Abstract
Purpose :
The PainVision™ system was recently developed for quantitative pain assessment. Here, we used this system to evaluate the effect of plexus brachialis block on postoperative pain after arthroscopic rotator cuff repair.
Methods :
Fifty-five patients who underwent arthroscopic rotator cuff repair were included in this study. First 26 cases received no plexus brachialis block (control group), and the next 29 cases received the plexus brachialis block before surgery (block group). Patients completed the visual analog scale at 4, 8, 16, and 24 hours after surgery, and the intensity of postoperative pain was assessed with PainVision™ at 16 hours. The postoperative use of non-steroidal anti-inflammatory agents was also recorded.
Results :
The pain intensity at 16 hours after surgery assessed by PainVision™ was significantly lower in the block group than in the control group (block, 252.0 ± 47.8, control, 489.0 ± 89.1, P < 0.05). However, there were no differences in the VAS values at 16 hours between the 2 groups (block, 4.3 ± 0.6, control, 5.7 ± 0.4, P = N.S.). The pain intensity and VAS at 16 hours after surgery were highly correlated (r = 0.59, P = 0.006 in the block group and r = 0.62, P = 0.003 in the control group). The effect size of the assessment by PainVision™ was bigger than that of VAS (r=0.31 in VAS and 0.51 in Pain vision).
Conclusion :
The PainVision™ system could be useful to evaluate postoperative pain because it enables the quantification and comparison of pain intensity independent of individual pain thresholds.
Keywords: Analysis device, arthroscopic rotator cuff repair, pain intensity, pain quantitative plexus brachialis block, postoperative pain, visual analog scale
INTRODUCTION
Shoulder surgery is often associated with postoperative pain, and approximately 30-70% of patients who undergo shoulder surgery have severe postoperative pain [1]. This postoperative pain has to be controlled to enable the patients to participate in early rehabilitation exercise [2]. Boss et al. reported that severe postoperative pain, particularly within the first postoperative 48 hours, is frequently observed after rotator cuff repair [3]. However, postoperative pain cannot be easily controlled. A variety of techniques are currently used to reduce postoperative pain, such as intra-articular morphine [4-7], regional nerve blocks [8], patient-controlled analgesia [9], and continuous-flow cold therapy [10-12]. A recent study showed that brachial plexus block is one of the most effective treatment modalities during arthroscopic shoulder surgery [13]. However, several side effects have been reported, including failure of the nerve block, phrenic nerve palsy, and rebounding pain.
Pain is a sensation associated with subjective factors and it is therefore difficult to measure and assess [14]. Accordingly, subjective assessment methods such as the visual analogue scale (VAS) or face pain rating scale have been mainly used [15, 16]. These systems have some drawbacks; for example, the VAS has an upper boundary and the face pain rating scale cannot assess continuous variables. In recent years, the PainVision™ system (PS-2100, Nipro Corporation, Osaka, Japan), a quantitative assessment device that functions by substituting pain with different sensory stimuli, has been developed and used mainly in the field of anesthesiology and in pain clinics [17, 18].
In the present study, we used the PainVision™ system to evaluate the effect of plexus brachialis block on postoperative pain after arthroscopic rotator cuff repair. The hypothesis of this study is that the PainVision™ system is more accurate than the VAS to evaluate postoperative pain after arthroscopic rotator cuff repair.
PATIENTS AND METHODS
We performed the case-control study including a total of 55 patients recruited from July 1, 2010, to December 31, 2012. The inclusion criteria were as follows: (1) patients had rotator cuff tear with no other concomitant injury of the involved shoulder, and (2) patients were scheduled to undergo primary arthroscopic rotator cuff repair. Exclusionary criteria were known allergy or hypersensitivity to local anesthetic medications; history of infection at the surgical site within 1 year; history of substance abuse; history of chronic pain syndrome or neuropathy; history of mental illness; use of antidepressants; need for concomitant procedures such as an acromioclavicular joint resection, labral repair, biceps tenodesis, or regional block perioperatively; history of a previous rotator cuff repair; and need for open rotator cuff repair. The IRB protocols were approved by the Institutional Review Board of our institution. All patients received general anesthesia. Induction was achieved with propofol 1.5−2 mg/kg, rocuronium 0.6−1.0 mg/kg, and fentanyl 1−2 μg/kg, and general anesthesia was maintained with 2−5% sevoflurane and 66% N2O in oxygen. For the first 26 cases, no plexus brachialis block was performed (control group; without plexus brachialis block), and for the next 29 cases, the plexus brachialis block was performed by the anesthesiologist under ultrasonographic guidance using 5−10 mL of ropivacaine before surgery (block group; receiving plexus brachialis block). All surgeries were performed by the same senior author. Arthroscopic rotator cuff repair with subacromial decompression was performed using standard techniques. A single row technique was used for small tears, and a suture bridge technique was used for medium to large-sized and massive tears. Concomitant arthroscopic procedures were recorded, and the tear size, operative time, and number of anchors were also recorded. The tear size in complete tears was classified according to the Cofield classification [19]. After closure, patients received a bolus injection of 20 mL of 0.375% ropivacaine into the gleno-humeral joint. All patients were provided with a sling bandage appropriate for the surgery performed.
