Abstract
Background: Numerous studies have evaluated the association between NQO1 609C>T polymorphism and gastrointestinal (GI) cancer. However, the results remain inconclusive. To obtain a more precise estimation of the relation, we conducted an analysis of all available case-control studies. Methods: Eligible studies were identified by searching the databases and finally 19 articles were included in the meta-analysis. Odds ratio (OR) with 95% confidence interval (95% CI) was applied to assess the association between NQO1 609C>T polymorphism and GI cancer risk. Z test was used to evaluate the significance of OR and 95% CI. Results: In the overall analysis, there existed a significant association between NQO1 609C>T polymorphism and GI cancer susceptibility (T vs. C: OR = 1.07, 95% CI = 1.01-1.14). The subgroup analysis based on ethnicity showed that NQO1 609C>T polymorphism was associated with susceptibility to GI cancer in mixed population (TT vs. CC: OR = 2.21, 95% CI = 1.44-3.40; TT vs. CT + CC: OR = 2.26, 95% CI = 1.48-3.44; Allele T vs. Allele C: OR = 1.24, 95% CI = 1.05-1.47). For the subgroup analysis according to source of control, a remark relationship of 609C>T with increased risk of GI cancer was observed in HB population (Allele T vs. Allele C: OR = 1.07, 95% CI = 1.01-1.14). Conclusion: Our results demonstrated that NQO1 609C>T polymorphism might be associated with susceptibility to GI cancer.
Keywords: NQO1, polymorphism, gastrointestinal cancer
Introduction
Gastrointestinal (GI) cancer mainly affects the digestive system that involves cancers of oesophagus, gallbladder, liver, pancreas, stomach and bowel [1-4]. It has been reported that the incidence of GI cancer is increasing, with approximately 2 million new cases worldwide per year. As we all know, GI cancer arises from stomach and small intestine [5-9], but the pathogenesis of it is still unclear. Genetic factors, including the sequence alterations and organization aberrations of the cellular genome that range from single-nucleotide substitutions to gross chromosome, could modulate important biological progresses and alter susceptibility to cancers consequently [10,11]. Recently, many studies have investigated the role of NQO1 gene in the pathogenesis of GI cancer.
NQO1 gene is located on chromosome 16q22.1, spanning 17.2 kb and consisting of 6 exons and 5 introns [12], which encodes NAD(P)H dehydrogenase 1 [13]. The gene is a member of NAD(P)H dehydrogenase family and encodes a cytoplasmic 2-electron reductase. The studies have suggested that mutations in NQO1 are associated with increased risk of tardive dyskinesia (TD), hematotoxicity after exposure to benzene and cancers [14]. The 609C>T polymorphism, with proline-to-serine amino acid change, is implicated in pathogenesis of cancers [15]. Although the relationship of NQO1 609C>T polymorphism with GI cancer has been extensively investigated, the results were still inconclusive.
The reported genetic effects varied across the published studies, and a clear impact on cancer risk is also limited by the insufficient statistical power of these individual studies with a relatively small sample size. Therefore, we performed a meta-analysis, based on published articles, to evaluate the influence of the NQO1 609C>T polymorphism on the risk of GI cancer.
Materials and methods
Searching strategy
Databases of PubMed, EMBASE, and other database were searched to retrieve eligible studies. Key words included “gastrointestinal”, “NQO1”, “polymorphism”, “cancer”, “esophageal”, “stomach” and “gastric”. Reference lists of related studies and reviews were manually searched for additional publications.
Inclusion criteria
We defined inclusion criteria as follows: written in English or Chinese; case-control design; sufficient information for estimating ORs and their 95% CIs; genotype frequencies in the controls were in agreement with Hardy-Weinberg equilibrium (HWE). Meanwhile, if the studies showed overlapping data, the most recent study with larger sample size was selected.
Quality assessment
The quality of each study was assessed by the Newcastle-Ottawa quality assessment scale.
Data extraction
Data were extracted from included studies independently by authors. For each study, the following data were collected: last name of the first author, year of publication, country, ethnicity, study design, numbers of subjects, source of controls, genotyping method, allele and genotype frequencies. In case of conflicting evaluations, disagreements were resolved through discussion by other authors.
