Abstract
BACKGROUND
Global deaths from cardiovascular disease are increasing as a result of population growth, the aging of populations, and epidemiologic changes in disease. Disentangling the effects of these three drivers on trends in mortality is important for planning the future of the health care system and benchmarking progress toward the reduction of cardiovascular disease.
METHODS
We used mortality data from the Global Burden of Disease Study 2013, which includes data on 188 countries grouped into 21 world regions. We developed three counterfactual scenarios to represent the principal drivers of change in cardiovascular deaths (population growth alone, population growth and aging, and epidemiologic changes in disease) from 1990 to 2013. Secular trends and correlations with changes in national income were examined.
RESULTS
Global deaths from cardiovascular disease increased by 41% between 1990 and 2013 despite a 39% decrease in age-specific death rates; this increase was driven by a 55% increase in mortality due to the aging of populations and a 25% increase due to population growth. The relative contributions of these drivers varied by region; only in Central Europe and Western Europe did the annual number of deaths from cardiovascular disease actually decline. Change in gross domestic product per capita was correlated with change in age-specific death rates only among upper-middle income countries, and this correlation was weak; there was no significant correlation elsewhere.
CONCLUSIONS
The aging and growth of the population resulted in an increase in global cardiovascular deaths between 1990 and 2013, despite a decrease in age-specific death rates in most regions. Only Central and Western Europe had gains in cardiovascular health that were sufficient to offset these demographic forces. (Funded by the Bill and Melinda Gates Foundation and others.)
Globally, deaths from cardiovascular and circulatory diseases are increasing.1 This increase represents the combined effect of population growth, the aging of populations, and epidemiologic changes in cardiovascular disease. It is important to disentangle these drivers of the observed trends in global mortality for a number of reasons. First, regional and national investments in cardiovascular health can target only the epidemiologic causes of cardiovascular disease. Second, understanding the roles and relative magnitude of these demographic and epidemiologic trends is important in planning for the health care system and in developing policy. Third, the effects of the aging and growth of the population should be excluded when progress toward the goal set by the United Nations for a 25% reduction in premature mortality due to cardiovascular disease by the year 2025 is benchmarked.2,3
The Global Burden of Disease Study 2013 (GBD 2013) used standardized methods to estimate age-specific cardiovascular mortality in 188 countries from 1990 through 2013, allowing comparisons over time and across regions. To better understand the observed trends in mortality in the context of large demographic shifts, we examined separately the contribution of three causes of change in the number of cardiovascular deaths: change in population size, aging of the population, and changes in age-specific cardiovascular death rates. Because epidemiologic changes in cardiovascular disease in developing nations have been attributed to the economic growth of those nations, we also examined the relationship between changes in cardiovascular mortality due to age-specific death rates and changes in gross domestic product (GDP) per capita for each country.4
METHODS
ESTIMATION OF MORTALITY
The methods used in GBD 2013 have been reported elsewhere,5 and relevant aspects are summarized in the Supplementary Appendix, available with the full text of this article at NEJM.org. In brief, the study included 188 countries, which were grouped into 21 globally exhaustive regions for analysis (Fig. 1, and Table S1 in the Supplementary Appendix). We defined 240 causes of death, including 10 distinct cardiovascular causes of death and a combined category for less common cardiovascular and circulatory causes of death (Table 1). All available data on global mortality were collected, including death records from vital registration, sample registration, and verbal autopsy, burial and mortuary data, data on in-hospital deaths, police reports, national census data, and relevant surveys. (Vital registration systems seek to collect all death records, whereas sample registration systems collect death records from a representative subsample of a population.) Nonspecific conditions reported as an underlying cause of death were redistributed with the use of statistical methods or with causes assigned by consensus among experts.7 Different versions of codes from the international systems for the classification of disease were mapped to a uniform system. We used ensemble models to estimate cause-specific mortality according to age and sex across all countries in the study; estimates were based on the data collected on mortality and a large set of country-level covariates.8 Out-of-sample validity testing was performed for each cause-specific model, and we determined uncertainty intervals by taking 1000 draws from the posterior distribution of ensemble models, with point estimates taken as the median value. An algorithm was used to adjust these estimates for consistency with global estimates of all-cause mortality.
