Abstract
Background
Coronary artery bypass graft (CABG) surgery patients participating in cardiac rehabilitation (CR) experience improvements in aerobic fitness but there has been little study of outcomes for heart valve (HV) surgical patients. The primary aims of this study are to evaluate baseline peak aerobic capacity for HV patients participating in CR and to compare outcomes between HV and CABG patients.
Methods
Five hundred and seventy six consecutive patients who underwent HV (N=125), valve plus coronary artery bypass surgery (HV+CABG, N=57), or CABG (N=394) (all with classic sternotomy) and enrolled in CR were prospectively studied. Changes in outcome measures were assessed for individuals that completed CR (N=313).
Results
Valve patients were significantly older and had a greater percent of females than the CABG only group. Combining HV and HV+CABG groups, valvular disorders included: 134 mitral, 39 aortic and 8 combined abnormalities (mitral and aortic). For the entire cohort, the mean number of CR exercise sessions attended was 23.6±11.7. Peak VO2 increased 19.5% from 17.4±4.4 to 20.8±5.5 mLO2*kg−1*min−1(p<0.0001). Improvements in peak VO2 with CR exercise training were similar between the 3 groups of patients. Within the group of patients who had HV surgery, percent change in peak VO2 was similar between the 3 types of valvular abnormalities (i.e. Mitral [19.2%], Aortic [24.4%], and Mitral + Aortic [21.9%]) (p=0.27).
Conclusions
Heart valve surgery patients gain similar improvements in aerobic fitness from participating in CR exercise training as individuals that have CABG. The observed improvements in aerobic fitness are similar regardless of the type of valve abnormality or whether coronary artery bypass was performed concurrently.
Introduction
Individuals with heart valve (HV) disorders, in contrast with coronary bypass grafting surgery (CABG) patients, often experience cardiac abnormalities and diminished functional capacity for several years before surgery1. A period of post-surgical convalescence results in further declines in functional capacity for both HV and CABG patients. Peak aerobic capacity for CABG patients entering CR is exceedingly low2 and there is evidence that values for individuals after HV surgery are particularly reduced3–5.
The Center for Medicare and Medicaid Services expanded cardiac rehabilitation (CR) coverage in 2006 to include patients following HV surgery. Current CR guidelines for HV patients are based primarily on results from randomized clinical trials in patients with coronary artery disease6. While patients after CABG have experienced improvements in aerobic fitness from CR exercise7, 8, there is a paucity of studies examining the outcomes for HV patients. The primary aims of this study, therefore, are to evaluate baseline peak aerobic capacity for HV patients participating in CR and to compare demographic and exercise training-related outcomes between patients undergoing HV and CABG surgery. We hypothesized that patients after HV surgery are less fit than patients after CABG but benefit similarly from the exercise training component of CR.
Methods
Five hundred and seventy six consecutive patients who underwent open heart surgery with a classic sternotomy : HV (N=125), valve plus coronary artery bypass surgery (HV+CABG, N=57), or CABG (N=394) and enrolled in CR between January 2006 and December 2012 were prospectively studied. The study protocol was approved by the Internal Review Board at the University of Vermont and Fletcher Allen Health Care.
The number of CR sessions completed and, when appropriate, the self-reported reason for program discontinuation was recorded. Participation in CR was individualized. The number of CR sessions attended (up to maximum of 36) was determined by medical necessity, insurance coverage, an individual’s goals and objectives and personal preference. Participants were considered “completers” of the program if they attended CR sessions and underwent a post-program assessment.
Peak aerobic capacity was assessed during symptom-limited graded exercise test on a treadmill prior to commencing with CR. Post-program exercise stress test was performed approximately 4-months from the baseline evaluation, regardless of the number of CR sessions attended. If an individual was unable to walk on a treadmill at a minimum of 2 miles per hour a stress test was not performed (N=52, 9%). Expired gas was continuously analyzed during the modified Balke exercise testing protocol using a Medgraphics Ultima CPX metabolic cart (Minneapolis, MN) and subjects exercised to voluntary exhaustion. Peak VO2 was considered to be the highest 30 second average during the test.