Statistical analysis
Hardy Weinberg Equilibrium (HWE) was tested in control group with chi-square test. The association between NQO1 609C>T polymorphism and GI cancer risk was estimated by pooled ORs with 95% CIs. Pooled ORs and 95% CI were calculated under the five genetic models of TT vs. CC, TT + CT vs. CC, TT vs. CT + CC, Allele T vs. Allele C and CT vs. CC. Z test was used to evaluate the significance of the pooled OR, and if P < 0.05, statistically significance was confirmed. Q test was used to check the statistical heterogeneity between studies. The heterogeneity was considered significant when P < 0.10. The fixed-effects model (based on Mantel-Haenszel method) or random-effects model (based on DerSimonian-Laird method) was used to calculate ORs with 95% CIs in the overall analysis. The random-effects model was employed when there was significant heterogeneity; otherwise, the fixed-effects model was applied. Sensitivity analyses were performed to identify the effect of individual study on pooled results and test the reliability of results. Potential publication bias were estimated by Begg’s funnel plot and Egger’s linear regression test, and P < 0.05 was considered significant. All the analysis was conducted with STATA Version 12.0 software.
Results
Study characteristics
Through literature search, a total of 203 relevant studies were identified (Figure 1). After careful review and selection, 19 eligible case-control studies were included in this meta-analysis [16-34]. The detailed characteristics of eligible studies were summarized in Table 1.
Figure 1.
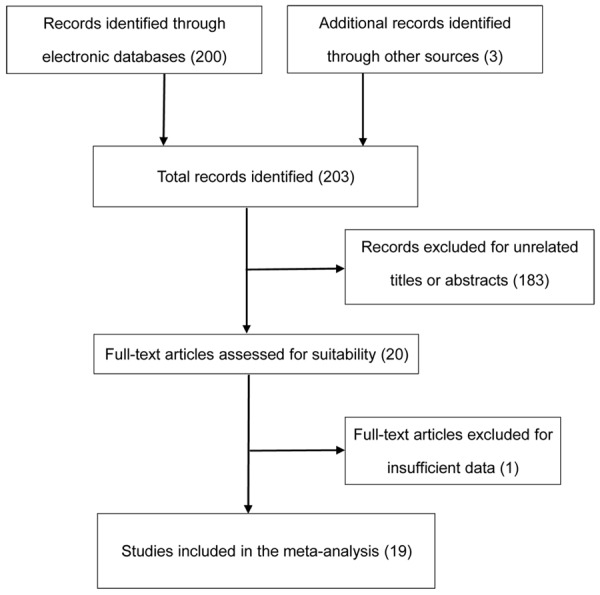
Flow diagram of the study selection process.
Table 1.
Main characteristics of all studies included in the meta-analysis
| First author | Year | source | Country | Ethnicity | Genotyping method | HWE |
|---|---|---|---|---|---|---|
| Marjani | 2010 | Hospital based control | Iran | Asian | PCR-RFLP | 0.47 |
| Martino | 2007 | Hospital based control | United Kingdom | Caucasian | PCR-RFLP | 0.99 |
| Rahden | 2004 | Hospital based control | German | Caucasian | PCR-RFLP | 0.17 |
| Sarbia | 2003 | Hospital based control | German | Caucasian | PCR-RFLP | 0.60 |
| Zhang | 2003 | Hospital based control | German | Mixed | PCR-RFLP | 0.19 |
| Zhang | 2003 | Hospital based control | China | Asian | PCR-RFLP | 0.39 |
| Hamajima | 2002 | Hospital based control | Japan | Asian | PCR-RFLP | 0.08 |
| Malik | 2010 | Hospital based control | India | Asian | PCR-RFLP | 0.31 |
| Sachse | 2002 | Population-based control | United Kingdom | Caucasian | PCR-RFLP | 0.98 |
| Hlavata | 2010 | Hospital based control | Czech | Caucasian | PCR-RFLP | 0.85 |
| Sameer | 2010 | Hospital based control | India | Asian | PCR-RFLP | 0.45 |
| Nisa | 2010 | Hospital based control | Japan | Asian | PCR-RFLP | 0.07 |
| Begleiter | 2006 | Hospital based control | Canada | Mixed | PCR-RFLP | 0.29 |
| van der Logt | 2006 | Population-based control | New Zealand | Caucasian | PCR-RFLP | 0.95 |
| Harth | 2000 | Population-based control | German | Caucasian | PCR-RFLP | 0.79 |
| Mitrou | 2002 | Hospital based control | United Kingdom | Caucasian | PCR-RFLP | 0.58 |
| Mohelnikova-Duchonova | 2010 | Hospital based control | Czech | Caucasian | TaqMan assay | 0.93 |
| Bartsch | 1998 | Hospital based control | German | Caucasian | PCR-RFLP | 0.27 |
| Akkiz | 2010 | Hospital based control | Turkey | Asian | PCR-RFLP | 0.81 |
Meta-analysis results
In order to explore the association between NQO1 609C>T polymorphism and the risk of GI cancer, a meta-analysis was conducted. The pooled ORs and their 95% CIs were calculated under the fixed effects model. In the overall analyses, we found that there was a significant association between NQO1 609C>T polymorphism and GI cancer susceptibility (T vs. C: OR = 1.07, 95% CI = 1.01-1.14). In addition, we conducted subgroup analysis according to ethnicity and source of control.
