Abstract
Fentanyl-induced cough (FIC) should be effectively prevented in patients requiring stable induction of general anesthesia. Our study was to evaluate the suppressive effects of different doses of intravenous dezocine on FIC during the induction of general anesthesia. A total of 400 patients of American Society of Anesthesiologists (ASA) physical status I and II were randomized into four groups (n = 100). Right before Fentanyl bolus, the four groups were given intravenously a matching placebo (group I) (equal volume of 0.9% saline), dezocine 0.025 mg/kg (group II), 0.05 mg/kg (group III), and 0.1 mg/kg (group IV), respectively. Patients were induced with fentanyl 3 µg/kg and the injection time of fentanyl was less than 5 s in all patients. The occurrence of cough was recorded 2 min after fentanyl bolus. The incidence of FIC was 40% in group I, 12% in group II, 4% in group III, and 0 in group IV. Group I had significantly higher incidence of FIC than Groups II, III and IV (P < 0.05). Group IV had lower incidence of FIC than Groups II (0% vs 12%; P = 0.0003) and III (0% vs 4%; P = 0.043). Our study showed that intravenous dezocine reduced the incidence of FIC during anesthetic induction. The suppressive effect was dose-dependent.
Keywords: Fentanyl, cough, dezocine, general anesthesia
Introduction
Fentanyl is a synthetic opioid, which is a popular drug for anesthesiologists because of its quick onset, short duration of action, ease of titrability, intense analgesia, cardiovascular stability and low histamine release [1,2]. However, fentanyl-induced cough (FIC) is often reported after intravenous bolus administration of fentanyl during anesthesia induction [3-5]. FIC may be undesirable because of the increase of intracranial, intraocular, and intra-abdominal pressures. FIC is transient and not severe in most patients. But FIC should be effectively prevented when patients were associated with pneumothorax, cerebral aneurysm, brain trauma, brain hernia, open eye injury, arterial aneurysm resection, hypersensitive airway disease, full stomach and so on [6-9].
Dezocine is a mixed agonist-antagonist opioid, a full agonist of κ-receptor and partial agonist of μ-receptor [10-12]. Dezocine is widely applied as perioperative pain analgesic agent in China. Fentanyl binds most readily to the μ-receptor and less well to the κ-receptor. This implies that FIC may be from agonism at the μ-receptor. Recently Sun et al. [13] demonstrated that intravenous administration of 0.1 mg/kg dezocine completely suppressed FIC during induction. Although Sun et al. has demonstrated a proper dosage for dezocine to prevent FIC. In this study iv dezocine was administered 10 min before induction, which may be not a convenient practice in some emergent situations. Furthermore, the effects of different doses of dezocine on FIC are still unknown.
The hypothesis of this study was that the effects of different doses of dezocine on FIC might be different. So we designed a prospective, randomized, double blinded, and placebo controlled study to investigate the effects of different doses of dezocine on FIC in patients during the induction of general anesthesia. The primary outcome was the incidence of cough.
Methods
This prospective randomized, double-blind trial (ChiCTR. org ID ChiCTR-TRC-13003359) was approved by the Cancer Hospital, Fudan University Institutional Human Ethics Committee, Shanghai, China (Chairperson Professor Dr J. Wu; protocol number: 1307124-2) on 17 July 2013. After having obtained written informed consent, 400 American Society of Anesthesiologists physical status I-II patients, aged 20-70 years were included in the trial. Exclusion criteria included a history of smoking, asthma, chronic cough, pregnancy, upper airway infection within 2 weeks of surgery, bronchodilators, or steroids in the previous 2 weeks.
