Abstract
Non-Hodgkin's lymphoma (NHL) represents 4% of newly diagnosed cancer in 2013 with a 59-82% 5-year survival depending on the tumor location. Primary presentation of lymphoma consists of lymphadenopathy or swelling of the lymph nodes and non-specific systemic symptoms such as fevers, night sweats, and weight loss. Less commonly, NHL arises from non-lymphoid tissue. We report a unique case of NHL arising from the ureteral wall which was visualized via non-contrast CT and direct vision through ureteroscopy.
Key Words: Ureteral lymphoma, Ureteral carcinoma
Introduction
Lymphoma involving the ureters is most commonly a result of direct extension or extrinsic compression from bulky retroperitoneal lymphadenopathy. Occasionally primary lymphoma of the bladder may extend in retrograde fashion to involve the distal ureters. However, primary extra nodal lymphoma of the ureter is exceedingly rare with less than 20 cases reported worldwide [1]. A majority of these reported cases describe encasement of the ureters by lymphomatous deposits or infiltrating tumor surrounding the ureter. We report a unique case of primary extra nodal lymphoma presenting as an intraluminal ureteral mass causing symptoms of acute obstructive uropathy.
Case Report
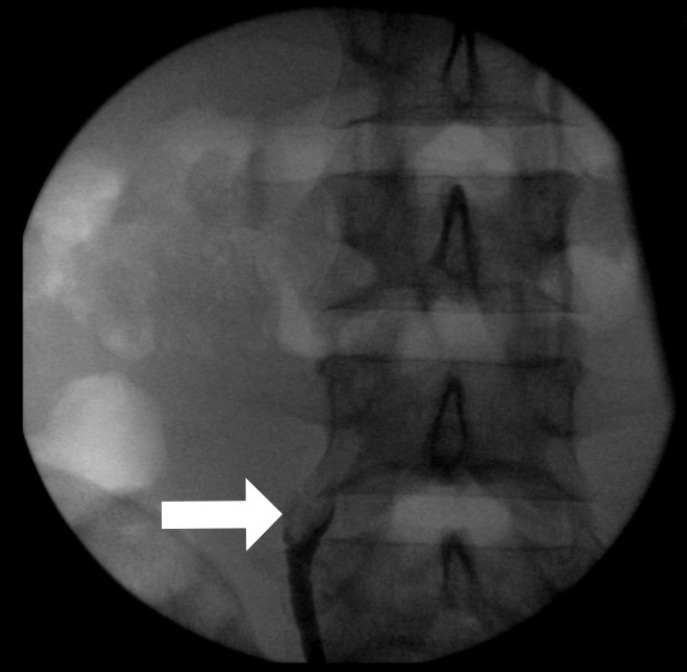
A 28-year-old male with a past medical history of sickle-cell trait and tobacco use, presented to the emergency room with nausea and sharp right-sided flank pain. Laboratory values revealed an elevated serum creatinine of 1.7 mg/ml. Urinalysis and all other laboratory values were unremarkable. Non contrast CT of the abdomen and pelvis revealed an enlarged right kidney with moderate hydroureteronephrosis and blunted calyces. The proximal right ureter was fluid filled and mildly dilated measuring 4 mm further dilating in its mid portion to 12 mm (fig. 1). At its widest portion the ureter was filled with an ill-defined soft-tissue density mass with peripheral punctuate calcification. The right ureter distal to this lesion was completely decompressed (fig. 2). No renal, ureteral or bladder calculi were present and no other pathologic abnormalities noted on CT scan.
Fig. 1.
CT pelvis with measured increase in diameter of the right ureter.
Fig. 2.
CT pelvis revealing the dilated ureter and soft tissue mass. Also of note are the small calcifications.
The patient subsequently underwent cystoscopy and diagnostic retrograde pyelogram. A right mid-ureteral obstruction was identified which prevented the passage of any contrast dye. The obstructing lesion was an irregular intraluminal filling defect demonstrating a “goblet” sign, consisting of focal dilatation of the ureter around and slightly below the mass (fig. 3). After failing to pass a standard 0.035 guidewire into the renal pelvis, ureteroscopy was performed which identified an obstructing mass in the right mid ureter (fig. 4). A guide wire was then passed into the kidney, and multiple biopsies of the mass were obtained. A retrograde pyelogram was completed and a 6-french ureteral stent was left in place to relieve the obstruction. The remainder of the ureter and renal collecting system were normal. Pathology at that time was positive for proliferation of large cells which stained positive for CD5 suggesting T-cell origin but inconclusive for a specific diagnosis.
Fig. 3.
Goblet sign. Retrograde pyelogram demonstrating filling defect in right mid-ureter.
