Abstract
Background and objectives: Numerous clinical studies have evaluated the potential benefits of DGHL for symptomatic hemorrhoids, particularly with regard to the perioperative parameters. However, the exact value of Doppler-assisted localization of vessels in hemorrhoid operations is still not clear. The aim of this study is to systematically analyze the randomized controlled trials on the effectiveness of DGHL and HL without Doppler guidance or other procedures for HD by using the principles of meta-analysis. Materials and methods: Relevant RCTs which assessed DGHL as the primary procedure and reported clinical outcomes as primary end-points were selected from Pubmed database, Embase database and the Cochrane library. Mean difference (MD) was used to represent effect-quantity for continuous variable results, while Odds ratio (RR) was used to represent effect-quantity for discontinuous variable results. Statistical analysis was performed by RevMan 5.0 and STATA 12.0 software. Results: Five RCTs with a total of 388 patients were analyzed systematically. The main results showed that DGHL and HL without Doppler guidance or other procedures are equally effective in terms of treatment success rate (RR = 0.89, 95% CI 0.73-1.09, P = 0.27), operation time (MD = 11.41, 95% CI -9.26-32.09, P = 0.28), postoperative complications (RR = 0.89, 95% CI 0.62-1.28, P = 0.53), postoperative pain (MD = -1.01, 95% CI -2.27-0.26, P = 0.12) and incidence of HD recurrence (RR = 1.07, 95% CI 0.83-1.39, P = 0.60). Conclusion: Our findings suggest that DGHL may not have evident superiority for the management of HD in terms treatment success rate, operation time, postoperative complications, postoperative pain and incidence of HD recurrence. However, further large scale randomized and multicentre studies are needed to confirm these findings.
Keywords: Haemorrhoid, Doppler-guided, dearterialization, artery ligation, meta-analysis
Introduction
Hemorrhoidal disease (HD) is one of the most commonly occurring proctologic diseases, the symptoms related to which are usually bothersome and difficult to attenuate. As patients are often reluctant to undergo painful treatments for benign conditions, management of HD has evolved to develop more effective but less invasive treatment during the last century. One of these new techniques is Doppler-guided hemorrhoidal artery ligation (DGHL) [1]. First described by Morinaga in 1995 [2], the procedure uses a specially designed proctoscope coupled with a Doppler transducer for identification and ligation of haemorrhoidal arteries [3]. Ligation of these arteries disrupts the inflow of blood to the haemorrhoidal venous plexuses and subsequently results in shrinkage of the pathological tissue and subsequent symptom relief [2]. Numerous clinical studies including five randomized controlled trials (RCTs) [4-8] have evaluated the potential benefits of DGHL for symptomatic hemorrhoids, particularly with regard to the perioperative parameters such as postoperative pain, relief of symptoms and recurrence rate. However, the exact value of Doppler-assisted localization of vessels in hemorrhoid operations is still not clear. The aim of this study is to systematically analyze the randomized controlled trials on the effectiveness of DGHL and HL without Doppler guidance or other procedures for HD by using the principles of meta-analysis.
Materials and methods
Study identification and selection
A systematic literature search in Pubmed database, Embase database and the Cochrane library (updated to October 1, 2014) were carried out to identify studies involving the effect of DGHL as the primary procedure for the management of HD of any grade. The search terms were as follows: Doppler, dearterialization, artery ligation and hemorrhoid. The languages were limited to English. A manual search of the references of the retrieved articles was conducted subsequently.
Relevant RCTs which assessed DGHL as the primary procedure and reported clinical outcomes as primary end-points were included. Specific exclusion criteria comprised: (1) not an intervention study with an appropriate comparison group; (2) reviews, commentaries, letters and editorials with no further information from authors; and (3) not an article translated into English. Primary end-points were recurrence and postoperative pain. Secondary end-points were operation time, postoperative complications and treatment success rate [9]. Reviews, commentaries, letters and editorials as well as articles not translated into English were excluded. Two authors independently screened the articles for inclusion. Disagreements between the reviewers were resolved by consensus.