Handgrip strength was measured using the dominant hand with the shoulder adducted and neutrally rotated, elbow in 90 degrees of flexion and the forearm and wrist neutrally positioned using a Jamar handgrip dynamometer (Jamar, Bolingbrook, Il). The reported handgrip measure represented the mean of 3 consecutive attempts.
A diagnosis of hypertension and diabetes mellitus (DM) were recorded at the point of entry to CR and smoking history was self-reported. Prescribed cardiac and preventive medications were reviewed and confirmed with the patient at entry to CR. Glycated hemoglobin (HbA1c) values were obtained during hospitalization. A co-morbidity score was determined by assessing for peripheral vascular disease, cerebrovascular disease, chronic lung disease or orthopedic limitations. If a co-morbid condition was present it was quantified by severity as follows: 1, present but not exercise–limiting; 2, present and impacts on exercise performance; and 3, exercise-limiting. A total co-morbidity score ranging from 0 to 12 was thus determined. Self-reported physical functioning was assessed using the Medical Outcomes Study Short Form-36 survey questionnaire9 (0–100 scale) with 100 representing excellent physical functioning. Depressive symptoms were assessed using the Geriatric Depression Scale10 scored 0–15 was recorded with higher numbers indicating more depressive symptoms.
Specific details regarding surgery were gathered retrospectively via chart review. The type of valve abnormality was obtained from the surgical report as well as the number of surgical arterial anastomosis. Left ventricular ejection fraction was obtained, from the pre-operative echocardiogram or if not available, from the left heart catheterization. Whether the patient was discharged to home or sub-acute rehabilitation was documented from the hospital discharge records. The time between the date of hospitalization and enrollment in CR was recorded.
The exercise training program has been described elsewhere11 and is similar to that performed at most rehabilitation programs around the United States12. Subjects performed CR exercise at an intensity of 70 to 85% of their peak heart rate (65 to 75% of peakVO2) and/or a Borg Scale rating of perceived exertion (RPE) of between “light” and “somewhat hard” (12 to 14 on a scale of 6 to 20)13. Generally, individuals exercise for 45 to 60 minutes per CR session on a variety of modalities including: treadmills, elliptical trainers and rowing, cycle and arm ergometers. Typically, an exercise prescription consisted of 30 minutes of treadmill walking and 8 minutes on 2 other ergometers. Patients performed weight-training exercise consisting of 1 set of 10 repetitions for 6 different exercise targeting major muscle groups. Upper body strength training began 3-months post-operatively. All patients were encouraged to exercise aerobically on non-CR days.
Statistical analysis
Values are presented as mean ± standard deviation. For analysis, the cohort was separated into 3 groups: HV, HV+CABG, and CABG. Analysis of variance was used to compare baseline variables between surgical groups. Contingency table analysis was used to compare nominal variables. For all valve patients, a stepwise linear multiple regression analysis was used to determine which variables independently correlated with change in peakVO2. Variables included in the regression analysis were age, gender, days from the index cardiac event and entry stress test, baseline body weight, entry body mass index (BMI), waist circumference, type of valve abnormality, left ventricular ejection fraction, number of CR sessions attended, peakVO2, handgrip strength, and total co-morbidity, depression and physical function scores. A level of significance of P < 0.05 (two-tailed test) was used for hypothesis testing. Statistical analyses were carried out using Stat View (SAS Institute Inc, Cary, NC) statistical package.
Results
Demographic and clinical characteristics for the cohort are listed in Table 1. Valve + CABG were significantly older than HV only patients and both groups of valve patients were significantly older than individuals in the CABG group. The number of days from index event to entry into CR was similar between groups. The percentage of females was greater for HV than in the HV+CABG and CABG groups. Individuals in the CABG group weighed significantly more than HV patients but weight was similar between valve groups. For both BMI and waist circumference, significantly higher values were observed in each of the CABG groups compared to HV only patients.
Table 1.
