Abstract
[Purpose] This study aimed to identify factors influencing the BMI classifications of 3,583 Korean adults using data from the fifth Korean National Health and Nutrition Examination Survey. [Subjects and Methods] Measures included lifestyle factors, physiologic factors, perceived health state, stress, subjective body recognition, health-related quality of life, and weight control behavior. [Results] Body perception scores were lower with underweight and higher with overweight and obesity than with a healthy weight. There was a lower proportion of underweight men and a higher proportion of overweight or obese men than women. Instances of Alcohol Use Identification Scores (AUDIT) ≥ 9 were proportionately lower with underweight and more with overweight or obesity relative to an AUDIT score < 9 with healthy weight. Hemoglobin A1c and systolic blood pressure were higher with obesity than with healthy weight. The total cholesterol level was greater with overweight and obesity than with healthy weight. [Conclusion] These results suggest that obesity intervention for adults should be based on age and sex and should include drinking habits and physical activity.
Key words: Adults, Body mass index, Obesity
INTRODUCTION
The worldwide prevalence of obesity has consistently increased since 1980, more than doubling in 2008 to 200 million obese men and 300 million obese women. In Korea, the prevalence of obesity in adults was 7.3%, which was higher than the 4.5% in Japan and 5.6% in China1). The proportion of obese adults in Korea increased rapidly from 26% in 1998 to 32% in 20122), and decreased energy, fat intake, and lack of physical activity were associated with the increased in obesity2). Obese adults have a reduced quality of life and physical activity, and they have an increased frequency of cholecystectomy caused by gallstones, fecal incontinence, hypertension, sphincter muscle disturbance, diabetes, lung disease, infertility, hyperlipidemia, cardiovascular disease, osteoarthritis, respiratory function, and asthma3,4,5,6,7,8,9, 19, 27). Adults who are underweight and those who are severely obese (body mass index [BMI] > 35) have increased mortality10, 18), thus obesity can be a life-threatening condition.
According to a health insurance policy survey by the Research Institute of the National Health Insurance Corporation, 23 types of diseases are related to obesity, and hypertension, chronic low back pain, osteoarthritis, diabetes, and stroke in Korea are representative of these disease. Total health care expenditures caused by overweight or obesity increased by 41.9% to Korean won 2.7 trillion in 2011 from 1.9 trillion in 2007, accounting for 5.8% of the total cost of health insurance in 201114). The treatment cost of all diseases associated with obesity has become the largest portion of costs, comprising 22.31% of the total medical cost in 201114). In addition, obesity, drinking, and smoking are responsible for increased medical costs, as well as obesity-related diseases such as diabetes, hypertension, hyperlipidemia, and coronary artery disease1, 12, 13). To solve the problem of obesity nationally, the United States, the United Kingdom, and France have proposed taxes upon carbonated beverages and junk food that contribute to obesity11).
In one study, subjects were divided into underweight, healthy weight, overweight, and obese groups according to BMI and were followed for 15 years. Subjects that stayed overweight or obese, or progressed to overweight or obese groups had reduced health-related quality of life compared to those maintaining a normal body weight14). Thus, obesity causes physical and mental health problems, a reduction in quality of life, both in Korea and abroad. Moreover, an increase in obesity causes personal and social economic loss. Thus, to maintain health status and quality of life, it is important to maintain normal body weight.
To clarify factors associated with BMI classification, data from the fifth triennial Korean National Health and Nutrition Examination Survey (KNHANES) from 201310) were analyzed to compare BMI classification with sociological characteristics, lifestyle factors, physiological variables, subjective health status, subjective stress, subjective body image, quality of life, and body weight regulation in adult subjects.
SUBJECTS AND METHODS
This was a descriptive study using secondary analysis to identify factors associated with BMI classifications of adults using raw data from the fifth KNHANES10).
The fifth triennial KNHANES10) was conducted from January 2012 to December 2012 and surveyed household members > 19 years old from 3,800 households in 192 survey districts throughout Korea. Data were obtained through “confirmation of plan for raw data use” from the Korean Centers for Disease Control and Prevention through the KNHANES website (http://knhanes.cdc.go.kr) with permission. KNHANES data includes Koreans residing in Korea, and excludes foreigners and those admitted to nursing homes, serving in the military, or incarcerated in prison. Sample designs, including sampling rates and plots, have been presented elsewhere10). This study meets the ethical principles of the Declaration of Helsinki (1975, revised 1983), and the Institutional Review Board of the Korean Centers for Disease Control and Prevention approved all procedures. Written informed consent was obtained from all subjects.
