Abstract
Background: Transcutaneous electric acupoint stimulation (TEAS) at Jiaji acupuncture points has therapeutic potential for relieving viscera pain and opioid-related side effects. This prospective, randomized, triple-blinded, placebo-controlled trial was to investigate the efficacy of TEAS on abdominal pain after colonoscopy. Methods: Consecutive outpatients with American Society of Anesthesiologists (ASA) physical status I or II underwent selective colonoscopy were randomly assigned into two groups for either TEAS or sham pretreatment. The primary outcomes were the incidence of abdominal pain after colonoscopy. The secondary outcomes included the incidence of abdominal distension, postoperative nausea and vomiting (PONV), duration of PACU stay, and patient’s satisfaction and acceptance. Results: Among the 229 patients analyzed, fewer occurrence of post-procedural abdominal pain (11.4% vs 25.2%, P = 0.007) and distension (1.8% vs 7.8%, P = 0.032) were observed in TEAS group, when compared with the sham group. The duration of PACU stay was significant shortened in TEAS group (P < 0.001). Meanwhile, patients’ satisfaction score to medical service was higher (P < 0.001), and their acceptance to colonoscopy was improved (P = 0.011). Conclusion: Pretreatment with TEAS can reduce post-procedural discomfort, provide more efficient medical resources utilization, and improved patient’s satisfaction and colonoscopy acceptance.
Keywords: Transcutaneous electric acupoint stimulation, Jiaji points, colonoscopy, abdominal pain, distension
Introduction
Early colonoscopy screening is encouraged in prevention of development of colorectal cancer [1]. Abdominal pain or distension developed after colonoscopy has ever since been a common phenomenon in clinical practice [2,3]. Progression has been made by replacing the insufflated air with carbon dioxide, yet the overall prevalence of these abdominal discomfort after colonoscopy vary from 14.6% to 48.5% [4,5]. Though generally self-limited, these symptoms lead to post-procedural distress, which affect patients’ compliance and acceptance to colonoscopy screening, and may require additional costs and risks for this routine examination for colorectal cancer.
Most of the pharmacological interventions were restricted by their modest effectiveness or potential complications. For example, opioids and NSAIDs were the most commonly used analgesics. However, these medications can lead to cardiovascular or respiratory complications in certain groups of people [6,7]. To ensure the comfort and safety for our patients, a combination with complementary alternative approach has been recommended [8]. Among them, acupuncture and related technique was noted to have therapeutic potential for relieving viscera pain and opioid-related side effects, though the exact mechanism remained obscured [9].
TEAS applied transcutaneous electrical stimulation over acupuncture point, which was the most common type of acupuncture analgesia nowadays [10]. Previous study suggested that TEAS can effected on enhancing rectal perception threshold, alleviating abdominal pain, promoting intestinal peristalsis and improving defecation in patients with irritable bowel syndrome [11]. While the efficacy of TEAS to prevent abdominal pain or distension after colonoscopy need to be further clarified. Therefore, we conducted this prospective, randomized, triple-blinded, sham-controlled trial to identify whether outpatients pretreated with TEAS could result in favorable outcomes after colonoscopy procedure.
Methods and materials
Study subjects ss
This prospective, randomized, triple-blinded, placebo-controlled trial was conducted in accordance with the principles of the Declaration of Helsinki (Version 2010) [12] and the CONSORT statement (Version 2010) [13]. Consecutive patients aged 18 to 65, with ASA physical status I or II, asymptomatic, who scheduled for ambulatory colonoscopy between July 2014 and December 2014 at the Endoscopy Center of Fujian Provincial Hospital were recruited. The exclusion criteria included a history of narcotic analgesic abuse, prior use of TEAS device or acupuncture related treatment within 8 hours, injury or infection around the acupuncture site, dementia or other disease limiting cognition or communication, pregnancy and emergency. Written informed consent was obtained from all participants, and the study protocol was approved by the Ethics Committee of Fujian Provincial Hospital.
Randomization and blinding
Consecutive patients who met the inclusion criteria were randomly assigned to either TEAS or sham group, according to the sequential code generated by computer program (Random Number Generators, IBM, SPSS Statistic, Version 20.0). The group allocation numbers were then sealed in opaque envelopes. The envelopes were kept and distributed by an assistant. Each envelope for patients enrolled was opened by an experienced acupuncturist, who was independent to the study and in charge of the corresponding interventions. All participants, researchers, and the statistics analyzes were concealed from the implementation of intervention.
