Abstract
Adjuvant sufentanil could achieve effective spinal anesthesia with low dose of hyperbaric ropivacaine for cesarean delivery. Two previous studies had calculated the 50% effective dose (ED50) of intrathecal ropivacaine coadministered with sufentanil for cesarean delivery. However, the 95% effective dose (ED95) of intrathecal hyperbaric ropivacaine coadministered with sufentanil for cesarean delivery remains uncertain. This study determined the ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil for cesarean delivery. 80 ASA physical status I or II parturients undergoing elective cesarean delivery were enrolled in this prospective, randomized, double-blind investigation. A combined spinal and epidural anesthesia was performed at the L3-L4 interspace. Patients received a dose of spinal ropivacaine coadministered with sufentanil 5 μg diluted to 3.0 ml with normal saline and 0.5 ml of 10% dextrose: 7.5 mg (n = 20), 9.0 mg (n = 20), 10.5 mg (n = 20), or 12 mg (n = 20). An effective dose was defined as a dose that provided bilateral sensory block to T7 within 10 min after intrathecal drug administration and required no epidural top-up for surgery to be completed. The ED50 and ED95 values for successful anesthesia were determined using a logistic regression model. The ED50 (95% confidence interval [CI]) for successful anesthesia was 8.4 (4.0-9.8) mg and the ED95 (95% CI) was 11.4 (9.7-13.9) mg. The results show that the ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil 5 μg for cesarean delivery was 11.4 mg. The addition of sufentanil could significantly reduce the dosage of ropivacaine.
Keywords: Cesarean delivery, ropivacaine, sufentanil, spinal anesthesia
Introduction
Ropivacaine, a new long-acting amino-amide local anesthetic with differential sensory motor block, had been wildly used in obstetric patients [1]. Compared with bupivacaine, ropivacaine has less cardiac and CNS toxicity [2,3], less motor blocking properties, and earlier mobilization [4]. The 50% effective dose (ED50) and the estimated 95% effective dose (ED95) of spinal plain ropivacaine alone for cesarean delivery were 16.7 and 26.8 mg, respectively [5].
Low dose of intrathecal local anesthetic could reduce adverse effects of spinal anesthesia such as hypotension [6], whereas potentially increase spinal anesthetic block failures. However, successful anesthesia can be achieved by low dose of local anesthetics coadministered with opioids [7,8]. Sufentanil, a more lipophilic and higher analgesic opioid compared with fentanyl or morphine [9-11], is a suitable opioid used for cesarean delivery. The ED50 of intrathecal ropivacaine coadministered with sufentanil for cesarean delivery was 6.44 mg or 8.1 mg in two previous studies [12,13]. However, the ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil for cesarean delivery remains uncertain.
The present study was undertaken to determine the ED95 of intrathecal hyperbaric ropivacaine when coadministered with sufentanil 5 μg for cesarean delivery.
Methods
This study was approved by the Clinical Research Ethics Committee of the Second Affiliated Hospital of Wenzhou Medical University. After receiving written informed consent from all patients, 80 full term singleton parturients (ASA physical status I or II, aged from 20 to 35) scheduled for elective cesarean delivery were randomly allocated by drawing coded shuffled opaque envelops to receive one of four doses of spinal ropivacaine (AstraZeneca, Södertälje Sweden) coadministered with sufentanil 5 μg: 7.5, 9.0, 10.5, or 12 mg. All doses were diluted to 3.0 ml with normal saline and 0.5 ml of 10% dextrose. The mixed solutions for spinal anesthesia were prepared under sterile conditions by an anesthetist and administered by a second anesthetist who remained blinded to its contents. Exclusion criteria were history of allergy or sensitivity to amide-type local anesthetics, history of bronchial asthma or cardiac disease, contraindication in spinal anesthesia, suspected fetal abnormality, and pregnancy induced hypertension.
No premedication was given. All patients had an intravenous catheter inserted into a large peripheral arm vein and 500 ml Lactated Ringer’s solution administered before spinal anesthesia. Continuous pulse oximetry (SpO2), electrocardiogram (ECG) and Non-invasive arterial pressure (NIBP) were applied. NIBP, heart rate and SpO2 were measured automatically at 2-min intervals from the start of anesthesia for 10 min, and at 5-min intervals until the end of surgery. Parturients were performed combined spinal epidural anesthesia lying in the left lateral position. Using the method of loss of resistance to air, an 18-G Tuohy needle was inserted into the epidural space at the L3-L4 interspace. After performing spinal puncture with a 25-G pencil point needle, spinal solutions were injected over 30 s when free flow of cerebrospinal fluid was conformed. Epidural catheter was threaded into the epidural space and fixed. Patients were then moved to supine with a 15º left lateral tilt and received intravenous ephedrine 5 mg. Oxygen was given at 2 L/min via nasal cannulae during the operation.