Patients were randomly allocated into 4 groups by the use of computer-generated codes. Allocation concealment was established by placing the randomization sequence in consecutively numbered, opaque envelopes. Group I received saline; Group II received dezocine 0.025 mg/kg; Group III received 0.05 mg/kg; Group IV received dezocine 0.1 mg/kg. Patients in Group II, III, IV received dezocine which was diluted with saline to 10 ml, just before fentanyl bolus; whereas patients in Group I received the equal volume of 10 ml saline. The study was carried out by three investigators in a blinded manner as follows: Each test solution was prepared in a syringe by the first investigator, who was also responsible for subject grouping. The second investigator, who was blinded to the type of test solution, performed the iv injection. The variables were recorded by the third investigator, who was blinded to the type of test solution.
None of the patients received any premedication. Before being taken to the operating room, a 20-gauge cannula was inserted into the dorsum of each patient’s hand and connected to a T-connector for drug administration. Upon arrival, standard ASA monitors were attached, including non-invasive arterial pressure, electrocardiography, and pulse oximetry. Then, patients were given the following medications intravenously: Group I received saline; Group II dezocine 0.025 mg/kg; Group III 0.05 mg/kg; Group IV dezocine 0.1 mg/kg.
Just after dezocine administration, fentanyl 3 µg/kg was administered through the peripheral iv line less than 5 seconds. The occurrence and severity of cough for 2 min after the fentanyl injection were recorded since the cough generally happens within this period of time. The severity of cough was graded, based on the number of episodes of cough, as none (0), mild (1-2), moderate (3-4), or severe (5 or more). Systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and SpO2 were recorded before the administration of dezocine or normal saline (T0) and 2 min (T1) later after fentanyl injection. The oxygen saturation was closely observed and when SpO2 dropped below 90%, manually assisted mask ventilation with oxygen was to be applied immediately. The incidences of apnea and truncal rigidity were also recorded. Apnea was defined as a pause in breathing for more than 15 seconds. Truncal rigidity was defined as increased large trunk muscle tone, which renders facemask ventilation difficult or impossible. Propofol and cisatracurium were administered after 2 min fentanyl bolus.
All statistical analyses were performed with SPSS version 12.0 software package (SPSS Inc., Chicago, IL). The sample size was based upon previously published study [3], and 91 patients per group would be required to detect a 50% reduction in the incidence of cough, assuming a 40% baseline incidence of cough after an IV bolus of fentanyl (errors: α = 0.05 and β = 0.8). To compensate for potential dropouts, we enrolled 100 patients in each group.
Continuous variables are presented as mean ± SD. Pearson chi-square test Yates’s correction or Fisher’s exact probability test was used to compare differences in the incidences and number of coughs. Patient age, height, weight, SBP, DBP, HR and SpO2 were compared between the groups using one-way analysis of variance (ANOVA) followed by a Turkey post hoc test.
Results
Of the four hundred and sixty enrolled patients, sixty patients were excluded from the study due to a history of asthma, upper respiratory tract infection in the previous 2 weeks or smoking. Therefore, 100 patients in each group were included and subjected to further statistical analysis (Figure 1).
Figure 1.
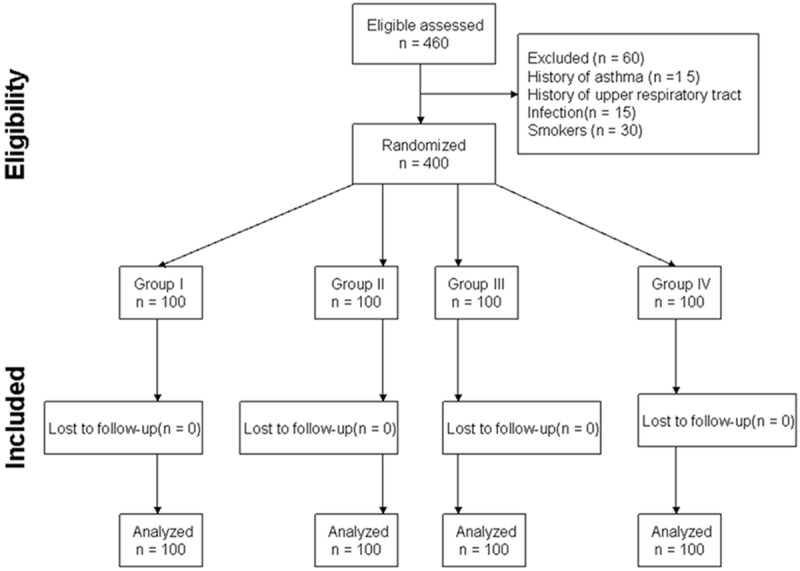
Flow diagram of subjects.