Data extraction and quality evaluation
Two reviewers extracted all data independently according to the inclusion, and reached a consensus on all items. In case of disagreement, a third author would assess these articles. The methodological quality of each study was assessed using the bias risk assessment method about RCT in The Cochrane Collaboration System Evaluation Handbook 5.0.2. [10], which consists of 6 items: (1) method of randomized distribution; (2) concealment of the distribution plan; (3) blinding method for the targets of research, practitioners of the therapeutic plan, and those measuring outcomes; (4) wholeness of consequent data; (5) result of research into selective reports; and (6) other sources of deviation. For each item, matching means low bias, and mismatching means high risk; if information reported in the literature is not enough to make a definite judgment, the item was defined as indeterminate, indicating moderate risk.
Statistical analysis
Meta-analysis was performed using RevMan 5.0 software supplied by The Cochrane collaboration and STATA 12.0 (StataCorp LP, College Station, TX). Heterogeneity was evaluated by a χ2 based Q statistic and was considered statistically significant when P < 0.10. When the p value was < 0.10, combined analysis was performed with the random effect model; otherwise, the fixed effect model should be used. Mean difference (MD) was used to represent effect-quantity for continuous variable results, while Odds ratio (RR) was used to represent effect-quantity for discontinuous variable results. Publication bias was tested by Egger’s funnel plots. Funnel plot symmetry was further assessed using Egger’s linear regression method. In a sensitivity analysis, 0.5 was added to each cell frequency for trials in which no event occurred in either the treatment or control group, according to the method recommended by Deeks et al. [11].
Results
Studies selection process and characteristics
The article selection process used in this study is summarized in Figure 1. A total of five RCTs [4-8] published between 2009 and 2012 met the inclusion criteria and were included in the present meta-analysis. Overall, the five selected studies, which originated from four countries (Hungary, Netherlands, India and Italy), included 388 individuals. Table 1 shows the characteristics of studies enrolled. Variables used to achieve a combined outcome are given in Table 2.
Figure 1.
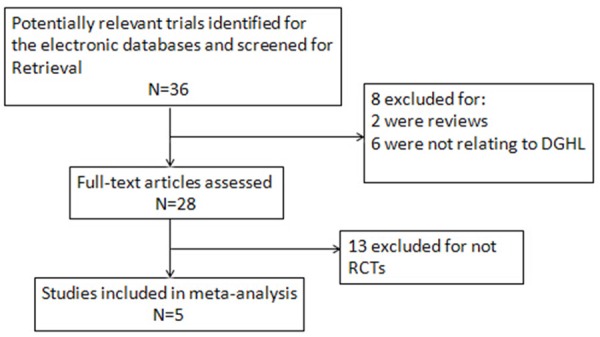
Flow chart of selection process for eligible articles.
Table 1.
Characteristics of studies enrolled
| Author, year | Country | Patients (n) | Age at DGHL (mean ± SD) | HD grade at DGHL | Compared procedure | Age of control (mean ± SD) | HD grade of control |
|---|---|---|---|---|---|---|---|
| Bursics A, et al. 2004 | Hungary | 60 | 47.4 ± 15 | I/II/III/IV | MMH | 46.4 ± 13 | II/III/IV |
| Festen S, et al. 2009 | Netherlands | 41 | Mean 39 | III/IV | PPH | Mean 35 | III/IV |
| Gupta PJ, et al. 2011 | India | 45 | 44 ± 11.2 | III | HL without Doppler guidance | 47.4 ± 10.4 | III |
| Infantino A, et al. 2012 | Italy | 169 | 47.6 ± 11.9 | III | PPH | 46.2 ± 11.5 | III |
| Shuurman JP, et al. 2012 | Netherlands | 73 | 50 ± 13.0 | II/III | HL without Doppler guidance | 51 ± 13.7 | II/III |
MMH, Milligan-Morgan haemorrhoidectomy; PPH, procedure for prolapse and haemorrhoids; HL, haemorrhoidal artery ligation.
Table 2.