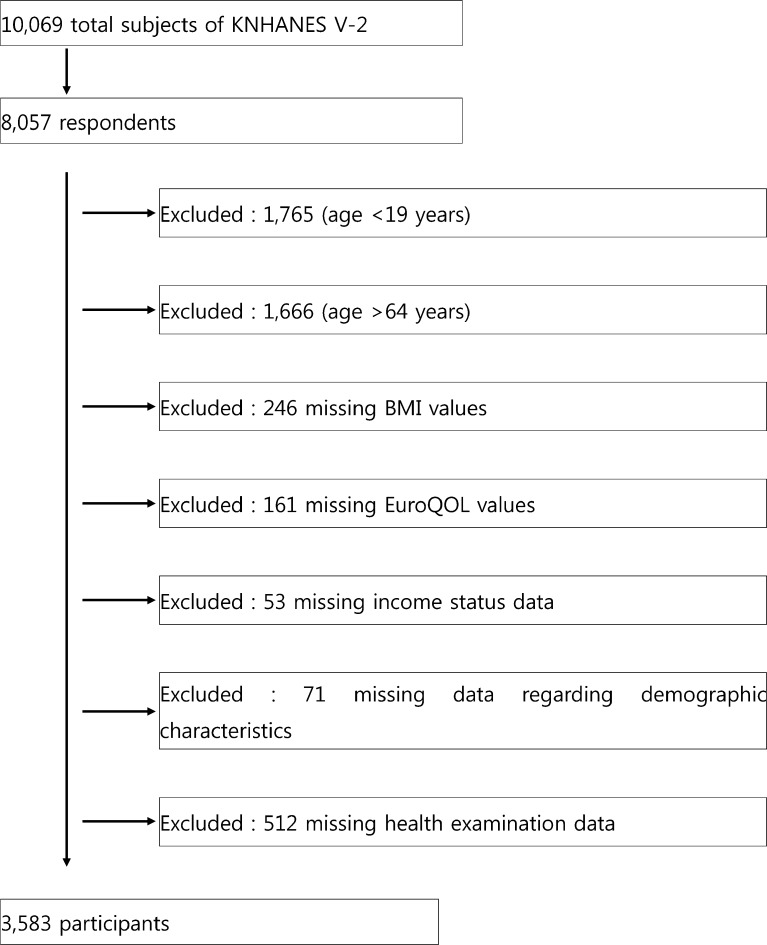
The KNHANES was completed by 7,645 individuals, a participation rate of 75.9%. Of these, 4,627 subjects were > 19 years of age and < 65 years of age. Of these, 1,044 subjects were excluded: 246 did not have a calculated BMI, 161 lacked a EuroQOL score, 53 did not have an income classification, and 583 were missing demographic characteristics and/or physiological variables. Thus, the final analysis included 3,583 subjects (Fig. 1).
Fig. 1.
Flow chart illustrating the selection process of participants included in the present study. KNHANES V-3: fifth Korean National Health and Nutrition Examination Survey; BMI: body mass index
BMI is calculated by dividing weight (kg) by the square of height (m)2. The guidelines presented by the World Health Organization of the Asia Pacific Region and the Korean Society for the Study of Obesity present the following definitions: underweight (< 18.5 kg/m2), healthy weight (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), and obese (≥25 kg/m2)12).
The following demographic characteristics of the subjects were collected: gender, age, marital status, education, household income, and employment status. Education status was classified as elementary or lower graduating from junior high school, high school, or college or higher. Household income was divided into quartiles and classified as low, middle-low, middle-high, and high. Employment status was classified as either yes or no.
