Abstract
Objective: To determine the optimal selection of proximal fusion level for degenerative scoliosis (DS) and investigate the long-term proximal-related complications. Methods: Profiles of 95 consecutive patients with DS who underwent posterior long instrumented fusion were analyzed retrospectively. Perioperative parameters were reviewed stratified into 3 groups according to the relationship between the upper instrumented vertebrae (UIV), horizontal vertebrae (HV) and upper end vertebrae (UEV), namely HV Group (UIV = HV or above), HV-UEV Group (UIV = between HV and UEV) and UEV Group (UIV = UEV or below) in coronal plane and 3 groups in sagittal plane according to segment levels. Clinical and radiographic parameters were studied statistically. Results: Average follow-up was 7.8 years (range, 5-13 years). HV Group showed a significant increase in operative time, intraoperative blood loss, postoperative in-bed time, and hospital stays. UEV Group showed greater average Cobb angle, AVT and DW. UEV Group showed significant increase in operative time, blood loss, postoperative in-bed time, and inpatient stay. All three groups showed significant improvement in ODI compared to baseline, while there was no significant difference in LL between three groups. Proximal-related late complications included recurrent junctional scoliosis in 4 cases and junctional kyphosis in 4 cases. Conclusions: Recurrent junctional scoliosis developed more commonly when the fusion was at or below the UEV, and fusion at L1 or L2 showed the highest incidence of junctional kyphosis. Long instrumented fusion to T11 or T12 appeared to be a reasonable alternative when the UIV was above UEV in DS.
Keywords: Degenerative scoliosis, proximal fusion level, proximal-related late complications, junctional scoliosis, junctional kyphosis
Introduction
As the senile population is steadily increasing, degenerative scoliosis (DS) becomes a major health problem. The rising number of elderly patients suffering from associated symptoms due to spinal deformity and neural compression may fail conservative treatment and may become eligible for surgical intervention. In contrast to idiopathic scoliosis, the goals of surgery for DS include decompression of symptomatic neural elements, stabilization of involved segments, and, when appropriate, restoration of spinal balance.
Posterior long instrumented fusion has become one of the major surgical treatments for DS, and the selection of fusion levels play an important role in the treatment success. Inappropriate selection of fusion levels or insufficient correction of coronal and sagittal curve in the scoliosis results in disease progression or decompensation. Although many studies have reported on the selection of distal fusion level for DS, less attention has been paid to the selection of proximal fusion level.
We have performed a retrospective comparative analysis of clinical and radiographic profiles of proximal fusions at 3 levels in DS surgeries. The purpose of the current study is to determine the optimal selection of proximal fusion level in posterior long instrumented fusion for DS.
Materials and methods
Demographic data
From January 1st, 1999 to December 31st, 2007, we included 128 consecutive patients with DS who underwent posterior long instrumented fusion for DS. Radiographic inclusion criteria included: 1) spondylolisthesis; 2) lateral listhesis at least 2 mm; 3) coronal Cobb angle of least 25 degrees; 4) lordosis from L1 to S1 of less than 20 degrees; and 5) kyphosis from T10 to L2 of greater than 20 degrees. Clinical inclusion criteria were: 1) age at least 50 years at the time of diagnosis; 2) persisting symptoms (low back pain, radicular leg pain, or intermittent claudication) refractory to conservative treatment for at least 6 months; 3) no history of idiopathic scoliosis; 4) long instrumented fusion for at least 3 levels; and 5) follow-up for at least 5 years.
Surgical indication and selection of fusion levels
The primary indication of surgery was radicular leg pain and/or intermittent claudication associated with DS. Both the coronal and sagittal planes were evaluated thoroughly when deciding fusion levels. In the coronal plane, we preferred to include fusion of the most rotated vertebrae or the most tilted vertebrae. The fusion was extended proximally if the junctional kyphotic angle in the sagittal plane was more than 10 degrees. As for the distal fusion level, fusion stopped at L5 if the L5-S1 disc appeared healthy on preoperative MRI. The fusion was extended to the sacrum in case of a preexisting L5-S1 deformity, such as spondylolisthesis and spinal stenosis. In patients with significant sagittal imbalance, the fusion was also extended to the sacrum even if L5-S1 was healthy because of the high incidence of adjacent level degeneration.