Data of outcome variables extracted from included randomized trials (DGHL/Control)
| Trial | Patients (DGHL/Control) | Treatment success (DGHL/Control) | Operative time (min) (DGHL/Control) | Complications (DGHL/Control) | Pain VAS score (DGHL/Control) | Recurrence (DGHL/Control) |
|---|---|---|---|---|---|---|
| Bursics A, et al | 30/30 | 25/26 | Not reported | 6/5 | Not reported | Not reported |
| Festen S, et al | 23/18 | 18/15 | Not reported | 2/3 | 3.1 ± 0.1/5.1 ± 0.1 | 5/5 |
| Gupta PJ, et al | 22/23 | Not reported | 31 ± 5.4/9 ± 6.3 | 4/4 | Not reported | 4/3 |
| Infantino A, et al | 85/84 | Not reported | 26.6 ± 8.4/25.7 ± 7.8 | 26/33 | 2.0 ± 0.5/2.4 ± 0.5 | 12/6 |
| Shuurman JP, et al | 38/35 | 8/11 | Not reported | 3/0 | 3.9 ± 1.0/4.5 ± 1.0 | 30/30 |
Quality of included RCTs
Most of the included RCTs showed relatively high quality. All trials were conducted in a randomized fashion, among which one used a digital method for randomization [7]. Two trials used a distribution concealing method [6,7]. One study used a single blinding method for evaluators [8], but the remainder did not mention the blinding method. No study provided detailed baseline data, but only mentioned baseline conditions and comparability. The risk of bias in the included RCTs is shown in Figure 2.
Figure 2.
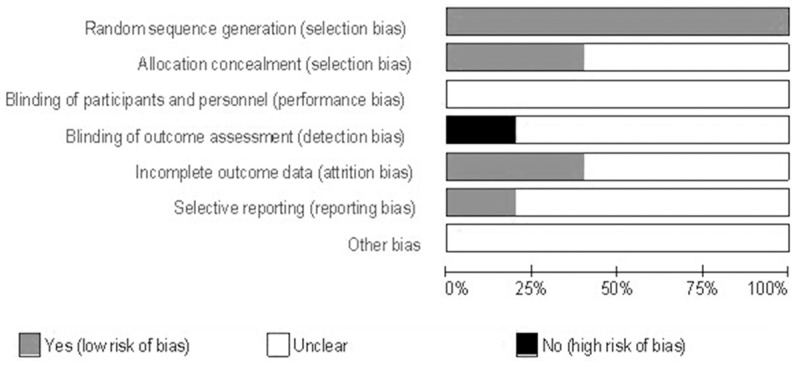
Analysis of bias in the included studies.
Quantitative data synthesis
Treatment success rate
Three trials [4,5,8] contributed to the combined calculation of this outcome. Meta-analysis results demonstrated that there was no significant difference in the treatment success rate between DGHL group and control group (RR = 0.89, 95% CI 0.73-1.09, P = 0.27) (Figure 3).
Figure 3.
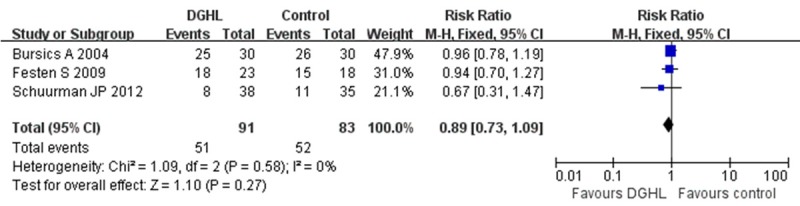
Meta-analysis forest graph about treatment success rate of DGHL and other procedures for HD.
Operative time
Data in two studies [6,7] were combined by meta-analysis to compare this outcome in the two groups. The operation time for DGHL was longer compared to control group, though the difference was not statistically significant (MD = 11.41, 95% CI-9.26-32.09, P = 0.28) (Figure 4).
Figure 4.
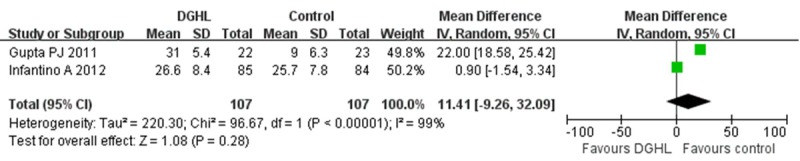
Meta-analysis forest graph about operative time of DGHL and other procedures for HD.
