Abstract
Surgical approaches to the condylar fracture include intraoral, preauricular, submandibular, and retromandibular approaches. Each approach has its own advantages and disadvantages. When a patient needs esthetic results and an intraoral approach is not feasible, the transmasseteric antero-parotid facelift approach is considered. This approach permits direct exposure and allow the surgeon to fixate the fractured unit tangentially. Tangential fixation is critical to osteosynthesis. Disadvantages of the transmasseteric antero-parotid facelift approach include damage to the facial nerve and a longer operation time. However, after the initial learning curve, facial nerve damage can be avoided and operation time may decrease. We report three cases of subcondylar fractures that were treated with a transmasseteric antero-parotid facelift approach. Among these, two cases had trivial complications that were easily overcome. Instead of dissecting through the parotid gland parenchyma, the transmasseteric antero-parotid facelift approach uses transmasseteric dissection and reduces facial nerve damage more than the retromandibular transparotid approach. The esthetic result is superior to that of other approaches.
Keywords: Transmasseteric antero-parotid facelift approach, Condylar fracture
I. Introduction
The surgical procedures follow the sequences.
1. Markings and incision
The line connecting the mandibular angle to 2 cm lateral to the malar eminence area, the inferior anterior border of the parotid gland, and the superficial musculoaponeurotic system (SMAS) layer will be incised to search for the anterior edge of the parotid gland. The line connecting the tip of the mastoid process to the corner of the mouth represents the course of the buccal branch of the nerve.
A standard face-lift incision was used. In women, the face-lift incision is modified by an endaural extension, and the postauricular incision must be positioned anterior to the auricular crease by 2 to 3 mm. For men, the post auricular incision can be positioned at the auricular crease and does not need to be positioned anteriorly.
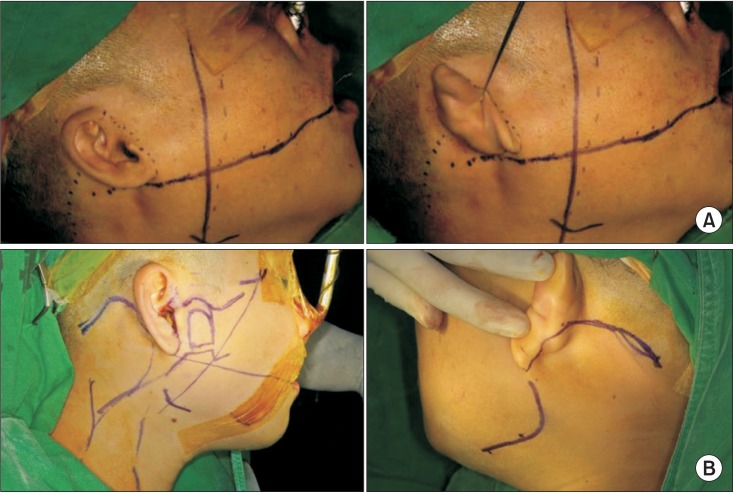
The preauricular incision follows the curve of the root of the helical crus and then continues posteriorly to the tragus. The incision then enters the hairline or runs parallel to the hair line for approximately 5 to 6 cm in a posterior-inferior direction at the level of external auditory canal and extends further1.(Fig. 1)
Fig. 1. A. Outline of a rhytidectomy incision incorporating a preauricular incision in men. The incision extends into the posterior auricular crease, and runs parallel to the hair line for approximately 5 to 6 cm in a posteroinferior direction. B. In women, an endaural incision must be used. The post-auricular incision must be positioned anterior to the auricular crease. Usually, the incision line is anterior to the crease by 2 to 3 mm.
2. Skin dissection and exposure of the anterior edge of the parotid gland
The skin flap is raised forward at the cutaneous level to expose the anterior edge of the parotid gland. When the postauricular skin flap is raised, sharp dissection with a scalpel is feasible. Subcutaneous dissection of the preauricular area is initiated with the scalpel, and a skin hook retractor is used for the first 1 to 2 cm because the deep tissue in this region is more adherent to the overlying skin than the skin further forward over the cheek. Once the proper plane of dissection is identified, subsequent elevation of the preauricular facial skin flap is performed with face-lift scissors or Metzenbaum scissors under direct vision after the first 1 to 2 cm1. The line from the mandibular angle to 2 cm lateral to the malar eminence area helps to infer the location of the anterior edge of the parotid gland. During skin flap elevation, the greater auricular nerve can be found below the ear lobe and must be preserved. The parotid gland is covered with the SMAS layer above and the parotidomasseteric fascia below.(Fig. 2)
Fig. 2. The skin flap is elevated to expose the anterior edge of the parotid gland.
