Abstract
Hypertension and diabetes are clinical conditions which contribute to the development of chronic kidney disease as well as risk factors for cardiovascular events. In recent years, lipocalin-type-prostaglandin-D-synthase (beta trace protein; BTP) has increasingly been studied as an alternative to creatinine for the evaluation of renal function as well as for being a possible biomarker for cardiovascular disease. It is expected that the levels of BTP in patients with cardiovascular disease are elevated, as is the case with patients with renal dysfunction. The objective of this study is to realize a systematic review of the pertinent literature in respect to BTP as a biomarker of renal dysfunction in diabetic patients. Using the database MEDLINE, a search up to year 2014 was conducted using the follow descriptors: “lipocalin type prostaglandin d synthase” AND “diabetes”; “lipocalin type prostaglandin d synthase” and “diabetic nephropathy”; “beta trace protein” AND “diabetes”; “beta trace protein” AND “diabetic nephropathy”. The criteria used for inclusion were the presence of the referring to terms in title or abstract and study conducted in humans. About 17 articles were selected, of which six articles were duplicates, and of which six articles did not investigate any possible relationship between the protein (BTP) and either diabetes or nephropathy. The final result yielded five articles to be analyzed. This review found BTP is not influenced by race, by body mass index nor by patient’s sex. BTP can be considered as a reliable early biomarker of renal dysfunction in diabetics. BTP is associated with metabolic syndrome and is also associated with greater cardiovascular risk. Prospective data establishing a correlation between BTP and mortality would have been of great interest, but such articles were not found in this review.
Keywords: renal lesions, type 2 diabetes, lipocalin-type-prostaglandin-D-synthase, diabetes predictor
Introduction
Research has shown that both systemic hypertension and type 2 diabetes are multi-factorial clinical conditions which present metabolic alterations as well as alterations to the target organ. These alterations in turn result in an increased risk of cardiovascular events as well as renal insufficiency.1,2
Currently, the glomerular filtration rate (GFR) is considered to be the gold standard to measure renal function. However, given the limitations of creatinine as a biomarker of this GFR, and therefore of renal function, new alternative biomarkers are being investigated, such as low molecular weight proteins.3
Lipocalin-type-prostaglandin-D-synthase (or, beta trace protein, BTP) can be considered a protein with a double function: first, BTP acts as an enzyme in the production of PGD2; and second, after being secreted, BTP acts as an extracellular transporter due to its lipophilic nature. It has been identified in many fluids and tissues since it was first isolated in cerebral spinal fluid in 1961. Since then, BTP levels were measured in other tissues like leptomeninges, arachnoid cells, vascular endothelial cells, skin melanocytes and gastric tissue, proximal tubules, loop of Henle and glomerulus as well.4
The overall importance of BTP to the cardiovascular system is confirmed by the fact that mRNA for BTP has been found in myocardial cells, in endocardial cells of both the atrium and the ventricle, in coronary arteries, in smooth muscle cells, and even in arteriosclerotic plaque.5
Given the widespread presence of mRNA of BTP in these locations, elevated levels of BTP should be expected in patients with cardiovascular diseases. In a recent trial, patients with atrial fibrillation were divided according to their BTP serum levels. Their major adverse cardiac outcomes were assessed and also the major bleeding episodes. Those with a higher level of BTP had a higher mortality rate, higher bleeding events, and also more cardiac adverse events.6
The objective of this study is to realize a systematic review of the literature of the association between lipocalin-type-prostaglandin-D-synthase and kidney disease in patients with type 2 diabetes.
Methods
Using the database MEDLINE, a search was conducted using the follow descriptors: “lipocalin type prostaglandin d synthase” AND “diabetes”; “lipocalin type prostaglandin d synthase” and “diabetic nephropathy”; “beta trace protein” AND “diabetes”; “beta trace protein” AND “diabetic nephropathy”.
The criteria used for inclusion in the study were: the presence of the referring terms in the title or abstract; the research had been conducted with human subjects; and the research had been conducted within the last 10 years. Articles which included “beta trace protein” or “lipocalin type prostaglandin” in the title or abstract but did not indicate an association with the terms “diabetes” or “diabetic nephropathy” were excluded.
The review was conducted independently by two researchers, while a third researcher revised the final selection using the pre-established criteria.
Results
About 17 articles were selected, of which six articles were duplicates, and of which six articles did not investigate any possible relationship between the protein (BTP) and either diabetes or nephropathy. The final result yielded five articles (Table 1). Figure 1 shows a flow chart illustrating the selection of articles. Also, other articles related to BTP as a biomarker in other situations were added in the “Discussion” section.
Table 1.
