Abstract
Background: The aim of this study was to explore the correlation of gene polymorphisms of human leukocyte antigen-DQB1 (HLA-DQB1) with the infection outcome and replication status of hepatitis B virus (HBV) positive patients in the Xinjiang Uygur population in China. Methods: 110 cases of chronic hepatitis B (CHB) of Xinjiang Uygur were examined clinically, which were named as the CHB group; 100 cases carrying chronic HBV (ASC) served as ASC group; 80 cases of self-limited HBV infection (RHBS) were recorded as RHBS group. Genotypes of HLA-DQB1 were detected by sequence specific primer-polymerase chain reaction (PCR-SSP) method, and the differences of gene frequency among groups were also compared. The distribution frequencies of the HLA-DQB1 gene under different replication states of HBV were compared. Results: The distribution frequency of DQB1*0201 in the RHBS group was higher than that of the ASC group (18.75%, 10.50%, χ2 = 5.959, P < 0.05, OR = 2.257). The distribution frequency of DQB1*0201 in the CHB group was higher than that of the ASC group (17.73%, 10.50%, χ2 = 5.363, P < 0.05, OR = 2.066). The distribution frequency of DQB1*0301 in the CHB group was higher than that of the ASC group (26.82%, 16.50%, χ2 = 9.062, P < 0.05, OR = 2.349). The distribution frequency of DQB1*0303 in the CHB group was lower than that of the ASC group (19.55%, 31.00%, χ2 = 10.996, P < 0.05, OR = 0.393). There was no statistically significant difference in the allele frequencies among all other groups. The distribution frequency of DQB1*0201 in the low replication group was higher than that of the high replication group (17.08%, 10.56%, χ2 = 4.295, P < 0.05, OR = 1.939). Conclusion: HLA-DQB1*0201 is a HBV resistance gene in Xinjiang Uygur. DQB1*0301 is correlated with continuous infection of HBV. DQB1*0303 is a susceptibility gene of ASC.
Keywords: Hepatitis B virus, HLA-DQB1, Uygur
Introduction
Hepatitis B is a global public health problem. The clinical phenotypes of different races and regions of hepatitis B virus (HBV) after infection are dissimilar, but the exact mechanism is not entirely clear. Previous data [1] demonstrated that, as an important genetic control gene for immune characteristics, human leukocyte antigen (HLA) HBV’s gene polymorphism has certain correlation with the outcome of HBV infection. HLA-II class molecules are distributed on the surfaces of macrophages, B lymphocytes and the activated T cells during immune response and they are responsible for presenting exogenous antigens to CD4+ cytotoxic T cells. The antigen presenting efficiencies can vary due to gene loci. In addition, the HLA-II class molecules can also regulate lymphocytes and modulate the effect of tumor necrosis factor on the proliferative response of HBcAg, playing a role in immunoregulation. These factors further affect the clearance of HBV after infection and the progression of the disease. Xinjiang Uygur has a Caucasian ancestry, and its genetic background is different from that of the other ethnic groups in China. Furthermore, previous studies [2] report that the susceptibility of Xinjiang Uygur to HBV was generally less than that of the Han population in the same area. Here we investigated Uygur patients in Xinjiang area with different forms of clinical outcomes after infection of HBV. The gene polymorphisms of HLA-DQB1 on the outcomes of HBV infection were analyzed by using the sequence specific primer-polymerase chain reaction (PCR-SSP).
Materials and methods
Research subjects
110 cases of Uyghur patients with chronic hepatitis B (CHB) without sibship of the Xinjiang Uygur Autonomous Region people’s hospital inpatient and outpatient were collected from June 2010 to March 2012. There were 78 male cases aged between 18-59 years (36.23 ± 10.23) and 32 female cases aged 20-60 years (37.11 ± 10.13). There were 100 cases of chronic HBV carriers (asymptomatic HBV carrier, ASC), of whom 55 cases were male aged 19-59 years (36.13 ± 10.17) and 45 cases were female aged 20-59 years (36.41 ± 10.33). There were 80 self-limited HBV infection cases (resolved from HBV infection spontaneously, RHBS), of whom 45 male cases were aged 19-57 years (35.77 ± 10.31) and 35 female cases aged 21-61 years old (37.41 ± 10.28).