Clinical and demographic characteristics for the entire cohort and separated by surgical group (N=576).
|
Total ‡ N=576 |
Valve N=125 |
Valve + CABG N=57 |
CABG N=394 |
Between group p Value |
|
|---|---|---|---|---|---|
| Age (years) | 64.9±10.4 | 66.3±12.2 | 71.0±10.4 | 63.6±9.4 | 0.0001 |
| Days since event | 49.2±35.5 | 52.6±40.9 | 55.2±27.9 | 47.4±34.6 | 0.6 |
| Male (%) | 78.0 | 64.0 | 71.9 | 83.2 | 0.0001 |
| Weight (kg) | 84.3±17.7 | 79.0±17.2 | 83.2±17.2 | 90.0±17.6 | 0.003 |
| Waist (cm) | 100.5±13.7 | 95.8±13.7 | 101.1±13.0 | 101.6±13.5 | 0.002 |
| Body Mass Index (kg/m2) | 29.0 ± 5.5 | 27.6 ± 5.0 | 29.6 ± 5.9 | 29.4 ± 5.5 | 0.006 |
| Type of Valve (N) Mitral Aortic Mitral & Aortic |
134 39 8 |
85 31 8 |
49 8 |
Not applicable | |
| Anastomosis (N) | 3.2 ± 1.1 | Not Applicable | 2.0 ± 1.0 | 3.4 ± 1.0 | |
| Ejection Fraction (%) | 55.2±11.5 | 58.1±9.8 | 56.1±13.1 | 54.3±11.5 | 0.01 |
| Risk Factors (%) Hypertension Type 2 Diabetes Mellitus Current smoker Ex-smoker |
68.4 26.4 4.5 43.2 |
61 12.8 0.8 33.6 |
73 21.1 3.5 47.4 |
74 31.5 5.8 45.6 |
0.02 0.001 0.06 0.05 |
| Glycated hemoglobin A1c | 6.3 ± 1.6 | 5.7± 1.2 | 5.8 ± 0.5 | 6.6 ± 1.8 | 0.002 |
| Medication (%) β Blocker Calcium Blocker ACE-Inhibitor Statin |
86.1 10.9 41.8 84.2 |
80.0 11.2 36.0 57.6 |
91.2 12.3 36.8 36.8 |
87.3 10.7 44.4 91.9 |
0.07 0.92 0.19 0.0001 |
| Co-morbidity Score | 0.6 ± 1.3 | 0.5 ± 1.1 | 0.7 ± 1.3 | 0.7 ± 1.3 | 0.45 |
| Sub-Acute Rehabilitation (%) | 12.9 | 22.4 | 26.3 | 7.9 | 0.0001 |
| Physically unable to perform stress test (N, %) | 52, 9.0% | 8, 6.4% | 11, 19.3% | 33, 8.4% | 0.02 |
| Peak VO2 (mLO2*kg−1*min−1) (N=524) |
17.5 ± 4.7 | 17.3 ± 5.2 | 15.5 ± 4.8 | 17.8 ± 4.4 | 0.006 |
| Handgrip Strength (kg) | 15.5 ± 4.9 | 14.3 ± 5.3 | 14.4 ± 5.0 | 16.0 ± 4.6 | 0.005 |
| Physical Function Score * | 57.4 ± 22.4 | 58.3 ± 20.9 | 56.1 ± 23.0 | 57.3 ± 22.8 | 0.87 |
| Depression Scale † | 3.4 ± 2.9 | 3.2 ± 2.6 | 3.5 ± 3.1 | 3.4 ± 3.0 | 0.86 |
| Number of cardiac rehabilitation session | 23.6 ± 11.7 | 24.7 ± 11.5 | 26.6 ± 11.4 | 22.8 ± 11.8 | 0.05 |
Values are presented mean ± SD. Categorical variables are presented as percentage.