Intervention protocols
Pretreatment with TEAS was applied in the holding area before the induction by the experienced acupuncturist. Jiaji (EX-B2) points were located on both sides of the spinous column, 0.5 cun lateral to the lower border of each spinous process [14]. Among which, the ninth and twelfth thoracic vertebrae of Jiaji (EX-B2) points were identified and selected under the instruction of the traditional anatomical localization (Figure 1). A constant electrical stimulation for 30 min, with a dense-and-disperse frequency at 2/100 Hz was provided by a dual-channel electric stimulation apparatus (Han’s Acupoint Nerve Stimulator, HANS-200A, Nanjing Jisheng Medical Technology Co., Ltd., Nanjing, China). The optimal intensity was set to initiate visible slightly twitching of the surrounding muscle. While the sham group received identical electrodes placement without electrical output.
Figure 1.
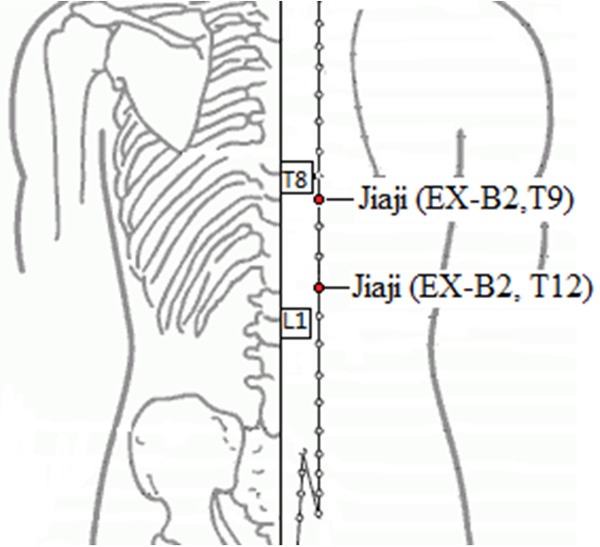
Location of Jiaji (EX-B2) points at T9 and T12.
Standardized management
All patients received standard monitoring, including electrocardiogram, noninvasive blood pressure and pulse oximetry. Anesthesia was induced and maintained with intravenous sufentanil 0.05 μg/kg and propofol titrated to the clinical requirements. The colonoscopy was performed by experienced endoscopic physicians, with video endoscope (OLYMPUS, PCF-H290I, EVIS LUCERA, video colonoscopy) and center supply carbon dioxide insufflation system. Patients were transferred to the recovery room after colonoscopy, and discharged when reached a score of 10 on the Aldrete scale [15].
Outcome measurements
Our primary outcomes were the incidence of the post-procedural abdominal pain. The most severe pain during their recovery was documented using a visual analogue scale (VAS), where 0 was no pain and 10 was unbearable pain. The secondary outcomes included incidence of abdominal distension and PONV, duration of PACU stay, patients’ satisfaction and acceptance. General assessments involved demographic characteristics (age, gender, weight, height, and body mass index), ASA physical status, duration of colonoscopy, anesthetic consumption. Patient’s satisfaction were evaluated by a 10-point numerical rating scale, where 10 was considered the best and 1 the worst assessment, and whether they would prefer an additional colonoscopy in the future.
Sample size estimation
Our sample size calculation for the two-tailed testing of the TEAS superiority hypothesis was based on the incidence of abdominal pain. The incidence of abdominal pain was 32% based on our pilot study. We accepted a 50% difference represents a clinically relevant difference. To yield a power of 80% with a significant level of 5%, a sample size of at least 111 subjects in each group was required. The sample size was then increased to 120 for each group to allow for possible dropouts.
Statistical analysis
Collected data were processed by the Statistical Package for the Social Sciences (IBM SPSS Statistics Version 20.0). Data in compliance with normal distribution was verified by Kolmogorov-Smirnov test. Numerical variables in normal distribution were described as mean (standard deviation [SD]) and analyzed by the independent Student’s t-test. Non-normal distributions were presented as median (interquartile range [IQR]) and evaluated using the Mann-Whitney U-test. Categorical variables were reported as the number (proportion) of patients and compared with the Chi-square test or Fisher’s exact test when appropriate. A probability value of less than 0.05 was considered to be statistically significant.