There were no significant differences in age, body weight, height among the four groups (Table 1).
Table 1.
Demographic data
| Group I (n = 100) | Group II (n = 100) | Group III (n = 100) | Group IV (n = 100) | P | |
|---|---|---|---|---|---|
| Age (years) | 45 ± 12 | 46 ± 13 | 43 ± 14 | 44 ± 14 | 0.49 |
| Sex (M/F) | 59/41 | 55/45 | 64/36 | 65/35 | 0.41 |
| Weight (kg) | 63 ± 9 | 61 ± 10 | 63 ± 8 | 65 ± 10 | 0.54 |
| Height (cm) | 162 ± 7 | 161 ± 8 | 164 ± 6 | 163 ± 7 | 0.83 |
| ASA I/II (n) | 60/40 | 65/35 | 62/38 | 64/36 | 0.89 |
Values are expressed as mean ± SD or numbers. ASA, American Society of Anesthesiololgists. No statistical differences were observed between groups.
The incidence of FIC was 40% in group I, 12% in group II, 4% in group III, and 0 in group IV (Table 2). Group I had significantly higher incidence of FIC than Groups II, III and IV (P < 0.05). Group IV had significantly lower incidence of FIC than Groups II (0% vs 12%; P = 0.0003) and III (0% vs 4%; P = 0.043). Group II had significantly higher incidence of FIC than Groups III (12% vs 4%; P = 0.037). Group I had significantly higher severity of FIC than Groups II, III and IV (P < 0.05). No severe cough was observed in Groups II, III and IV.
Table 2.
Fentanyl-induced cough and its severity in the four groups
| Group | I (n = 100) | II (n = 100) | III (n = 100) | IV (n = 100) | P | |
|---|---|---|---|---|---|---|
| Cough (n, %) | 40 (40) | 12 (12)*,†,# | 4 (4)*,† | 0 (0)* | ||
| Severity | Mild | 25 | 8 | 3 | 0 | <0.001 |
| Moderate | 10 | 4 | 1 | 0 | ||
| Severe | 5 | 0 | 0 | 0 | ||
Data are presented as numbers.
P<0.05 vs Group I;
P<0.05 vs Group IV;
P<0.05 vs Group III.
The severity of cough was graded: none (0), mild (1-2), moderate (3-4), or severe (5 or more).
There was no significant differences in the hemodynamic data (BP, HR, and SpO2) among the four groups before or after fentanyl administration (Table 3). None of the patients suffered from hypoxemia (SpO2 < 89%), desaturation, apnea, truncal rigidity, or other adverse effects after fentanyl injection.
Table 3.