Total cohort and surgical groups: Heart valve alone; Valve + Coronary artery bypass surgery (CABG), and CABG
Physical Function Score, Medical Outcomes Short-Form-36 Questionnaire
Geriatric Depression Scale
Combining valve groups, valvular disorders included: 134 mitral, 39 aortic and 8 combined abnormalities (mitral and aortic). There were a mean of 3.2±1.1 and 2.0±1.0 anastomosis in the CABG and the HV+CABG groups, respectively. Left ventricular ejection fraction was significantly higher in both HV groups compared to CABG patients. Prevalence of hypertension and smoking along with a diagnosis of type 2 diabetes mellitus (T2DM) and were significantly lower in the HV group than both of the CABG groups. HbA1c values were significantly lower in both of the valve groups compared to CABG patients. Cardio-preventive medication (β-Blocker, Calcium Channel Blocker and Angiotensin-converting-enzyme inhibitor) use was similar between groups except that significantly more patients in CABG group were on statin therapy. Co-morbid score was similar between the 3 groups. Upon hospital discharge, significantly more patients in the valve groups convalesced at a sub-acute rehabilitation facility than individuals in the CABG-only group.
Overall, 52 individuals or 9% of the cohort were unable to perform an entry stress test. Compared to CABG and HV patients, a significant greater percentage of individuals in the HV+CABG group were unable to perform a baseline stress test. For individuals that were able to do an entry CR stress test, peak VO2 was lower in HV+CABG group than for CABG and HV patients. Handgrip strength was lower for both groups of valve patients compared to individuals with CABG. MOS-SF-36 and Geriatric Depression Scale scores were similar among all surgical groups. The mean number of CR sessions attended was significantly greater in the HV+CABG group than the CABG and HV groups.
Changes in outcome were assessed for individuals that had measures obtained at baseline and completion of CR (N=313, 54.3% of total). Consequently, individuals that “completed” the program but did not have baseline peak VO2 measurements were excluded. A similar percentage of patients in each group (CABG = 53.6%, HV = 58.4%, HV+CABG = 52.6%, p=0.55) had outcomes data for the program. For the entire cohort, the peak VO2 increased 19.5% from 17.4 ± 4.4 to 20.8 ± 5.5 mLO2*kg−1*min−1 (Table 2) (p<0.0001). Improvements in peak VO2 with CR exercise training were similar between the 3 groups of patients (Figure1).
Table 2.
Pre- and post-cardiac rehabilitation (CR) values for the entire cohort and separated by surgical group.
|
Total group N=313 |
Valve N=73 |
Valve + CABG N=29 |
CABG N=211 |
|
|---|---|---|---|---|
| Peak VO2 pre (mLO2*kg−1*min−1) post % change |
17.4±4.4 20.8±5.5 * + 19.5 |
17.2±5.1 20.7±6.1 * + 20.3 |
16.2±4.8 19.1±6.1 * + 17.9 |
17.7±4.1 21.1±5.2 * + 19.2 |
| Handgrip (kg) pre post % change |
15.3±4.8 16.5±5.3 * + 7.8 |
13.6±5.2 15.0±5.5 * + 10.3 |
14.6±4.7 16.1±5.5 † + 10.3 |
15.9 ± 4.6 17.0 ± 5.1* + 6.9 |
| Weight (kg) pre post |
82.0 ± 16.3 82.0 ± 16.3 |
77.6 ± 16.4 77.9 ± 16.7 |
80.7 ± 16.1 81.3 ± 15.7 |
83.7 ± 16.1 83.5 ± 16.2 |
| Physical Function pre post % change |
59.4±20.9 84.0±19.1* + 41.4 |
59.6±20.3 81.4±20.0 * + 36.6 |
60.2±22.1 85.2±19.1 * + 41.5 |
59.2±21.1 84.5±18.8 * + 42.7 |
| Depression Scale pre Post % change |
3.2 ± 2.7 1.9 ± 2.4 * − 40.6 |
3.2 ± 2.3 2.2 ± 2.4 † − 31.3 |
3.9 ± 3.2 2.4 ± 2.5 † − 38.5 |
3.1 ± 2.7 1.8 ± 2.3 * − 41.9 |
p<0.0001
p<0.05, within group
Comparison of between group difference with cardiac rehabilitation exercise, all p=NS
Figure 1.