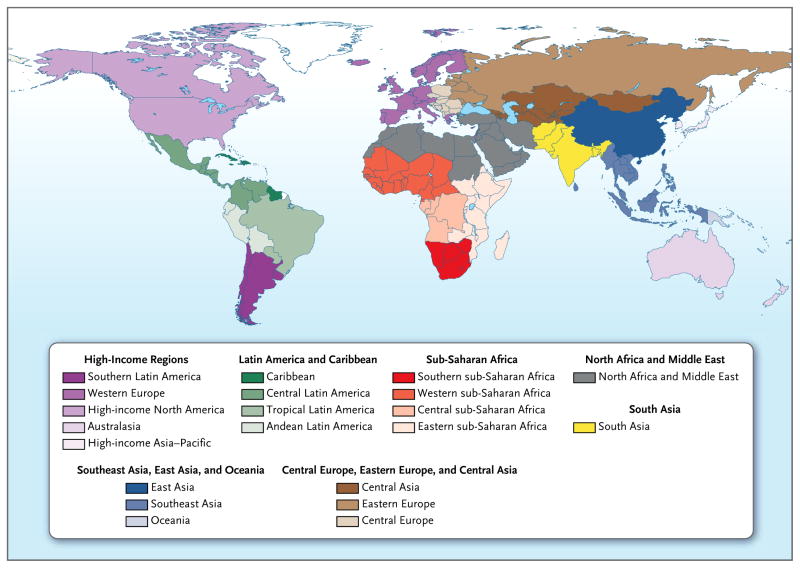
Figure 1. Regions Analyzed in the Global Burden of Disease Study 2013.
No estimates are provided for the areas in white.
Table 1.
Observed and Counterfactual Changes in Global Deaths Due to Cardiovascular Diseases, 1990–2013.*
| Disease | Deaths in 1990 | Deaths in 2013 | Percentage Change, 1990–2013 | Deaths Expected (2013 Population, 1990 Population Age Structure, 1990 Death Rates) | Percentage Change from 1990 Due to Population Growth | Deaths Expected (2013 Population, 2013 Population Age Structure, 1990 Death Rates) | Percentage Change from 1990 Due to Population Aging | Percentage Change from 1990 Due to Change in Age-Specific Death Rates |
|---|---|---|---|---|---|---|---|---|
| Ischemic heart disease | 5,737,483 | 8,139,852 | 41.7 | 7,089,534 | 23.6 | 10,104,606 | 52.5 | −34.4 |
| Ischemic stroke | 2,182,865 | 3,272,924 | 50.2 | 2,652,984 | 21.6 | 4,009,559 | 62.1 | −33.5 |
| Hemorrhagic stroke | 2,401,931 | 3,173,951 | 30.7 | 3,046,620 | 26.8 | 4,475,353 | 59.5 | −55.9 |
| Hypertensive heart disease | 622,148 | 1,068,585 | 74.1 | 804,870 | 29.5 | 1,201,735 | 63.6 | −19.0 |
| Cardiomyopathy and myocarditis | 293,896 | 443,297 | 51.4 | 373,574 | 27.4 | 486,334 | 38.4 | −14.2 |
| Rheumatic heart disease | 373,493 | 275,054 | −26.5 | 493,302 | 31.8 | 653,518 | 42.8 | −101.3 |
| Aortic aneurysm | 99,644 | 151,493 | 52.1 | 133,978 | 34.5 | 172,230 | 38.3 | −20.7 |
| Atrial fibrillation and flutter | 28,916 | 112,209 | 288.1 | 39,136 | 35.4 | 52,484 | 46.2 | 206.5 |
| Endocarditis | 45,053 | 65,036 | 46.3 | 64,331 | 42.2 | 78,714 | 32.0 | −28.8 |
| Peripheral vascular disease | 15,875 | 40,492 | 155.3 | 24,406 | 53.7 | 27,386 | 18.7 | 82.5 |
| Other cardiovascular and circulatory diseases | 478,261 | 554,588 | 15.2 | 638,716 | 33.7 | 852,357 | 44.9 | −63.2 |
| Total | 12,279,565 | 17,297,480 | 40.8 | 15,361,450 | 25.1 | 22,114,276 | 55.0 | −39.3 |
Decomposition6 of the observed number of cardiovascular deaths in 1990 and 2013 was used to calculate the contribution of three explanatory components: growth in the population, aging of the population, and change in the age-, sex-, and cause-specific rate of death. The age-, sex-, and cause-specific rate of death, which in this study is referred to as epidemiologic change, includes all changes in mortality that are not explained by demographic change (the aging or growth of the population) and includes the effect of both change in the prevalence of cardiovascular risk factors and access to health care. The sum of these three components is equal to the observed change in the total number of deaths.