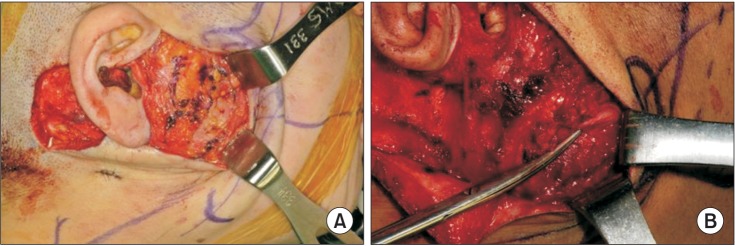
3. Incision of the SMAS layer and finding branches of the facial nerve
After the anterior edge of the parotid gland is defined, an incision is made in the SMAS from the line of the mandibular angle to 2 cm lateral to the malar eminence area. This exposes the branch of the facial nerve that emerges from the anterior border of the parotid gland. A location between the buccal and marginal branches is used to treat lower subcondylar fractures, while a location between the temporal and zygomatic branches is used to treat high condylar fractures. (Fig. 3)
Fig. 3. A. Incision of the subcutaneous musculoaponeurotic system on the anterior edge of the parotid gland exposes the emerging facial nerve. B. The tip of the scissors indicates the buccal branch of the facial nerve.
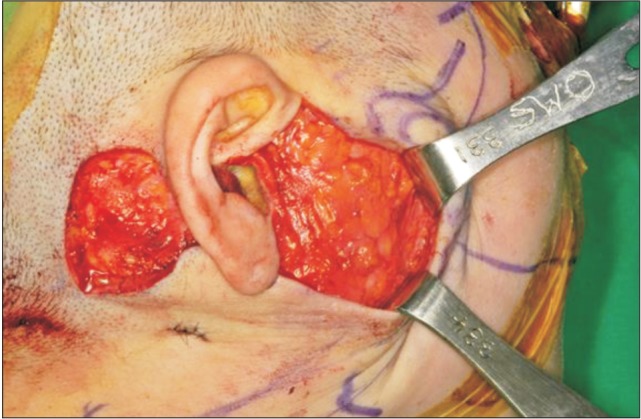
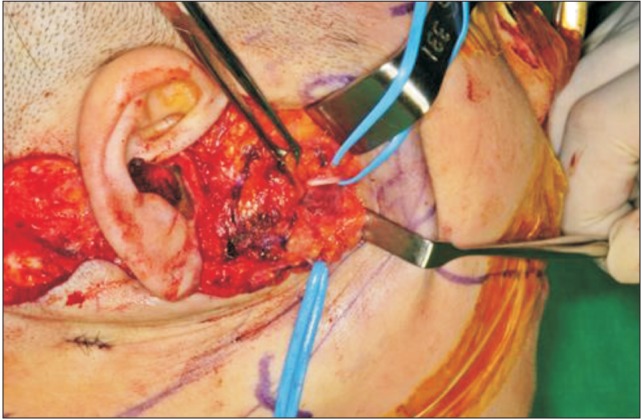
4. Retraction of parotid gland and facial nerve and exposing the masseter muscle
The parotid parenchyma is retracted posteriorly, and retraction of facial nerve branches away from the surgical field exposes the masseter muscle below. The field is now prepared for incision of the masseter muscle and its fascia.(Fig. 4)
Fig. 4. Retraction of the parotid gland exposes the underlying masseter muscle, and branches of facial nerve are retracted away from the surgical field with the aid of vessel loops. The vessel loops retracted the upper and lower buccal branches.
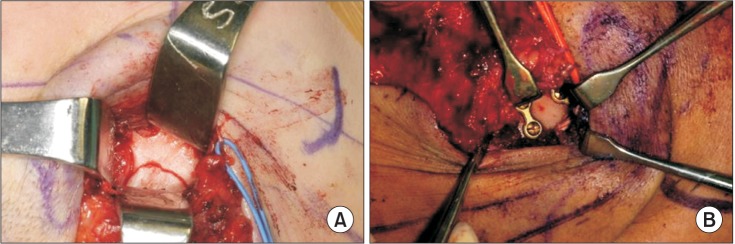
5. Exposure of fractured site and plate fixation
The muscle fibers of the masseter muscle are oriented obliquely, and if the muscle over the facture site is incised obliquely, the fractured site will be exposed. Using a small retractor, the fractured site is exposed effectively and direct miniplate fixation is possible. Generally, two miniplates are used in condylar fractures. Occlusion is checked after fixation.(Fig. 5)
Fig. 5. A. The muscle fibers of the masseter muscle are incised obliquely to expose the fractured site. B. Miniplate fixation was performed after reduction of the fractured site.