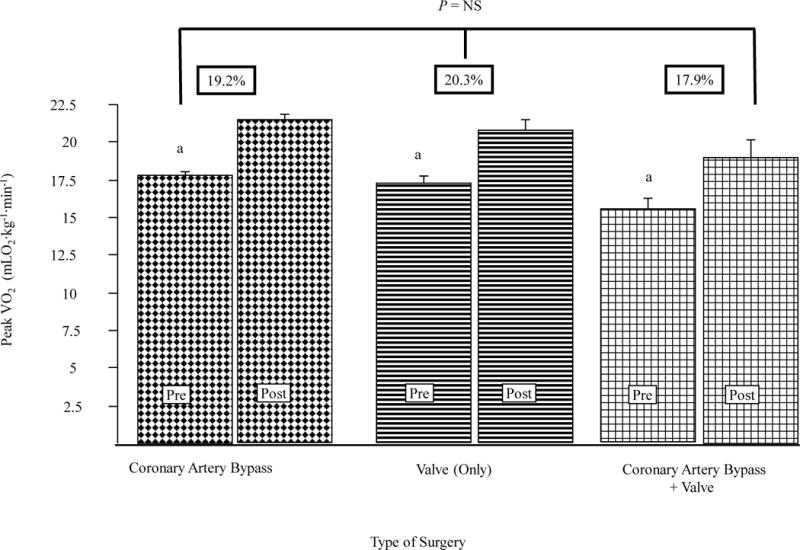
Exercise capacity according to type of surgery at the start and the end of cardiac rehabilitation is presented. Percent improvement from pre- to post-cardiac rehabilitation for each group is included above the bars.
aP <.0001 for within group comparisons.
P = NS for between group comparisons.
Within the group of patients who had valve surgery, the peak VO2 increased 22.0% from 16.8 ± 5.2 to 20.3 ± 6.4 mLO2*kg−1*min−1 (p<0.0001, data not shown). The percent increase in peak VO2 was similar between the 3 types of valvular abnormalities (i.e. Mitral [+19.2%], Aortic [+24.4%], and Mitral + Aortic [+21.9%]) (p=0.27, data not shown).
Forty-three (23.6%) of all valve patients went to sub-acute rehabilitation upon hospital discharge compared with 31 (7.9%) of the CABG patients. Compared to individuals that did not, a significantly greater percentage of individuals that went to sub-acute were unable to perform an entry stress test (4.3% vs 30.2%, respectively, p<0.0001). For those valve patients that performed a baseline stress test, individuals that went to sub-acute rehabilitation had a lower baseline peakVO2 than patients who were discharged to home (13.0±3.0 vs 17.6±5.2 mLO2*kg−1*min−1, respectively, p<0.0001). Similar improvements in peakVO2 were achieved for valve patients that went to sub-acute rehabilitation (2.7±2.1 mLO2*kg−1*min−1) compared to those that did not (3.5±2.8 mLO2*kg−1*min−1) (p<0.22, between groups). Additionally, among all individuals that went to sub-acute rehabilitation, similar improvements in peakVO2 were observed among CABG patients (+1.7±2.4 mLO2*kg−1*min−1) as compared to all valve patients (+2.6±2.1 mLO2*kg−1*min−1) (p<0.29, between groups).
Valve, HV+CABG, and CABG groups all achieved similar gains in strength as measure by handgrip dynamometer (Table 2). Self-reported physical function and Depression Questionnaire scores improved, overall, and the changes were similar between groups (Table 2). Weight was unchanged, overall, and within each group (Table 2).
For all valve patients, factors that correlated with improvement in peak VO2 included: HbA1c (r=−0.18, p<0.004); diagnosis of T2DM (r=−0.07, p<0.008); total co-morbid score (r=−0.06, p<0.02); age (r=−0.05, p<0.03); and there is a trend with the number of days between index event and entry to CR (r=−0.04, p<0.07). By stepwise multivariate analysis, HBA1c and age independently negatively correlated with change in peakVO2 (cumulative total r=0.51, adjusted R2=0.23, p<0.002).