Postoperative complications
Data in all five studies were compared with meta-analysis about the frequency of postoperative complications in two groups. DGHL was associated with fewer postoperative complications compared to the control group, but the difference was not statistically significant (RR = 0.89, 95% CI 0.62-1.28, P = 0.53) (Figure 5).
Figure 5.
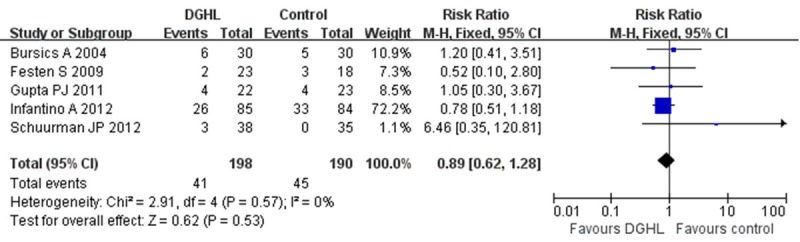
Meta-analysis forest graph about postoperative complications of DGHL and other procedures for HD.
Postoperative pain
Data in three trials [5,7,8] were combined to calculate overall VAS scores in the two groups. Meta-analysis results showed that postoperative pain following DGHL was lower compared to the control group, though the difference was not statistically significant (MD = -1.01, 95% CI-2.27-0.26, P = 0.12) (Figure 6).
Figure 6.
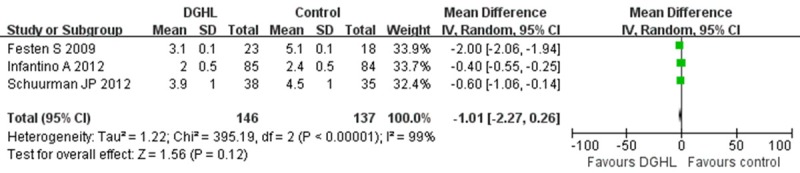
Meta-analysis forest graph about postoperative pain of DGHL and other procedures for HD.
Recurrence of haemorrhoids
Four trials [5-8] contributed to the combined calculation of this outcome. The results demonstrated that there was no significant difference in the recurrence rate between DGHL group and control group (RR = 1.07, 95% CI 0.83-1.39, P = 0.60) (Figure 7).
Figure 7.
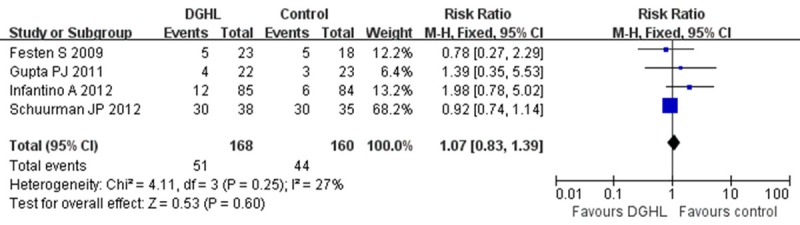
Meta-analysis forest graph about recurrence rate of DGHL and other procedures for HD.
Publication bias
The publication bias was evaluated using an Egger’s funnel plot about the recurrence rate of DGHL versus the control, which showed no significant evidence of asymmetry (Figure 8). We also performed an Egger’s test to quantify the publication bias, and the P value was 0.535, suggesting no significant bias of the analysis.
Figure 8.
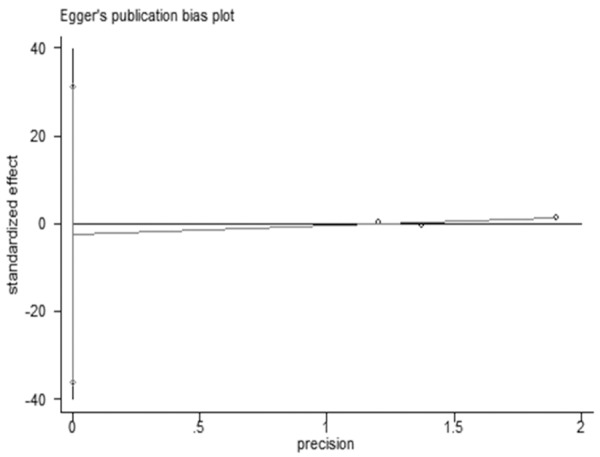
Overall analysis of publication bias about the recurrence rate of DGHL versus the control.