Collected data on lifestyle factors included smoking, drinking, and physical activity. Smoking was classified as current smoker, former smoker, and never smoker. Drinking status was investigated using the Alcohol Use Disorder Identification Test (AUDIT)20), which consists of 10 questions related to alcohol consumption over the past year, including the amount and frequency of drinking, alcohol-related problems, and symptoms of alcoholism dependence. Each item is scored from 0–4 points, giving a total range of 0–40 points. An AUDIT score ≤ 8 points is normal, between 8–15 points indicates alcohol abuse, 16–19 points indicates alcohol abuse requiring continued observation, and ≥ 20 points indicates alcohol abuse requiring detailed examination20). However, in the present study, groups were divided into normal (< 9 points) and abnormal (≥ 9 points or more). Finally, physical activity was determined using the International Physical Activity Questionnaire, which calculates average physical activity into metabolic equivalent task (MET)-minute scores based on reported physical activity levels7). Physical activity was classified as low activity (does not display any activity or does not include other activity), moderate activity ([1] ≤ 600 MET-min/week of exercise for > 3 days with vigorous activity of ≥ 20 minutes for at least one day, or [2] physical activity of ≥ 600 MET-min/week for > 5 days in combination with ≥ 5 days of walking and moderate activity ≥ 30 minutes per day of walking or moderate or strenuous physical activity), or high activity ([1] physical activity ≥ 1,500 MET-min/week, [2] vigorous activity > 3 days per week, [3] complex physical activity such as walking > 7 days per week, or [4] moderate or vigorous activity with physical activity during work of ≥ 3,000 MET-min/week)7).
Physiological factors included systolic and diastolic blood pressure, fasting blood glucose, hemoglobin A1c, and total cholesterol. The normal range was ≤ 120/80 mm Hg or less for systolic/diastolic blood pressure, 70–110 mg/dL for fasting blood glucose, < 6.4% for hemoglobin A1c, and 0–240 mg/dL for total cholesterol.
Subjective health status was classified as very good (5 points), good (4 points), average (3 points), bad (2 points), and very bad (1 point); thus, a higher average score indicates a healthier state.
Subjects self-reported their stress in response to the question “How much stress do you feel in daily life?” Possible responses included very much (1 point), a lot (2 points), a little (3 points), and very rarely (4 points); thus, a higher score indicates low stress.
Subjects self-reported their subjective body perception in response to the question “What do you think of your current body image?” Possible responses included very thin (1 point), slightly thin (2 points), normal (3 points), slightly obese (4 points), and very obese (5 points); thus, a high score denotes a negative self-perception of body image.
To determine whether subjects had attempted weight control in past year, participants reported efforts to lose weight, efforts to maintain weight, efforts to gain weight, or absence of efforts to regulate body weight.
The EuroQol-5 dimension (EQ-5D) test developed by the Euro Quality of Life (EuroQol) Group21) was used to assess health-related quality of life. The EQ-5D is composed of five areas of mobility, self-care, usual activity, pain/discomfort, and anxiety/depression. Each area was reported as “no problem (1 point)”, “there is a problem (2 points)”, or “there is a serious problem (3 points)”; thus, higher scores indicate a lower quality of life17).
The EQ-5D index was calculated using the weighted model of Nam et al.17), and values were distributed between 1 point, indicating a condition of complete health and −1, indicating that living could not be worse than death.
The data collected were analyzed using SPSS/WIN 18.0 software. Factors studied in association with BMI classification are reported by frequency, percentage, mean, and standard deviation. The homogeneity of two populations was assayed using ANOVA and the χ2 test. To determine the odds ratio following the classification of BMI, multinomial logistic regression referenced to healthy weight (18.5–22.9 kg/m2) was performed, and the results are presented as 95% confidence intervals and odds ratios. A p-value < 0.05 was considered statistically significant.
RESULTS
Of the 3,950 subjects, 188 were classified as underweight, 1,590 as healthy weight, 913 as overweight, and 1,259 as obese.
Demographical, sociological, and physiological characteristics of the subjects are presented in Table 1. The subject’s mean age was 43.2 years, and the ratio of men to women was nearly equal.