Changes in vital signs after treatment in both groups
| Variables | T0 | T1 | P |
|---|---|---|---|
| SBP (mmHg) | |||
| I | 115 ± 15 | 114 ± 14 | 0.73 |
| II | 114 ± 17 | 113 ± 16 | 0.82 |
| III | 117 ± 16 | 115 ± 17 | 0.69 |
| IV | 116 ± 15 | 113 ± 15 | 0.59 |
| DBP (mmHg) | |||
| I | 69 ± 10 | 70 ± 11 | 0.81 |
| II | 70 ± 11 | 69 ± 10 | 0.76 |
| III | 71 ± 12 | 72 ± 11 | 0.87 |
| IV | 72 ± 11 | 73 ± 12 | 0.83 |
| HR (bpm) | |||
| I | 79 ± 11 | 78 ± 12 | 0.85 |
| II | 80 ± 10 | 79 ± 11 | 0.84 |
| III | 81 ± 12 | 80 ± 11 | 0.88 |
| IV | 82 ± 11 | 81 ± 12 | 0.81 |
| SpO2 (%) | |||
| I | 98.4 ± 1.5 | 98.3 ± 1.4 | 0.89 |
| II | 98.3 ± 1.4 | 98.4 ± 1.5 | 0.85 |
| III | 98.5 ± 1.2 | 98.6 ± 1.3 | 0.87 |
| IV | 98.3 ± 1.3 | 98.5 ± 1.4 | 0.84 |
SBP, Systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate; SpO2, pulse oximeter oxygen saturation; T0, Time. Before administration of dezocine or normal saline injection; T1, 2 min after fentanyl injection. No statistical differences were observed between groups.
Discussion
The study demonstrated that intravenous dezocine 0.025, 0.05, 0.1 mg/kg reduced the incidence of FIC during anesthetic induction, with the effect being most marked for dezocine 0.1 mg/kg.
Many physical methods have been reported to prevent FIC, including huffing maneuver [14], dilution of fentanyl [15], reduced speed of fentanyl injection. The prophylactic efficacy of these methods for preventing FIC remains controversial. A huffing maneuver [14] was reported as an effective way to prevent FIC. But if patients received midazolam or propofol during induction of general anesthesia, they cannot use this maneuver. Yu et al. [15] showed that if dilution of fentanyl was combined with a prolonged injection time, FIC could be eliminated. However, according to Schäpermeier and Hopf’s study [16], FIC does not depend on injection speed. Prolonged injection may not be convenient for fentanyl administration in some emergent circumstances.
Many pharmacological interventions have been reported to prevent FIC, including lidocaine [17,18], ephedrine [19], clonidine [20], betamethasone, dexamethasone [21], ketamine [22], propofol [23], dexmedetomidine [24]. But the use of the drugs in these earlier studies was unable to completely prevent FIC. Pretreatment with a high dose of lidocaine [17,18] might be avoided in patients susceptible to the arrhythmogenic effects of lidocaine. And its vasodilatory effect could augment the cardiovascular depression caused by induction agents. Intravenous ephedrine [19] before fentanyl injection may be contraindicated if patients are with coronary artery disease or moderate to severe hypertension or have a cerebral aneurysm. Pretreatment with clonidine [20] is also associated with respiratory depression, drowsiness, and severe hypotension. Betamethasone and dexamethasone [21] are steroids and should be used under strict conditions. Ketamine [22] is avoided in patients with hypertension, elevation of intracranial pressure, and intraocular pressure. Using high doses of propofol [23] can be associated with a high incidence of hypotension. Known side effects of pretreatment with dexmedetomidine include bradycardia and hypotension [24].
The analgesic effects of dezocine derive mainly from binding to the κ receptor, and dezocine also has the potential to attenuate the μ receptor-related effects. The analgesic effect of fentanyl derives mainly from binding to the μ receptor and less to the κ receptor. When combining fentanyl and dezocine, the analgesic effect from μ receptor decreases, but the analgesic effect from κ receptor increases. In our study, there was no significant difference in the hemodynamic data (BP, HR, and SpO2) among the four groups before or after fentanyl administration. Our results support that the attenuated analgesic effect at the μ receptor can be compensated by the increased analgesic effect at the κ receptor [25]. In our study the cuffs were used, so a transient increase of HR or BP in those patients who coughed might have been missed.
Previous study demonstrated that intravenous administration of 0.1 mg/kg dezocine 10 min before general anesthesia completely suppressed FIC during induction. In our study these four groups were given intravenous dezocine just before the fentanyl bolus, thereby removing the necessity to wait 10 min before iv fentanyl. So the practice in our study may be more convenient.