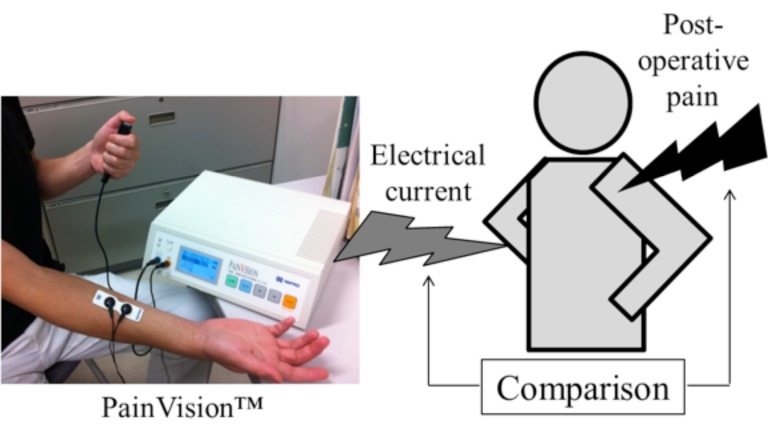
The postoperative resting pain was assessed using the VAS at 8, 16, 24, and 48 hours after surgery. Assessment using the PainVision™ system was performed at 16 hours after surgery. First, sensors transmitting an electric current were attached to the medial forearm contralateral to the operated limb. The current perception threshold, which indicated the pain threshold of each subject, was measured twice, and the mean value was recorded. Second, the pain-compatible electrical current was measured as follows: a gradually increasing pulsed current was applied to the contralateral medial forearm. When the pain caused by the arthroscopic shoulder surgery and the magnitude of electric stimulation were believed to be equal, the current was defined as the pain-compatible electrical current (Fig. 1). The pain-compatible electrical current was measured twice, and the mean value was recorded. On the basis of these measurements, pain intensity was calculated using the following equation:
Fig. (1).
Assessment of pain intensity using the PainVision™ system.
The current perception threshold and the pain-compatible electrical current were measured. On the basis of these measurements, pain intensity was calculated using the following equation: Pain intensity = 100 × (pain-compatible electrical current − current perception threshold)/current perception threshold.
Pain intensity = 100 × (pain-compatible electrical current − current perception threshold)/current perception threshold.
If the patients requested further pain control, non-steroidal anti-inflammatory agents (NSAIDs), diclofenac sodium (50 mg) was administered. Abnormal symptoms such as tingling, perioral numbness, hearing disturbances, visual disturbances, dysarthria, dizziness, nausea, and vomiting were recorded during the first 48 hours after surgery. Shoulder shrugging and active motions of the fingers, wrist, and elbow were permitted immediately after the procedure.
The results were statistically analyzed using a software package (Statview 5.0; Abacus Concepts Inc., Berkeley, CA). Data are expressed as the mean ± standard deviation. Statistical analyses were performed with the Student’s t-test. Comparison of gender between the 2 groups was performed with the chi-square analysis. The ANOVA test was used to compare the size of tears between the 2 groups. The relationship between the pain intensity and VAS was statistically analyzed using Pearson’s correlation coefficient. P < 0.05 was used to denote statistical significance.
RESULTS
In the backgrounds of 55 patients enrolled in the study, there were no significant differences between the 2 groups regarding age, gender, type of tear, operative time, or number of anchors used for rotator cuff repair (Table 1).
Table 1.