Table 1. Comparison of the effects of various categorized demographic characteristics on body mass index (BMI) categories (n=3,583).
| Characteristics | n (%) and mean±SD | |||||
|---|---|---|---|---|---|---|
| Underweight (n=175) |
Healthy (n=1,448) |
Overweight (n=821) |
Obesity (n=1,139) |
Total (n=3,583) |
||
| Age (years)* | 33.9±11.8 | 41.1±12.3 | 46.3±11.9 | 45.1±11.6 | 43.2±12.4 | |
| Gender* | Male | 35 (20.0) | 524 (36.2) | 423 (51.5) | 608 (53.4) | 1,590 (44.4) |
| Female | 140 (80.0) | 924 (63.8) | 398 (48.5) | 531 (46.6) | 1,993 (55.6) | |
| Family income* | Low | 16 (9.1) | 98 (6.8) | 66 (8.0) | 96 (8.4) | 276 (7.7) |
| Middle-low | 38 (21.7) | 351 (24.2) | 197 (24.0) | 304 (26.7) | 890 (24.8) | |
| Middle-high | 49 (28.0) | 484 (33.4) | 222 (27.0) | 352 (30.9) | 1,107 (30.8) | |
| High | 72 (41.1) | 515 (35.6) | 336 (40.9) | 387 (34.0) | 1,310 (36.5) | |
| Education level* | Elementary level or lower | 7 (4.0) | 114 (7.9) | 127 (15.5) | 164 (14.4) | 412 (11.5) |
| Middle | 7 (4.0) | 101 (7.0) | 97 (11.8) | 115 (10.1) | 320 (8.9) | |
| High | 80 (45.7) | 608 (42.0) | 305 (37.1) | 476 (41.8) | 1,469 (41.0) | |
| College level or higher | 81 (46.3) | 625 (43.2) | 292 (35.6) | 384 (33.7) | 1,382 (38.6) | |
| Marital status* | Married | 93 (53.1) | 1,080 (74.6) | 709 (86.4) | 971 (85.3) | 2,853 (79.6) |
| Never married/separated/ divorced/widowed | 82 (46.9) | 368 (25.4) | 112 (13.6) | 168 (14.7) | 730 (20.4) | |
| Employee status* | Employed | 107 (61.1) | 936 (64.6) | 580 (70.6) | 832 (73.0) | 2,455 (68.5) |
| Unemployed | 68 (38.9) | 512 (35.4) | 241 (29.4) | 307 (27.0) | 1,128 (31.5) | |
| Smoking status* | Current smoker | 26 (16.6) | 313 (21.7) | 198 (23.1) | 315 (27.6) | 855 (23.8) |
| Former smoker | 19 (10.9) | 216 (14.9) | 199 (24.2) | 253 (22.2) | 687 (19.1) | |
| Never smoked | 127 (72.6) | 919 (63.5) | 424 (51.6) | 571 (50.1) | 2,041 (56.8) | |
| AUDIT* | <8 | 37 (21.1) | 372 (25.7) | 238 (29.0) | 398 (34.9) | 1,045 (29.2) |
| ≥8 | 138 (78.9) | 1,076 (74.3) | 583 (71.0) | 741 (65.1) | 2,538 (70.8) | |
| Weight control behavior in past year* | Effort to lose weight | 22 (12.6) | 462 (31.9) | 384 (46.8) | 735 (64.5) | 1,603 (44.7) |
| Effort to maintain weight | 31 (17.7) | 336 (23.2) | 188 (22.9) | 153 (13.4) | 708 (19.8) | |
| Effort to gain weight | 33 (18.9) | 112 (7.7) | 13 (1.6) | 4 (0.4) | 162 (4.5) | |
| No effort to control weight | 89 (50.9) | 538 (37.2) | 236 (28.7) | 247 (21.7) | 1,110 (31.0) | |
| Systolic blood pressure (mmHg)* | 107.3±13.8 | 112.2±14.0 | 117.0±15.3 | 121.3±15.3 | 116.0±15.3 | |
| Diastolic blood pressure (mmHg)* | 70.9±8.5 | 73.6±10.0 | 77.0±10.1 | 80.0±10.8 | 76.3±10.7 | |
| Fasting glucose level (mg/dL)* | 88.0±13.0 | 92.1±16.2 | 97.9±20.2 | 102.8±25.6 | 96.6±21.0 | |
| Hemoglobin A1c (%)* | 5.4±0.5 | 5.5±0.6 | 5.7±0.7 | 5.9±0.9 | 5.7±0.7 | |
| Total cholesterol (mg/dL)* | 170.0±30.5 | 183.6±33.7 | 193.4±34.2 | 195.9±38.4 | 189.1±35.9 | |
| EQ-5D index* | 0.97±0.05 | 0.97±0.07 | 0.96±0.08 | 0.96±0.09 | 0.96±0.08 | |
| Subjective health status* | 2.9±0.7 | 2.7±0.8 | 2.7±0.8 | 2.8±0.8 | 2.8±0.8 | |
| Subjective body perception* | 1.9±0.7 | 2.9±0.7 | 3.5±0.6 | 4.1±0.6 | 3.4±0.9 | |
| MET (MET-min/week)* | 1,196.0±509.8 | 1,180.9±557.5 | 1,097.0±604.0 | 1,125.7±557.3 | 1,144.9±567.2 | |
| Stress* | 2.7±0.7 | 2.8±0.6 | 2.8±0.7 | 2.8±0.7 | 2.8±0.7 | |
AUDIT: Alcohol Use Disorder Identification Test; MET: metabolic equivalent of task; SD: standard deviation, *p<0.05
Using the healthy weight group as the reference group, Table 2 presents the odds ratios (OR) with 95% confidence intervals of the logistic regression analysis regarding factors associated with BMI classifications of adults. All the differences reported below are made with reference to the healthy weight group, unless otherwise stated.