Sensory and motor block were assessed at 2.5 min intervals for the first 10 min after spinal injection and then at 10-min intervals until the end of surgery. The level of sensory block was assessed bilaterally along the mid clavicular line by the loss of pinprick sensation and was performed using a 17 G needle. Sensory level to pinprick was assessed by the Hollmen scale [6] 0 = ability to appreciate a pinprick as sharp; 1 = ability to appreciate a pinprick as less sharp; 2 = inability to appreciate a pinprick as sharp (analgesia); and 3 = inability to appreciate a pin touching (anesthesia). Motor block in the lower limbs was determined according to the Bromage Scale [14] (0 = able to lift extended leg at hip; 1 = able to flex knee but not lift extended leg; 2 = able to move foot only; and 3 = unable to move foot). The time for sensory block to develop to T10 (onset time to T10), maximum sensory block height, and the time to motor block of Bromage 1 (onset time to Bromage 1) were recorded. Subjective pain was assessed with a 10-cm linear visual analogue scale (VAS).
According to Khaw et al [5], the endpoint of an effective or ineffective dose of ropivacaine was defined. An effective dose was defined as a bilateral sensory block to T7 within 10 min of intrathecal drug administration, with no additional epidural top-up required during surgery. An ineffective dose was defined as a T7 sensory level was not obtained within 10 min of intrathecal drug administration, or a T7 sensory level was obtained within 10 min of intrathecal drug administration but epidural top-up was required during surgery because of patient reported a significant pain (VAS > 2). In case of ineffective dose, the epidural was topped up using 2% lidocaine administrated in 5 ml bolus until successful anesthesia was obtained.
Side effects such as hypotension, bradycardia, respiratory depression, nausea, vomiting, shivering, and pruritus during surgery were recorded. Hypotension was defined as a decrease in systolic arterial pressure to less than 100 mmHg or less than 80% from baseline [5]. Ephedrine 5 mg was given when hypotension developed. The total dose of ephedrine administered was recorded. Respiratory depression was defined as oxygen saturation below 95%. Bradycardia was defined as a heart rate less than 50 beats/min.
The sample size estimation was based on an assumed SD of 1.33 mg as being one-sixth the range of likely dose (8-16 mg). A value of 0.9 had the power to a difference of 2 mg at P < 0.05. It was then estimated that a minimum of 16 patients would be necessary in each group. Demographic data are presented as mean ± SD or median (interquartile range) where appropriate. Statistical analysis was performed with the use of SPSS 16.0 for Windows (SPSS Inc., Chicago, IL). Normally distributed data were assessed by one-way analysis of variance. Nonnormally distributed data assessed by Kruskal-Wallis test. The Fisher exact test was used for incidence data. A value of P < 0.05 was considered as statistically significant.
The dose-response relation for spinal hyperbaric ropivacaine when coadministered with sufentanil was determined using probit analysis [5]. Dates for successful rate for each dosage were used to plot a probit log dose-response relation and a sigmoid dose-response curve. Using SPSS 16.0, a probit regression was performed to plot a probit log dose-response relation to get the coefficients, and interpolation was used to obtain the ED50 and ED95.
Results
All 80 patients completed the study. Demographic and surgical data were similar among the groups for age, weight, height, duration of surgery, and gestational age (Table 1).
Table 1.