Comparison of characteristics and demographics between 2 groups.
| Block Group (n = 26) |
Control Group (n =29) |
P Value |
|
|---|---|---|---|
| Age [mean (range)] (year) | 67.9 (48-83) | 66.2 (33-83) | 0.48 |
| Gender ( male/female) | 19/7 | 20/9 | 0.86 |
| Type of tear | - | - | 0.65 |
| partial | 4 | 6 | - |
| small | 2 | 2 | - |
| medium | 7 | 6 | - |
| large | 4 | 5 | - |
| masstve | 9 | 10 | - |
| Operative time (mean± SD) (min) |
154.3±38.8 | 147.0±44.2 | 0.54 |
| Number of anchor (mean± SD) |
3.8±0.2 | 3.7±0.3 | 0.82 |
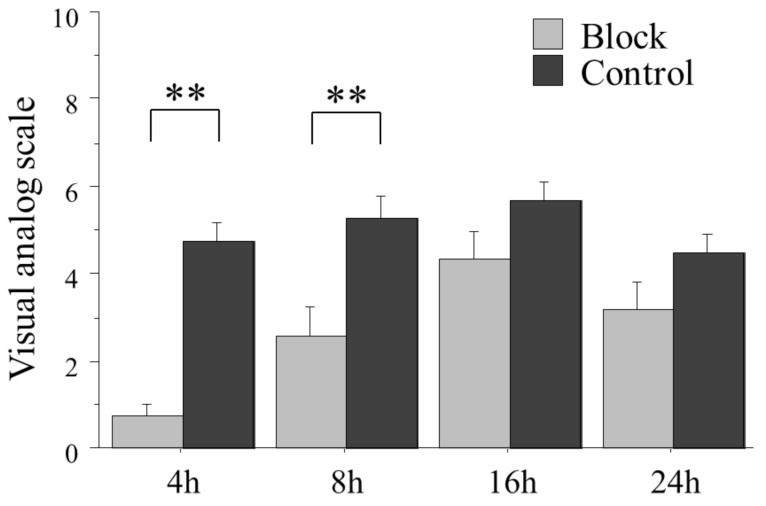
The mean VAS values at 4 and 8 hours postoperatively were significantly lower in the block group than in the control group. However, no differences in the VAS values at 16 and 24 hours were detected between the 2 groups (4 hours: P < 0.01, 16 hours: P = N.S., 24 hours: P = N.S.) (Fig. 2).
Fig. (2).
The mean VAS values at 4 and 8 hours postoperatively were significantly lower in the block group than in the control group. However, no differences in the VAS values at 16 and 24 hours were detected between the 2 groups. (**; P < 0.01).
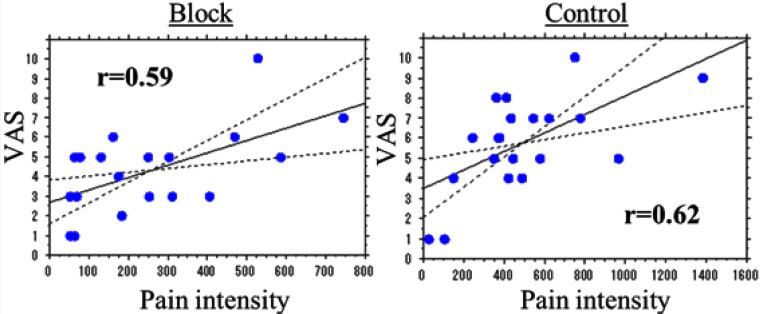
The pain intensity at 16 hours after surgery, as assessed by PainVision™, was significantly lower in the block group than in the control group (P < 0.05) (Fig. 3). The pain intensity and VAS at 16 hours after surgery were highly correlated in both block and control groups (Pearson’s correlation coefficient r = 0.59, P = 0.006 in the block group and r = 0.62, P = 0.003 in the control group) (Fig. 4). The effect size of the assessment by PainVision™ was bigger than that of VAS (r=0.31 in VAS and 0.51 in Pain vision).
Fig. (3).
The pain intensity at 16 hours after surgery, as assessed by PainVision™, was significantly lower in the block group than in the control group. (*; P < 0.05).
Fig. (4).
The pain intensity and VAS at 16 hours after surgery were highly correlated in both block and control groups (Pearson’s correlation coefficient r = 0.59 (P = 0.006) in the block group and r = 0.62 (P = 0.003) in the control group).