Table 2. Multinomial logistic regression for factors influencing the body mass index (BMI) categories.
| Estimated β | SE | Wald | OR | 95% CI | |
|---|---|---|---|---|---|
| Underweight | |||||
| Intercept | 9.95 | 2.670 | 13.87 | ||
| Age | −0.07 | 0.010 | 38.29 | 0.94 | 0.92–0.96 |
| Male | −2.29 | 0.280 | 65.25 | 0.10 | 0.06–0.18 |
| SHS | 0.24 | 0.140 | 2.79 | 1.27 | 0.96–1.68 |
| QOL | 1.77 | 1.820 | 0.949 | 5.84 | 0.17–206.74 |
| BP | −2.53 | 0.18 | 205.849 | 0.08 | 0.06–0.11 |
| AUDIT (≥8) | 0.05 | 0.26 | 0.039 | 1.05 | 0.63–1.76 |
| Stress | 0.01 | 0.22 | 0.009 | 1.01 | 0.65–1.56 |
| FBS | 0.01 | 0.01 | 0.319 | 1.01 | 0.98–1.03 |
| HbA1c | −0.60 | 0.32 | 3.34 | 0.55 | 0.29–1.04 |
| TC | −0.01 | 0.00 | 5.85 | 0.995 | 0.99–1.00 |
| Total MET | 0.00 | 0.00 | 0.02 | 1.00 | 1.00–1.00 |
| SBP | −0.01 | 0.01 | 0.56 | 0.99 | 0.97–1.02 |
| DBP | −0.00 | 0.02 | 0.08 | 1.00 | 0.97–1.03 |
| Overweight | |||||
| Intercept | −10.50 | 1.13 | 87.05 | ||
| Age | 0.04 | 0.01 | 62.75 | 1.04 | 1.03–1.05 |
| Male | 1.55 | 0.13 | 142.45 | 4.70 | 3.65–6.06 |
| SHS | −0.13 | 0.07 | 3.11 | 0.88 | 0.77–1.017 |
| QOL | −1.26 | 0.75 | 2.80 | 0.29 | 0.07–1.24 |
| BP | 1.91 | 0.10 | 405.40 | 6.73 | 5.59–8.10 |
| AUDIT (≥8) | −0.35 | 0.13 | 7.50 | 0.70 | 0.55–0.90 |
| Stress | −0.03 | 0.123 | 0.07 | 0.97 | 0.76–1.23 |
| FBS | 0.01 | 0.01 | 0.90 | 1.01 | 1.00–1.02 |
| HbA1c | 0.22 | 0.14 | 2.51 | 1.25 | 0.95–1.63 |
| TC | 0.00 | 0.00 | 7.34 | 1.00 | 1.00–1.0 |
| Total MET | 0.00 | 0.00 | 7.42 | 1.00 | 1.00–1.00 |
| SBP | 0.00 | 0.01 | 0.60 | 1.00 | 0.99–1.02 |
| DBP | 0.01 | 0.01 | 0.58 | 1.01 | 0.99–1.02 |
| Obesity | |||||
| Intercept | −21.46 | 1.34 | 257.25 | ||
| Age | 0.04 | 0.01 | 39.69 | 1.04 | 1.03–1.05 |
| Male | 2.22 | 0.15 | 213.41 | 9.25 | 6.86–12.46 |
| SHS | −0.12 | 0.08 | 2.19 | 0.88 | 0.75–1.04 |
| QOL | −1.27 | 0.87 | 2.14 | 0.28 | 0.05–1.54 |
| BP | 3.82 | 0.13 | 904.35 | 45.49 | 35.47–58.34 |
| AUDIT (≥8) | −0.31 | 0.15 | 4.35 | 0.74 | 0.55–0.98 |
| Stress | 0.09 | 0.14 | 0.43 | 1.10 | 0.83–1.45 |
| FBS | 0.01 | 0.01 | 1.38 | 1.01 | 1.00–1.02 |
| HbA1c | 0.40 | 0.16 | 6.45 | 1.49 | 1.10–2.04 |
| TC | 0.01 | 0.00 | 7.73 | 1.01 | 1.00–1.01 |
| Total MET | 0.00 | 0.00 | 4.32 | 1.00 | 1.00–1.00 |
| SBP | 0.02 | 0.01 | 12.40 | 1.02 | 1.01–1.03 |
| DBP | 0.01 | 0.01 | 1.08 | 1.01 | 0.99–1.03 |
SHS: subjective health status; QOL: quality of life; BP: body perception; AUDIT: Alcohol Use Disorder Identification Test; FBS: fasting blood sugar; HbA1c: glycated hemoglobin; TC: total cholesterol; MET: metabolic equivalent of task; SBP: systolic blood pressure; DBP: diastolic blood pressure; CI: confidence intervals; OR: odds ratio; SE: standard error