Articles listed in this review
| Author | Year | Study design | Conclusion |
|---|---|---|---|
| Cheung et al9 | 2013 | Retrospective | Metabolic syndrome is associated with a reduced serum level of BTP |
| Juraschek et al7 | 2013 | Cohort | BTP, beta-2-microglobulin, cystatin C, and creatinine differ in their associations with demographic and clinical factors, suggesting variation in their non-GFR determinants |
| Kobata et al11 | 2004 | Cross-sectional | Serum BTP was a good marker for the identification of early renal impairment in type 2 diabetes |
| Uehara et al12 | 2009 | Cross-sectional | Urinary BTP excretions reflect the current increased permeability of injured glomerular capillary walls and better predict the future status of renal injury in type-2 diabetes with <30 mg/gCr albuminuria |
| Yoshikawa et al10 | 2007 | Cross-sectional | In type 2 diabetes patients, the elevation of urinary BTP secretion was closely associated with cardiovascular events and may be a supplemental or additional marker for metabolic syndrome criteria |
Abbreviations: BTP, beta trace protein; GFR, glomerular filtration rate.
Figure 1.
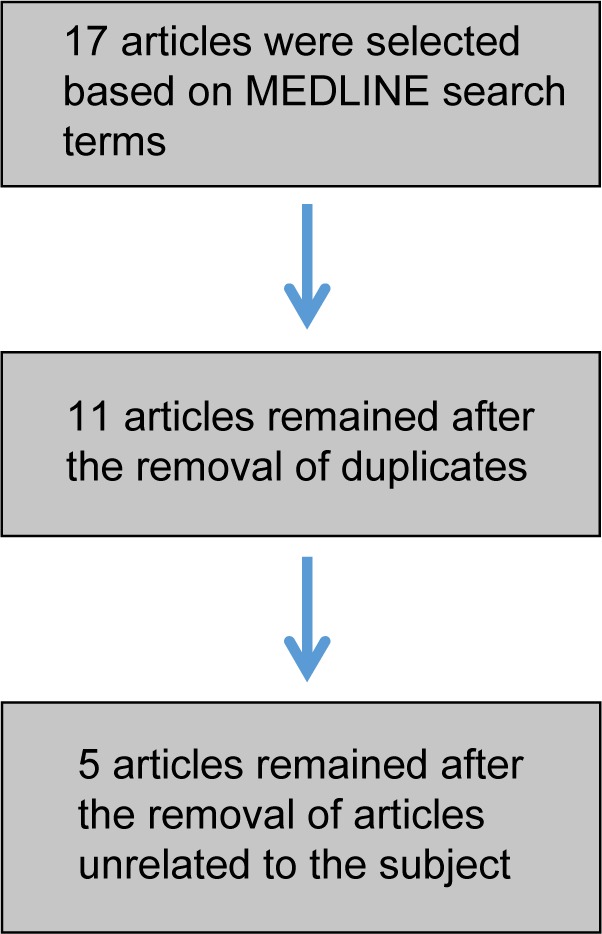
Flowchart of article selection.
Discussion
BTP is a member of the lipocalin family of proteins and has a low molecular weight. BTP was initially isolated from the spinal fluid, but an evaluation of the cDNA present in the fluid indicated that BTP could be isolated from various other tissues and fluids of the human body.7
Bachmann-Harildstad et al isolated BTP from the middle ear effusions of 103 infants with otitis media. It was the first report of isolation BTP in the tympanic cavity. BTP is found in abundance in the near regions of perilymph of the cochlea and cerebral spinal fluid. Moreover, in these infants, the effusion concentration was six times higher than the plasmatic ones. The inflammatory process might alter the permeability of the barrier from the perilymph cochlea and cerebral spinal fluid.8
Recently interest has grown in the study of BTP as an alternative to serum creatinine for the evaluation of renal function as well as being a biomarker for cardiovascular diseases. The expression of BTP is not influenced by race, by body mass index, nor by the sex of the patient, when standardized to creatinine, to beta-2-microglobulin and to cystatin C.7
In the last 10 years, only two articles have shown a direct relationship between alterations in BTP and either diabetes or kidney disease.9,10 Kobata et al showed the relationship between stages of diabetic nephropathy and BTP serum levels. There was a close relationship between higher levels of BTP in type 2 diabetic patients with macroalbuminuria but no renal dysfunction.11
As a predictor of early renal dysfunction, urinary BTP levels better predicted kidney disease than other traditional biomarkers when albuminuria was present in levels higher than 30 mg/g creatinine. Also, in the prospective arm of the study, those without albuminuria but higher excretion of BTP had evoluted with worse kidney function.12
In newborns, BTP is promising as a marker of GFR because its level rises as the gestational period advances. Creatinine should increase because of the gain in muscle mass of the baby. Cystatin C is a protein that crosses the maternal placenta and a rise in its level might be due to the influence of maternal cystatin. Only BTP remains constant suggesting its performance as a better GFR marker in newborns than creatinine and cystatin C.13
Cheung et al and Yoshikawa et al found a positive association with BTP in patients with metabolic syndrome (MetS) and kidney damage.9,10 Their results showed a different interpretation according to where BTP was measured. Cheung et al gathered 3,136 participants aged ≥20 years from the National Health and Nutrition Examination Survey III. Patients with reduced serum levels of BTP were associated positively with MetS and worse GFR even after adjusted models by ethnicity, age, and sex.9
Yoshikawa et al measured urinary levels of BTP in a cross-sectional study with type 2 diabetic Japanese patients. There was a direct association between the rise of urinary concentration of BTP and worse GFR and also MetS in this population. Though, the rate of cardiovascular events in the follow-up period was higher in those with higher urinary levels of BTP.10
Articles containing prospective data establishing a correlation between BTP and either morbidity or mortality in the spectrum of kidney disease would have been of great interest however there were no such articles in the period studied.