Discussion
Our results demonstrate that patients that undergo heart valve surgery have a similar baseline peak aerobic capacity and achieve similar improvements in aerobic fitness from CR exercise training as individuals that have undergone CABG. Additionally, HV patients, regardless of the type of abnormality or whether coronary artery bypass grafting was performed concurrently, experience similar improvements with CR exercise capacity.
It has been previously reported that CABG patient participating in CR experience significant improvements in aerobic fitness7, 8. While previous studies have demonstrated improvements in aerobic fitness for post-surgical HV patients participating in CR14–17, less well studied is the effect of exercise training following HV or HV + CABG surgery compared with patients who had undergone CABG surgery. In a study of exclusively HV patients from Belgium, Pardaens, et al17, reported similar improvements in aerobic fitness to our results. Additionally, Pardaens, et al17 reported that HV patients, regardless of preoperative risk or type of surgery (mini- or full sternotomy or port access), obtain a similar benefit from training. Together, these studies confirm that exercise training protocols employed in CR are effective for patients after undergoing HV surgery, CABG or both.
It has previously been shown that exercise capacity is related to subsequent survival in individuals with coronary heart disease18–20. Additionally, improvement in peak VO2 with CR exercise training is associated with decreased mortality21. A previous study by Goel, et al22, reported a significant survival benefit with CR participation in patients undergoing HV+CABG. Further study is needed to determine if, absent coronary heart disease, a similar survival benefit exist with improvements in aerobic fitness for HV patients participating in CR.
While our study groups experience similar improvements in aerobic fitness as a result of participating in CR, significant differences at baseline exists between the groups. Valve + CABG are significantly older than HV only or CABG patients. Valve and HV + CABG patients are more likely to convalesce, post-hospital discharge, in a sub-acute rehabilitation facility. Additionally, the length of time to enroll in CR was longest and baseline peak VO2 is lowest in the HV + CABG group. Finally, Valve + CABG patients are more often deemed unable to perform a baseline stress test due to extremely low aerobic fitness levels. Together, these characteristics suggest that Valve + CABG are more disabled at entry to CR than CABG or HV patients. Valve + CABG patients complete more sessions of CR than the other groups; however, they experience similar improvements in aerobic fitness, hand grip strength, and self-reported physical function and depression scores.
For the entire study cohort, individuals that attended sub-acute rehabilitation were more likely to be deemed too unfit to perform a baseline stress test. For patients that performed a baseline stress test, attendees of sub-acute rehabilitation had a lower peak aerobic capacity. For individuals that had baseline and exit measures, however, peakVO2 improved similarly for those individuals that went to sub-acute rehabilitation as compared to those that did not. Consequently, despite being significantly less aerobically fit at entry to CR, individuals that convalesce in sub-acute rehabilitation facilities should be encouraged to participate in CR as they experience similar improvements in aerobic fitness as those patients that do not.
Among valve patients, a diagnosis of T2DM was negatively correlated with changes in peak VO2 and HbA1c was the strongest independent factor associated with improvements in aerobic fitness. For individuals with coronary heart disease, it has been previously shown that a diagnosis of T2DM is associated with lesser improvements in peak VO211, 23. Similarly, our results indicate that T2DM and HbA1c are negatively associated with changes in aerobic fitness for individuals rehabilitating from valve-related surgery.
In addition to HbA1c, age was the other independent predictor of change in peak VO2 among the valve patients. In previous reports of CABG patients, age was not correlated with change in peak VO211. In the current study, the valve patients were significantly older than individuals in the CABG group. Alternatives to currently employed exercise training protocols maybe indicated for older valve patients.