Subgroup analysis for ethnicity
The meta-analysis included 10 studies in Caucasian population, 7 studies in Asian population, and 2 studies in mixed population. The pooled ORs with their 95% CIs are shown in Table 2. In the analysis, a remark relationship of NQO1 609C>T polymorphism and risk of GI cancer was observed in mixed population (TT vs. CC: OR = 2.21, 95% CI = 1.44-3.40; TT vs. CT + CC: OR = 2.26, 95% CI = 1.48-3.44; Allele T vs. Allele C: OR = 1.24, 95% CI = 1.05-1.47).
Table 2.
Pooled ORs with 95% CIs in the subgroup analysis by ethnicity
| Genetic model | OR (95% CI) | P (P value of heterogeneity) | |
|---|---|---|---|
| Overall | |||
| TT vs. CC | 1.15 (0.99-1.33) | 0.202 | |
| TT + CT vs. CC | 1.07 (1.00-1.14) | 0.728 | |
| TT vs. CT + CC | 1.13 (0.98-1.30) | 0.129 | |
| Allele T vs. Allele C | 1.07 (1.01-1.14) | 0.147 | |
| CT vs. CC | 1.06 (0.99-1.44) | 0.798 | |
| Ethnicity | |||
| Caucasians | TT vs. CC | 1.05 (0.81-1.37) | 0.790 |
| TT + CT vs. CC | 1.09 (1.00-1.20) | 0.453 | |
| TT vs. CT + CC | 1.02 (0.78-1.32) | 0.878 | |
| Allele T vs. Allele C | 1.09 (1.00-1.18) | 0.218 | |
| CT vs. CC | 1.10 (1.00-1.21) | 0.510 | |
| Asians | TT vs. CC | 1.02 (0.84-1.25) | 0.363 |
| TT + CT vs. CC | 1.02 (0.92-1.14) | 0.742 | |
| TT vs. CT + CC | 1.02 (0.84-1.23) | 0.217 | |
| Allele T vs. Allele C | 1.02 (0.93-1.12) | 0.316 | |
| CT vs. CC | 1.02 (0.91-1.15) | 0.798 | |
| Mixed | TT vs. CC | 2.21 (1.44-3.40) | 0.840 |
| TT + CT vs. CC | 1.11 (0.91-1.35) | 0.412 | |
| TT vs. CT + CC | 2.26 (1.48-3.44) | 0.800 | |
| Allele T vs. Allele C | 1.24 (1.05-1.47) | 0.266 | |
| CT vs. CC | 1.01 (0.81-1.25) | 0.517 | |
Subgroup analysis for source of control
The meta-analysis included 16 hospital-based (PB) studies and 3 population-based (HB) studies. The details about the ORs with 95% CIs were shown in Table 3. The results showed that NQO1 609C>T was associated with increased risk of GI cancer (Allele T vs. Allele C: OR = 1.07, 95% CI = 1.01-1.14) in HB population not in PB population.
Table 3.
Pooled ORs with 95% CIs in the subgroup analysis by source of control
| Genetic model | OR (95% CI) | P (P value of heterogeneity) | |
|---|---|---|---|
| Overall | |||
| TT vs. CC | 1.15 (0.99-1.33) | 0.202 | |
| TT + CT vs. CC | 1.07 (1.00-1.14) | 0.728 | |
| TT vs. CT + CC | 1.13 (0.98-1.30) | 0.129 | |
| Allele T vs. Allele C | 1.07 (1.01-1.14) | 0.147 | |
| CT vs. CC | 1.06 (0.99-1.14) | 0.798 | |
| Source of control | |||
| HB | TT vs. CC | 1.17 (1.00-1.37) | 0.109 |
| TT + CT vs. CC | 1.06 (0.98-1.14) | 0.712 | |
| TT vs. CT + CC | 1.16 (0.99-1.35) | 0.066 | |
| Allele T vs. Allele C | 1.07 (1.01-1.14) | 0.118 | |
| CT vs. CC | 1.05 (0.97-1.13) | 0.814 | |
| PB | TT vs. CC | 0.99 (0.65-1.49) | 0.903 |
| TT + CT vs. CC | 1.10 (0.95-1.29) | 0.331 | |
| TT vs. CT + CC | 0.94 (0.62-1.42) | 0.974 | |
| Allele T vs. Allele C | 1.09 (0.95-1.25) | 0.247 | |
| CT vs. CC | 1.12 (0.95-1.32) | 0.327 | |
HB: hospital-based; PB: population-based.