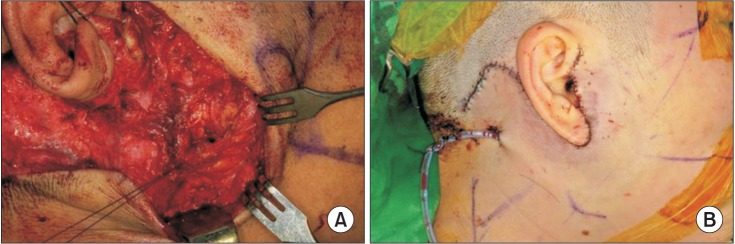
6. Closure
The SMAS layer must be closed to prevent salivary fistulae. The skin flap is closed in two layers; subdermal sutures and skin sutures are needed (Fig. 6), and a proper suction drain must be inserted. Usually, the suction drain is removed 5 to 6 days after the surgery.
Fig. 6. A. The subcutaneous musculoaponeurotic system layer is closed with 4-0 vicryl. B. The skin flap is closed in two layers; the subdermal layer is closed with 4-0 vicryl and the skin is closed with 5-0 and 6-0 nylon.
II. Cases Report
All patients were explained for the use of clinical images on this article and informed consent was gained.
1. Case 1
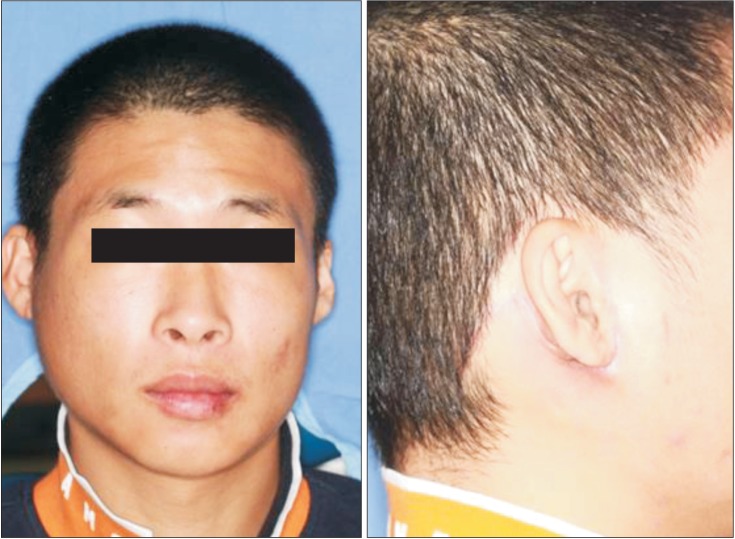
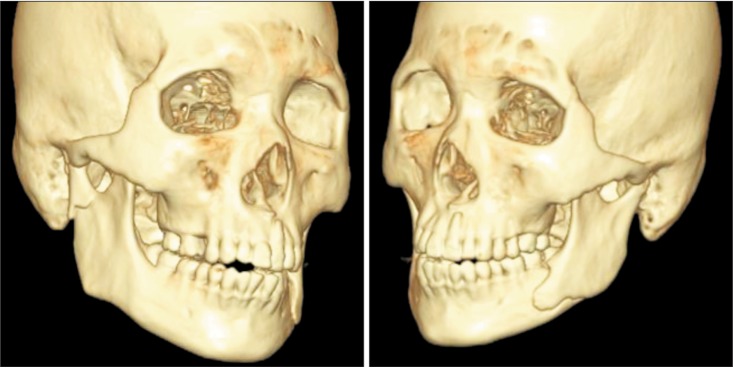
A 31-year-old male patient visited the emergency room due to facial swelling and malocclusion after he fell down the stairs. He had a right condylar and left mandible angle fracture.(Fig. 7) According to Lindahl's classification, this was a level IV condylar fracture2.
Fig. 7. The patient had a level IV condylar fracture on the right side and a mandibular angle fracture on the left side.
Our surgical teams thought that an intraoral approach was unlikely to produce good results, because the fracture line was oblique and therefore difficult to reduce. Therefore, we recommend an extraoral approach including a Risdon incision, retromandibular incision, and submandibular incision. However, the patient did not want a scar line, so the surgical team performed a face-lifting approach to reduce the fracture and fixate the condyle. Total surgical time was 3.5 hours. The mandibular angle fracture was managed intraorally. There was no facial nerve weakness and the patient achieved good occlusion and mouth opening.(Fig. 8)
Fig. 8. Postoperative X-ray.