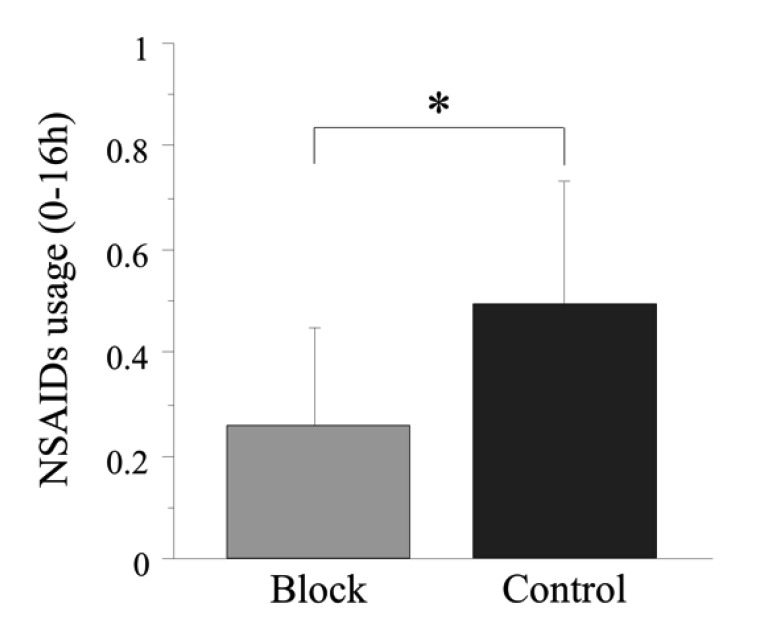
To support the results of VAS and the pain intensity assessed by PainVision™, the NSAIDs usage after surgery was checked. The total amount of the NSAIDs used during postoperative hours 0−16 was significantly greater in the control group than in the block group. (P < 0.05) (Fig. 5).
Fig. (5).
The amount of the NSAIDs used during postoperative hours 0−16 was significantly greater in the control group than in the block group. (*; P<0.05).
No severe complications such as infection, nerve injury, or pneumothorax were observed.
DISCUSSION
Shoulder surgery frequently results in severe postoperative pain, and the underlying mechanism has been characterized as follows: the nerves located in the shoulder joint can be damaged during surgery, exerting pressure on nociceptors associated with intra-operative damage; reflective muscle contractions are induced in many muscles connecting the vertebral spine and the upper extremities adjacent to these joints [20]. Therefore, the preemptive and intraoperative analgesia provided by local infiltration, intravenous regional anesthesia, intra-articular anesthesia, neuraxial block, peripheral nerve block, and continuous infusions should be considered [7]. An increase in postoperative pain is correlated with a decrease in patient’s quality of recovery in the immediate postoperative period [21]. It was reported that postoperative pain control is essential following surgery so that patients can participate in early rehabilitation exercise [2]. Especially, the first 24 hours after surgery are important for the control of pain after arthroscopic shoulder surgery [20].
Currently, subjective methods such as the VAS are frequently used as pain assessment methods [14-16]. In these methods, the intensity of pain is determined by comparing the reported pain level with a “pain of maximum intensity” value. However, quantitative data comparisons are difficult with these subjective methods, as the sensitivity to pain varies greatly among individuals. A quantitative analysis device for perception and pain called “PainVision™” was recently developed and has been used in the field of pain and anesthesiology [7, 17]. This system is based on the provision of alternative painless sensory stimulation equivalent to pain (through the stimulation of sensory nerve fibers Aβ and Aδ) and the measurement of the intensity of the stimulation. Because individual pain thresholds are evaluated first for accurate subsequent measurement with the device, pain intensity can be quantitatively compared among patients. Therefore, this device enables a more objective evaluation when compared with other commonly used methods. The results of the present study showed that, in the correlation analysis, the pain intensity and VAS at 16 hours after surgery were highly correlated. Therefore, the PainVision™ system could be considered as efficient as the VAS for the assessment of postoperative pain. The results of PainVision™ assessment showed that the pain intensity at 16 hours after surgery was significantly lower in the block group than in the control group. On the other hand, the mean VAS at 16 hours postoperatively showed a lower score in the block group than in the control group, although the difference between the 2 groups did not reach statistical significance. To compare the strength of relationship between VAS and Pain vision system, we calculated the effect size. The results demonstrated that the effect size of the assessment by PainVision™ was bigger than that of VAS. As an effect size is a measure of the strength of relationship and relates to the power of a study, this result indicated that the PainVision™ system could be more accurate in the assessment of postoperative pain compared with VAS. Our result of NSAIDs usage indicated that the patients felt more pain during postoperative hours 0−16, which would support the validity in the results assessed by PainVision™. Matsumura et al. also reported that the PainVision™ system is more sensitive than conventional assessment methods such as the VAS because it enables a highly reproducible quantification and comparison of pain intensity independent of individual pain thresholds [17]. Similarly, a discrepancy of the statistical results at 16 hours postoperatively between the VAS and PainVision™ systems might be associated with differences in pain sensitivity. From these results in this paper, it could be possible that the PainVision™ system would make us evaluate the postoperative pain more objectively and accuracy.