DETERMINATION OF DRIVERS OF CARDIOVASCULAR MORTALITY
To analyze the drivers of cardiovascular mortality, we used age-specific, sex-specific, and cause-specific mortality data from GBD 2013. We determined the total number of cardiovascular deaths by summing the numbers of deaths for each specific cardiovascular cause in each region. We decomposed the drivers of change in the number of cardiovascular deaths from 1990 to 2013 into three explanatory components for each country: growth in the total population, the change in the population structure with regard to age and sex, and the change in the age-, sex-, and cause-specific rates of death. The age-, sex-, and cause-specific rates of death, which we refer to as epidemiologic change, includes all changes in mortality that are not explained by demographic change (the aging or growth of the population) and includes the effect of both risk factors and health care. The net change in these three constituents is equal to the observed change in the total number of deaths.
We computed two different numbers for death using a set of simple counterfactual scenarios. First, we calculated a scenario for population growth in which the number of deaths was equal to the number expected in 2013 if the total population increased as actually observed from 1990 to 2013 but the age- and sex-specific population structure and death rates remained as they were in 1990. Second, we calculated a scenario for population growth and aging in which the number of deaths was equal to the number expected in 2013 using 2013 age- and sex-specific population numbers but holding constant 1990 age- and sex-specific rates of death. The difference between deaths observed in 1990 and those estimated for 2013 through the population-growth scenario is the change in the number of deaths due to population growth alone. The difference between the population-growth scenario and the scenario for population growth and aging is the change due to population aging alone. The difference between the scenario for population growth and aging and the number of deaths actually observed in 2013 is the epidemiologic change in the age-, sex-, and cause-specific death rates. We repeated our analysis 1000 times for each age-, sex-, and country-specific rate of death using the complete set of 1000 draws from the results of ensemble models and report both the mean and 95% uncertainty interval of the resulting distribution.
Each difference is presented as a change in the absolute number of cardiovascular deaths and the percentage change, with 1990 as the reference year. For example, there were 349,153 cardiovascular deaths in the high-income Asia–Pacific region in 1990. In 2013, there were 487,170 cardiovascular deaths, which is less than the 910,042 that would have been expected if 1990 death rates had remained constant, given the population size and the age structure in that region in 2013. We report this difference as a net decrease of 121% in the age- and sex-specific death rates (422,872 fewer cardiovascular deaths than expected divided by 349,153 cardiovascular deaths observed in 1990). We used Pearson’s and Spearman’s correlation coefficients to examine the relationship between the change in GDP per capita and the change in age-specific death rates within World Bank income strata. GDP was obtained from a complete time series of country-specific GDP per capita, expressed in 2005 international dollars, for the years 1990 and 2013.9
RESULTS
GLOBAL DEATHS DUE TO CARDIOVASCULAR DISEASES
In 2013, the number of people who died from cardiovascular disease was more than 17.3 million (95% uncertainty interval, 16.5 to 18.1), representing an increase from 1990 of 40.8% (95% uncertainty interval, 36.2 to 46.4), despite a decrease in deaths attributable to epidemiologic changes of 39.3% (95% uncertainty interval, 33.6 to 44.1) (Table 1). This increase was driven by the change in the number of deaths attributed to population aging (55% increase from 1990; 95% uncertainty interval, 54.5 to 55.4) and population growth (25.1% increase from 1990; 95% uncertainty interval, 24.7 to 25.5).
The combination of increases in the number of deaths due to population growth and population aging and declines in age-specific death rates represented the most common epidemiologic profile among the specific cardiovascular causes of death (Table 1). This pattern was also present in trends for ischemic heart disease, ischemic stroke, hemorrhagic and other nonischemic causes of stroke, hypertensive heart disease, cardiomyopathy, myocarditis, aortic aneurysm, and endocarditis. Ischemic heart disease was the largest contributor to the increase in the number of cardiovascular deaths (2.4 million of the overall increase of 5.0 million cardiovascular deaths), despite an estimated decline of 34.4% (95% uncertainty interval, 27.1 to 40.4) owing to global epidemiologic changes in ischemic heart disease. Even larger declines (more than 55%) were seen as a result of epidemiologic changes in the risk of hemorrhagic stroke.