After several weeks, facial scar line was inconspicuous on profile and frontal views.(Fig. 9)
Fig. 9. Good esthetic results were achieved. The facial scar line was inconspicuous on profile and frontal views.
2. Case 2
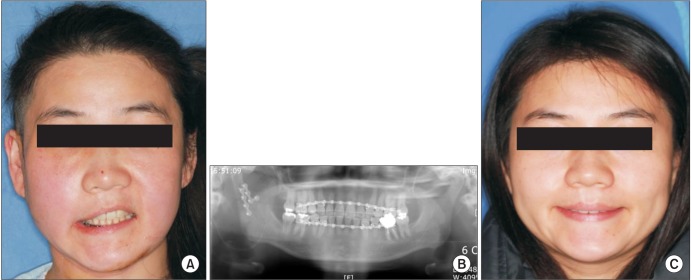
A 30-year-old female patient visited the emergency room due to limited mouth opening after a fall. She had a right level IV subcondylar fracture.
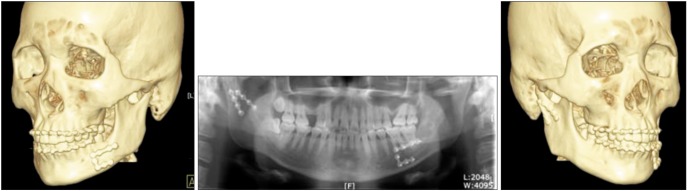
She wanted no visible scar, so the same surgical procedure was performed. Total operation time was 4 hours. However, the upper branch of the facial nerve was damaged and she showed a weak upper lip. This might be due to a severe retraction of the facial nerve during the operation, but the esthetic result was superior. Three months after the operation, nerve function had almost recovered.(Fig. 10)
Fig. 10. A. After the operation, paralysis of the upper lip occurred, possibly due to severe retraction of the facial nerve. B. Postoperative panoramic view. C. Nerve function recovered after three months.
3. Case 3
A 32-year-old female visited the emergency room after falling down stairs. She had a symphysis and left level IV condylar fracture. After the operation, she experienced lower lip palsy, but recovered from the facial nerve damage 5 months later. Total operation time was 4 hours.
III. Discussion
Surgical approaches to the condylar area include intraoral, preauricular, submandibular, and retromandibular approaches. Each approach has its own advantages and disadvantages.
The intraoral approach leaves no scars, but it is difficult to perform and sometimes produces suboptimal results. The extraoral approach exposes a wide surgical field which allows direct reduction and fixation of the fractured unit. However, facial nerve damage and visible scarring may follow.
The intraoral approach is not feasible when treating high condylar fractures, especially level I or II fractures. The intraoral approach with some endoscopically assisted modifications may offer better cosmetic results than the extraoral approach. However, the intraoral approach requires special instruments and endoscopic training. In addition, it is often difficult to reduce and fixate the fractured segment3,4.
When treating high condylar fractures, a preauricular approach is indicated, but it provides an unsatisfactory view in other cases, especially lower fractures5. However, if the skin heals well, the scar may be inconspicuous.
Submandibular modification approaches are preferred for fractures of the lower condylar neck and ramus6. Wide exposure of the high condylar area needs aggressive retraction, which damages the marginal branch of the facial nerve, and sometimes it is difficult to tighten the screw tangentially. Widmark et al.7 reported that the incidence of facial nerve injury after submandibular incision was 5.3% to 48.1%.
Retromandibular modification approaches provide direct exposure to the condylar unit, but require dissection through the parotid parenchyma, so facial nerve injury and salivary fistulae may readily occur, and it may leave visible scars8. Ellis et al.9 reported that the incidence of facial nerve injury during retromandibular access using this method was 6% to 10.5%. For patients who do not want visible scars and surgeons who require a direct approach to the fractured site, the face-lifting approach (rhytidectomy approach) may be a solution.
Traditionally, rhytidectomy approaches used the same technique as the retromandibular approach, which means that dissection of the parotid gland is required. The transmasseteric-anteroparotid approach in this article uses a rhytidectomy incision. However, instead of dissecting the parotid gland, the parotid gland is retracted posteriorly to expose the masseter muscle, and the muscle fiber is incised obliquely to directly expose the lower and high condylar areas. These provide direct access to fracture sites for direct plating and screw fixation, with excellent exposure and the ability to distract the mandibular ramus because of access to the gonial angle. This incision also provides the best access to the ramus and condylar areas, and it leaves an invisible scar after healing. However, there can be potential damage to the facial nerve through excess retraction or direct nerve damage. In addition, this surgery requires a longer operation time then retromandibular and submandibular approaches because it requires tedious skin and facial nerve dissection. However, if the SMAS layer anterior to the edge of the parotid gland is incised, nerve findings with a nerve stimulator will reduce the possibility of nerve damage.