In summary, BTP can be considered as a promising biomarker of kidney dysfunction in diabetes and is associated with the presence of MetS and greater cardiovascular risk.
Acknowledgments
This study received funding from São Paulo Research Foundation (FAPESP-2014/04596-8).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Department of Arterial Hypertension of Brazilian Society of Cardiology. Alessi A, Bonfim AV, et al. I Brazilian Position Statement on Arterial Hypertension and Diabetes Mellitus. Arq Bras Cardiol. 2013;100(6):491–501. doi: 10.5935/abc.20130123. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Standards of medical care in diabetes. Diabetes Care. 2013;36(Suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão; Sociedade Brasileira de Nefrologia VI Diretrizes Brasileiras de Hipertensão [VI Brazilian Guidelines on Hypertension] Arq Bras Cardiol. 2010;95(1 Suppl):1–51. Portuguese. [PubMed] [Google Scholar]
- 4.White CA, Ghazan-Shahi S, Adams MA. β-Trace protein: a marker of GFR and other biological pathways. Am J Kidney Dis. 2015;65(1):131–146. doi: 10.1053/j.ajkd.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 5.Orenes-Pinero E, Manzano-Fernández S, López-Cuenca Á, et al. β-Trace protein: from GFR marker to cardiovascular risk predictor. Clin J Am Soc Nephrol. 2013;8(5):873–881. doi: 10.2215/CJN.08870812. [DOI] [PubMed] [Google Scholar]
- 6.Vílchez JA, Roldán V, Manzano-Fernández S, et al. β-Trace protein and prognosis in patients with atrial fibrillation receiving anticoagulation treatment. Chest. 2013;144(5):1564–1570. doi: 10.1378/chest.13-0922. [DOI] [PubMed] [Google Scholar]
- 7.Juraschek SP, Coresh J, Inker LA, et al. Comparison of serum concentrations of β-trace protein, β2-microglobulin, cystatin C, and creatinine in the US population. Clin J Am Soc Nephrol. 2013;8(4):584–592. doi: 10.2215/CJN.08700812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bachmann-Harildstad G, Müller R, Michel O. Beta-trace protein in pediatric otitis media with effusion. Int J Pediatr Otorhinolaryngol. 2014;78(4):659–662. doi: 10.1016/j.ijporl.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 9.Cheung CL, Cheung TT, Lam KS, Cheung BM. Reduced serum beta-trace protein is associated with metabolic syndrome. Atherosclerosis. 2013;227(2):404–407. doi: 10.1016/j.atherosclerosis.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Yoshikawa R, Wada J, Seiki K, et al. Urinary PGDS levels are associated with vascular injury in type 2 diabetes patients. Diabetes Res Clin Pract. 2007;76(3):358–367. doi: 10.1016/j.diabres.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Kobata M, Shimizu A, Rinno H, et al. Beta-trace protein, a new marker of GFR, may predict the early prognostic stages of patients with type 2 diabetic nephropathy. J Clin Lab Anal. 2004;18(4):237–239. doi: 10.1002/jcla.20029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uehara Y, Makino H, Seiki K, et al. Urinary excretions of lipocalin-type prostaglandin D synthase predict renal injury in type-2 diabetes: a cross-sectional and prospective multicentre study. Nephrol Dial Transplant. 2009;24(2):475–482. doi: 10.1093/ndt/gfn515. [DOI] [PubMed] [Google Scholar]
- 13.Filler G, Lopes L, Harrold J, Bariciak E. β-trace protein may be a more suitable marker of neonatal renal function. Clin Nephrol. 2014;81(4):269–276. doi: 10.5414/CN108089. [DOI] [PubMed] [Google Scholar]