Although many mechanisms of FIC have been reported, the exact mechanism still remains unclear. Fentanyl could inhibit central sympathetic outflow and thereby activate the vagus nerve. So a possible cause of cough and reflex bronchoconstriction may be the enhancement of vagal activity [26,27]. Other possible mechanisms included a pulmonary chemoreflex mediated by rapidly adapting receptors (irritant receptors) or vagal C-fiber receptors located in proximity to pulmonary vessels [28], or stimulation of the irritant receptors in the upper pulmonary mucosa secondary to fentanyl-induced tracheal smooth muscle constriction [29]. Recently Kamei et al showed that fentanyl enhances the excitability of rapidly adapting receptors to cause cough via the enhancement of histamine release in the airways [30].
In our study intravenous dezocine 0.025, 0.05, 0.1 mg/kg effectively reduced the incidence of FIC during anesthetic induction, with the effect being most marked for dezocine 0.1 mg/kg. The suppressive effect was dose-dependent. Intravenous dose of dezocine 0.1 mg/kg completely suppressed FIC during induction. Dezocine activates κ receptors, which in turn antagonize fentanyl-activated μ receptors, thereby reducing cough. So the mechanism of decreased coughing incidence may be explained by the fact that when dezocine was given before fentanyl, some receptors responsible for cough would be occupied, blocking any potential interaction with fentanyl. Otherwise dezocine is an antitussive. These may be the reason why dezocine pretreatment in Group II, III, IV patients had a reduced incidence of cough compared with Group I.
Dezocine is not a well-known drug and has not being used in Western countries. Pentazocine is also a mixed agonist-antagonist opioid and has a similar profile of receptor effects. We speculated that pentazocine might substitute for dezocine.
Our study has its own limitations. Although our results provide convenient method to suppress FIC in clinical practice, we did not verify the exact mechanisms by which fentanyl induces cough and dezocine prevents FIC. Second, we did not record the effects of dezocine on post-operative analgesia, nausea and vomiting. Given 2-3 hr half life of dezocine, it will be expected to interfere with fentanyl analgesia. Data exist reported the increased incidence of vomiting with dezocine [31]. We speculated that dezocine may increase vomiting rate.
Although precise mechanism of how dezocine prevents FIC are not yet clear, our study showed that dezocine is a novel drug to prevent FIC and the suppressive effect is dose-dependent during general anesthesia induction. For prevention of FIC, the optimal dose of dezocine is 0.1 mg/kg.
Disclosure of conflict of interest
None.
References
- 1.Grell FL, Koons RA, Denson JS. Fentanyl in anesthesia: a report of 500 cases. Anesth Analg. 1970;49:523–532. [PubMed] [Google Scholar]
- 2.Bovill JG, Sebel PS, Stanley TH. Opioid analgesics in anesthesia: with special reference to their use in cardiovascular anesthesia. Anesthesiology. 1984;61:731–755. [PubMed] [Google Scholar]
- 3.Lin CS, Sun WZ, Chan WH, Lin CJ, Yeh HM, Mok MS. Intravenous lidocaine and ephedrine, but not propofol, suppress fentanyl-induced cough. Can J Anaesth. 2004;51:654–659. doi: 10.1007/BF03018421. [DOI] [PubMed] [Google Scholar]