Stratification
According to the relationship between the upper instrumented vertebrae (UIV), horizontal vertebrae (HV), and upper end vertebrae (UEV), the patients were divided into three groups in the coronal plane: Group HV (when the UIV was the HV or above), Group HV-UEV (when the UIV was between the HV and the UEV), Group UEV (when the UIV was the UEV or below) (Figure 1), and three groups in sagittal plane: Group T9-10 (UIV between T9 and T10), Group T11-12 (UIV between T11 and T12), Group L1-2 (UIV between L1 and L2).
Figure 1.
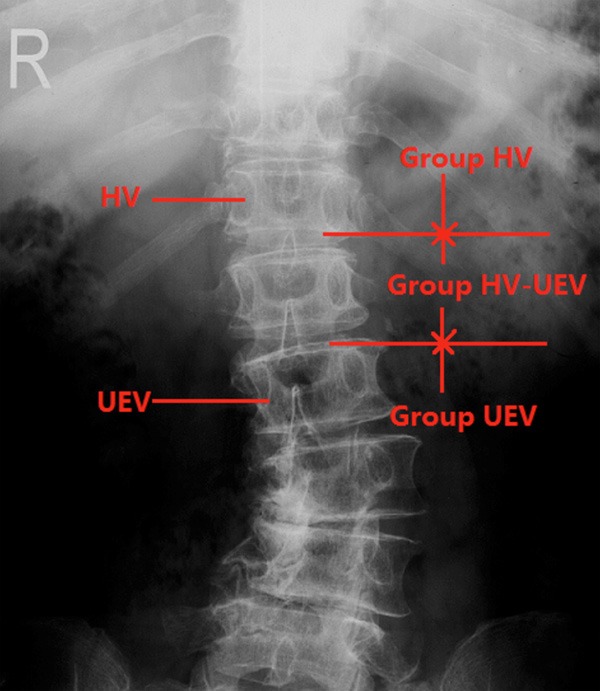
Diagram showing categorizing method of three groups in the coronal plane. The patients were divided into three groups in the coronal plane: Group HV (UIV HV or above); Group HV-UEV (UIV between HV and UEV); Group UEV (UIV UEV or below). HV horizontal vertebrae; UEV upper end vertebrae.
Data collection
Perioperative parameters included operation time, intraoperative blood loss, postoperative in-bed time and hospital stays, and the segments fused. Clinical outcomes were assessed using Oswestry Disability Index (ODI). Follow-ups were performed based on questionnaires and radiographic evaluations. Informed consent was acquired in each patient and this study was approved by local institutional review board. Pre- and post-operative thoracolumbar anteroposterior and lateral standing radiographs were taken and assessed before surgery, within 1 month after surgery, and at final follow-up. Coronal Cobb angle of the major curve, lateral apical vertebral translation (AVT) and disc wedging above UIV (DW) were measured in the coronal plane. AVT was measured using the distance from the central sacral line to the mid-point of the apical vertebrae/disc. DW above UIV was measured between the line along the cephalad endplate of the UIV and the caudal endplate of the vertebrae above the UIV. Lumbar lordosis (LL), thoracolumbar kyphosis (TLK) and junctional kyphosis (JK) were measured in the sagittal axis. LL was measured from the upper endplate of L1 to that of S1 on the lateral radiograph. TLK was measured from the upper endplate of T10 to the lower endplate of L2 on the lateral radiograph. JK was measured from the lower endplate of the UIV to the upper endplate of one vertebra above the UIV. Recurrent junctional scoliosis in the coronal plane was defined as Cobb angle of greater than 10 degrees and the DW above UIV worsened by more than 10 degrees compared to the preoperative value. Junctional kyphosis in the sagittal plane was defined as more than 10 degrees compared to the preoperative value.
Statistical analysis
The data from this study were analyzed using SPSS 17.0 statistics software (SPSS Inc., USA). Comparison of the clinical parameters before surgery and at final follow-up was studied using paired T tests. Pearson Chi-square tests were used to compare the clinical and radiographic parameters between three groups. A p value of less than 0.05 was considered statistically significant.
