional demands of sports participation. Evaluating impairment-based outcomes has been a focus of previous research,9 so the current review focused on the current evidence for modifiable contextual factors given the potential relevance of such factors to sports medicine clinicians.
Figure 1.
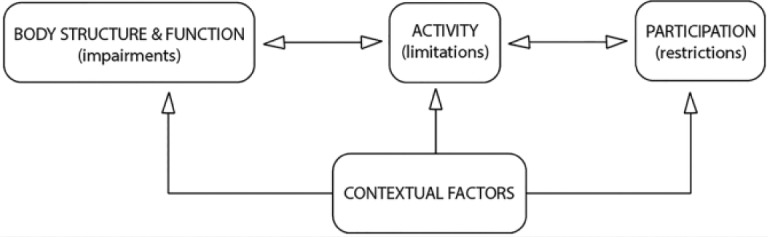
Conceptual model of the International Classification of Functioning, Disability, and Health (ICF).65
The Influence of Contextual Factors on Return To Sport
Nonmodifiable Factors
There are a number of nonmodifiable contextual factors that may influence whether an athlete returns to sport after ACL reconstruction. These factors include the graft type, age, sex, and level of sport the athlete participated in before their injury.6 There are significantly greater odds (odds ratio [OR], 1.2; 95% CI, 1.1-1.5) of returning to the preinjury level for athletes who receive patellar tendon autografts, and greater odds of returning to competitive level for athletes who receive hamstrings tendon autografts (OR, 2.4; 95% CI, 1.9-3.1).6 Being younger has a small effect, favoring returning to the preinjury level sport (effect size, 0.3).6 Those older than 25 years are 50% less likely to be playing their preinjury level sport at an average of 39 months after surgery than their younger counterparts (OR, 0.5; 95% CI, 0.3-0.8),4 and of those athletes older than 32 years, 2 of every 3 are not playing at their preinjury level.4 Men are approximately 1.5 times more likely than women to return to the preinjury level of sport (OR, 1.4; 95% CI, 1.2-1.7) and competitive sport (OR, 1.7; 95% CI, 1.2-2.3).6 Elite athletes have 2.5 times greater odds of returning to the preinjury level (OR, 2.5; 95% CI,2.0-3.1) and 6 times greater odds of returning to their competitive level (OR, 5.9; 95% CI, 4.6-7.5) than nonelite athletes.6
Modifiable Factors
There is growing evidence to suggest that psychological factors matter when it comes to returning to the preinjury level after ACL reconstruction; and this may have important implications for clinical practice. Recent systematic reviews have shown that positive psychological responses, including motivation, confidence, self-efficacy, optimism, and low fear, are associated with a greater likelihood of returning to the preinjury level after athletic injury5 and ACL reconstruction.15,17,57 In their meta-analysis, Ardern et al6 found large effect sizes (d = 0.9-1.0) based on the results of 4 studies, indicating that lower fear of reinjury32,37 and greater psychological readiness to return to sport34,63 favored returning to the preinjury level after surgery. There are additional empirical data that have been published since the previous meta-analysis, and the current review presents a new synthesis of the most recent findings regarding psychological factors and appraisals of knee function and returning to sport after ACL reconstruction.
The literature search identified 10 studies that examined the effect of modifiable contextual factors on returning to the preinjury level after ACL reconstruction.7,8,10,13,32,34,36,37,45,63 Data were combinable for 3 factors: fear of reinjury, psychological readiness to return to sport, and subjective assessment of knee function.
When data from 6 studies (n = 504) were combined, a moderately large effect (pooled standardized mean difference, 0.7; 95% CI, 0.4-1.0) was found for lower fear of reinjury, favoring returning to the preinjury level of sport (Figure 2).
Figure 2.
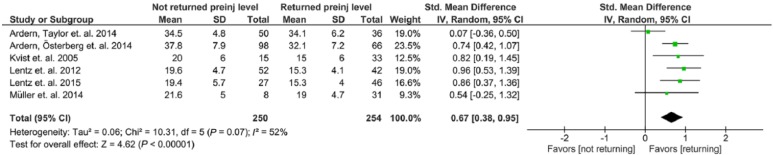
Forest plot showing comparison of fear of reinjury between people who had and had not returned to their preinjury level of sport after anterior cruciate ligament reconstruction.
When data from 6 studies (n = 697) were combined, a large effect (pooled standardized mean difference, 0.9; 95% CI, 0.6-1.1) for greater psychological readiness to return to sport favoring returning to the preinjury level of sport was found (Figure 3).