Results
We initially assessed 255 patients for eligibility to participate in this study (Figure 2). Of these, eight patients did not meet the inclusion criteria, seven patients declined to participate. The remaining 240 patients enrolled in the study and randomized to the treatment allocation. Six patients from the TEAS group and five patients from the sham group were later excluded because of protocol breach. A total of 229 patients completed the study, with 114 in TEAS group and 115 in sham group, which data were included in the analysis. Two groups were comparable in age, gender, ASA physical status, BMI, duration of procedures, and anesthetic consumptions, as described in Table 1 (P > 0.05).
Figure 2.
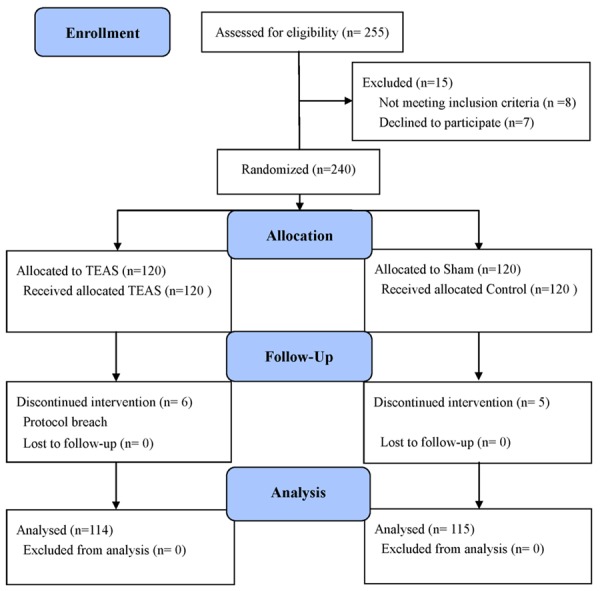
Consolidated Standards of Reporting Trials (CONSORT) flow diagram depicts the progress of subject through the trail. TEAS, transcutaneous electric acupoint stimulation.
Table 1.
Demographic characteristics and procedural parameters
| Group TEAS (n = 114) | Group Sham (n = 115) | P-value | |
|---|---|---|---|
| Age (years) | 49.2 (94) | 48.2 (96) | 0.402 |
| ASA (I/II) | 90/24 | 88/27 | 0.660 |
| Gender (Male/Female) | 66/48 | 62/53 | 0.545 |
| Height (cm) | 165.5 (78) | 165.9 (78) | 0.672 |
| Weight (kg) | 63.8 (111) | 64.1 (109) | 0.705 |
| BMI (kg/cm2) | 23.1 (31) | 23.2 (30) | 0.856 |
| Propofol (mg) | 157.9 (385) | 158.8 (361) | 0.864 |
| Procedure duration (min) | 10.7 (62) | 9.5 (52) | 0.097 |
Values were mean (standard deviation) or number (proportion). ASA, American Society of Anesthesiologists; BMI, body mass index; TEAS, transcutaneous electric acupoint stimulation.
Incidence of abdominal pain was significantly lower in TEAS group after colonoscopy (P = 0.007). As shown in Table 2, patients developed abdominal pain after colonoscopy were 13 (11.4%) and 29 (25.2%) in the TEAS group and the sham group, respectively. Meanwhile, the VAS score (median [IQR]) of the worst pain during recovery was lower in TEAS group (2 [2,3]), compared with the sham group (3 [2,5]) (P = 0.044).
Table 2.
Complications and satisfaction after colonoscopy
| Group TEAS (n = 114) | Group Sham (n = 115) | P-value | |
|---|---|---|---|
| Abdominal pain [n (%)] | 13 (11.4) | 29 (25.2) | 0.007 |
| Maximum pain score | 2 (2~3) | 3 (2~5) | 0.044 |
| Abdominal distension [n (%)] | 2 (1.8) | 9 (7.8) | 0.032 |
| Nausea or Vomiting [n (%)] | 1 (0.9) | 3 (2.6) | 0.318 |
| Duration of PACU stay (min) | 12 (10~14) | 14 (13~17) | < 0.001 |
| Satisfaction score | 8 (8~9) | 7 (6~8) | < 0.001 |
| Acceptance [n (%)] | 81 (71.1) | 63 (54.8) | 0.011 |
Values were number (proportion) or median (interquartile range). TEAS, transcutaneous electric acupoint stimulation; VAS, visual analogue scale.