Results
The average follow-up time was 7.8 years (range, 5 to 13 years). There were 37 men and 58 women with the average age of 58.5 ± 8.5 years. All patients had severe low back pain, 86 patients (92.2%) had different severity of neurogenic claudication, 20 patients (21.1%) had no pain relief by flexion, and 4 patients (4.1%) exhibited a foot drop before surgery. All patients underwent nonsurgical treatment for at least 6 months that failed to provide relief of symptoms.
Relationship between UIV, UEV, HV and NV (neutral vertebrae)
The UIV included vertebrae from T9 to L2. The most commonly performed UIV was at L1 (27 patients) and the second most commonly used UIV was at T12 (20 patients). The UEV included vertebrae from T10 to L2. The most commonly used UEV was L1 (33 patients) and the second most commonly used UEV at L2 (28 patients). The NV included vertebrae from T10 to L2. The most commonly used NV was at T12 (36 patients) and the second most commonly performed HV was at T11 (25 patients). The HV included vertebrae from T8 to L1, which was cephalad to UEV or NV. The most commonly performed HV was at T10 (40 patients) and the second most commonly performed HV was at T11 (28 patients) (Figure 2).
Figure 2.
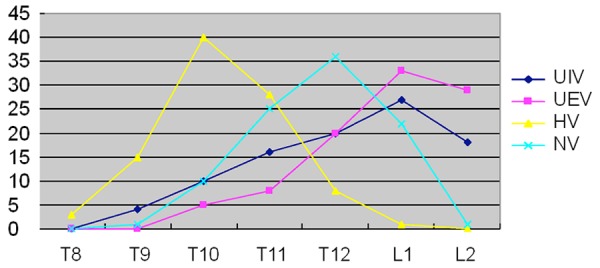
The number of patients who had UIV, UEV, HV and NV at each level; UIV: upper instrumented vertebrae; UEV upper end vertebrae; HV horizontal vertebrae; NV neutral vertebral.
Comparison of coronal plane groups
In the coronal plane, 95 patients were stratified into Group HV (n = 21), Group HV-UEV (n = 29), and Group UEV (n = 45). Since the HV was placed cephalad to UEV, Group HV showed a much longer fusion level than the other two groups (P < 0.001). The average number of fusion levels was 7.4 ± 0.8 segments in Group HV, 5.8 ± 1.4 segments in Group HV-UEV, and 4.0 ± 0.9 segments in Group UEV. There were no significant differences between three groups with regard to age, sex ratio and body mass index (BMI) (P = 0.88; P = 0.69; P = 0.11). Group HV showed a significant increase in operation time, intraoperative blood loss, postoperative in-bed time and hospital stay compared to the other two groups (P = 0.01; P = 0.02; and P = 0.04; P = 0.01, respectively). There were no significant differences between three groups in preoperative and postoperative ODI (P = 0.48; and P = 0.09, respectively), while all the three groups had a significant improvement in ODI at final follow-up compared to baseline levels (P = 0.038; P = 0.002; and P = 0.048, respectively) (Table 1). There were no significant differences between three groups in Cobb angle, AVT and DW preoperatively (P = 0.69; P = 0.98; and P = 0.09, respectively). Immediately after surgery there were no significant differences between three groups in Cobb angle, AVT and DW (P = 0.08; P = 0.38; and P = 0.10, respectively). However, at final follow-up Group UEV showed significantly greater Cobb angle, AVT and DW than the other two groups (P = 0.02; P = 0.03; and P = 0.004, respectively) (Table 2).
Table 1.