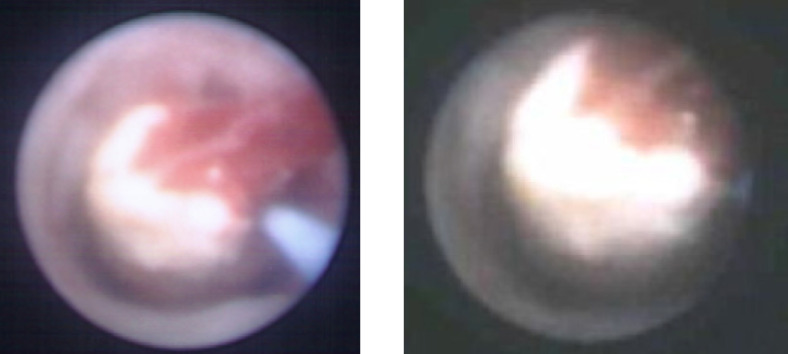
Fig. 4.
a Ureteroscopic image of the lymphoma; b Ureteroscopic image of the lymphoma.
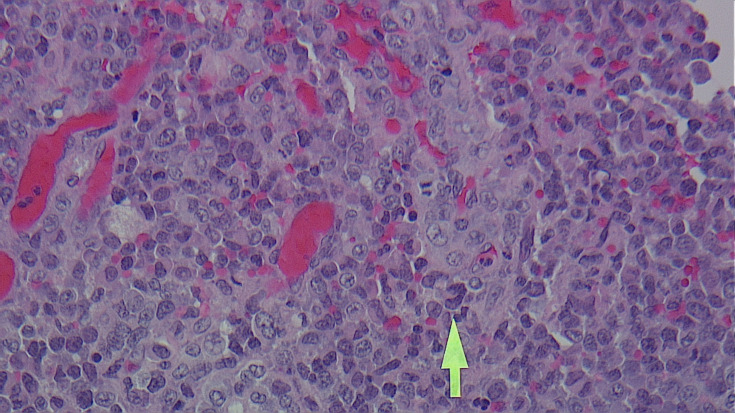
One month later, the patient underwent repeat ureteroscopy which again revealed a papillary, bulbous, avascular mass which was approximately 3 cm in length. Holmium laser excision was performed with careful sparing of the ureteral mucosa. Biopsy histology confirmed the mass to be ALK positive anaplastic large-cell lymphoma (fig. 5). PET/CT performed prior to treatment demonstrated the right ureteral mass to be mildly FDG avid with an SUV of 2. Two FDG avid lymph nodes, one 1.6 cm node in the right groin and one 0.9 cm node in the retroperitoneum, were identified and the patient was staged as IVa.
Fig. 5.
Histology identifies infiltrating T-lymphocyte lymphoma cells.
Discussion
The estimated incidence of any type of ureteral malignancy in 2013 is less than 0.1% of all cancers, with urothelial carcinoma by far the most common primary ureteral malignancy [2]. Metastatic disease to the ureter is relatively rare with the most common primary sites including: melanoma, breast, prostate, cervix and colon cancer and may be bilateral in up to 30% of cases [4]. Most metastases are discovered at autopsy. Non-Hodgkin lymphoma arising primarily from the ureteral wall is exceedingly uncommon, with fewer than 20 reported cases [1,3,5,6,7,8,9,10,11,12,13,14]. When lymphoma affects the ureters it is usually as indirect displacement by bulky retroperitoneal adenopathy [15]. Furthermore, anaplastic large-cell lymphoma is a less common variant comprising less than 15% of all cases of non-Hodgkin lymphoma in adults [16]. To our knowledge it has never been documented originating from the ureter.
Anaplastic large-cell lymphoma, most frequently presents with painless lymphadenopathy. On rare occasions, patients can present with symptoms secondary to tumor mass effect [17]. In the reported cases of ureteral lymphoma patients complain of either vague flank pain or abnormal renal function secondary to the indolent obstruction. In the majority of these reports hydronephrosis was caused by encasement of the ureter by lymphomatous deposits or diffuse infiltration of the ureteral wall. Because mucosal involvement is so rare, patients do not usually present with hematuria [3].
The unique features of this case include the presentation, imaging findings and unusual pathology. When lymphoma involves the ureters its source is either direct invasion or hematogenous spread to the adventitia. In our case at initial presentation the only site of lymphoma was an intra-luminal ureteral mass. The initial CT demonstrated the classic findings of an acute ureteral obstruction which, uncharacteristically in a young adult, was due to a mass rather than a calculus. The retrograde pyelogram demonstrated an intraluminal ureteral mass more typical of an urothelial malignancy. Lastly, the pathologic type of lymphoma was a less common variant of non-Hodgkin's lymphoma.