Abdominal distension was less frequently happened in TEAS group than in the sham group (P = 0.032). Three patients in sham group and one patient in TEAS group reported slight nausea within a couple of minutes, whereas no statistical significance was observed between them (P = 0.318).
Patients’ discharge were faster in TEAS group (P < 0.001) when comparing with the sham group. In addition, their satisfaction scores were significantly higher (P < 0.001), acceptance to colonoscopy were improved (P = 0.011), simultaneously. No other adverse events occurred in both groups.
Discussions
In this study, a decrease in both frequency and intensity of post-procedural abdominal pain, abdominal distension were observed in outpatients pretreated with TEAS on T9 and T12 of Jiaji points (EX-B2) before colonoscopy. And the prevalence of nausea and vomiting presents a downward trend with the application of TEAS. Besides, pretreatment with TEAS shorten the duration of PACU stay, improve the overall satisfaction of our patients, and enhance their acceptance for colonoscopy in the study.
Acupuncture and related techniques can be complementary or alternative to conventional sedatives, antiemetic and analgesic for prophylaxis and treatment [9]. It has been adopted to facilitate clinical practice in several medical conditions approved by the World Health Organization (WHO) and Food and Drug Administration (FDA) [16]. Although the exact mechanism remains to be clarified, the applications of acupuncture has gain more preference than other complementary therapies like herbal or massage [17], and its therapeutic effects has been elaborated in related literatures [9]. Among all the acupuncture related techniques, TEAS has been widely applied in clinical settings with prominent advantages.
As a non-invasive, non-pharmaceutical, standardize treatment, TEAS is less painful or scary than manual practice, and requiring fewer techniques. By setting appropriate parameters, TEAS can produce the desired effects. We conducted a single session of 30 minutes pretreatment of TEAS under the instruction of the standard treatment [18] during routinely preparation before colonoscopy. With mixed frequency of 2/100 Hz and an individualized electric current intensity, TEAS was expected to achieve more favorable outcomes than the sham group [18-21].
Considered the specific points of treatment, T9 and T12 of Jiaji (EX-B2) points were chosen based on a combination of Zangfu-meridians theory in traditional Chinese medicine, and neurophysiologic foundation of Jigjig points in modern science [22]. Jiaji points were introduced in treatments of cardiovascular, digestive, urinary, and reproductive systems disorders as alternatives to Back-Shu points for security concerns in ancient clinical practice, however, they have proven to be the best substitutes for Back-Shu points [14]. Clinical observations thereafter, has confirmed their therapeutic effects on gastrointestinal dysfunctions [23,24]. Also demonstrated by randomized controlled trial that the curative effects of Jiaji points on relieving symptoms of viscera pain were certain [22].
Besides the inevitable discomfort caused by colonoscopy interventions [25], many known factors contribute to the high prevalence of abdominal pain after colonoscopy. Main reasons are followed, patients with poor bowel preparation, previous history of lower abdominal or pelvic surgery, less experienced examiner, inadequate sedation and analgesic etc. [26]. By observing the same group of examiners who performed the colonoscopy diagnosis and treatment, the interference of different examiners was minimized in our study. Without the implementation of TEAS, the incidence of post-procedural abdominal pain was about 25%, which is at an average level given by previous studies [4,5,27,28]. When applied with TEAS pretreatment, the incidence was significantly decreased by 60%, which suggested that TEAS can exert preventive effect for the prevalence of abdominal pain after colonoscopy. While large scale studies were required to confirm these findings.
To our knowledge, limited documents regarding the application of TEAS in ambulatory colonoscopy can be retrieved. Also, studies investigating the role of Jiaji acupuncture point in alleviating viscera pain were rare. Our study was designed in consistence with some high-quality research to validated that pretreated with TEAS can reduce the incidence and severity of abdominal pain after colonoscopy. In addition, faster recovery and rapid discharge are potential benefits for our patients to resume work and normal life after procedure.