Comparisons of clinical parameters between three groups in the coronal plane
| Group HV (n = 21) | Group HV-UEV (n = 29) | Group UEV (n = 45) | P value | |
|---|---|---|---|---|
| Age (years) | 57.2 ± 7.2 | 58.3 ± 6.1 | 59.2 ± 4.8 | 0.88 |
| Sex ratio (M/F) | 9:12 | 11:18 | 17:28 | 0.79 |
| BMI (kg/m2) | 22.7 ± 4.7 | 23.1 ± 3.9 | 23.2 ± 4.1 | 0.99 |
| No. of fused levels | 7.4 ± 0.8 | 5.8 ± 1.4 | 4.0 ± 0.9 | 0.00 |
| Operation time (h) | 5.5 ± 0.8 | 4.2 ± 1.2 | 3.8 ± 1.1 | 0.01 |
| Blood loss (ml) | 1240 ± 210 | 780 ± 180 | 690 ± 120 | 0.02 |
| In-bed time (d) | 9.6 ± 1.2 | 6.1 ± 0.8 | 5.7 ± 1.1 | 0.04 |
| Hospital stays (d) | 21.2 ± 3.3 | 15.8 ± 2.4 | 14.1 ± 1.2 | 0.01 |
| Pre-op ODI | 34.9 ± 9.6 | 33.2 ± 7.8 | 32.9 ± 7.7 | 0.09 |
| Post-op ODI | 13.2 ± 6.9 | 12.5 ± 5.9 | 11.1 ± 4.8 | 0.66 |
BMI indicates body mass index; Pre-op indicates pre-operative; Post-op indicates post-operative.
Table 2.
Comparisons of radiographic parameters between three groups in the coronal plane
| Group HV | Group HV-UEV | Group UEV | P value | ||
|---|---|---|---|---|---|
| Cobb angle (°) | Pre-op | 27.8 ± 7.8 | 28.4 ± 9.3 | 28.6 ± 5.6 | 0.69 |
| IMPO | 3.2 ± 1.1 | 4.0 ± 1.8 | 3.2 ± 1.2 | 0.08 | |
| Post-op | 6.6 ± 2.8 | 7.5 ± 3.5 | 18.8 ± 3.6 | 0.02 | |
| Δ1 | -19.9 ± 6.8 | -20.2 ± 7.1 | -20.8 ± 5.4 | 0.19 | |
| Δ2 | -17.7 ± 5.7 | -18.6 ± 5.9 | -3.8 ± 6.0 | 0.01 | |
| AVT (mm) | Pre-op | 8.9 ± 2.3 | 9.3 ± 2.7 | 8.8 ± 1.9 | 0.98 |
| IMPO | 2.8 ± 1.8 | 3.2 ± 2.1 | 3.7 ± 1.3 | 0.38 | |
| Post-op | 3.0 ± 1.7 | 3.3 ± 1.9 | 7.8 ± 2.9 | 0.03 | |
| Δ1 | -6.3 ± 1.5 | -5.9 ± 0.8 | -5.4 ± 1.1 | 0.06 | |
| Δ2 | -5.3 ± 2.6 | -6.7 ± 1.8 | -1.0 ± 1.7 | 0.01 | |
| DW Above UIV (°) | Pre-op | 2.3 ± 1.2 | 3.6 ± 1.7 | 4.2 ± 1.8 | 0.09 |
| IMPO | 2.1 ± 1.4 | 3.1 ± 1.2 | 3.7 ± 2.2 | 0.10 | |
| Post-op | 3.4 ± 1.8 | 4.2 ± 1.3 | 10.8 ± 4.6 | 0.004 | |
| Δ1 | 0.0 ± 0.7 | -0.4 ± 0.5 | -0.7 ± 0.9 | 0.17 | |
| Δ2 | 1.2 ± 0.6 | 1.0 ± 0.3 | 6.7 ± 2.9 | 0.04 |
Pre-op indicates pre-operative; IMPO indicates immediate postoperative; Post-op indicates post-operative; Δ1 = IMPO-Pre-op; Δ2 = Post-op-Pre-op.
Comparison of sagittal plane groups
In the sagittal plane, 95 patients were stratified into Group T9-10 (n = 22), Group T11-12 (n = 33), and Group L1-2 (n = 40). The average fusion levels were 7.8 ± 0.9 segments in Group T9-10, 6.1 ± 1.0 segments in Group T11-12, and 4.5 ± 0.9 segments in Group L1-2. There were no significant differences between three groups with regard to age, sex ratio and body mass index (BMI) (P = 0.18; P = 0.66; and P = 0.94, respectively). Group L1-2 showed a significant increase in operation time, intraoperative blood loss, postoperative in-bed time and hospital stay compared to the other two groups (P = 0.03; P = 0.04; P = 0.026; and P = 0.001, respectively). There were no significant differences between the three groups in preoperative and postoperative ODI (P = 0.28; and P = 0.19), while all the three groups showed a significant improvement in ODI at final follow-up compared to baseline levels (P = 0.033; P = 0.012; and P = 0.044, respectively) (Table 3). There were no significant differences between three groups in preoperative LL, TLK and JK (P = 0.69; P = 0.98; and P = 0.09, respectively). Immediately after surgery there were no significant differences between the three groups in LL, TLK and JK (P = 0.09; P = 0.88; and P = 0.14, respectively). However, at final follow-up Group L1-2 showed significantly greater TLK and JK than other two groups (P = 0.001; P = 0.038) (Table 4).