The directional trends for rheumatic heart disease were similar with respect to population growth, aging, and age-specific death rates. However, the magnitude of the decline due to epidemiologic changes — a decrease of more than 100% — led to an estimated decline in the number of deaths of 26.5% (95% uncertainty interval, 17.2 to 33.6). Rheumatic heart disease was the only cardiovascular condition for which there were fewer total deaths globally in 2013 than in 1990. Atrial fibrillation or flutter and peripheral vascular disease are notable exceptions to the demographic and epidemiologic pattern for cardiovascular disease. Deaths from each of these conditions increased dramatically between 1990 and 2013, driven not only by population growth and aging but also by increases in age- and sex-specific death rates. However, the absolute numbers of deaths ascribed to these conditions remained relatively low as compared with those ascribed to ischemic heart disease and stroke.
CARDIOVASCULAR DEATHS ACCORDING TO REGION
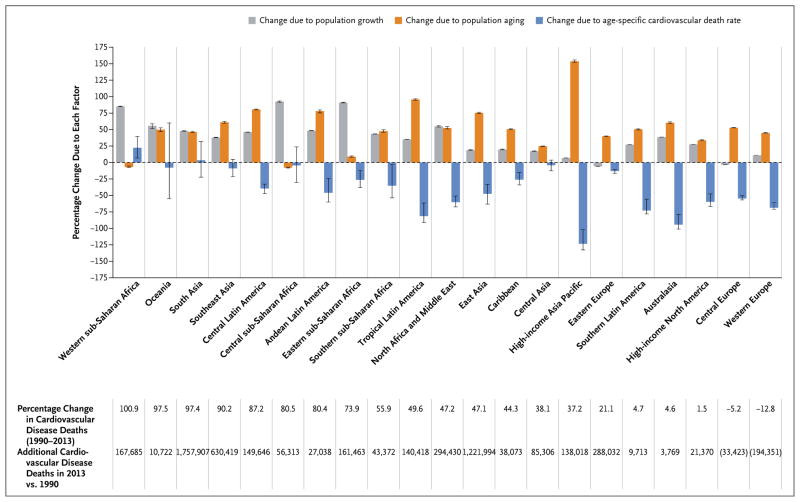
The percentage change from 1990 to 2013 in the total number of deaths from all cardiovascular causes varied significantly by region (Fig. 2). In absolute terms, South Asia had the largest estimated increase in deaths from cardiovascular disease, reporting more than 1.7 million more deaths in 2013 than in 1990. This change represents an increase of 97.4% (95% uncertainty interval, 72 to 126.1). East Asia reported more than 1.2 million additional deaths in 2013, representing a 47.2% increase from 1990. The only regions with a significant decrease in cardiovascular deaths were Central Europe and Western Europe, which had declines of an estimated 5.2% and 12.8%, respectively. Southern Latin America, Australasia, and high-income North America had no detectable change in the number of deaths from 1990 to 2013 (as indicated by an uncertainty interval crossing 0) because population aging and growth balanced out declines in age-specific death rates. According to our estimates, epidemiologic change led to an increase in cardiovascular deaths in only one region of the world (western sub-Saharan Africa).
Figure 2.
Contribution of Changes in Population Growth, Population Aging, and Rates of Age-Specific Cardiovascular Death to Changes in Cardiovascular Mortality, 1990–2013.
The combined effects of population growth, population aging, and changing age-specific death rates underlie the disparate trends in total cardiovascular deaths observed across world regions. To better understand these complex interactions, we categorized the regions into six general demographic and epidemiologic patterns (Table 2). Categories 1, 2, and 3 represent regions in which population aging and population growth served to drive relative increases in the number of cardiovascular deaths. Categories 4, 5, and 6 represent regions in which gains in cardiovascular health, represented by declines in the age-specific cardiovascular death rate, appear to have partially or completely negated the increase in cardiovascular deaths due to population growth and aging. For example, deaths in the high-income Asia–Pacific region have increased since 1990, but not as much as would have been seen if large declines in the risk of cardiovascular death had not occurred. Smaller relative gains in health, paired with a lesser degree of population aging, account for the decline in total cardiovascular deaths in Western Europe.
Table 2.