Our study has limitations. The results presented are from one CR center. The study design, while prospective, was observational and non-randomized. Cardiac rehabilitation, however, is considered standard of care12 precluding randomizing individuals to a non-exercising control group. Without a control group, the extent of the observed improvements in aerobic fitness that are spontaneous and the amount that is the result of participating in CR is unknown. Previous studies suggest, however, that without participating in CR exercise capacity does not improve for individual recovering from valve surgery24, 25. Despite the lack of a control group, our results are relevant as they represent what was observed in a clinical CR program. Our analysis is also limited in that we do not have outcome measures for the individuals that did not have both pre- and post-CR measures and we do not have information regarding exercise training intensity.
Conclusion
Patients that undergo heart valve surgery gain similar improvements in aerobic fitness from participating in CR exercise training as individuals that have undergone CABG. The observed improvements in aerobic fitness are similar regardless of the type of valve impairment or whether coronary artery bypass was performed concurrently. Additionally, CABG and HV patients experience similar improvements in strength, and self-reported physical function and depression scores.
Acknowledgments
This research was supported in part by National Institutes of Health Center of Biomedical Research Excellence award P20GM103644 from the National Institute of General Medical Sciences (NIGMS).
Footnotes
Statement of submission:
All authors have read and approved submission of the manuscript and the manuscript has not been published and is not being considered for publication elsewhere in whole or part in any language except as an abstract.
References
- 1.Bissessor N, Stewart R, Wee YS, et al. Complex valve disease: pre-surgical functional capacity evaluation using peak oxygen consumption. J Heart Valve Dis. 2009 Sep;18(5):554–61. [PubMed] [Google Scholar]
- 2.Ades PA, Savage PD, Brawner CA, et al. Aerobic capacity in patients entering cardiac rehabilitation. Circulation. 2006;113(23):2706–12. doi: 10.1161/CIRCULATIONAHA.105.606624. [DOI] [PubMed] [Google Scholar]
- 3.Khan JH, McElhinney DB, Hall TS, Merrick SH. Cardiac valve surgery in octogenarians: improving quality of life and functional status. Arch Surg. 1998 Aug;133(8):887–93. doi: 10.1001/archsurg.133.8.887. [DOI] [PubMed] [Google Scholar]
- 4.Niemelä K, Ikäheimo M, Takkunen J. Determination of the anaerobic threshold in the evaluation of functional status before and following valve replacement for aortic regurgitation. Cardiology. 1985;72(4):165–73. doi: 10.1159/000173870. [DOI] [PubMed] [Google Scholar]
- 5.Nakamura M, Chiba M, Ueshima K, et al. Effects of mitral and/or aortic valve replacement or repair on endothelium-dependent peripheral vasorelaxation and its relation to improvement in exercise capacity. Am J Cardiol. 1996 Jan 1;77(1):98–102. doi: 10.1016/s0002-9149(97)89146-1. [DOI] [PubMed] [Google Scholar]
- 6.Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;7:CD001800. doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lan C, Chen SY, Hsu CJ, Chiu SF, Lai JS. Improvement of cardiorespiratory function after percutaneous transluminal coronary angioplasty or coronary artery bypass grafting. Am J Phys Med Rehabil. 2002 May;81(5):336–41. doi: 10.1097/00002060-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Hsu CJ1, Chen SY, Su S, et al. The effect of early cardiac rehabilitation on health-related quality of life among heart transplant recipients and patients with coronary artery bypass graft surgery. Transplant Proc. 2011 Sep;43(7):2714–7. doi: 10.1016/j.transproceed.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 9.Ware JE, Sherbourne CD. The Medical Outcomes Study: a 36 item short-form health survey (SF-36), Conceptual framework and item selection. Med Core. 1992;30:473–83. [PubMed] [Google Scholar]