Conclusion
In summary, primary ureteral lymphoma of any variety is extremely rare. To our knowledge, this is the first reported case of anaplastic large-cell lymphoma arising primarily from the ureter in a patient presenting with acute obstructive uropathy.
References
- 1.Buck DS, Peterson MS, Borochovitz D, Bloom EJ. Non-Hodgkin lymphoma of the ureter: CT demonstration with pathologic correlation. Urol Radiol. 1992;14:183–187. doi: 10.1007/BF02926925. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 3.Numakura K, Tsuchiya N, Obara T, Tsuruta H, Saito M, Narita S, Inoue T, Horikawa Y, Satoh S, Habuchi T. A case of ureteral malignant lymphoma diagnosed by laparoscopic needle biopsy. Jpn J Clin Oncol. 2011;41:440–442. doi: 10.1093/jjco/hyq220. [DOI] [PubMed] [Google Scholar]
- 4.Marincek B, Scheidegger JR, Studer UE, Kraft R. Metastatic disease of the ureter: patterns of tumoral spread and radiologic findings. Abdom Imaging. 1993;18:88–94. doi: 10.1007/BF00201710. [DOI] [PubMed] [Google Scholar]
- 5.Chen HH, Panella JS, Rochester D, Ignatoff JM, McVary KT. Non-Hodgkin lymphoma of ureteral wall: CT findings. J Comput Assist Tomogr. 1988;12:157–158. doi: 10.1097/00004728-198801000-00034. [DOI] [PubMed] [Google Scholar]
- 6.Fujisawa H, Takagane H, Shimosegawa K, Sakuma T. Primary malignant lymphoma of the ureter: a case report. Hinyokika Kiyo. 2004;50:721–724. [PubMed] [Google Scholar]
- 7.Haitani T, Shimizu Y, Inoue T, Okubo K, Watanabe J, Kamba T, Yoshimura K, Kanematsu A, Nishiyama H, Ogawa O, Sumiyoshi S, Mikami Y, Nishikori M. A case of ureteral malignant lymphoma with concentric thickening of the ureteral wall. Hinyokika Kiyo. 2012;58:209–213. [PubMed] [Google Scholar]
- 8.Hashimoto H, Tsugawa M, Nasu Y, Tsushima T, Kumon H. Primary non-Hodgkin lymphoma of the ureter. BJU Int. 1999;83:148–149. doi: 10.1046/j.1464-410x.1999.00856.x. [DOI] [PubMed] [Google Scholar]
- 9.Kawashima A, Shiotsuka Y, Nin M, Kokado Y. Malignant lymphoma of the ureter: a case report. Hinyokika Kiyo. 2005;51:269–272. [PubMed] [Google Scholar]
- 10.Kubota Y, Kawai A, Tsuchiya T, Kozima K, Yokoi S, Deguchi T. Bilateral primary malignant lymphoma of the ureter. Int J Clin Oncol. 2007;12:482–484. doi: 10.1007/s10147-007-0685-7. [DOI] [PubMed] [Google Scholar]
- 11.Lebowitz JA, Rofsky NM, Weinreb JC, Friedmann P. Ureteral lymphoma: MRI demonstration. Abdom Imaging. 1995;20:173–175. doi: 10.1007/BF00201532. [DOI] [PubMed] [Google Scholar]
- 12.McMillin KI, Gross BH. CT demonstration of peripelvic and periureteral non-Hodgkin lymphoma. AJR Am J Roentgenol. 1985;144:945–946. doi: 10.2214/ajr.144.5.945. [DOI] [PubMed] [Google Scholar]
- 13.Ruth K, El-Amm J, Sotelo T, Aragon-Ching JB. Primary diffuse large B-cell lymphoma of the ureter in a patient with HIV: a case report and review of literature. Clin Lymphoma Myeloma Leuk. 2013;13:324–326. doi: 10.1016/j.clml.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Tozzini A, Bulleri A, Orsitto E, Morelli G, Pieri L. Hodgkin's lymphoma: an isolated case of involvement of the ureter. Eur Radiol. 1999;9:344–346. doi: 10.1007/s003300050677. [DOI] [PubMed] [Google Scholar]
- 15.Babaian RJ, Johnson DE, Ayala AG, Sie ET. Secondary tumors of ureter. Urology. 1979;14:341–343. doi: 10.1016/0090-4295(79)90075-x. [DOI] [PubMed] [Google Scholar]
- 16.Yoshii T, Horiguchi A, Shirotake S, Tobe M, Hayakawa M, Sumitomo M, Asano T. Spontaneous rupture of the ureter as the primary symptom of malignant lymphoma. Hinyokika Kiyo. 2010;56:639–643. [PubMed] [Google Scholar]
- 17.Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107:265–276. doi: 10.1182/blood-2005-06-2508. [DOI] [PMC free article] [PubMed] [Google Scholar]