This study has some limitations. Firstly, to perform standard sedation during colonoscopy [29] and ensure patients’ comfort and safety, sufentanil was adopted in our study. Though same dosage was administered in both groups, this medication may have masked the putative efficacy of TEAS. Secondly, we merely recruited the asymptomatic patients in this study; our results may not be generalizable to more extensive outpatients. In addition, due to different culture and education, the changes in validity and reliability pain score should take into consideration when interpreting the results.
In conclusion, TEAS pretreatment reduce the incidence and intensity of post-procedural discomfort after ambulatory colonoscopy. As preparation before colonoscopy, TEAS enhances patient’s satisfaction to the medical service quality, and improve their compliance to colonoscopy screening. The application of TEAS saves medical resources by accelerating discharge from outpatient department and diminishing extra costs for the undesirable effects. With all benefits mentioned above, we recommended that TEAS at Jiaji points can be used as complementary medical interventions in patients with colonoscopy.
Acknowledgements
This study was supported in part by Social Development of Key Projects in Fujian Province (2012Y0012) and Natural Science Foundation of Fujian Province (2015J01373). We would like to thank Dr. Xiaoling Zheng and Dr. Wanyin Deng (Endoscopy Center of Fujian Provincial Hospital, Fuzhou, China), for their support and cooperation. We also appreciate our patients for their participation. And feel grateful to whom offering help, suggestion or guidance.
Disclosure of conflict of interest
None.
References
- 1.Scott BB. Gastroenterology in the Trent Region in 1992 and a review of changes since 1975. Gut. 1995;36:468–472. doi: 10.1136/gut.36.3.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schutz SM, Lee JG, Schmitt CM, Almon M, Baillie J. Clues to patient dissatisfaction with conscious sedation for colonoscopy. Am J Gastroenterol. 1994;89:1476–1479. [PubMed] [Google Scholar]
- 3.Kim WH, Cho YJ, Park JY, Min PK, Kang JK, Park IS. Factors affecting insertion time and patient discomfort during colonoscopy. Gastrointest Endosc. 2000;52:600–605. doi: 10.1067/mge.2000.109802. [DOI] [PubMed] [Google Scholar]
- 4.Baudet JS, Diaz-Bethencourt D, Aviles J, Aguirre-Jaime A. Minor adverse events of colonoscopy on ambulatory patients: the impact of moderate sedation. Eur J Gastroenterol Hepatol. 2009;21:656–661. doi: 10.1097/MEG.0b013e328314b7e3. [DOI] [PubMed] [Google Scholar]
- 5.Lee YC, Wang HP, Chiu HM, Lin CP, Huang SP, Lai YP, Wu MS, Chen MF, Lin JT. Factors determining post-colonoscopy abdominal pain: prospective study of screening colonoscopy in 1000 subjects. J Gastroenterol Hepatol. 2006;21:1575–1580. doi: 10.1111/j.1440-1746.2006.04145.x. [DOI] [PubMed] [Google Scholar]
- 6.Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89:409–423. [PubMed] [Google Scholar]
- 7.Schug SA, Torrie JJ. Safety assessment of postoperative pain management by an acute pain service. Pain. 1993;55:387–391. doi: 10.1016/0304-3959(93)90016-I. [DOI] [PubMed] [Google Scholar]
- 8.Wang SM, Peloquin C, Kain ZN. The use of auricular acupuncture to reduce preoperative anxiety. Anesth Analg. 2001;93:1178–1180. doi: 10.1097/00000539-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Chernyak GV, Sessler DI. Perioperative acupuncture and related techniques. Anesthesiology. 2005;102:1031–1078. doi: 10.1097/00000542-200505000-00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han JS, Terenius L. Neurochemical basis of acupuncture analgesia. Ann Rev Pharmacol Toxicol. 1982;22:193–220. doi: 10.1146/annurev.pa.22.040182.001205. [DOI] [PubMed] [Google Scholar]
- 11.Xiao WB, Liu YL. Rectal hypersensitivity reduced by acupoint TENS in patients with diarrhea-predominant irritable bowel syndrome: a pilot study. Dig Dis Sci. 2004;49:312–319. doi: 10.1023/b:ddas.0000017458.55517.33. [DOI] [PubMed] [Google Scholar]