All the patients were diagnosed according to the related diagnostic criteria of 2010 “Chronic hepatitis B prevention and treatment guidelines”, excluding hepatitis A virus (HAV), hepatitis C virus (HCV), hepatitis D virus (HDV), hepatitis E virus (HEV), human immunodeficiency virus (HIV) infection and autoimmune liver diseases and other chronic liver diseases induced by alcoholic liver disease or hepatolenticular degeneration and other causes. There were no significant differences in ages and genders between 4 groups. At the same time, the patients of the CHB group and the ASC group were divided into groups according to the HBV DNA quantitative detection results and the serological marker of HBV: 1) HBV, DNA < 103 copies group and HBeAg (-) HBV low replication group, and 2) HBV DNA ≥ 103 copies group and/or HBeAg (+) HBV high copy.
Main reagents and instruments
ELISA kits were provided by Shanghai Rongsheng Biological Technology Co., Ltd. Whole blood small dose DNA extraction kits were provided by Shanghai SANGON Biological Engineering Technology Company. Primers were synthesized by Shanghai SANGON Biological Engineering Technology Company. PCR instrument (model of 580BR11774), electrophoresis apparatus trophoresis and gel image analyzer were all purchased from America Bio-RAD Company.
Methods
Sample collection
10 ml venous blood was collected from each subject, of which 5 ml was used for separation of serum for detection of HBV markers and liver function, and the other 5 ml was placed into an EDTA anticoagulant tube (-80°C) for preservation in order to extract DNA and measure HLA-DQB1 genotypes.
Detection of HLA-DQB1 genotypes by PCR-SSP
① Primer design: 11 pairs of primers were designed according to the reference [3] (Table 1). ② PCR amplification system contained 50 ng of genomic DNA of 2 μL of 2 μmol/L upstream primers 2 μL, and 2 μL of 2 μmol/L downstream primers. In order to eliminate the false negative results, the reaction system was added into positive internal control primers 0.4 μL and 2 μmol/L of human growth hormone gene. The PCR amplification conditions were as follows: initial denaturation at 94°C for 2 minutes, denaturation at 94°C for 30 seconds, annealing at 66°C for 30 seconds, extension at 72°C for 30 seconds, with a total of 30 cycles, finally extension at 72°C for 10 minutes. For PCR amplification product identification: 4 μL PCR products were mixed with 1 μL bromophenol blue for staining, and then the mixture was subjected to 1% agarose gel electrophoresis for 20 minutes at 140 V voltage. Using ultraviolet projection, bands clearly appeared in the corresponding lanes in the positive control lanes.
Table 1.
Designed primers for the amplification of various sites of HLA-DQB1
| Genes | Sequences of primers | Length (bp) |
|---|---|---|
| HLA-DQB1*0501 | F-5’-CGGAGCGCGTGCGGGG-3’ | 128 |
| R-5’-GCTGTTCCAGTACTCGGCAA-3’ | ||
| HLA-DQB1*0201 | F-5’-GTGCGTATTGTGAGCAGAAG-3’ | 205 |
| R-5’-GCAAGGTCGTGCGGAGCT-3’ | ||
| HLA-DQB1*0303 | F-5’-GACGGAGCGCGTGCGTCT-3’ | 129 |
| R-5’-CTGTTCCAGTACTCGGCGT-3’ | ||
| HLA-DQB1*0502 | F-5’-TGCGGGGTGTGACCAGAC-3’ | 117 |
| R-5’-TGCGGGGTGTGACCAGAC-3’ | ||
| HLA-DQB1*0602 | F-5’-CGTGCGTCTTGTGACCAGAT-3’ | 121 |
| R-5’-GCTGTTCCAGTACTCGGCAT-3’ | ||
| HLA-DQB1*0603/8 | F-5’-GGAGCGCGTGCGTCTTGTA-3’ | 127 |
| R-5’-GCTGTTCCAGTACTCGGCAT-3’ | ||
| HLA-DQB1*0604 | F-5’-CGTGTACCAGTTTAAGGGCA-3’ | 254 |
| R-5’-GCAGGATCCCGCGGTACC-3’ | ||
| HLA-DQB1*0201/0302 | F-5’-GACGGAGCGCGTGCGTCT-3’ | 129 |
| R-5’-CTGTTCCAGTACTCGGCGG-3’ | ||
| HLA-DQB1*0301 | F-5’-GACGGAGCGCGTGCGTTA-3’ | 122 |
| R-5’-AGTACTCGGCGTCAGGCG-3’ | ||
| HLA-DQB1*0302/3 | F-5’-GACGGAGCGCGTGCGTCT-3’ | 122 |
| R-5’-AGTACTCGGCGTCAGGCG-3’ | ||
| HLA-DQB1*0401 | F-5’-CACCAACGGGACCGAGCG-3’ | 200 |
| R-5’-GGTAGTTGTGTCTGCATACG-3’ |
Statistical analysis
SPSS 13.0 statistical software was used in the statistical analysis of the data. The measurement data was represented as X̅ ± s. Single factor variance analysis was used in the analyStatistical analysissis between groups. X2 test or Fisher exact probability method was used in the comparisons of frequencies between groups.