Sensitivity analysis
Sensitivity analysis was conducted in order to evaluate the influence of each single publication on the overall results. After excluding each study one by one at a time and comparing the results before and after, we did not find any remarkable changes, which suggested that our meta-analysis results were stable.
Publication bias
Begg’s funnel plot and Egger’s test were performed to assess the publication bias. The shape of the funnel plot revealed no obvious asymmetry. Moreover, the Egger’s test showed no obvious publication bias (P = 0.352).
Discussion
GI cancer is a rare, slow-growing cancer that affects certain cells in the lining of the stomach and intestines [35]. It has been demonstrated that hormones secreted by the cells could regulate the production of digestive juices and muscles that move food through the stomach and intestines. Moreover, GI cancer is associated with increased risk of other cancers of digestive system, which seriously affects population lives. To obtain more information on the pathogenesis of GI cancer, many studies have investigated the association of genes with the risk of GI cancer.
NQO1 is an important enzyme which can catalyze the two-electron reduction of quinoid compounds into hydroquinones [36]. NAD (P) H, decoded by NQO1, also plays a prominent role in maintaining cellular homeostasis [37,38]. Additionally, NQO1 is essential for the antioxidant defense system, stabilization of tumor suppressors and activation of quinone based chemotherapeutics. Overexpression of NQO1 in solid tumors coupling with its ability to convert quinone-based chemo-therapeutics into potent cytotoxic compounds has made it a very attractive target [39,40]. Single-nucleotide polymorphisms (SNPs) in genes coding metabolizing enzymes could modulate genetic functions and cellular toxicity in response to chemicals. NQO1 is an important detoxification enzyme involved in the catabolism of 1,4-benzoquinone (1,4-BQ), a benzene metabolite believed to be associated with bone-marrow toxicity and leukemia [41]. In recent years, the relationship of NQO1 609C>T polymorphism with GI cancer also has been reported. Since the effects of district, country and ethnicity, no conclusive results were obtained.
In the overall analyses, we detected a significant association between NQO1 609C>T polymorphism and GI cancer susceptibility. Indeed, in the subgroup analysis by ethnicity, significantly relationship was also found between NQO1 609C>T and GI cancer in the mixed group. In the subgroup analysis by source of control, significantly increased risk of GI cancer was observed in the HB group but not in the PB group. Further investigations with large sample sizes are needed to clarify the possible effects of NQO1 609C>T on GI cancer.
Heterogeneity is a potential problem when interpreting the results of all meta-analyses. Throughout the overall and subgroup analyses, the heterogeneity was not detected in the meta-analyses. Moreover, the sensitivity analysis and Egger’test suggested that our results were stable and reliable. However, several limitations should be addressed. First, most of the studies were involved in Caucasians and Asians, and only two studies were mixed ethnicities. Second, only published studies were included in the meta-analysis, therefore, publication bias might have occurred, even though the statistical test showed no bias. Third, the sample sizes of included studies were relatively small and the matching criteria for the cases and controls were also not strict. In conclusion, this meta-analysis suggested that NQO1 609C>T polymorphism may be associated with increased risk of GI cancer. Future larger and well-designed studies in different ethnic populations and different sites of GI cancer are needed to validate our findings.
Disclosure of conflict of interest
None.