Table 3.
Comparisons of clinical parameters between three groups in the sagittal plane
| Group T9-10 (n = 22) | Group T11-12 (n = 33) | Group L1-2 (n = 40) | P value | |
|---|---|---|---|---|
| Age (years) | 56.2 ± 4.2 | 59.4 ± 7.1 | 60.2 ± 4.3 | 0.18 |
| Sex ratio (M/F) | 10:12 | 13:20 | 14:26 | 0.10 |
| BMI (kg/m2) | 23.8 ± 6.7 | 22.4 ± 6.9 | 22.9 ± 5.1 | 0.55 |
| No. of fused levels | 7.8 ± 0.9 | 6.1 ± 1.0 | 4.5 ± 0.9 | 0.00 |
| Operation time (h) | 5.9 ± 1.8 | 4.8 ± 1.7 | 3.9 ± 1.3 | 0.03 |
| Blood loss (ml) | 1240 ± 210 | 780 ± 180 | 690 ± 120 | 0.04 |
| In-bed time (d) | 8.8 ± 1.2 | 6.0 ± 0.8 | 4.7 ± 1.1 | 0.026 |
| Hospital stays (d) | 23.2 ± 4.3 | 15.6 ± 2.7 | 13.3 ± 3.6 | 0.001 |
| Pre-op ODI | 33.8 ± 7.6 | 32.0 ± 6.8 | 32.7 ± 9.7 | 0.33 |
| Post-op ODI | 11.2 ± 5.9 | 13.5 ± 6.9 | 10.9 ± 4.4 | 0.068 |
BMI indicates body mass index; Pre-op indicates pre-operative; Post-op indicates post-operative.
Table 4.
Comparisons of radiographic parameters between three groups in the sagittal plane
| Group T9-10 | Group T11-12 | Group L1-2 | P value | ||
|---|---|---|---|---|---|
| LL (°) | Pre-op | 18.8 ± 10.4 | 19.4 ± 10.3 | 21.6 ± 12.6 | 0.69 |
| IMPO | 23.2 ± 10.1 | 28.0 ± 11.8 | 30.2 ± 10.9 | 0.09 | |
| Post-op | 22.6 ± 12.8 | 27.5 ± 13.5 | 29.8 ± 13.6 | 0.22 | |
| Δ1 | 5.9 ± 6.8 | 7.2 ± 7.1 | 8.8 ± 5.4 | 0.19 | |
| Δ2 | 3.7 ± 2.7 | 5.6 ± 1.9 | 6.8 ± 3.0 | 0.11 | |
| TLK (°) | Pre-op | 10.9 ± 5.3 | 9.3 ± 4.7 | 10.8 ± 4.9 | 0.98 |
| IMPO | 7.8 ± 3.8 | 7.2 ± 2.9 | 8.7 ± 4.3 | 0.88 | |
| Post-op | 9.0 ± 2.7 | 8.3 ± 3.9 | 16.8 ± 5.9 | 0.001 | |
| Δ1 | -1.3 ± 1.5 | -1.9 ± 1.8 | -2.1 ± 1.3 | 0.06 | |
| Δ2 | -0.9 ± 1.6 | -1.1 ± 1.0 | 7.9 ± 2.7 | 0.01 | |
| JK (°) | Pre-op | 3.5 ± 2.8 | 4.5 ± 2.9 | 3.8 ± 2.3 | 0.09 |
| IMPO | 4.5 ± 2.3 | 5.0 ± 1.7 | 4.9 ± 2.6 | 0.14 | |
| Post-op | 4.9 ± 6.1 | 5.7 ± 4.4 | 14.2 ± 4.5 | 0.038 | |
| Δ1 | 1.2 ± 2.6 | 0.8 ± 1.3 | 1.3 ± 1.1 | 0.17 | |
| Δ2 | 1.4 ± 3.3 | 1.2 ± 2.1 | 10.8 ± 3.7 | 0.04 |
Pre-op indicates pre-operative; IMPO indicates immediate postoperative; Post-op indicates post-operative; Δ1 = IMPO-Pre-op; Δ2 = Post-op-Pre-op.