Demographic and obstetric date
| 7.5 mg (n = 20) | 9.0 mg (n = 20) | 10.5 mg (n = 20) | 12.0 mg (n = 20) | |
|---|---|---|---|---|
| Age, yr | 28 ± 3 | 28 ± 4 | 29 ± 4 | 30 ± 5 |
| Height, cm | 162 ± 7 | 160 ± 5 | 161 ± 4 | 159 ± 3 |
| Weight, kg | 70 ± 6 | 68 ± 9 | 70 ± 7 | 69 ± 8 |
| Gestational age, wk | 39 ± 1 | 40 ± 1 | 39 ± 2 | 39 ± 1 |
| Weight of neonate, g | 3370 ± 443 | 3403 ± 424 | 3418 ± 346 | 3347 ± 276 |
| Duration of surgery, min | 43 ± 8 | 42 ± 7 | 44 ± 8 | 43 ± 10 |
A simple bar chart of inadequate block height, intraoperative pain, and successful anesthesia for each dose was shown (Figure 1). Overall success of spinal anesthesia was 25, 70, 90, and 95% in the 7.5, 9, 10.5, and 12 mg group, respectively. Using probit analysis, a probit log dose-response relation was plotted. The linear regression analysis of the log (dose) response showed a regression coefficient (r) of 0.986 (P < 0.01) and a coefficient of determination (r2) of 0.972 (Figure 2). Then, interpolations were used to draw a sigmoid dose-response curve (Figure 3). The ED50 (95% confidence interval [CI]) for success anesthesia was 8.4 (4.0-9.8) mg and the ED95 (95% CI) was 11.4 (9.7-13.9) mg.
Figure 1.
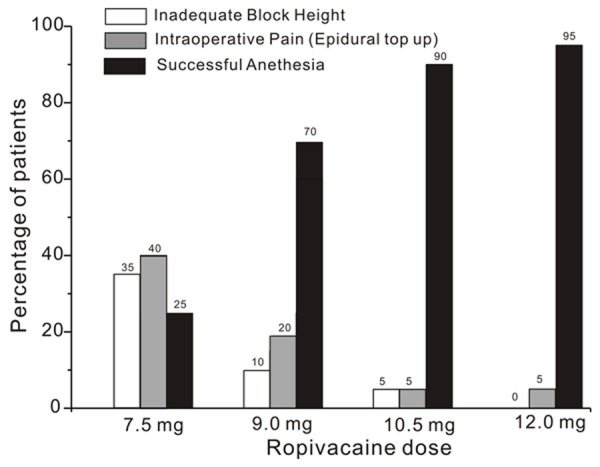
Proportions (%) of patients with inadequate block height, intraoperative pain needed epidural top up, and successful anesthesia at different doses of intrathecal hyperbaric ropivacaine. The white bar represents inadequate block height (defined as a bilateral a T7 sensory level was not obtained within 10 min of intrathecal drug administration), the gray bar represents intraoperative pain needed epidural top up (defined as a bilateral T7 sensory level was obtained within 10 min of intrathecal drug administration but epidural top-up was required during surgery because of patient reported a significant pain (VAS>2) and the black bar represents successful anesthesia (defined as a bilateral sensory block to T7 within 10 min of intrathecal drug administration, with no additional epidural top-up required during surgery).
Figure 2.
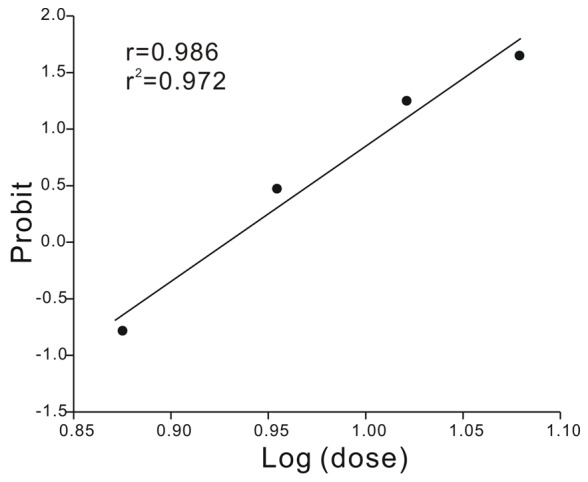
Linear regression plot of the probit value against the log (dose).
Figure 3.
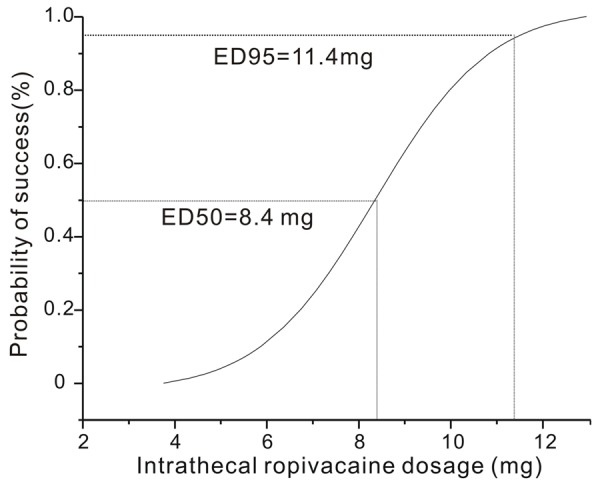
The ED50 and ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil 5 μg for cesarean delivery calculated from the linear regression plot of probability of successful anesthesia versus dose of intrathecal ropivacaine. Probabilities of 0.05 and 0.95 were used to derive the ED50 and ED95, respectively.