- 4.Lin JA, Yeh CC, Lee MS, Wu CT, Lin SL, Wong CS. Prolonged injection time and light smoking decrease the incidence of fentanyl-induced cough. Anesth Analg. 2005;101:670–674. doi: 10.1213/01.ANE.0000159161.31276.DB. [DOI] [PubMed] [Google Scholar]
- 5.Du BX, Cao L, Zhao WL, Xu ZH, Song J, Shi XY. Pre-emptive small dose of fentanyl suppresses fentanyl-induced cough: a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2014;7:826–836. [PMC free article] [PubMed] [Google Scholar]
- 6.Uvelin A, Rakic G. Guidelines for prevention of fentanyl-induced cough. Acta Anaesthesiol Scand. 2009;53:1228–1229. doi: 10.1111/j.1399-6576.2009.02041.x. [DOI] [PubMed] [Google Scholar]
- 7.Tweed WA, Dakin D. Explosive coughing after bolus fentanyl injection. Anesth Analg. 2001;92:1442–1443. doi: 10.1097/00000539-200106000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Ambesh SP, Singh N, Srivastava K. Fentanyl induced coughing caused life-threatening airway obstruction in a patient with arteriovenous malformation of tongue and hypopharynx. Internet J Anesthesiol. 2009;20:7. [Google Scholar]
- 9.Kim JE, Min SK, Chae YJ, Lee YJ, Moon BK, Kim JY. Pharmacological and nonpharmacological prevention of fentanyl-induced cough: a meta-analysis. J Anesth. 2014;28:257–266. doi: 10.1007/s00540-013-1695-4. [DOI] [PubMed] [Google Scholar]
- 10.Downing JW, Brock-Utne JG, Barclay A, Schuegrnann IL. WY-16225 (dezocine), a new synthetic opiate agonistantagonist and potent analgesic: lower abdominal surgery. Br J Anaesth. 1981;53:59–64. doi: 10.1093/bja/53.1.59. [DOI] [PubMed] [Google Scholar]
- 11.Sun Q, Zhou W, Wu B, Ji MH, Peng YG. Dezocine: a novel drug to prevent fentanyl-induced cough during general anesthesia induction? J Anesth. 2012;26:470. doi: 10.1007/s00540-011-1318-x. [DOI] [PubMed] [Google Scholar]
- 12.O’Brien JJ, Benfield P. Dezocine: a preliminary review of its pharmacokinetic properties, and therapeutic efficacy. Drugs. 1989;38:226–248. doi: 10.2165/00003495-198938020-00005. [DOI] [PubMed] [Google Scholar]
- 13.Sun ZT, Yang CY, Cui Z, Zhang J, Han XP. Effect of intravenous dezocine on fentanyl-induced cough during general anesthesia induction: a double-blinded, prospective, randomized, controlled trial. J Anesth. 2011;25:860–863. doi: 10.1007/s00540-011-1237-x. [DOI] [PubMed] [Google Scholar]
- 14.Ambesh SP, Singh N, Gupta D, Singh PK, Singh U. A huffing manoeuvre, immediately before induction of anaesthesia, prevents fentanyl-induced coughing: a prospective, randomized, and controlled study. Br J Anaesth. 2010;104:40–43. doi: 10.1093/bja/aep333. [DOI] [PubMed] [Google Scholar]
- 15.Yu H, Yang XY, Zhang X, Li Q, Zhu T, Wang Y. The effect of dilution and prolonged injection time on fentanyl induced coughing. Anaesthesia. 2007;62:919–922. doi: 10.1111/j.1365-2044.2007.05147.x. [DOI] [PubMed] [Google Scholar]
- 16.Schäpermeier U, Hopf HB. Fentanyl-induced cough does not depend on injection speed: a randomized study. Acta Anaesthesiol Scand. 2008;52:1071–1075. doi: 10.1111/j.1399-6576.2008.01721.x. [DOI] [PubMed] [Google Scholar]
- 17.Pandey CK, Raza M, Ranjan R, Lakra A, Agarwal A, Singh U, Singh RB, Singh PK. Intravenous lidocaine suppresses fentanyl induced coughing: a double-blind, prospective, randomized placebo-controlled study. Anesth Analg. 2004;99:1696–1698. doi: 10.1213/01.ANE.0000136967.82197.82. [DOI] [PubMed] [Google Scholar]