Proximal-related late complications
Proximal-related late complications included recurrent junctional scoliosis in the coronal plane in 4 cases and junctional kyphosis in the sagittal plane in another 4 cases during the study period.
Discussion
DS usually has two curves in the lumbar spine: a major curve in the mid-lumbar spine and a compensatory curve in the lower lumbar spine. The thoracic curve is not commonly seen. The proximal lumbar curve has the apex at L2 or L3, usually with L3-L4 rotatory subluxation and L4-L5 lateral listhesis, and ends proximally at the thoracolumbar (TL) junction. The HV, UEV and NV are all placed in TL junction, which is likely to be susceptible to injury or degenerative changes. All these anatomical features of DS will influence our decision-making about proximal fusion level.
When determining the extent of fusion in DS, spinal alignment should be evaluated in both coronal and sagittal planes. In the coronal plane, ideally, the fusion includes all the segments within the deformity [8]. Therefore, HV can be chosen as UIV to create a balanced spine, but may lead to higher perioperative risks due to a relatively larger surgery. Previous studies have advocated that proximal fusion level should be horizontal, neutral and stable in the coronal plane [9-12]. However, there are several options since the HV, NV and UEV are usually not the same vertebra in the same patient [13]. Cho KJ et al reported that proximal adjacent segment diseases developed more commonly when proximal fusion stopped at UEV or below in a cohort of 51 DS patients at an average follow-up of 3.4 years, and they thus suggested that UIV should be above UEV in the coronal plane [7]. Our study demonstrated that Group UEV had greater Cobb angle, AVT and DW than the other two groups at final follow-up, and junctional recurrent scoliosis in the coronal plane developed more commonly when the proximal fusion stopped at the UEV or below in DS, which has never been reported before.
In this cohort, 4 patients in Group UEV demonstrated junctional recurrent scoliosis 2 years after surgery with an average Cobb angle of 25.5 degrees and an average DW above UIV of 19.6 degrees. All 4 patients underwent a revision surgery with a longer fusion to HV (Illustrative case: Figure 3). We propose possible reasons for these complications: 1) when proximal fusion stopped at UEV or below, the UIV was not parallel with the upper adjacent vertebrae, which would lead to an asymmetric DW above UIV. This asymmetric angle then resulted in the increase of shear stress of the adjacent segment, which can cause asymmetric degeneration of the disc and facet joints; 2) After long instrumented fusion from the thoracolumbar spine to L5 or S1, due to lack of the compensatory rotation of the adjacent vertebrae, stress concentration on the proximal junctional area in the coronal plane could not be transmitted to the sagittal plane, which could accelerate coronal junctional scoliosis. It is worth noting that all the 4 patients underwent a long fusion to S1, which sacrifices the motion of the lumbosacral joint. Thus, stress concentration by a relatively longer fusion might have predisposed recurrent scoliosis of the proximal junctional area.
Figure 3.
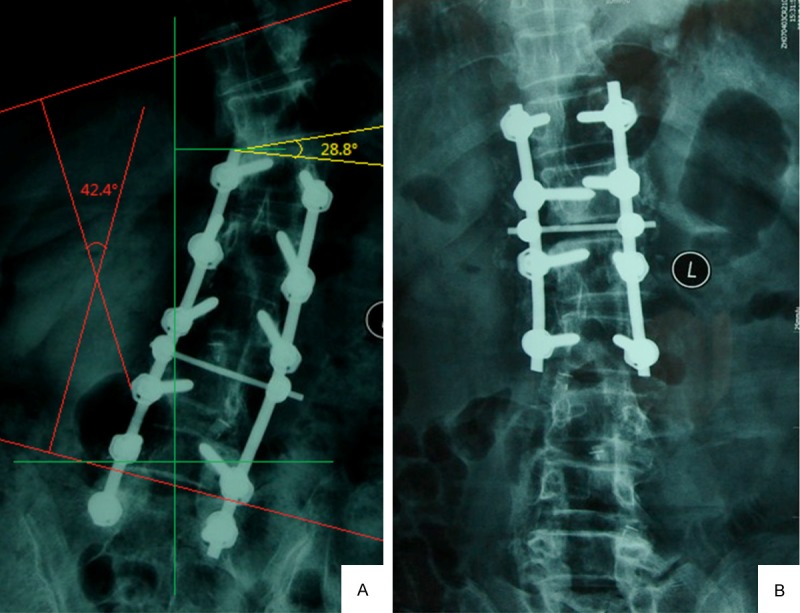
Female 68 years A. 2 years after surgery lumbar anterioposterior film showed a junctional recurrent scoliosis with a Cobb angle of 42.4 degrees and a DW above UIV of 28.8 degrees. B. Coronal deformity was corrected after the revision surgery.