Results
Comparison of the distribution frequency of HLA-DQB1 gene polymorphisms in the RHBS and the ASC groups
The data demonstrates that the distribution frequency of DQB1*0201 in the RHBS group was higher than that in the ASC group (P < 0.05) (Table 2).
Table 2.
Comparisons of distribution frequency of HLA-DQB1 gene polymorphisms in the RHBS and ASC groups
| HLA-DQB1*0501 | 5.00 | 6.00 | 0.180 | 0.671 | 0.815 | 0.316~2.101 |
|---|---|---|---|---|---|---|
| HLA-DQB1*0201 | 18.75 | 10.50 | 5.959 | 0.015 | 2.257 | 1.166~4.370 |
| HLA-DQB1*0303 | 24.38 | 31.00 | 3.168 | 0.075 | 0.583 | 0.321~1.058 |
| HLA-DQB1*0502 | 3.75 | 4.50 | 0.131 | 0.717 | 0.820 | 0.279~2.408 |
| HLA-DQB1*0602 | 9.38 | 9.00 | 0.017 | 0.897 | 1.051 | 0.492~2.245 |
| HLA-DQB1*0603/8 | 1.25 | 1.50 | 0.041 | 0.839 | 0.829 | 0.135~5.085 |
| HLA-DQB1*0604 | 0.63 | 1.00 | 0.153 | 0.696 | 0.620 | 0.055~6.966 |
| HLA-DQB1*0201/0302 | 8.75 | 8.50 | 0.008 | 0.930 | 1.036 | 0.476~2.254 |
| HLA-DQB1*0301 | 21.88 | 16.50 | 0.257 | 0.612 | 1.167 | 0.643~2.117 |
| HLA-DQB1*0302/3 | 8.13 | 7.50 | 0.053 | 0.818 | 1.100 | 0.490~2.469 |
| HLA-DQB1*0401 | 3.75 | 4.00 | 0.015 | 0.901 | 0.932 | 0.310~2.806 |
Comparison of the distribution frequency of DQB1*0201 gene polymorphisms in the CHB and the ASC groups
The data shows that the distribution frequency of DQB1*0201 in the CHB group was higher than that in the ASC group (P < 0.05). The distribution frequency of DQB1*0301 in the CHB group was higher than that in the ASC group (P < 0.05). The distribution frequency of DQB1*0303 in the CHB group was lower than that in the ASC group (P < 0.05) (Table 3).
Table 3.
Comparison of distribution frequency of HLA-DQB1 gene polymorphisms in the CHB and the ASC groups
| HLA-DQB1 loci | CHB group (%, n = 110) | ASC group (%, n = 100) | χ2 value | P value | OR value | 95% CI |
|---|---|---|---|---|---|---|
| HLA-DQB1*0501 | 4.55 | 6.00 | 0.473 | 0.492 | 0.733 | 0.302~1.780 |
| HLA-DQB1*0201 | 17.73 | 10.50 | 5.363 | 0.021 | 2.066 | 1.112~3.841 |
| HLA-DQB1*0303 | 19.55 | 31.00 | 10.996 | 0.001 | 0.393 | 0.225~0.686 |
| HLA-DQB1*0502 | 5.91 | 4.50 | 0.444 | 0.505 | 1.355 | 0.553~3.322 |
| HLA-DQB1*0602 | 8.64 | 9.00 | 0.019 | 0.890 | 0.951 | 0.467~1.935 |
| HLA-DQB1*0603/8 | 0.45 | 1.50 | 1.226 | 0.268 | 0.297 | 0.030~2.899 |
| HLA-DQB1*0604 | 0.45 | 1.00 | 0.443 | 0.506 | 0.450 | 0.040~5.035 |
| HLA-DQB1*0201/0302 | 6.82 | 8.50 | 0.459 | 0.498 | 0.771 | 0.363~1.639 |
| HLA-DQB1*0301 | 26.82 | 16.50 | 9.062 | 0.003 | 2.349 | 1.341~4.114 |
| HLA-DQB1*0302/3 | 8.18 | 7.50 | 0.074 | 0.786 | 1.109 | 0.526~2.338 |
| HLA-DQB1*0401 | 3.18 | 4.00 | 0.211 | 0.646 | 0.782 | 0.273~2.239 |
Distribution of HLA-DQB1 alleles in different replication statuses of HBV
The data displays that the distribution frequency of DQB1*0201 in the low copy group was higher than that in the high copy group (P < 0.05), as demonstrated in Table 4.