Discussion
Doppler-guided haemorrhoidal artery ligation (DGHL) utilizes a specialized anoscope incorporating a Doppler ultrasound probe to allow identification and targeted ligation of haemorrhoidal arteries [12], which can be performed in day care under epidural anaesthesia [13]. Several studies evaluating the efficacy of DGHL in approximately 1000 patients have been published, but the results were controversial. Recently, a systemic review by PH Pucher, et al. suggests that DGHL is safe and efficacious with a low level of postoperative pain [14]. However, studies included were of poor overall quality and no synthetically quantitative data was provided. So the present meta-analysis was performed to systematically estimate the therapeutic effect and security of DGHL for management of HD. The included RCTs compared DGHL vs. HL without Doppler guidance or other procedures for HD.
In the current study, we analyzed five RCTs with a total of 198 patients who underwent DGHL, and 190 patients having HL without Doppler guidance or other procedures for HD. The main results showed that although DGHL is associated with lower treatment success, longer operation time, less postoperative pain, less postoperative complications and higher recurrence rate, the differences are not significant, indicating that DGHL and HL without Doppler guidance or other procedures are equally effective in terms of treatment success rate, operation time, postoperative complications, postoperative pain and incidence of HD recurrence. These results are in consistent with the systemic review performed by PH Pucher, et al [14]. Nevertheless, future trials should also include cost/effectiveness analysis to evaluate the effectiveness of different techniques for HD comprehensively. It has been reported that over 61000 haemorrhoid procedures are carried out in the NHS in the UK every year [15], which is associated with significant cost including the cost of the disposable equipment that is approximately £500 per operation for PPH, while for DGHL the cost has been estimated at £420 per operation [7], and for MMH that is much lower. Therefore both clinical and economic factors must be taken into consideration when establishing the optimum treatment for HD.
There are several points that should be addressed in our meta-analysis. First, the small sample-sized studies in this review may not have been large enough to identify the small differences between two groups. Second, there might be significant differences about inclusion criteria (e.g. grade of haemorrhoids) among included trials. Third, differences also exist among the definitions of “treatment success rate” and “measurement scales for postoperative pain” in different trials. Fourth, because of the limited number of included trials, we didn’t perform subgroup analysis based on HD grade, so it is not clear that for which HD grade DGHL is more safe and effective. According to previous studies, DGHL for grade IV haemorrhoids recurrence was as high as 50-60% [4,16], so this treatment may not at present be recommended as treatment for this stage of disease. Lastly, although the included RCTs were conducted in a randomized fashion, a specific description of the randomization process (especially distribution-concealing measures and information on practitioners) was lacking, which may bring higher degree of bias. Thereby, these points should be considered when explaining the result of this meta-analysis.
In conclusion, this meta-analysis explored the role of DGHL in the management of HD, and provided some evidence to help colorectal surgeons in decision making about the type and technique of surgical intervention for the management of HD. More randomized and multicentre studies should be performed to evaluate whether Doppler guidance in haemorrhoidal artery ligation is really necessary or not. Additional trials on the potential effects of DGHL on HD at different grades are also needed.
Acknowledgements
We thank all authors of primary studies included in our meta-analyses.
Disclosure of conflict of interest
None.