Figure 3.
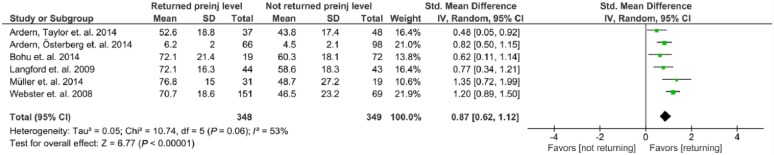
Forest plot showing comparison of psychological readiness to return to sport between people who had and had not returned to their preinjury level of sport after anterior cruciate ligament reconstruction.
When data from 4 studies (n = 384) were combined, a large effect (pooled standardized mean difference, 1.0; 95% CI, 0.5-1.6) for positive subjective rating of knee function (measured with the International Knee Documentation Committee [IKDC] subjective evaluation form28) favoring returning to the preinjury level was found (Figure 4).
Figure 4.
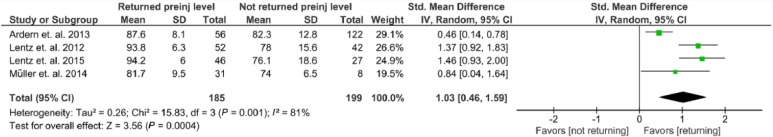
Forest plot showing comparison of subjective rating of knee function between people who had and had not returned to their preinjury level of sport after anterior cruciate ligament reconstruction.
The results of the meta-analyses in the current review corroborate the findings of the meta-analysis by Ardern et al.6 With the addition of empirical data from 6 studies8,10,13,32,36,45 that were not included in the previous meta-analysis,6 moderately large to large effect sizes were found favoring returning to the preinjury level of sport. The most noticeable difference between the results of the current analysis compared with the previous meta-analysis6 was in the effect size for fear of reinjury. With the additional data, there was a 20% reduction in the effect size (from 0.9 to 0.7). This may be due to the nonsignificant results of 2 studies8,45 published since the previous meta-analysis.6 However, taken together, the results show a consistent and sizable effect, supporting the notion that fear of reinjury may be a hindrance to returning to the preinjury level after surgery.5
Fear of reinjury is one of the most frequently cited reasons by athletes for not returning to their preinjury level of sport after ACL reconstruction, and the results of the current review provide empirical evidence of its impact. It is difficult to know the basis of the fear of reinjury. Perhaps it is not wanting to go through surgery and rehabilitation again? Perhaps it is because a new injury could have implications for participation in employment or school, or impact on family commitments? Fear is also a prominent emotion for many athletes around the time of their transition from rehabilitation to returning to sport.26,30,61 Athletes who return to sport report using fear as a motivating factor for their return61 and that testing their knee in sport helps to allay their fears, provided the return goes well.30 On the other hand, when athletes perceive pressure to return to sport and a lack of control over their return, negative psychological responses may prevail.5 These responses may in turn thwart self-motivation for returning to sport.5 As many as 1 in 2 athletes who do not return to their preinjury level of sport report that the main reason is fear of sustaining a new injury.10,21 Athletes who do not return may be fearful of pain or the consequences of sustaining a new injury,61 and some report being unwilling to risk being injured again, even though they know their knee has sufficient physical capacity to cope with the demands of sport.61
The evidence presented in the current review demonstrates the importance of athletes being psychologically ready to return to sport to making a successful transition back to the preinjury level. The scale used to evaluate psychological readiness to return to sport (the ACL–Return to Sport after Injury scale63) assesses emotions, confidence, and risk appraisals associated with returning to sport after ACL reconstruction. Psychological readiness to return to sport and knee self-efficacy (measured using the Knee Self-Efficacy scale59) are factors that have been found to predict returning to sport and physical activity after surgery.7,8,34,45,58 Both of these psychological factors involve the injured athlete making a prospective appraisal of their capacity to return to sport before attempting to return and suggest that athletes who feel less confident about their knee function and their ability to participate may be less likely to return to sport after surgery.43,53 Attitudes and motivation likely play an important role in determining self-efficacy and psychological readiness to return to sport,3,53 and supporting this notion is the fact that people who place greater importance on exercising are more likely to return to their preinjury level of sport.24
The finding of a large effect for subjective assessment of knee function favoring return to the preinjury level of sport supports the fact that an individual athlete’s appraisals about their ability to participate in sport may be an important determinant of returning. It may be a particularly important consideration for clinicians who must recognize that athletes’ appraisals of knee function do not necessarily match the results of clinical assessments.51 Psychological factors and appraisals of knee function may also be inextricably linked. For example, the experience of pain may influence returning to sport via an influence on an individual’s prospective judgment of their readiness to return to sport.17 Pain perceptions, including catastrophization of pain, can hinder wound healing, physical and psychological recovery, and ultimately return to sport after athletic injury.64 Therefore, an athlete who perceives that pain is an alert that their knee lacks sufficient physical capacity to cope with the demands of returning to sport, or that pain indicates that there is something going wrong with their knee, may have reduced self-motivation to return to sport.