Table 4.
Distribution of HLA-DQB1 alleles in different replication statuses of HBV
| HLA-DQB1 | HBV low replication group (n = 120) | HBV high replication group (n = 90) | P value | ||
|---|---|---|---|---|---|
|
|
|
||||
| Positive (n) | gene (frequency) | Positive (n) | gene (frequency) | ||
| HLA-DQB1*0501 | 14 | 5.83 | 8 | 4.44 | 0.515 |
| HLA-DQB1*0201 | 41 | 17.08 | 19 | 10.56 | 0.038 |
| HLA-DQB1*0303 | 70 | 29.17 | 45 | 25.00 | 0.230 |
| HLA-DQB1*0502 | 10 | 4.17 | 12 | 6.67 | 0.242 |
| HLA-DQB1*0602 | 17 | 7.08 | 20 | 11.11 | 0.129 |
| HLA-DQB1*0603/8 | 2 | 0.83 | 2 | 1.11 | 0.771 |
| HLA-DQB1*0604 | 2 | 0.83 | 1 | 0.56 | 0.737 |
| HLA-DQB1*0201/0302 | 20 | 8.33 | 12 | 6.67 | 0.506 |
| HLA-DQB1*0301 | 49 | 20.42 | 43 | 23.89 | 0.316 |
| HLA-DQB1*0302/3 | 18 | 7.50 | 15 | 8.33 | 0.743 |
| HLA-DQB1*0401 | 9 | 3.75 | 6 | 3.33 | 0.817 |
Agarose gel electrophoresis image of the PCR-SSP products of the HLA-DQB1 alleles
As illustrated in Figure 1, 11 alleles of the HLA-DQB1 region from 4 groups of subjects were analyzed by PCR-SSP. The alleles of HLA-DQB1 were examined by 2% agarose gel electrophoresis image.
Figure 1.
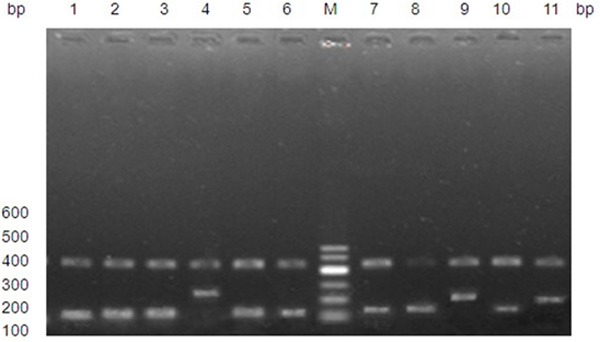
2% agarose gel electrophoresis image of the PCR-SSP products of the HLA-DQB1 alleles.
Discussion
HLA-II class genes which are responsible for the regulation of human immune functions have rich polymorphisms. The capacity for HBV infection has been shown to correlate with the HLA-II gene polymorphisms, which are responsible for varying antigen presentation efficiencies [4]. Polymorphic differences in this gene are especially apparent between different races, and have subsequently received greater attention in regards to the progression of disease in different races after infection with HBV. In this study, Xinjiang Uygur CHB, ASC and RHBS patients were selected for our study, where 3 groups of patients had been infected with HBV with same exposure history and high comparability, so the comparison results are more accurate.
Currently, research related to HLA-II class genes and HBV infection outcomes have been mainly focused on HLA-DRB1 and DQA1, while fewer studies have examined DQB1. Vaughan et al. [5] selected Poland HBV patients with nephritis as the subjects of a study and discovered that the gene frequency of HLA-DQB1*0303 of HBV infected people was higher than that of the healthy population. In comparison, Bhimma et al. [6] discovered that the black children HBV patients with nephritis had high gene frequency of DQB1*0603. Thio et al. [7] reported that the HLA-DQB1*0301 gene of black Americans were related to persistent HBV infections, while the persistent HBV infection of Turks correlated with DQB1*05 and DQB1*02 [8].