Patterns of Demographic and Epidemiologic Change in Cardiovascular Mortality.
| Category | Change in Cardiovascular Deaths, 1990–2013 | Effect of Population Growth | Effect of Population Aging | Effect of Age-Specific Cardiovascular Death Rate | Regions |
|---|---|---|---|---|---|
| Category 1 — Population growth and aging: Regions with large and continuous increases in the number of cardiovascular deaths due to population growth or aging but little change in age-specific rates of death | Increase | Large (≥20%) | Large (>30%) | Small (decline <30%) | Oceania, South Asia, Southeast Asia, Caribbean |
| Category 2 — Population growth: Regions with increases in deaths due mostly to population growth | Increase | Large (>80%) | Small (<10%) | Small (decline <30%) | Central sub-Saharan Africa, Western sub-Saharan Africa, Eastern sub-Saharan Africa |
| Category 3 — Population aging: Regions in which cardiovascular deaths rose and then fell during the preceding 20 years, resulting in a net increase in deaths due to population aging and only a small decrease in age-specific rates of cardiovascular death | Increase then decrease | Very small (<20%) | Moderate (>20%) | Very small (decline <15%) | Eastern Europe, Central Asia |
| Category 4 — Improved health moderating effect of population aging: Regions in which large increases in the number of cardiovascular deaths due to population aging were moderated by a fall in age-specific rates of death | Increase | Small (<30%) | Very large (>70%) | Large (decline >30%) | High-income Asia–Pacific, East Asia |
| Category 5 — Improved health moderating effect of population growth and aging: Regions with large relative increases in the number of cardiovascular deaths due to both population growth and aging that were moderated by a fall in age-specific rates of death | Increase | Large (>30%) | Large (>30%) | Large (decline >30%) | Central Latin America, Tropical Latin America, Andean Latin America, Southern sub-Saharan Africa, North Africa and Middle East |
| Category 6 — Improved health exceeding effect of population growth and aging: Regions in which large declines in age-specific cardiovascular death rates have led to only small increases or even a decline in the number of cardiovascular deaths despite the large effects of an aging population | Small increase or decrease | Small (<40%) | Large (>30%) | Large (decline >30%) | Southern Latin America, Australasia, high-income North America, Central Europe, Western Europe |
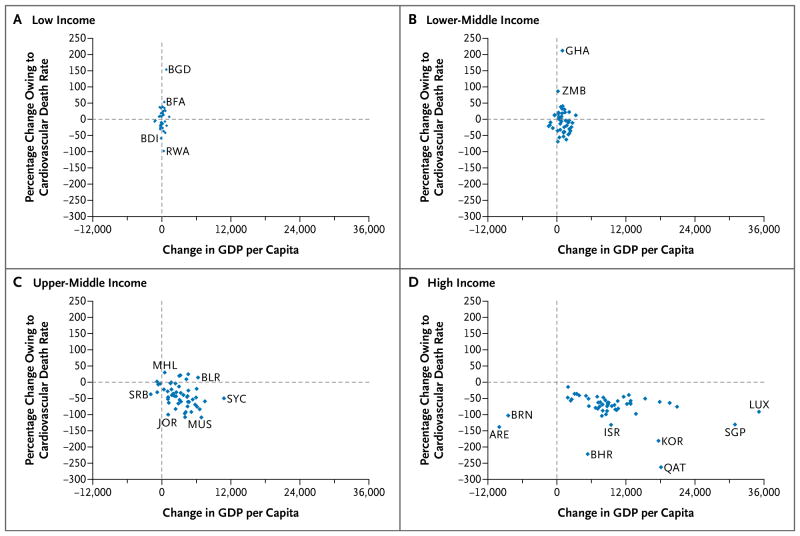
CARDIOVASCULAR DEATHS AND NATIONAL INCOME PER CAPITA
In order to investigate the relationship between national income per capita and the contribution of the age-specific death rate to cardiovascular mortality, we examined the correlation in these values between 1990 and 2013 in countries categorized by the World Bank as low income, lower-middle income, upper-middle income, and high income. Most countries had an increase in income per capita and a decline in the number of cardiovascular deaths due to epidemiologic change. However, the two variables had a significant correlation only within the category of upper-middle income. Pearson’s correlation coefficients for the four levels of income were as follows: low income, r=0.20, P=0.24; lower-middle income, r=−0.08, P=0.60; upper-middle income, r=−0.33, P=0.02; and high income, r= −0.19, P= 0.18. Spearman’s rho coefficients were as follows: low income, r=0.16, P=0.37; lower-middle income, r=−0.14, P=0.35; upper-middle income, r=−0.37, P=0.006; and high-income, r=−0.27, P=0.05 (Fig. 3).