As age increased, underweight (OR = 0.94, p < 0.001) decreased and overweight (OR = 1.04, p < 0.001) and obesity (OR = 1.04, p < 0.001) increased. In men, underweight (OR = 0.10, p < 0.001) was 0.10-fold lower, but overweight (OR = 4.07, p < 0.001) and obesity (OR = 9.25, p < 0.001) were lower. Health-related quality of life and subjective health status were not significantly different. As subjective body perception increased, underweight (OR = 0.08, p < 0.001) decreased, and overweight (OR = 6.73, p < 0.001) and obesity (OR = 45.49, p < 0.001) increased. An AUDIT score < 9 was associated with decreased overweight (OR = 0.70, p < 0.001) and obesity (OR = 0.74, p < 0.001) relative to an AUDIT score ≥ 9.
Fasting glucose and stress were not significantly different. Glycated hemoglobin was significantly higher with obesity (OR = 6.45, p < 0.001). As total cholesterol level increased, underweight (OR = 0.99, p < 0.001) decreased, and overweight (OR = 7.34, p < 0.001) and obesity (OR=7.73, p < 0.001) increased. As total physical activity increased, overweight (OR = 1.00, p < 0.001) and obesity (OR = 1.00, p < 0.001) increased. Systolic blood pressure was higher with obesity (OR = 1.02, p < 0.001).
DISCUSSION
The present study identified factors associated with BMI classifications of Korean adults based on data from the fifth triennial KNHANES10).
The obesity group comprised 46.6% women, and men had a higher prevalence of obesity than women. This is consistent with previous findings1). Although the World Health Organization study also included those aged over 65 years; the lower obesity rate of women may be related to their longer lifespan.
There were proportionately fewer men than women in the underweight and healthy weight groups, and there were proportionately more men in the overweight and obesity groups. This result is similar to a previous finding of showing increased underweight or severe obesity and decreased overweight and obesity in women, and increased underweight, obesity, and severe obesity and decreased overweight in men15, 23). Only men in the overweight group had proportionately a higher than women.
One factor underlying the greater obesity rate of Korean men may be alcohol consumption. Among 185 countries, Korea is ranked 20th for alcohol consumption. Drinking or alcohol consumption is closely related to obesity, and men drink more than women1, 14, 18, 24, 25).
As age increased, there was a reduction in the proportion of underweight and increases the proportions of overweight and obese subjects. This is in contrast with a previous study which reported that the proportion of extreme obesity between 25 to 59 years increased relative to healthy weight, while the proportions of underweight, overweight, and obesity decreased. In that study, those > 60 years of age showed increases in underweight and severe obesity compared to healthy weight, whereas the obesity and overweight groups showed relative declines11). It has been suggested that the number of obese people has increased due to the Westernization of the Korean diet14, 16).