- 12.Goodyear MD, Krleza-Jeric K, Lemmens T. The declaration of Helsinki. BMJ. 2007;335:624–5. doi: 10.1136/bmj.39339.610000.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;1:100–7. doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cabioglu MT, Arslan G. Neurophysiologic basis of Back-Shu and Huatuo-Jiaji points. Am J Chin Med. 2008;36:473–479. doi: 10.1142/S0192415X08005916. [DOI] [PubMed] [Google Scholar]
- 15.Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilopoulos G. Risk of perforation from a colonoscopy in adults: a large population-based study. Gastrointest Endosc. 2009;69:654–664. doi: 10.1016/j.gie.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Eskinazi DP, Jobst KA. National Institutes of Health Office of Alternative Medicine-Food and Drug Administration Workshop on Acupuncture. J Altern Complement Med. 1996;2:3–6. doi: 10.1089/acm.1996.2.3. [DOI] [PubMed] [Google Scholar]
- 17.Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158:2303–2310. doi: 10.1001/archinte.158.21.2303. [DOI] [PubMed] [Google Scholar]
- 18.Carneiro N, Shih-Min L. Acupuncture technique. Lancet. 1989;345:1577. doi: 10.1016/s0140-6736(95)91128-6. [DOI] [PubMed] [Google Scholar]
- 19.Leung WW, Jones AY, Ng SS, Wong CY, Lee JF. Acupuncture transcutaneous electrical nerve stimulation reduces discomfort associated with barostat-induced rectal distension:a randomized-controlled study. World J Gastroenterol. 2013;21:381–8. doi: 10.3748/wjg.v19.i3.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamza MA, White PF, Ahmed HE, Ghoname EA. Effect of the frequency of transcutaneous electrical nerve stimulation on the postoperative opioid analgesic requirement and recovery profile. Anesthesiology. 1999;91:1232–1238. doi: 10.1097/00000542-199911000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Q, Gao Z, Wang H, Ma L, Guo F, Zhong H, Xiong L, Wang Q. The effect of pre-treatment with transcutaneous electrical acupoint stimulation on the quality of recovery after ambulatory breast surgery: a prospective, randomised controlled trial. Anaesthesia. 2014;69:832–839. doi: 10.1111/anae.12639. [DOI] [PubMed] [Google Scholar]
- 22.Chen H, Liu TY, Kuai L, Zhu J, Wu CJ, Liu LM. Electroacupuncture treatment for pancreatic cancer pain: a randomized controlled trial. Pancreatology. 2013;13:594–597. doi: 10.1016/j.pan.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Xing LY, Qu LX, Chen H, Gao S. Clinical observation on acupressure at Jiaji points for irritable bowel syndrome. Zhongguo Zhen Jiu. 2013;33:739–742. [PubMed] [Google Scholar]
- 24.Yue Z, Zhenhui Y. Ulcerative colitis treated by acupuncture at Jiaji points (EX-B2) and tapping with plum-blossom needle at Sanjiaoshu (BL22) and Dachangshu (BL 25)-a report of 43 cases. J Tradit Chin Med. 2005;25:83–84. [PubMed] [Google Scholar]
- 25.Bell GD, Charlton JE. Colonoscopy-is sedation necessary and is there any role for intravenous propofol? Endoscopy. 2000;32:264–267. doi: 10.1055/s-2000-97. [DOI] [PubMed] [Google Scholar]
- 26.Fisher DA, Maple JT, Ben-Menachem T, Cash BD, Decker GA, Early DS, Evans JA, Fanelli RD, Fukami N, Hwang JH, Jain R, Jue TL, Khan KM, Malpas PM, Sharaf RN, Shergill AK, Dominitz JA. Complications of colonoscopy. Gastrointest Endosc. 2011;74:745–752. doi: 10.1016/j.gie.2011.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Ko CW, Riffle S, Shapiro JA, Saunders MD, Lee SD, Tung BY, Kuver R, Larson AM, Kowdley KV, Kimmey MB. Incidence of minor complications and time lost from normal activities after screening or surveillance colonoscopy. Gastrointest Endos. 2007;65:648–656. doi: 10.1016/j.gie.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005;48:1295–1300. doi: 10.1007/s10350-004-0940-1. [DOI] [PubMed] [Google Scholar]
- 29.Li Z, Deng X, Zhang S, Liu J. Chinese gastrointestinal endoscopy sedation anesthesia expert consensus. Chinese Journal of Practical Internal Medicine. 2014;58:756–764. [Google Scholar]