In the sagittal plane, the TL junction (T10-L2) has unique anatomic characteristics. It serves as the transition from the immobile thoracic spine to the mobile lumbar spine. There is a change in the orientation of the facet joints from the coronal plane proximally to the sagittal plane distally. The sagittal alignment changes from thoracic kyphosis to lumbar lordosis. Biomechanically, the true ribs tend to increase the stability of the thoracic spine through the thoracic rib cage. The rib cage effectively lengthens the transverse dimensions of the spine, giving the thoracic spine greater resistance to bending in the sagittal, coronal, and axial planes. The upper 10 thoracic vertebrae (T1-T10) take this mechanical support through the true ribs, but T11 and T12 have floating ribs without costosternal articulation. These levels lack the ligamentous support provided by the costovertebral articulations, the costocorporeal joint and the costotransverse joint. Due to these anatomic and biomechanical characteristics, some previous studies insisted that proximal junctional problems, consisting of proximal adjacent segment degeneration, compression fracture proximal to the UIV, or screw failure in the UIV, occured more frequently with fusions ending at T11 to L2 as compared with those ending at T10 or above [14-16]. Some demonstrated that fusions ending at L1 or L2 had a higher prevalence of junctional kyphosis or UIV failure, but there were no obvious differences between T9-10 and T11-12 [14]. Others however reported these three different proximal fusion levels did not demonstrate significant radiographic and clinical outcomes or proximal-related complications after surgery [17-19]. Our study demonstrated that Group L1-L2 showed greater TLK and JK than the other two groups at final follow-up and stopping fusion at L1 or L2 showed the highest incidence of junctional kyphosis in the sagittal plane.
It is noteworthy that our data showed, in spite of no significant differences in postoperative clinical outcomes between three groups in the coronal plane, the incidence of junctional recurrent scoliosis was highest in Group UEV. Therefore, we suggest that proximal fusion between the HV and UEV appears to be a reasonable selection. In the sagittal plane, the three groups showed no significant differences in postoperative clinical outcomes, and the incidence of junctional kyphosis was highest in Group L1-2. Thus, considering the risks and benefits of long instrumented fusion for DS in both coronal and sagittal planes, fusion to T11 or T12 appears to be a reasonable alternative when UIV is above UEV in the coronal plane.
Our study has limitations. First, the study is of retrospective nature. Though we attempted to study a consecutive series of patients, we were only able to reach 74.2% of patients for final follow-up. Second, we did not assess coronal and sagittal balance due to lack of anteroposterior and lateral radiographs for the whole spine due to loss of radiographic data. This will inevitably influence the integrity and validity of the study.
Conclusions
Recurent junctional scoliosis in the coronal plane developed more commonly when the proximal fusion stopped at UEV or below in DS. Stopping fusion at L1 or L2 showed the highest incidence of junctional kyphosis in the sagittal plane. Considering the risks and benefits of long instrumented fusion for DS in both coronal and sagittal planes, fusion to T11 or T12 appears to be an alternative selection when UIV is above UEV in the coronal plane.
Disclosure of conflict of interest
None.