Health-related quality of life and subjective health status were higher in the healthy weight and underweight groups compared to the overweight and obesity groups. This result is similar to those reported in other studies11, 22). Compared to the healthy weight group, the underweight group perceived themselves as thin, whereas the obese and overweight groups perceived themselves as obese. This result supports the findings of a previous study26). State of subjective body perception and those attempting to reduce or maintain weight were highest in the obesity group, followed by the overweight, healthy weight, and underweight groups. There were proportionately fewer employed subjects in the underweight group than in the healthy weight group, and more in the overweight and obese groups. These results are consistent with those of a previous study which reported that obesity prevalence increases with exposure to an occupational environment, and especially among those who work > 40 hours/week, and those who sit for a longer time1). These results suggest that workers tend to have a more sedentary lifestyle. Thus, programs targeting normal body weight will need to include measurable to tackle, programs including a reduction in sedentary lifestyles and encourage smoking cessation.
It was previously reported that lifetime non-smokers were more underweight than healthy weight, overweight, or obese subjects22). The degree of physical activity in all groups was moderate, but that of the healthy weight group was lower than those of the underweight group, and higher than those of the overweight and obesity groups. In addition, physical activity in the overweight and obesity groups was lower than that of the healthy weight group. This is consistent with the reduction in physical activity observed in obese individuals5). Moreover, stress was higher in the healthy weight group than in the underweight group, but similar in the overweight and obesity groups. These results agree with previous findings suggesting that obesity is related to physical activity and not to mental health5). In terms of alcohol consumption, the overweight and obese groups had higher proportion of subjects with an AUDIT score ≥ 9, a result in agreement with a prior study reporting that visceral obesity, whole body obesity, and abdominal obesity increased based on drinking habits25).
In addition, the obese group showed higher age, systolic blood pressure/diastolic blood pressure, fasting blood glucose, and total cholesterol level. These results agree with reports that obese groups have higher blood lipids, blood pressure, and fasting blood glucose, and that those who scored well in self-perception about obesity made greater efforts to improve their lifestyle11). Glycated hemoglobin, systolic blood pressure, and total cholesterol levels in the overweight and obesity groups were significantly higher than in the healthy weight group. This corroborates evidence reporting that obesity is significantly associated with hypertension, diabetes and hyperlipidemia3, 8).
In conclusion, the present study showed that as age increases, men rather than women showed a tendency to overweight or obesity. Other factors associated with obesity included subjects with an AUDIT score ≥ 9, indicating an abnormal drinking state, decreased physical activity, and increased glycated hemoglobin, total cholesterol, and systolic blood pressure. These results suggest that weight management programs should include counseling regarding smoking cessation, drinking habits, and physical activity in the workplace. In addition, weight management programs may help to prevent primary disease such as diabetes, hypertension, hyperlipidemia, and secondary diseases such as stroke and cardiovascular disease. Moreover, they may also help to reduce medical costs both nationally and individually, and increase subjective quality of life11).
One shortcoming of this study is that there were missing values in the KNHANES10) data. However, this does not detract from the above findings showing the associations of various factors with BMI classifications of Korean adults.
REFERENCES
- 1.Apovian CM: The clinical and economic consequences of obesity. Am J Manag Care, 2013, 19: s219–s228. [PubMed] [Google Scholar]
- 2.de Hollander EL, Picavet HS, Milder IE, et al. : The impact of long-term body mass index patterns on health-related quality of life: the Doetinchem Cohort Study. Am J Epidemiol, 2013, 178: 804–812. [DOI] [PubMed] [Google Scholar]
- 3.Ellington DR, Polin MR, Szychowski JM, et al. : The effect of obesity on fecal incontinence symptom distress, quality of life, and diagnostic testing measures in women. Int Urogynecol J Pelvic Floor Dysfunct, 2013, 24: 1733–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farooq R, Lutfullah S, Ahmed M: Serum leptin levels in obese infertile men and women. Pak J Pharm Sci, 2014, 27: 67–71. [PubMed] [Google Scholar]
- 5.Ha YJ, Park H: Association between obesity and self-rated health in Korean males and females. J Korean Biol Nurs Sci, 2012, 14: 203–211. [Google Scholar]
- 6.Lee HC, Heo T: Effects of exercise therapy on blood lipids of obese women. J Phys Ther Sci, 2014, 26: 1675–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.IPAQ Research Committee: Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) − Short and Long Forms. Revised Nov 2005. http://www.ipaq.ki.se/scoring.htm.