Another consideration is the influence of motivation on the transition back to sport after an injury,5,48 given the theorized impact of motivation on behavior.3,53 It is reasonable to hypothesize that athletes with higher motivation to return to sport could be more likely to return after ACL reconstruction.24 While there are few empirical studies investigating motivation to return to sport after surgery, the findings of 2 studies (which were not able to be synthesized using meta-analysis because of heterogeneity) support the hypothesis of a relationship between self-motivation and returning to sport after ACL reconstruction. In one study, motivation to return to sport measured preoperatively predicted returning to the preinjury level of sport at 2 years after surgery (effect size, 1.9).25 In another study of athletes who had not returned to their preinjury level of sport at 1 year after surgery, those who subsequently returned to their preinjury level rated their self-motivation to return to sport at 1 year significantly higher than those who were not playing sport at 2 years (effect sizes ranged from 0.2 to 0.9).8
Systematically addressing potentially modifiable contextual factors in postoperative rehabilitation programs may be warranted to improve return to sport rates after surgery, yet these factors are not addressed in current evidence-based clinical guidelines.2 Interventions including motivational interviewing, imagery, and goal setting have shown promise in improving self-efficacy and reducing reinjury anxiety in athletes with sports injury.16,29 There is also evidence of effectiveness in improving clinical and function outcomes in people with ACL reconstruction.47,66 Given the overall good physical function outcomes achieved after surgery9 and the fact that positive psychological responses have been shown to predict returning to the preinjury level of sport,5,7 it may be hypothesized that adding psychological interventions to current physical rehabilitation interventions could be a way to help athletes make the transition back to sport. Although, randomized studies of new multifactorial rehabilitation paradigms are required to test this hypothesis. The results of the current review may also suggest that clinical screening for psychological responses that could hinder returning to sport might help clinicians to identify athletes who could be at risk of not returning to sport and target interventions at athletes who may need additional support to return to sport. Scores on the ACL–Return to Sport after Injury scale have been shown to predict athletes who return to their preinjury level of sport after surgery,7,34,45 suggesting this scale may have clinical merit in identifying at-risk athletes.
Conclusion
Returning to sport after ACL reconstruction is complex and multifactorial. One in 3 athletes does not return to his or her preinjury level of sport, and 1 in 2 does not return to competitive-level sport after surgery. There are modifiable and nonmodifiable factors that may influence returning to sport after surgery. The contextual factors of female sex, older age, and participating at a nonelite level prior to ACL injury are nonmodifiable factors that may increase the risk of not returning to the preinjury level of sport after surgery. Moderately large to large effects (standardized mean difference, 0.7-1.0) were found for lower fear of reinjury, greater psychological readiness to return to sport, and more positive subjective assessment of knee function favoring return to the preinjury level of sport after surgery. These potentially modifiable factors may be responsive to appropriate interventions during postoperative rehabilitation, and future research should investigate the efficacy of multifactorial rehabilitation paradigms for improving returning to sport. Early screening for maladaptive responses that could impact returning to the preinjury level of sport after surgery may also help athletes and clinicians maximize the chances of returning to sport.
Acknowledgments
Thanks to Nicholas Taylor, Kate Webster, and Julian Feller from La Trobe University and Joanna Kvist from Linköping University for the comments and discussion that helped shape this article.
Footnotes
The author reports no potential conflicts of interest in the development and publication of this article.