The interscalene brachial plexus block is the most frequently used pain relief technique in arthroscopic shoulder surgery [22-24]. Singelyn et al. reported that this block was the most efficient analgesic technique after arthroscopic acromioplasty [24]. Therefore, in our institute, a single-dose interscalene block is performed during arthroscopic shoulder surgery. The results of our study indicated that a single-dose interscalene block could significantly reduce postoperative pain for 8−16 hours after surgery and decrease the total amount of NSAIDs used 16 hours postoperatively. Therefore, the plexus brachialis blockade is effective to reduce postoperative pain after arthroscopic rotator cuff repair. Additionally, a recent study reported that single-dose interscalene block with continuous intralesional infusion of ropivacaine provides effective pain control [25]. On the other hand, Klein et al. reported that continuous intra-articular infusion of ropivacaine combined with single-dose interscalene block provides better pain relief than interscalene block alone [26]. As a next step, we plan to compare the effectiveness of single-dose interscalene block with that of single-dose interscalene block combined with continuous intra-articular infusion of ropivacaine.
The present study has some limitations, such as the small number of subjects and the inclusion of a single institution. However, one of the advantages is that all the surgeries were performed by a single surgeon. Second, the patients did not use narcotics as an analgesic because of the protocol of this study, which was different from usual situation. Third, we assessed the pain intensity assessed by PainVision™ in just one time 16 hours after surgery. The further examination will be needed.
CONCLUSION
The results of our study indicated that the PainVision™ system could be useful for the evaluation of postoperative pain because it enables the quantification and comparison of pain intensity independent of individual pain thresholds.
ACKNOWLEDGEMENTS
Declared none.
LIST OF ABBREVIATIONS
- NSAIDs
= Non-steroidal anti-inflammatory agents
- VAS
= Visual analog scale
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Moote CA. The prevention of postoperative pain. Can J Anaesth. 1994;41:527–33. doi: 10.1007/BF03011550. [DOI] [PubMed] [Google Scholar]
- 2.Borgeat A, Ekatodramis G. Anaesthesia for shoulder surgery. Best Pract Res Clin Anaesthesiol. 2002;16:211–25. doi: 10.1053/bean.2002.0234. [DOI] [PubMed] [Google Scholar]
- 3.Boss AP, Maurer T, Seiler S, Aeschbach A, Hintermann B, Strebel S. Continuous subacromial bupivacaine infusion for postoperative analgesia after open acromioplasty and rotator cuff repair preliminary results. J Shoulder Elbow Surg. 2004;13:630–34. doi: 10.1016/j.jse.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Boden BP, Fassler S, Cooper S, Marchetto PA, Moyer RA. Analgesic effect of intraarticular morphine, bupivacaine, and morphine/bupivacaine after arthroscopic knee surgery. Arthroscopy. 1994;10:104–7. doi: 10.1016/s0749-8063(05)80301-9. [DOI] [PubMed] [Google Scholar]
- 5.Jaureguito JW, Wilcox JF, Cohn SJ, Thisted RA, Reider B. A comparison of intraarticular morphine and bupivacaine for pain control after outpatient knee arthroscopy.A prospetive randomized, double-blinded study. Am J Sports Med. 1995;23:350–3. doi: 10.1177/036354659502300318. [DOI] [PubMed] [Google Scholar]
- 6.Lundin O, Rydgren B, Sward L, Karlsson J. Analgesic effects of intra-articular morphine during and after knee arthroscopy a comparison of two methods. Arthroscopy. 1998;14:192–6. doi: 10.1016/s0749-8063(98)70040-4. [DOI] [PubMed] [Google Scholar]
- 7.Richardson MD, Bjorksten AR, Hart JA, McCullough K. The efficacy of intra-articular morphine for postoperative knee arthroscopy analgesia. Arthroscopy. 1997;13:584–9. doi: 10.1016/s0749-8063(97)90184-5. [DOI] [PubMed] [Google Scholar]
- 8.Edkin BS, Spindler KP, Flanagan JF. Femoral nerve block as an alternative to parenteral narcotics for pain control after anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:404–9. doi: 10.1016/0749-8063(95)90191-4. [DOI] [PubMed] [Google Scholar]