The Xinjiang Uygur patients with different clinical outcomes from HBV infection were examined. The data demonstrated that the distribution frequency of HLA-DQB1*0201 in the RHBS group was significantly higher than that in the ASC group, indicating that DQB1*0201 may be a HBV resistance gene in Xinjiang Uygur. This polymorphism may resist HBV infection and reduce the incidence rate of hepatitis B. The distribution frequencies of DQB1*0301 and DQB1*0201 in the CHB group were higher than that in the ASC group. The studies [7,9,10] have shown that DQB1*0301 correlate with the continuous infection of HBV, while DQB1*0201 was a HBV resistance gene. The genotype frequencies of the two genes were higher in the CHB group. We hypothesize that the host immunological status of the patients with HBV infection and carrying DQB1*0301 are changed.
T cells are activated under conditions such as fatigue, depression and other factors. Concurrent with removal of HBV, tissue damage was induced and a series of clinical symptoms appeared such as tired greasy, fever, abnormally increased aminotransferase and aurigo, contributing to the formation of CHB. For DQB1*0201, it may be that the HLA molecule regulates host antigen presenting cells and causes specific cytotoxic T lymphocyte responses. In turn, hepatocytes are damaged and even lysed at the same time of viral clearance by cells. The clearance process for the virus is spontaneous and involves hepatocyte damage and the induction of clinical symptoms of the disease.
The distribution frequency of DQB1*0303 in the CHB group was significantly lower than that in the ASC group, suggesting that DQB1*0303 is the resistance gene of CHB. In 2008, Z. Xi-Lin et al [3] selected 134 ASC patients and 136 CHB patients of Han in Beijing as the research subjects, and the research demonstrated that DQB1*0303 correlated with viral clearance, and it was believed that HLA determined the genetic susceptibility of the diseases. DQB1*0303 was associated with the suppression of CHB formation. In addition, we also think that ASC may be related to the low viral removal efficiency rate of DQB1*0303, which was insufficient to cause liver cell injury.
Our data demonstrated that the distribution frequency of HLA-DQB1*0201 in the low copy group was higher than that of the high copy group, suggesting that DQB1*0201 was associated with the low replication status of HBV and further indicating that DQB1*0201 contributed to the clearance of virus after infection of HBV. The distribution frequency of DQB1*0303 in the low copy group was higher than that of the high copy group, but there were no statistically significant differences. However, our study may have a deviation in grouping, as there was a high replication of HBV HbeAg (-) in liver tissues. Because of the limitations of these conditions, liver biopsy and puncture could not be conducted on the experimental samples to test the replication state of HBV. In addition, we also compared the frequency of HLA-DQB1 gene in the normal population of Xinjiang Uygur with that of the Han population in Beijing [2], but there were no significant differences. Therefore, the HLA-DQB1 polymorphisms cannot be used to entirely explain the susceptibility of HBV in Uygur and Han and the differences of disease progression. The results obtained from this study are insufficient to reveal the whole picture of the genetic factors of HLA.
The HLA system is an important research topic for human genetics. There are large differences in the HLA system between different races and ethnic populations. The results in the present study showed HLA-DQB1*0201 was a HBV resistance gene of Xinjiang Uygur, DQB1*0301 was related to persistent infection of HBV, and DQB1*0303 was a susceptibility gene of ASC, which may be associated with a low viral clearance efficiency rate. Previous studies [11-14] revealed that DRB1*13 correlated with HBV in: transient infection, chronic severe hepatitis, chronic and acute liver failure, and early cirrhosis. We believe that this gene induces hepatic cell damage at the same time of viral clearance. If virus was cleared in short term, RHBS was produced. Otherwise, chronic CHB was produced, and there is the possibility of formation of liver cirrhosis in long term. If hepatitis B, liver cirrhosis and hepatocellular carcinoma of Xinjiang Uygur are related to DQB1, and whether its mechanism is the same with the above formation mechanism, remains to be further studied.
Acknowledgements
This work was supported by grant 20130202 from Hospital project of Xinjiang Uygur Autonomous Region people’s Hospital.
Disclosure of conflict of interest
None.