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2:2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179-211. [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years following anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40:41-48. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Taylor NF, Feller JA, Webster KE. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47:1120-1126. [DOI] [PubMed] [Google Scholar]
- 6. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [DOI] [PubMed] [Google Scholar]
- 7. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41:1549-1558. [DOI] [PubMed] [Google Scholar]
- 8. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year. A prospective follow-up of physical function and psychological factors in 122 athletes [published online January 12, 2015]. Am J Sports Med. 10.1177/0363546514563282. [DOI] [PubMed] [Google Scholar]
- 9. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [DOI] [PubMed] [Google Scholar]
- 10. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613-1619. [DOI] [PubMed] [Google Scholar]
- 11. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697-1705. [DOI] [PubMed] [Google Scholar]
- 12. Blonna D, Castoldi F, Delicio D, et al. Validity and reliability of the SPORTS score. Knee Surg Sports Traumatol Arthrosc. 2012;20:356-360. [DOI] [PubMed] [Google Scholar]
- 13. Bohu Y, Klouche S, Lefevre N, Webster K, Herman S. Translation, cross-cultural adaptation and validation of the French version of the Anterior Cruciate Ligament-Return to Sport after Injury (ACL-RSI) scale [published online March 28, 2014]. Knee Surg Sports Traumatol Arthrosc. 10.1007/00167-014-2942-4. [DOI] [PubMed] [Google Scholar]
- 14. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 15. Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2013;48:356-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Evans L, Hardy L. Injury rehabilitation: a goal-setting intervention study. Res Q Exerc Sport. 2002;73:310-319. [DOI] [PubMed] [Google Scholar]
- 17. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:752-762. [DOI] [PubMed] [Google Scholar]
- 18. Fabbriciani C, Milano G, Mulas PD, Ziranu F, Severini G. Anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendon graft in rugby players. Knee Surg Sports Traumatol Arthrosc. 2005;13:2-7. [DOI] [PubMed] [Google Scholar]
- 19. Feller JA, Webster KE. Return to sport following anterior cruciate ligament reconstruction. Int Orthop. 2013;37:285-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Feucht MJ, Cotic M, Saier T, et al. Patient expectations of primary and revision anterior cruciate ligament reconstruction [published online October 2, 2014]. Knee Surg Sports Traumatol Arthrosc. 10.1007/s00167-014-3364-z. [DOI] [PubMed] [Google Scholar]
- 21. Flanigan DC, Everhart JS, Pedroza A, Smith T, Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1322-1329. [DOI] [PubMed] [Google Scholar]
- 22. Fowler P, Snyder-Mackler L. Commentary. J Orthop Sports Phys Ther. 2001;31:661. [Google Scholar]
- 23. Fransen J, Uebelhart D, Stucki G, Langenegger T, Seitz M, Michel BA. The ICIDH-2 as a framework for the assessment of functioning and disability in rheumatoid arthritis. Ann Rheum Dis. 2002;61:225-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gignac MAM, Cao X, Ramanathan S, et al. Perceived personal importance of exercise and fears of re-injury: a longitudinal study of psychological factors related to activity after anterior cruciate ligament reconstruction. BMC Sports Sci Med Rehabil. 2015;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14:1021-1028. [DOI] [PubMed] [Google Scholar]
- 26. Heijne A, Axelsson K, Werner S, Biguet G. Rehabilitation and recovery after anterior cruciate ligament reconstruction: patients’ experiences. Scand J Med Sci Sports. 2008;18:325-335. [DOI] [PubMed] [Google Scholar]
- 27. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29:600-613. [DOI] [PubMed] [Google Scholar]
- 29. Johnson U. Short-term psychological intervention: a study of long-term injured competitive athletes. J Sport Rehabil. 2000;9:207-218. [Google Scholar]
- 30. Johnston L, Carroll D. The context of emotional responses to athletic injury: a qualitative analysis. J Sport Rehabil. 1998;7:206-220. [Google Scholar]
- 31. Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34:269-280. [DOI] [PubMed] [Google Scholar]
- 32. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:393-397. [DOI] [PubMed] [Google Scholar]
- 33. Kyritsis P, Witvrouw E. Return to sport after anterior cruciate ligament reconstruction: a literature review. J Nov Physiother. 2014;4:193. [Google Scholar]
- 34. Langford J, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43:377-388. [DOI] [PubMed] [Google Scholar]
- 35. Larsen JB, Farup J, Lind M, Dalgas U. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Hum Mov Sci. 2015;39:73-87. [DOI] [PubMed] [Google Scholar]
- 36. Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, function, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43:345-353. [DOI] [PubMed] [Google Scholar]