References
- 1.Giordano P, Overton J, Madeddu F, Zaman S, Gravante G. Transanal hemorrhoidal dearterialization: a systematic review. Dis Colon Rectum. 2009;52:1665–1671. doi: 10.1007/DCR.0b013e3181af50f4. [DOI] [PubMed] [Google Scholar]
- 2.Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flow meter. Am J Gastroenterol. 1995;90:610–613. [PubMed] [Google Scholar]
- 3.Scheyer M, Antonietti E, Rollinger G, Mall H, Arnold S. Doppler-guided hemorrhoidal artery ligation. Am J Surg. 2006;191:89–93. doi: 10.1016/j.amjsurg.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Bursics A, Morvay K, Kupcsulik P, Flautner L. Comparison of early and 1-year follow-up results of conventional hemorrhoidectomy and hemorrhoid artery ligation: a randomized study. Int J Colorectal Dis. 2004;19:176–180. doi: 10.1007/s00384-003-0517-9. [DOI] [PubMed] [Google Scholar]
- 5.Festen S, Van Hoogstraten MJ, Van Geloven AA, Gerhards MF. Treatment of grade III and IV haemorrhoidal disease with PPH or THD. A randomized trial on postoperative complications and short-term results. Int J Colorectal Dis. 2009;24:1401–1405. doi: 10.1007/s00384-009-0803-2. [DOI] [PubMed] [Google Scholar]
- 6.Gupta PJ, Kalaskar S, Taori S, Heda PS. Doppler-guided hemorrhoidal artery ligation does not offer any advantage over suture ligation of grade 3 symptomatic hemorrhoids. Tech Coloproctol. 2011;15:439–444. doi: 10.1007/s10151-011-0780-7. [DOI] [PubMed] [Google Scholar]
- 7.Infantino A, Altomare DF, Bottini C, Bonanno M, Mancini S THD group of the SICCR (Italian Society of Colorectal Surgery) Yalti T, Giamundo P, Hoch J, El Gaddal A, Pagano C. Prospective randomized multicentre study comparing stapler haemorrhoidopexy with Doppler-guided transanal haemorrhoid dearterialization for third-degree haemorrhoids. Colorectal Dis. 2012;14:205–11. doi: 10.1111/j.1463-1318.2011.02628.x. [DOI] [PubMed] [Google Scholar]
- 8.Schuurman JP, Rinkes I, Go P. Hemorrhoidal artery ligation procedure with or without doppler transducer in grade II and III hemorrhoidal disease. Ann Surg. 2012;255:840–845. doi: 10.1097/SLA.0b013e31824e2bb5. [DOI] [PubMed] [Google Scholar]
- 9.Sajid MS, Parampalli U, Whitehouse P, Sains P, McFall MR, Baig MK. A systematic review comparing transanal haemorrhoidal de-arterialisation to stapled haemorrhoidopexy in the management of haemorrhoidal disease. Tech Coloproctol. 2012;16:1–8. doi: 10.1007/s10151-011-0796-z. [DOI] [PubMed] [Google Scholar]
- 10.Higgins JPT, Altman DG, Sterne JAC. Chapter 8: assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. Available from www.cochrane-handbook.org. [Google Scholar]
- 11.Deeks JJ, Altman DG, Bradburn MJ. Systemic reviews in health care: metaanalysis in context. 2nd edition. London: BMJ Publication group; Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. [Google Scholar]
- 12.Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol. 1995;90:610–613. [PubMed] [Google Scholar]
- 13.Ratto C, de Parades V. Doppler-guided ligation of hemorrhoidal arteries with mucopexy: A technique for the future. J Visc Surg. 2015;152(Suppl):S15–21. doi: 10.1016/j.jviscsurg.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Pucher PH, Sodergren MH, Lord AC, Darzi A, Ziprin P. Clinical outcome following Doppler-guided haemorrhoidal artery ligation: a systematic review. Colorectal Dis. 2013;15:e284–94. doi: 10.1111/codi.12205. [DOI] [PubMed] [Google Scholar]
- 15.Hospital Episode Statistics 2010-11. http://www.heson line.nhs.uk/Ease/servlet/ContentServer? siteID = 1937&cate goryID = 203.
- 16.Spyridakis M, Christodoulidis G, Symeonidis D Dimas D, Diamantis A, Polychronopoulou E, Tepetes K. Outcomes of Doppler-guided hemorrhoid artery ligation: analysis of 90 consecutive patients. Tech Coloproctol. 2011;15(Suppl 1):S21–4. doi: 10.1007/s10151-011-0727-z. [DOI] [PubMed] [Google Scholar]