Block characteristics were showed in Table 2. We found the onset times of sensory block to T10, highest level of block, and the motor block to Bromage 1 were similar among groups. The median [range] maximum block height was higher and the motor block was significantly more intense when higher ropivacaine dose was used (P < 0.05).
Table 2.
Characteristics of spinal anesthesia
| 7.5 mg (n = 20) | 9.0 mg (n = 20) | 10.5 mg (n = 20) | 12.0 mg (n = 20) | |
|---|---|---|---|---|
| Sensory block (to pinprick) | ||||
| Highest level of block | T7 (T4-10) | T5 (T3-7)* | T5 (T3-8)* | T5 (T3-8)* |
| Onset time to T10 (min) | 2.5 (1-5) | 2.5 (1-5) | 2.5 (2-5) | 2.5 (1.5-5) |
| Time to highest level of block (min) | 10 (5-20) | 10 (5-20) | 8.75 (5-15) | 10 (7.5-20) |
| Motor block | ||||
| Maximum Bromage scale 0-1-2-3 | 7-8-4-1 | 4-9-5-2 | 0-5-9-6*,# | 1-2-10-7*,# |
| Onset time to Bromage 1 (min) | 7.5 (2.5-10) | 5 (2.5-7.5) | 5 (2.5-10) | 5 (2.5-10) |
P < 0.05 compared with the group of ropivacaine 7.5 mg;
P < 0.05 compared with the group of ropivacaine 9.0 mg.
No significant differences among groups were observed regarding the incidence of hypotension, bradycardia, respiratory depression, nausea, vomiting, shivering, pruritus, and the consumption of ephedrine (Table 3).
Table 3.
Adverse effects associated with different doses of intrathecal ropivacaine
| 7.5 mg (n = 20) | 9.0 mg (n = 20) | 10.5 mg (n = 20) | 12.0 mg (n = 20) | |
|---|---|---|---|---|
| Hypotension | 3 | 4 | 5 | 7 |
| Bradycardia | 1 | 0 | 0 | 0 |
| Respiratory depression | 0 | 0 | 0 | 0 |
| Nausea | 4 | 5 | 4 | 4 |
| Vomiting | 1 | 1 | 2 | 1 |
| Shivering | 0 | 0 | 0 | 1 |
| Pruritus | 6 | 8 | 7 | 10 |
| Ephedrine dose, mg | 5 (5-10) | 5 (5-10) | 5 (5-15) | 5 (5-15) |
Discussion
The present study determined the ED50 and ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil 5 μg for cesarean delivery. Using probit analysis, we quantified the ED50 (95% confidence interval [CI]) for successful anesthesia was 8.4 (4.0-9.8) mg and the ED95 (95% CI) was 11.4 (9.7-13.9) mg. Our result indicate that the ED50 and ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil 5 μg are much lower than the published report of the optimal doses of ropivacaine alone for cesarean delivery. Khaw et al [5] reported that the ED50 and estimated ED95 for spinal plain ropivacaine alone for cesarean delivery were 16.7 and 26.8 mg, respectively. This may be due to following several reasons.
First, we think the adjuvant sufentanil plays an important role in reducing the dosage of ropivacaine. Many studies had reported that the additional of opioids to low-dose local anesthetics can provide successful anesthesia for cesarean delivery [7,8,13-16]. One previous study showed that intrathecal sufentanil 5 μg produced a 28% reduction of the ED50 of intrathecal hyperbaric ropivacaine for cesarean delivery [12]. Gautier et al [17] used intrathecal isobaric ropivacaine 12 mg with sufentanil 2.5 μg for cesarean delivery and found 87% of the patients had a successful anesthesia. In our present study, we used sufentanil 5 μg (higher than 2.5 μg) with ropivacaine 11.4 mg could provide a successful anesthesia for 95% of the patients, which was in accordance with Gautier et al [17].
Second, we used hyperbaric local anesthetic solution for spinal anesthesia. Compared with plain local anesthetic solution, hyperbaric local anesthetic solution could produce more extensive spread and a greater success rate [18,19]. The addition of glucose to a local anesthetic solution encourages the spinal solution pull down to the lowest point of the thoracic hollow in the supine position [20,21].