- 37. Lentz TA, Zeppieri G, Jr, Tillman SM, et al. Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther. 2012;42:893-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49:335-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13:184-188. [DOI] [PubMed] [Google Scholar]
- 40. Makihara Y, Nishino A, Fukubayashi T, Kanamori A. Decrease of knee flexion torque in patients with ACL reconstruction: combined analysis of the architecture and function of the knee flexor muscles. Knee Surg Sports Traumatol Arthrosc. 2006;14:310-317. [DOI] [PubMed] [Google Scholar]
- 41. Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762-770. [DOI] [PubMed] [Google Scholar]
- 42. McDevitt ER, Taylor DC, Miller MD, et al. Functional bracing after anterior cruciate ligament reconstruction: a prospective, randomized, multi-centre study. Am J Sports Med. 2004;32:1887-1892. [DOI] [PubMed] [Google Scholar]
- 43. McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol Rev. 2011;5:97-144. [Google Scholar]
- 44. Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22:1467-1482. [DOI] [PubMed] [Google Scholar]
- 45. Müller U, Krüger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery [published online September 2, 2014]. Knee Surg Sports Traumatol Arthrosc. 10.1007/s00167-014-3261-5. [DOI] [PubMed] [Google Scholar]
- 46. Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39:127-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nyland J, Brand E. Psychological factors in the ACL reconstruction population: are they predictive of patient outcomes? In: Sanchis-Alfonso V, Monllau JC, eds. The ACL-Deficient Knee. London, England: Springer-Verlag; 2013:189-200. [Google Scholar]
- 48. Podlog L, Eklund R. The psychosocial aspects of a return to sport following serious injury: a review of the literature from a self-determination perspective. Psychol Sport Exerc. 2007;8:535-566. [Google Scholar]
- 49. Pollard B, Johnston M, Dieppe P. Exploring the relationships between International Classification of Functioning, Disability and Health (ICF) constructs of impairment, activity limitation and participation restrictions in people with osteoarthritis prior to joint replacement. BMC Musculoskelet Disord. 2011;12:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Renström P. Eight clinical conundrums relating to anterior cruciate ligament (ACL) injury in sport: recent evidence and a personal reflection. Br J Sports Med. 2013;47:367-372. [DOI] [PubMed] [Google Scholar]
- 51. Roos EM. Outcome after anterior cruciate ligament reconstruction—a comparison of patients’ and surgeons’ assessments. Scand J Med Sci Sports. 2001;11:287-291. [DOI] [PubMed] [Google Scholar]
- 52. Roos H, Ornell M, Gärdsell P, Lohmander LS, Lindstrand A. Soccer after anterior cruciate ligament injury—an incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop Scand. 1995;66:107-112. [DOI] [PubMed] [Google Scholar]
- 53. Ryan R, Deci E. Self-determination theory and the facilitation of intrinsic motivation, social development and well-being. Am Psychol. 2000;55:68-78. [DOI] [PubMed] [Google Scholar]
- 54. Sandberg R, Balkfors B. Reconstruction of the anterior cruciate ligament. A 5-year follow-up of 89 patients. Acta Orthop Scand. 1988;59:288-293. [DOI] [PubMed] [Google Scholar]
- 55. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292-299. [DOI] [PubMed] [Google Scholar]
- 56. Shelbourne KD, Urch SE. Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med. 2000;28:651-658. [DOI] [PubMed] [Google Scholar]
- 57. te Wierike SCM, van der Sluis A, van den Akker-Scheek I, Elferink-Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23:527-540. [DOI] [PubMed] [Google Scholar]
- 58. Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:118-127. [DOI] [PubMed] [Google Scholar]
- 59. Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports. 2006;16:181-187. [DOI] [PubMed] [Google Scholar]
- 60. Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1798-1805. [DOI] [PubMed] [Google Scholar]
- 61. Tjong VK, Murnaghan ML, Nyhof-Young JM, Ogilvie-Harris DJ. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: to play or not to play. Am J Sports Med. 2014;42:336-342. [DOI] [PubMed] [Google Scholar]
- 62. Urch S, Shelbourne K, Freeman H. Rehab speeds return after ACL surgery. http://lowerextremityreview.com/article/rehab-speeds-return-after-acl-surgery. Accessed August 9, 2009.
- 63. Webster K, Feller J, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9-15. [DOI] [PubMed] [Google Scholar]
- 64. Wiese-Bjornstal D. Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports. 2010;20:103-111. [DOI] [PubMed] [Google Scholar]
- 65. World Health Organization. Towards a Common Language for Functioning, Disability and Health: The International Classification of Functioning, Disability and Health. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 66. Zaffagnini S, Russo RL, Marcheggiani Muccioli GM, Marcacci M. The Videoinsight method: improving rehabilitation following anterior cruciate ligament reconstruction—a preliminary study. Knee Surg Sports Traumatol Arthrosc. 2013;21:851-858. [DOI] [PubMed] [Google Scholar]