- 8.Jepsen R, Aadland E, Andersen JR, et al. : Associations between physical activity and quality of life outcomes in adults with severe obesity: a cross-sectional study prior to the beginning of a lifestyle intervention. Health Qual Life Outcomes, 2013, 11: 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ito K, Kimura Y, Tajika A, et al. : Ultrasonographic changes of the knee joint cartilage associated with physical characterization in middle-aged women: 6-month observational survey. J Phys Ther Sci, 2007, 19: 277–282. [Google Scholar]
- 10.Korea Center for Disease Control and Prevention, Ministry of Health and Welfare: The Fifth Korea National Health and Nutrition Examination Survey (KNHANES V-3) 2013. Korea Centers for Disease Control and Prevention (Issue Brief No 11702). Seoul, Korea. [Google Scholar]
- 11.Korea Center for Disease Control and Prevention, Ministry of Health and Welfare: The fifth national health and nutrition examination survey statistics. http://knhanes.cdc.go.kr (Accessed Nov. 1, 2013)
- 12.Korean Society for the Study of Obesity: Obesity diagnostic criteria. Seoul, 2007. http://www.kosso.or.kr/.
- 13.Lee KS, Hwang IC, Kim SS, et al. : Perception of obesity and its related factors. J Korean Soc Study Obes, 2008, 18: 116–122. [Google Scholar]
- 14.Lee SM, Yeon YD, Hyun KR, et al. A study of a charge system of health related risk factor for health security financing resource. National Health Insurance Corporation, Health Insurance Policy Institute. no. 2012–08, 2012.
- 15.Luckhaupt SE, Cohen MA, Li J, et al. : Prevalence of obesity among U.S. workers and associations with occupational factors. Am J Prev Med, 2014, 46: 237–248. [DOI] [PubMed] [Google Scholar]
- 16.Mathus-Vliegen EM: Obesity and the elderly. J Clin Gastroenterol, 2012, 46: 533–544. [DOI] [PubMed] [Google Scholar]
- 17.Nam HS, Kim KY, Kwon SS, et al. : EQ-5D Korean valuation study using time trade of method. Seoul: Korea Centers for Disease Control and Prevention, 2007. [Google Scholar]
- 18.Orpana HM, Berthelot JM, Kaplan MS, et al. : BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring), 2010, 18: 214–218. [DOI] [PubMed] [Google Scholar]
- 19.Schatz M, Zeiger RS, Zhang F, et al. : Overweight/obesity and risk of seasonal asthma exacerbations. J Allergy Clin Immunol Pract, 2013, 1: 618–622. [DOI] [PubMed] [Google Scholar]
- 20.Saunders JB, Aasland OG, Babor TF, et al. : Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction, 1993, 88: 791–804. [DOI] [PubMed] [Google Scholar]
- 21.EuroQol Group: EuroQol—a new facility for the measurement of health-related quality of life. Health Policy, 1990, 16: 199–208. [DOI] [PubMed] [Google Scholar]
- 22.Vals K, Kiivet RA, Leinsalu M: Alcohol consumption, smoking and overweight as a burden for health care services utilization: a cross-sectional study in Estonia. BMC Public Health, 2013, 13: 772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization: World Health statistics 2013. NLM classification: WA 900.1. [Google Scholar]
- 24.World Health Organization: WHO global status report on alcohol. 2004. http://www.who.int/substance_abuse /publications/global_status_report_2004_overview.pdf (Accessed Dec. 10, 2011)
- 25.Kim DH: Relation of body mass index, waist and visceral fat area with alcohol consumption habits in Korea. Unpublished doctoral dissertation, Seoul: Korea University, 2007.
- 26.Poveda A, Ibáñez ME, Rebato E: Obesity and body size perceptions in a Spanish Roma population. Ann Hum Biol, 2014, 41: 428–435. [DOI] [PubMed] [Google Scholar]
- 27.Kim YM, Han JT, So Hyun P, et al. : The physical factors affecting on FVC, ERV, and MVV of Korean adults in their 20s. J Phys Ther Sci, 2013, 25: 367–369. [Google Scholar]