Finally, in our study, the surgical technique did not involve exteriorization of the uterus. In most hospitals of China, surgeons always apply abdominal cavity exploration instead of exteriorization of the uterus, which profoundly reduce the surgical stimulus that supposed to significantly reduce anesthetic requirement.
The onset times of sensory block to T10, heghest level of block, and the motor block to Bromage 1 were similar among groups, which were in accordance with previous reports indicating that the onset was not dose-dependent [5,22,23]. Khaw et al [5] found that there was no difference in the maximum block height between high and low dose of ropivacaine. In contrast, our results have shown that the mean height of sensory block was increased when higher ropivacaine dosages were used. We think the spread of the bolus of drug is related to dosage. With increasing dosage of ropivacaine, the number of patients developing full motor block increased which was similar to other published findings [5,22,23].
Increasing the dose of local anesthetic had been found to increase maternal hypotension and nausea [7]. Although we could not demonstrate that the ropivacaine dose has a statistically significant correlation with the overall incidence of hypotension, there were a slightly greater percentage patients had hypotension with higher doses of spinal ropivacaine. We think inadequate sample size might make this tendency insignificant.
There were several limitations to our study. Firstly, we only recorded the characteristics of sensory block and motor block during the operation and did not record the duration of the sensory and motor block because our primary aim was to determine the ED50 and ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil. Secondly, we did not perform umbilical blood gas analysis, which could give extra information about neonatal well-being. Thirdly, we did not determine the ED50 and ED95 of intrathecal sufentanil with hyperbaric ropivacaine for cesarean delivery, and further studies are needed. Finally, the sample size may not large enough to compare the incidence of hypotension among groups.
In this study, we quantified the ED95 of intrathecal hyperbaric ropivacaine coadministered with sufentanil 5 μg for cesarean delivery was 11.4 mg. The addition of sufentanil could significantly reduce the dosage of ropivacaine.
Disclosure of conflict of interest
None.
References
- 1.Geng G, Li W, Huang S. Pulmonary effects of bupivacaine and ropivacaine in parturients undergoing spinal anesthesia for elective cesarean delivery. Int J Clin Exp Med. 2014;7:1417–21. [PMC free article] [PubMed] [Google Scholar]
- 2.Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N. Central nervous and cardiovascular effects of i. v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78:507–14. doi: 10.1093/bja/78.5.507. [DOI] [PubMed] [Google Scholar]
- 3.Groban L, Deal DD, Vernon JC, James RL, Butterworth J. Cardiac resuscitation after incremental overdosage with lidocaine, bupivacaine, levobupivacaine, and ropivacaine in anesthetized dogs. Anesth Analg. 2001;92:37–43. doi: 10.1097/00000539-200101000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Van de Velde M, Dreelinck R, Dubois J, Kumar A, Deprest J, Lewi L, Vandermeersch E. Determination of the full dose-response relation of intrathecal bupivacaine, levobupivacaine, and ropivacaine, combined with sufentanil, for labor analgesia. Anesthesiology. 2007;106:149–56. doi: 10.1097/00000542-200701000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Khaw KS, Ngan Kee WD, Wong EL, Liu JY, Chung R. Spinal ropivacaine for cesarean section: A dose-finding study. Anesthesiology. 2001;95:1346–50. doi: 10.1097/00000542-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Carvalho B, Durbin M, Drover DR, Cohen SE, Ginosar Y, Riley ET. The ED50 and ED95 of intrathecal isobaric bupivacaine with opioids for cesarean delivery. Anesthesiology. 2005;103:606–12. doi: 10.1097/00000542-200509000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Ben-David B, Miller G, Gavriel R, Gurevitch A. Low-dose bupivacaine-fentanyl spinal anesthesia for cesarean delivery. Reg Anesth Pain Med. 2000;25:235–9. [PubMed] [Google Scholar]