Figure 3. Percentage Change in Cardiovascular Death Rate Owing to Changes in Age-, Sex-, and Cause-Specific Death Rates, According to Change in Country Income Level per Capita, 1990–2013.
Every country included in the study is represented by a blue diamond, which indicates the country’s percentage change in the number of cardiovascular deaths as a result of changes in the age-, sex-, and cause-specific cardiovascular death rate alone, separate from the effect of population growth and aging, and the change in gross domestic product (GDP) per capita (in international dollars) between 1990 and 2013. Outlier countries are identified by their International Organization for Standards (ISO) country code. ARE denotes United Arab Emirates, BDI Burundi, BFA Burkina Faso, BGD Bangladesh, BHR Bahrain, BLR Belarus, BRN Brunei, GHA Ghana, ISR Israel, JOR Jordan, KOR South Korea, LUX Lux-embourg, MHL Marshall Islands, MUS Mauritius, QAT Qatar, RWA Rwanda, SGP Singapore, SRB Serbia, SYC Seychelles, and ZMB Zambia.
DISCUSSION
Our analysis of the global trends in cardiovascular mortality shows the degree to which population aging and growth have offset reductions in cardiovascular mortality over the past two decades. For the most common cause of cardiovascular death, ischemic heart disease, the number of deaths increased by an estimated 41.7% from 1990 to 2013. Population aging contributed to an estimated 52.5% increase in these deaths, whereas population growth contributed to an estimated 23.6% increase. On the basis of these estimates, large reductions in the age-specific risk of death from ischemic heart disease have led to almost 2 million fewer deaths than would have been expected had death rates remained unchanged from 1990.
Dramatic reductions in cardiovascular deaths due to epidemiologic change can be seen in some regions, especially in high-income countries. These changes are probably due to the combined effect of birth cohorts’ decreased exposure to tobacco smoking, improvements in diet, and improved treatment of cardiovascular disease and cardio-metabolic risk factors targeting the prevention of cardiovascular disease, and improved treatment of cardiovascular disease.10 For example, the most dramatic declines in the prevalence of tobacco smoking have occurred in high-income regions, including Japan, South Korea, Canada, Italy, Germany, and the United Kingdom.11 A deterministic health policy model indicated that 40 to 55% of the decline in coronary heart disease in high-income countries can be attributed to the effects of medical and surgical treatments.12 However, the determination of the causes of the decline in age-specific rates of cardiovascular death is beyond the scope of our analysis.
In the high-income Asia–Pacific region, the potential for an increase in cardiovascular mortality caused by a rapidly aging population appears to have been limited by the world’s largest decline in age-specific rates of cardiovascular death. In contrast, South Asia had a dramatic rise in cardiovascular deaths due to population growth and aging without a significant decline in cardiovascular deaths due to epidemiologic change. North Africa and the Middle East offset a similar trend in population growth and aging with a significant decline in age-specific death rates.
In cardiovascular epidemiology, the effect of age is often removed in order to isolate modifiable risk factors. However, health-system planning also requires an understanding of the absolute burden of disease and the effect of aging. For example, countries with a declining incidence of myocardial infarction may still need to invest heavily in health promotion and treatment given trends in population growth and aging that increase the number of cases. Rather than using crude overall death rates across large age ranges, epidemiologists could use age-specific death rates to benchmark the performance of the health care system in a given country over time. Particular attention will need to be paid to the calculation of the age-specific metric when measuring progress toward the goal chosen by the United Nations for 2025 — a 25% reduction in the probability of premature death due to cardiovascular disease among persons between the ages of 30 and 70 years.
Our analysis adds to the perspective of Yusuf and colleagues on the effects of cardiovascular disease in developing countries.13,14 As they have noted, the classic model of “epidemiologic transition” does not fully reflect the heterogeneity of the burden of cardiovascular disease across countries. Our analysis shows that without the effect of population growth and aging, epidemiologic change would have led to a reduction in the numbers of cardiovascular deaths in most regions. However, in regions where this decrease was relatively small (i.e., regions in category 1), the combined effect of population growth and aging poses the greatest threat. We also show that increases in GDP per capita do not correlate well with declines in age-specific risk. Therefore, governments should not expect economic growth alone to address their countries’ burden of cardiovascular disease.