- 10.Burke WJ, Roccaforte WH, Wengel SP. The Short Form of the Geriatric Depression Scale: A Comparison With the 30-Item Form. J Geriatr Psychiatry Neurol. 1991;4:173–178. doi: 10.1177/089198879100400310. [DOI] [PubMed] [Google Scholar]
- 11.Savage PD, Antkowiak M, Ades PA. Failure to improve cardiopulmonary fitness in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2009 Sep-Oct;29(5):284–91. doi: 10.1097/HCR.0b013e3181b4c8bd. [DOI] [PubMed] [Google Scholar]
- 12.Williams MA, editor. AACVPR Guidelines for cardiac rehabilitation programs. 5. Human Kinetics; Champaign, Il: 2013. [Google Scholar]
- 13.Thompson WR, editor. ACSM’s Guidelines for Exercise Testing and Prescription. 8. Lippincott Williams and Wilkins; Baltimore, MD: 2010. [Google Scholar]
- 14.Gohlke-Bärwolf C, Gohlke H, Samek L, et al. Exercise tolerance and working capacity after valve replacement. J Heart Valve Dis. 1992;1(2):189–95. [PubMed] [Google Scholar]
- 15.Meurin P, Iliou MC, Ben Driss A, et al. Working Group of Cardiac Rehabilitation of the French Society of Cardiology Early exercise training after mitral valve repair: a multicentric prospective French study. Chest. 2005 Sep;128(3):1638–44. doi: 10.1378/chest.128.3.1638. [DOI] [PubMed] [Google Scholar]
- 16.Jairath N, Salerno T, Chapman J, Dornan J, Weisel R. The effect of moderate exercise training on oxygen uptake post-aortic/mitral valve surgery. J Cardiopulm Rehabil. 1995;15(6):424–30. doi: 10.1097/00008483-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Pardaens S, Moerman V, Willems AM, et al. Impact of the preoperative risk and the type of surgery on exercise capacity and training after valvular surgery. Am J Cardiol. 2014 Apr 15;113(8):1383–9. doi: 10.1016/j.amjcard.2014.01.413. [DOI] [PubMed] [Google Scholar]
- 18.Keteyian SJ, Brawner CA, Savage PD, et al. Peak aerobic capacity predicts prognosis in patients with coronary heart disease. Am Heart J. 2008;156(2):292–300. doi: 10.1016/j.ahj.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Kavanagh T, Mertens DJ, Hamm LF, et al. Peak oxygen intake and cardiac mortality in women referred for cardiac rehabilitation. J Am Coll Cardiol. 2003;42(12):2139–43. doi: 10.1016/j.jacc.2003.07.028. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh T, Mertens DJ, Hamm LF, et al. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation. 2002;106(6):666–71. doi: 10.1161/01.cir.0000024413.15949.ed. [DOI] [PubMed] [Google Scholar]
- 21.Vanhees L, Fagard R, Thijs L, Amery A. Prognostic value of training-induced change in peak exercise capacity in patients with myocardial infarcts and patients with coronary bypass surgery. Am J Cardiol. 1995;76(14):1014–9. doi: 10.1016/s0002-9149(99)80287-2. [DOI] [PubMed] [Google Scholar]
- 22.Goel K, Pack QR, Lahr B, et al. Cardiac rehabilitation is associated with reduced long-term mortality in patients undergoing combined heart valve and CABG surgery. Eur J Prev Cardiol. 2013 doi: 10.1177/2047487313512219. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Vergès B, Patois-Vergès B, Cohen M, et al. Effects of cardiac rehabilitation on exercise capacity in Type 2 diabetic patients with coronary artery disease. Diabet Med. 2004;21:889–895. doi: 10.1111/j.1464-5491.2004.01262.x. [DOI] [PubMed] [Google Scholar]
- 24.Habel-Verge C, Landry F, Desaulniers D, et al. Physical fitness improves after mitral valve replacement. CMAJ. 1987;136(2):142–7. [PMC free article] [PubMed] [Google Scholar]
- 25.Nakamura M, Chiba M, Ueshima K, et al. Effects of mitral and/or aortic valve replacement or repair on endothelium-dependent peripheral vasorelaxation and its relation to improvement in exercise capacity. Am J Cardiol. 1996 Jan 1;77(1):98–102. doi: 10.1016/s0002-9149(97)89146-1. [DOI] [PubMed] [Google Scholar]