References
- 1.Ploumis A, Transfledt EE, Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J. 2007;7:428–436. doi: 10.1016/j.spinee.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Liu HY, Zhou DG, Wang HM, Yi B, Wang B, Jin ZH, Zhang J. The surgical treatment for degenerative scoliosis. Chin Med J. 2003;83:1066–1069. [PubMed] [Google Scholar]
- 3.Mok JM, Hu SS. Surgical strategies and choosing levels for spinal deformity: how high, how low, front and back. Neurosurg Clin N Am. 2007;18:329–337. doi: 10.1016/j.nec.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 4.De Vries AA, Mullender MG, Pluymakers WJ, Castelein RM, van Royen BJ. Spinal decompensation in degenerative lumbar scoliosis. Eur Spine J. 2010;19:1540–1544. doi: 10.1007/s00586-010-1368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polly DW Jr, Hmmill CL, Bridwell KH. Debate: to fuse or not to fuse to the sacrum, the fate of the L5~S1 disc. Spine (Phila Pa 1976) 2006;31(Suppl):S179–184. doi: 10.1097/01.brs.0000234761.87368.ee. [DOI] [PubMed] [Google Scholar]
- 6.Edwards CC 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusions to L5 and the sacrum: a matched cohort analysis. Spine (Phila Pa 1976) 2004;29:1996–2005. doi: 10.1097/01.brs.0000138272.54896.33. [DOI] [PubMed] [Google Scholar]
- 7.Cho KJ, Suk SI, Park SR, Kim JH, Choi SW, Yoon YH, Won MH. Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. Eur Spine J. 2009;18:531–537. doi: 10.1007/s00586-009-0883-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HJ, Lenke LG, Shaffrey CI, Van Alstyne EM, Skelly AC. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery. Spine (Phila Pa 1976) 2012;37:S144–164. doi: 10.1097/BRS.0b013e31826d611b. [DOI] [PubMed] [Google Scholar]
- 9.Bridwell KH. Selection of instrumentation and fusion levels for scoliosis: where to start and where to stop. J Neurosurg Spine. 2004;1:1–8. doi: 10.3171/spi.2004.1.1.0001. [DOI] [PubMed] [Google Scholar]
- 10.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 11.Shufflebarger H, Suk SI, Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine (Phila Pa 1976) 2006;31(Suppl):S185–194. doi: 10.1097/01.brs.0000232811.08673.03. [DOI] [PubMed] [Google Scholar]
- 12.Simmons ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res. 2001;384:45–53. doi: 10.1097/00003086-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Kuklo TR. Principles for selecting fusion levels in adult spinal deformity with particular attention to lumbar curves and double major curves. Spine (Phila Pa 1976) 2006;31(Suppl):S132–138. doi: 10.1097/01.brs.0000236023.08226.90. [DOI] [PubMed] [Google Scholar]
- 14.Cho KJ, Suk SI, Park SR, Kim JH, Jung JH. Selection of proximal fusion level for adult degenerative lumbar scoliosis. Eur Spine J. 2013;22:394–401. doi: 10.1007/s00586-012-2527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang NG, Wang YP, Qiu GX, Zhang JG, Shen JX, Zhao Y, Li SG, Yu B. Radiological evaluation of intervertebral angles on short-segment fusion of degenerative lumbar scoliosis. Chin Surg J. 2010;48:506–510. [PubMed] [Google Scholar]
- 16.Kim JH, Kim SS, Suk SI. Incidence of proximal adjacent failure in adult lumbar deformity correction based on proximal fusion level. Asian Spine J. 2007;1:19–26. doi: 10.4184/asj.2007.1.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho KJ, Suk SI, Park SR, Kim JH, Kang SB, Kim HS, Oh SJ. Risk factors of sagittal decompensation after long posterior intrumentation and fusion for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2010;35:1595–1601. doi: 10.1097/BRS.0b013e3181bdad89. [DOI] [PubMed] [Google Scholar]
- 18.Lewis SJ, Abbas H, Chua S, Bacon S, Bronstein Y, Goldstein S, Magana S, Sullivan K, Dold AP, Bodrogi A. Upper instrumented vertebral fractures in long lumbar fusions. Spine (Phila Pa 1976) 2012;37:1407–1414. doi: 10.1097/BRS.0b013e31824fffb9. [DOI] [PubMed] [Google Scholar]
- 19.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Kim YW. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine J. 2007;32:2653–2661. doi: 10.1097/BRS.0b013e31815a5a9d. [DOI] [PubMed] [Google Scholar]