There are several limitations to our approach. First, cause-specific mortality data are lacking or of limited quality in some countries. Ensemble models incorporate data on regional patterns of mortality and other available information to derive estimates for countries with limited records on mortality. As a result, our estimates of the global burden of disease may not account for the actual variation in cardiovascular mortality among some countries. However, the rigorous out-of-sample predictive validity testing used in GBD 2013 is cause for some confidence. Second, although the use of codes from the International Classification of Diseases for death certification is a long-standing and widely accepted practice, cardiovascular diseases are complex and often attended by coexisting conditions. Our standard approach of attributing each death to a single underlying cause is intentionally defined according to GBD 2013 methods for the purpose of comparability and clarity. However, there will be some degree of misclassification bias. For example, undiagnosed diabetes may have preceded ischemic heart disease, or atrial fibrillation may have caused ischemic stroke. Furthermore, the remarkable increase in the age-specific rate of death from atrial fibrillation probably reflects increases in the screening, recognition, and attribution of death to atrial fibrillation in addition to changes in disease epidemiology. Similarly, the number of deaths resulting from rheumatic heart disease may not be completely captured by vital records in regions in which the condition is endemic. Third, we selected what we believe to be a straightforward procedure for decomposing death rates. However, calculations made with the traditional Shapley method and other methods used in econometrics may produce different results.6 Finally, we recognize that patterns of disease burden vary not just between but also within countries. Any summary provided at the level of a region or country may mask significant disparities within that area.
In conclusion, we found that population aging and growth accounted for the increase in the number of global deaths from cardiovascular disease between 1990 and 2013, despite an overall decrease in age-specific death rates in most regions. In only a few regions have gains in cardiovascular health offset these demographic forces to a degree sufficient to cause a decline in the number of cardiovascular deaths.
Supplementary Material
Acknowledgments
Supported by the Bill and Melinda Gates Foundation, a Western States American Heart Association Postdoctoral Fellowship (to Dr. Roth), and a National Heart, Lung, and Blood Institute award (K08 HL089675-01A1) and a Columbia University Irving Scholarship (to Dr. Moran).
APPENDIX
The authors’ affiliations are as follows: the Department of Medicine, Division of Cardiology (G.A.R.), and the Institute for Health Metrics and Evaluation (G.A.R., M.H.F., R.B., G.N., M.N., C.J.L.M.), University of Washington, Seattle; Department of Medicine, Division of General Medicine, Columbia University, New York (A.E.M.); National Institute for Stroke and Applied Neurosciences, Faculty of Health and Environmental Sciences, Auckland University of Technology, Auckland, New Zealand (V.L.F.); and the Center for Translation Research and Implementation Science, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD (G.A.M.).
Footnotes
The authors’ affiliations are listed in the Appendix.
The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, National Institutes of Health, or Department of Health and Human Services.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beaglehole R, Bonita R, Horton R, et al. Measuring progress on NCDs: one goal and five targets. Lancet. 2012;380:1283–5. doi: 10.1016/S0140-6736(12)61692-4. [DOI] [PubMed] [Google Scholar]
- 3.A comprehensive global monitoring framework, including indicators, and a set of voluntary global targets for the prevention and control of noncommunicable diseases. Geneva: World Health Organization; Jul, 2012. http://who.int/nmh/events/2012/discussion_paper3.pdf. [Google Scholar]
- 4.Ezzati M, Vander Hoorn S, Lawes CMM, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2(5):e133. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;385:117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shorrocks AF. Decomposition procedures for distributional analysis: a unified framework based on the Shapley value. J Econ Inequal. 2013;11:99–126. [Google Scholar]
- 7.Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10:1. doi: 10.1186/1478-7954-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James SL, Gubbins P, Murray CJ, Gakidou E. Developing a comprehensive time series of GDP per capita for 210 countries from 1950 to 2015. Popul Health Metr. 2012;10:12. doi: 10.1186/1478-7954-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 11.Ng M, Freeman MK, Fleming TD, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA. 2014;311:183–92. doi: 10.1001/jama.2013.284692. [DOI] [PubMed] [Google Scholar]
- 12.O’Flaherty M, Buchan I, Capewell S. Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s? Heart. 2013;99:159–62. doi: 10.1136/heartjnl-2012-302300. [DOI] [PubMed] [Google Scholar]
- 13.Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–64. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 14.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.