References
- 1.Guo X, Zhang Y, Li J, Ma J, Wei Z, Tan W, O’Brien SJ. Strong influence of human leukocyte antigen (HLA)-DP gene variants on development of persistent chronic hepatitis B virus carriers in the Han Chinese population. Hepatology. 2011;53:422–8. doi: 10.1002/hep.24048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuohuti K, Wufuer H, Zhang LZ, Palida , Rouzi H, Yimiti H, Cheng Q, Dong YL, Yushan GL, Aisha M, Xu ZX. Epidemiological survey and analysis of HBsAg carrying rate of Uygur of Hotan Prefecture and Han population. Journal of First Military Medical University. 2004;24:1287–8. [Google Scholar]
- 3.Xi-Lin Z, Te D, Jun-Hong L, Liang-Ping L, Xin-Hui G, Ji-Rong G, Chun-Yan G, Zhuo L, Ying L, Hui L. Analysis of HLA-DQB1 gene polymorphisms in asymptomatic HBV carriers and chronic hepatitis B patients in the Chinese Han population. Int J Immunogenet. 2006;33:249–54. doi: 10.1111/j.1744-313X.2006.00607.x. [DOI] [PubMed] [Google Scholar]
- 4.Gao YF, Yu L, Ye J, Zou GZ, Li JB, Shen JL, Li X. Exogenous microRNA-mediated RNA interference in inhibition of HBV replication and expression. Journal of Medical University of Anhui. 2010;45:443–6. [Google Scholar]
- 5.Vaughan RW, Zurowska A, Moszkowska G, Kondeatis E, Clark AG. HLA-DRB and -DQB1 alleles in Polish patients with hepatitis B associated membranous nephropathy. Tissue Antigens. 1998;52:130–4. doi: 10.1111/j.1399-0039.1998.tb02276.x. [DOI] [PubMed] [Google Scholar]
- 6.Bhimma R, Hammond MG, Coovadia HM, Adhikari M, Connolly CA. HLA class I and II in black children with hepatitis B virus-associated membranous nephropathy. Kidney International. 2002;61:1510–5. doi: 10.1046/j.1523-1755.2002.00287.x. [DOI] [PubMed] [Google Scholar]
- 7.Thio CL, Carrington M, Marti D, O’Brien SJ, Vlahov D, Nelson KE, Astemborski J, Thomas DL. Class II HLA alleles and hepatitis B virus persistence in African Americans. J Infect Dis. 1999;179:1004–6. doi: 10.1086/314684. [DOI] [PubMed] [Google Scholar]
- 8.Akcam Z, Sunbul M, Durupinar B, Eroglu C, Esen S, Leblebicioglu H. Tissue types as prognostic risk factor in hepatitis B virus infection. Indian J Gastroenterol. 2002;21:139–41. [PubMed] [Google Scholar]
- 9.Jiang YG, Wang YM, Liu TH. Correlation between HLA-II class gene polymorphism and outcome of hepatitis B. Journal of Immunology. 2006;22:416–22. [Google Scholar]
- 10.Jiang YG, Wang YM, Liu TH, Liu J. Association between HLA class II gene and susceptibility or resistance to chronic hepatitis B. World J Gastroenterol. 2003;9:2221–5. doi: 10.3748/wjg.v9.i10.2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramezani A, Hasanjani Roshan MR, Kalantar E, Eslamifar A, Banifazl M, Taeb J, Aghakhani A, Gachkar L, Velayati AA. Association of human leukocyte antigen polymorphism with outcomes of hepatitis B virus infection. J Gastroenterol Hepatol. 2008;23:1716–21. doi: 10.1111/j.1440-1746.2008.05482.x. [DOI] [PubMed] [Google Scholar]
- 12.Liang HX, Yu ZJ, Jiang HQ, Zhang XQ. Study on the correlation between the chronic severe hepatitis B and HLA-DRB1 gene polymorphism. Chinese Journal of Clinical and Experimental Pathology. 2009;23:364–6. [PubMed] [Google Scholar]
- 13.Guo JG, Xun YH, Chen ZY, Wu J, Liu Y, Shi WZ, Shi JP, Lou GQ. The relationship between. HLA-DRB1 gene polymorphism and hepatitis B virus related acute and chronic liver failure. Chinese Journal of Department of Internal Medicine. 2011;50:63–5. [Google Scholar]
- 14.Pajewski NM, Parker SD, Poland GA, Ovsyannikova IG, Song W, Zhang K, McKinney BA, Pankratz VS, Edberg JC, Kimberly RP, Jacobson RM, Tang J, Kaslow RA. The role of HLA–DR–DQ haplotypes in variable antibody responses to Anthrax Vaccine Adsorbed. Genes Immun. 2011;12:457–65. doi: 10.1038/gene.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]