- 9.Matheny JM, Hanks GA, Rung GW, Blanda JB, Kalenak A. A comparison of patient-controlled analgesia and continuous lumbar plexus block after anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:87–90. doi: 10.1016/s0749-8063(05)80350-0. [DOI] [PubMed] [Google Scholar]
- 10.Daniel DM, Stone ML, Arendt DL. The effect of cold therapy on pain, swelling, and range of motion after anterior cruciate ligament reconstructive surgery. Arthroscopy. 1994;10:530–33. doi: 10.1016/s0749-8063(05)80008-8. [DOI] [PubMed] [Google Scholar]
- 11.Speer KP, Warren RF, Horowitz L. The efficacy of cryotherapy in the postoperative shoulder. J Shoulder Elbow Surg. 1996;5:62–8. doi: 10.1016/s1058-2746(96)80032-2. [DOI] [PubMed] [Google Scholar]
- 12.Barber FA, McGuire DA, Click S. Continuous-flow cold therapy for outpatient anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:130–35. doi: 10.1016/s0749-8063(98)70030-1. [DOI] [PubMed] [Google Scholar]
- 13.Kempen PM, O'Donnell J, Lawler R, Mantha V. Acute respiratory insufficiency during interscalene plexus block. Anesth Analg. 2000;90:1415–6. doi: 10.1097/00000539-200006000-00029. [DOI] [PubMed] [Google Scholar]
- 14.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity a comparison of six methods. Pain. 1986;27:117–26. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 15.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales a critical review. Psychol Med. 1988;18:1007–19. doi: 10.1017/s0033291700009934. [DOI] [PubMed] [Google Scholar]
- 16.Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The faces pain scale-revised toward a common metric in pediatric pain measurement. Pain. 2001;93:173–83. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- 17.Matsumura H, Imai R, Gondo M, Watanabe K. Evaluation of pain intensity measurement during the removal of wound dressing material using 'the PainVision system' for quantitative analysis of perception and pain sensation in healthy subjects. Int Wound J. 2012;9:451–5. doi: 10.1111/j.1742-481X.2011.00911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fukada T, Iwakiri H, Ozaki M. A randomised double-blind crossover trial of the potential analgesic effect of a transdermal nicotine patch in non-smokers based on objective and subjective assessment. Eur J Anaesthesiol. 2011;28:592–6. doi: 10.1097/EJA.0b013e328347dfd4. [DOI] [PubMed] [Google Scholar]
- 19.Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet. 1982;154:667–72. [PubMed] [Google Scholar]
- 20.Lee SM, Park SE, Nam YS , et al. Analgesic effectiveness of nerve block in shoulder arthroscopy comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc. 2012;20:2573–8. doi: 10.1007/s00167-012-1950-5. [DOI] [PubMed] [Google Scholar]
- 21.Lewis RN. The use of combined suprascapular and circumflex (articular branches) nerve blocks in the management of chronic arthritis of the shoulder joint. Eur J Anaesthesiol. 1999;16:37–41. doi: 10.1046/j.1365-2346.1999.00401.x. [DOI] [PubMed] [Google Scholar]
- 22.Al-Kaisy A, McGuire G, Chan VW , et al. Analgesic effect of interscalene block using low-dose bupivacaine for outpatient arthroscopic shoulder surgery. Reg Anesth Pain Med. 1998;23:469–73. [PubMed] [Google Scholar]
- 23.Laurila PA, Lopponen A, Kanga-Saarela T, Flinkkila T, Salomaki TE. Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesthesiol Scand. 2002;46:1031–6. doi: 10.1034/j.1399-6576.2002.460818.x. [DOI] [PubMed] [Google Scholar]
- 24.Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery a comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg. 2004;99:589–92. doi: 10.1213/01.ANE.0000125112.83117.49. [DOI] [PubMed] [Google Scholar]
- 25.Oh JH, Kim WS, Kim JY, Gong HS, Rhee KY. Continuous intralesional infusion combined with interscalene block was effective for postoperative analgesia after arthroscopic shoulder surgery. J Shoulder Elbow Surg. 2007;16:295–9. doi: 10.1016/j.jse.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Klein SM, Nielsen KC, Martin A , et al. Interscalene brachial plexus block with continuous intraarticular infusion of ropivacaine. Anesth Analg. 2001;93:601–5. doi: 10.1097/00000539-200109000-00015. [DOI] [PubMed] [Google Scholar]