- 18.Gecaj-Gashi A, Nikolova-Todorova Z, Ismaili-Jaha V, Gashi M. Intravenous lidocaine suppresses fentanyl-induced cough in Children. Cough. 2013;9:20–24. doi: 10.1186/1745-9974-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin CS, Sun WZ, CHan WH, LIn CJ, Yeh HM, Mok MS. Intravenous lidocaine and ephedrine, but not propofol, suppress fentanyl-induced cough. Can J Anaesth. 2005;51:654–659. doi: 10.1007/BF03018421. [DOI] [PubMed] [Google Scholar]
- 20.Hung KC. The possible mechanism of clonidine to suppress fentanyl-induced coughing. Acta Anaesthesiol Scand. 2009;53:1227–1228. doi: 10.1111/j.1399-6576.2009.02027.x. [DOI] [PubMed] [Google Scholar]
- 21.Lin JA, Chen FC, Lee MS, Horng HC, Cherng CH, Yeh CC, Wong CS. Intravenous dexamethasone pretreatment reduces fentanyl-induced cough. J Formos Med Assoc. 2007;106:649–655. doi: 10.1016/S0929-6646(08)60022-4. [DOI] [PubMed] [Google Scholar]
- 22.Yeh CC, Wu CT, Huh BK, Lee MS, Lin SL, Sheen MJ, Wong CS. Premedication with intravenous low-dose ketamine suppresses fentanyl-induced cough. J Clin Anesth. 2007;19:53–56. doi: 10.1016/j.jclinane.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 23.Tang Q, Qian Y, Zhang Q, Yang J, Wang Z. Effects of different priming doses of propofol on fentanyl-induced cough during anesthesia induction: a preliminary randomized controlled study. Ups J Med Sci. 2010;115:121–124. doi: 10.3109/03009730903291034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu J, Lu Y, Dong C, Zhu H, Xu R. Premedication with intravenous dexmedetomidine-midazolam suppresses fentanyl induced cough. Ir J Med Sci. 2012;181:517–520. doi: 10.1007/s11845-012-0807-8. [DOI] [PubMed] [Google Scholar]
- 25.Yeh YC, Lin TF, Lin FS, Wang YP, Lin CJ, Sun WZ. Combination of opioid agonist and agonist-antagonist patient-controlled analgesia requirement and adverse events among different-ratio morphine and nalbuphine admixtures for postoperative pain. Br J Anaesth. 2008;101:542–548. doi: 10.1093/bja/aen213. [DOI] [PubMed] [Google Scholar]
- 26.Lui PW, Hsing CH, Chu YC. Terbutaline inhalation suppresses fentanyl-induced coughing. Can J Anaesth. 1996;43:1216–1219. doi: 10.1007/BF03013427. [DOI] [PubMed] [Google Scholar]
- 27.Agarwal A, Azim A, Ambesh S, Bose N, Dhiraj S, Sahu D, Singh U. Salbutamol, beclomethasone or sodium cromoglycate suppress coughing induced by iv fentanyl. Can J Anaesth. 2003;50:297–300. doi: 10.1007/BF03017801. [DOI] [PubMed] [Google Scholar]
- 28.Bohrer H, Fleischer F, Werning P. Tussive effect of a fentanyl bolus administered through a central venous catheter. Anaesthesia. 1990;45:18–21. doi: 10.1111/j.1365-2044.1990.tb14496.x. [DOI] [PubMed] [Google Scholar]
- 29.Yasuda I, Hirano T, Yusa T, Satoh M. Tracheal constriction by morphine and by fentanyl in man. Anesthesiology. 1978;49:117–119. doi: 10.1097/00000542-197808000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Kamei J, Nakanishi Y, Asato M, Ikeda H. Fentanyl enhances the excitability of rapidly adapting receptors to cause cough via the enhancement of histamine release in the airways. Cough. 2013;9:3–8. doi: 10.1186/1745-9974-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ding Y, White PF. Comparative effects of ketorolac, dezocine, and fentanyl as adjuvants during outpatient anesthesia. Anesth Analg. 1992;75:56–71. doi: 10.1213/00000539-199210000-00018. [DOI] [PubMed] [Google Scholar]