Surgical approaches depend on the location of the fracture site in the rhytidectomy-transmasseteric antero-parotid facelift approach for open reduction and internal fixation of condylar fractures. In condylar head fractures, the fractured end can be exposed by stripping the masseter between the temporal and zygomatic branches of the facial nerve. In condylar neck and subcondylar fractures, this area can be exposed by stripping the masseter between the upper and lower branches of the facial nerve. In mandibular ramus and coronoid process fractures, the fracture line can be exposed by stripping the masseter between the buccal branch of the facial nerve and the marginal mandibular branch. At the same time, this method is not only suitable for the surgical treatment of condylar fractures but also for fractures of the mandibular ramus and coronoid process8. Due to direct exposure of the fractured unit, tangential screw fixation is possible, which is a prerequisite for optimal osteosynthesis.
We reviewed three cases of lower subcondylar fracture. The preauricular approach did not allow reduction of the fracture segment due to its lower position, and all patients wanted invisible scars. Two of three patients experienced facial palsy, and there were other complications such as Frey's syndrome. We suspect that the facial palsy was brought on because the branches of facial nerve were retracted severely during the operation. All patients recovered from facial palsy several months later. In future operations, we must retract the branches carefully with a smaller retractor. Total operation time was around 4 hours. Comparing to other techniques, this approach requires more time, but leaves no visible scars.
If the facial nerve is protected and surgical skill is acquired, a transmasseteric antero-parotid approach using a face-lift incision is a good substitute for condylar fractures when the patients don't want visible scars and intraoral and endoscopic assisted approaches are not feasible.
Footnotes
This paper was supported by Wonkwang University in 2015.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Divaris M, Blugerman G, Paul MD. Face expressive lifting (FEL): an original surgical concept combined with bipolar radiofrequency. Eur J Plast Surg. 2014;37:69–76. doi: 10.1007/s00238-013-0908-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindahl L. Condylar fractures of the mandible. I. Classification and relation to age, occlusion, and concomitant injuries of teeth and teeth-supporting structures, and fractures of the mandibular body. Int J Oral Surg. 1977;6:12–21. doi: 10.1016/s0300-9785(77)80067-7. [DOI] [PubMed] [Google Scholar]
- 3.Lee C, Mueller RV, Lee K, Mathes SJ. Endoscopic subcondylar fracture repair: functional, aesthetic, and radiographic outcomes. Plast Reconstr Surg. 1998;102:1434–1443. discussion 1444-5. doi: 10.1097/00006534-199810000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Loukota RA. Endoscopically assisted reduction and fixation of condylar neck/base fractures--The learning curve. Br J Oral Maxillofac Surg. 2006;44:480–481. doi: 10.1016/j.bjoms.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Salgarelli AC, Anesi A, Bellini P, Pollastri G, Tanza D, Barberini S, et al. How to improve retromandibular transmasseteric anteroparotid approach for mandibular condylar fractures: our clinical experience. Int J Oral Maxillofac Surg. 2013;42:464–469. doi: 10.1016/j.ijom.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Manisali M, Amin M, Aghabeigi B, Newman L. Retromandibular approach to the mandibular condyle: a clinical and cadaveric study. Int J Oral Maxillofac Surg. 2003;32:253–256. doi: 10.1054/ijom.2002.0270. [DOI] [PubMed] [Google Scholar]
- 7.Widmark G, Bågenholm T, Kahnberg KE, Lindahl L. Open reduction of subcondylar fractures. A study of functional rehabilitation. Int J Oral Maxillofac Surg. 1996;25:107–111. doi: 10.1016/s0901-5027(96)80052-x. [DOI] [PubMed] [Google Scholar]
- 8.Tang W, Gao C, Long J, Lin Y, Wang H, Liu L, et al. Application of modified retromandibular approach indirectly from the anterior edge of the parotid gland in the surgical treatment of condylar fracture. J Oral Maxillofac Surg. 2009;67:552–558. doi: 10.1016/j.joms.2008.06.066. [DOI] [PubMed] [Google Scholar]
- 9.Ellis E, 3rd, McFadden D, Simon P, Throckmorton G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58:950–958. doi: 10.1053/joms.2000.8734. [DOI] [PubMed] [Google Scholar]