- 8.Choi DH, Ahn HJ, Kim MH. Bupivacaine-sparing effect of fentanyl in spinal anesthesia for cesarean delivery. Reg Anesth Pain Med. 2000;25:240–5. doi: 10.1016/s1098-7339(00)90005-1. [DOI] [PubMed] [Google Scholar]
- 9.Leysen JE, Gommeren W, Niemegeers CJ. [3H] Sufentanil, a superior ligand for mu-opiate receptors: binding properties and regional distribution in rat brain and spinal cord. Eur J Pharmacol. 1983;87:209–25. doi: 10.1016/0014-2999(83)90331-x. [DOI] [PubMed] [Google Scholar]
- 10.Grass JA, Sakima NT, Schmidt R, Michitsch R, Zuckerman RL, Harris AP. A randomized, double-blind, dose-response comparison of epidural fentanyl versus sufentanil analgesia after cesarean section. Anesth Analg. 1997;85:365–71. doi: 10.1097/00000539-199708000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Olofsson C, Nygards EB, Bjersten AB, Hessling A. Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients. Acta Anaesthesiol Scand. 2004;48:1240–4. doi: 10.1111/j.1399-6576.2004.00504.x. [DOI] [PubMed] [Google Scholar]
- 12.Chen X, Qian X, Fu F, Lu H, Bein B. Intrathecal sufentanil decreases the median effective dose of intrathecal hyperbaric ropivacaine for cesarean delivery. Acta Anaesthesiol Scand. 2010;54:284–90. doi: 10.1111/j.1399-6576.2009.02051.x. [DOI] [PubMed] [Google Scholar]
- 13.Parpaglioni R, Baldassini B, Barbati G, Celleno D. Adding sufentanil to levobupivacaine or ropivacaine intrathecal anesthesia affects the minimum local anaesthetic dose required. Acta Anaesthesiol Scand. 2009;53:1214–20. doi: 10.1111/j.1399-6576.2009.02033.x. [DOI] [PubMed] [Google Scholar]
- 14.Qian XW, Chen XZ, Li DB. Low-dose ropivacaine- sufentanil spinal anesthesia for cesarean delivery: a randomised trial. Int J Obstet Anesth. 2008;17:309–14. doi: 10.1016/j.ijoa.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 15.Wang LZ, Zhang YF, Tang BL, Yao KZ. Effects of intrathecal and i. v. small-dose sufentanil on the median effective dose of intrathecal bupivacaine for Cesarean section. Br J Anaesth. 2007;98:792–6. doi: 10.1093/bja/aem101. [DOI] [PubMed] [Google Scholar]
- 16.Ben-David B, Solomon E, Levin H, Admoni H, Goldik Z. Intrathecal fentanyl with small-dose dilute bupivacaine: Better anesthesia without prolonging recovery. Anesth Analg. 1997;85:560–5. doi: 10.1097/00000539-199709000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Gautier P, De Kock M, Huberty L, Demir T, Izydorczic M, Vanderick B. Comparison of the effects of intrathecal ropivacaine, levobupivacaine, and bupivacaine for cesarean section. Br J Anaesth. 2003;91:684–9. doi: 10.1093/bja/aeg251. [DOI] [PubMed] [Google Scholar]
- 18.Khaw KS, Ngan Kee WD, Wong M, Floria N, Lee A. Spinal ropivacaine for cesarean delivery: a comparison of hyperbaric and plain solutions. Anesth Analg. 2002;94:680–5. doi: 10.1097/00000539-200203000-00037. [DOI] [PubMed] [Google Scholar]
- 19.Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JA. Comparison of plain and hyperbaric solutions of ropivacaine for spinal anesthesia. Br J Anaesth. 2005;94:107–11. doi: 10.1093/bja/aei008. [DOI] [PubMed] [Google Scholar]
- 20.Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004;93:568–78. doi: 10.1093/bja/aeh204. [DOI] [PubMed] [Google Scholar]
- 21.Vercauteren MP, Coppejans HC, Hoffmann VH, Saldien V, Adriaensen HA. Small dose hyperbaric versus plain bupivacaine during spinal anesthesia for cesarean section. Anesth Analg. 1998;86:989–93. doi: 10.1097/00000539-199805000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Gautier PE, De Kock M, Van Steenberge A, Poth N, Lahaye-Goffart B, Fanard L, Hody JL. Intrathecal ropivacaine for ambulatory surgery. Anesthesiology. 1999;91:1239–45. doi: 10.1097/00000542-199911000-00013. [DOI] [PubMed] [Google Scholar]
- 23.McDonald SB, Liu SS, Kopacz DJ, Stephenson CA. Hyperbaric spinal ropivacaine: A comparison to bupivacaine in volunteers. Anesthesiology. 1999;90:971–7. doi: 10.1097/00000542-199904000-00007. [DOI] [PubMed] [Google Scholar]