References
- 1.Tye H, Jenkins BJ. Tying the knot between cytokine and toll-like receptor signaling in gastrointestinal tract cancers. Cancer Sci. 2013;104:1139–1145. doi: 10.1111/cas.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abedi-Ardekani B, Hainaut P. Cancers of the upper gastro-intestinal tract: a review of somatic mutation distributions. Arch Iran Med. 2014;17:286–292. [PubMed] [Google Scholar]
- 3.Zheng S, Huang KE, Pan YL, Zhou Y, Pan SD, Li X, Jia J, Zheng XL, Tao DY. KIT and BRAF heterogeneous mutations in gastrointestinal stromal tumors after secondary imatinib resistance. Gastric Cancer. 2014 doi: 10.1007/s10120-014-0414-7. [DOI] [PubMed] [Google Scholar]
- 4.Scherubl H, Faiss S, Knoefel WT, Wardelmann E. Management of early asymptomatic gastrointestinal stromal tumors of the stomach. World J Gastrointest Endosc. 2014;6:266–271. doi: 10.4253/wjge.v6.i7.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ray-Coquard I, Le Cesne A, Michallet V, Boukovinas I, Ranchere D, Thiesse P, Baty V, Blay JY. [Gastro-intestinal stromal tumors: news and comments] . Bull Cancer. 2003;90:69–76. [PubMed] [Google Scholar]
- 6.Sudhakar MK, Neeta , Senthil , Ahamed A, John S, Aggarwal G. Gastro-intestinal stromal tumour--a case report. J Indian Med Assoc. 2006;104:266, 270. [PubMed] [Google Scholar]
- 7.Heymann S, Imperiale A, Schlund-Schoettel E, Sauer B, Dourthe LM. [A rare case of bone metastasis from gastro-intestinal stromal tumour: place of radiotherapy] . Cancer Radiother. 2014;18:55–58. doi: 10.1016/j.canrad.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Agashe SR, Patil PP, Phansopkar MA, Shivani A, Kulkarni SH. Gastro-intestinal stromal tumour-a case report. J Indian Med Assoc. 2012;110:404–405. [PubMed] [Google Scholar]
- 9.Sirohi B, Philip DS, Shrikhande SV. Regorafenib in gastrointestinal stromal tumors. Future Oncol. 2014;10:1581–1587. doi: 10.2217/fon.14.101. [DOI] [PubMed] [Google Scholar]
- 10.Huang M, Dinney CP, Lin X, Lin J, Grossman HB, Wu X. High-order interactions among genetic variants in DNA base excision repair pathway genes and smoking in bladder cancer susceptibility. Cancer Epidemiol Biomarkers Prev. 2007;16:84–91. doi: 10.1158/1055-9965.EPI-06-0712. [DOI] [PubMed] [Google Scholar]
- 11.Ouerhani S, Cherif N, Bahri I, Safra I, Menif S, Abbes S. Genetic polymorphisms of NQO1, CYP1A1 and TPMT and susceptibility to acute lymphoblastic leukemia in a Tunisian population. Mol Biol Rep. 2013;40:1307–1314. doi: 10.1007/s11033-012-2174-y. [DOI] [PubMed] [Google Scholar]
- 12.Jaiswal AK. Human NAD(P)H:quinone oxidoreductase2. Gene structure, activity, and tissue-specific expression. J Biol Chem. 1994;269:14502–14508. [PubMed] [Google Scholar]
- 13.Lajin B, Alachkar A, Alhaj Sakur A. A quadruplex tetra-primer ARMS-PCR method for the simultaneous detection of TP53 Arg72Pro, IVS3 16bp Del/Ins and IVS6 + 62A>G, and NQO1 C609T polymorphisms. Gene. 2012;504:268–273. doi: 10.1016/j.gene.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 14.West AB, Dawson VL, Dawson TM. To die or grow: Parkinson’s disease and cancer. Trends Neurosci. 2005;28:348–352. doi: 10.1016/j.tins.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Han FF, Guo CL, Gong LL, Jin Z, Liu LH. Effects of the NQO1 609C>T polymorphism on leukemia susceptibility: evidence from a meta-analysis. Asian Pac J Cancer Prev. 2013;14:5311–5316. doi: 10.7314/apjcp.2013.14.9.5311. [DOI] [PubMed] [Google Scholar]
- 16.Akkiz H, Bayram S, Bekar A, Akgollu E, Ulger Y, Kaya BY, Sandikci M, Ozdil B. No association of NAD(P)H: quinone oxidoreductase 1 (NQO1) C609T polymorphism and risk of hepatocellular carcinoma development in Turkish subjects. Asian Pac J Cancer Prev. 2010;11:1051–1058. [PubMed] [Google Scholar]
- 17.Nisa H, Kono S, Yin G, Toyomura K, Nagano J, Mibu R, Tanaka M, Kakeji Y, Maehara Y, Okamura T, Ikejiri K, Futami K, Maekawa T, Yasunami Y, Takenaka K, Ichimiya H, Terasaka R. Cigarette smoking, genetic polymorphisms and colorectal cancer risk: the Fukuoka Colorectal Cancer Study. BMC Cancer. 2010;10:274. doi: 10.1186/1471-2407-10-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sarbia M, Bitzer M, Siegel D, Ross D, Schulz WA, Zotz RB, Kiel S, Geddert H, Kandemir Y, Walter A, Willers R, Gabbert HE. Association between NAD(P)H: quinone oxidoreductase 1 (NQ01) inactivating C609T polymorphism and adenocarcinoma of the upper gastrointestinal tract. Int J Cancer. 2003;107:381–386. doi: 10.1002/ijc.11430. [DOI] [PubMed] [Google Scholar]
- 19.Zhang J, Schulz WA, Li Y, Wang R, Zotz R, Wen D, Siegel D, Ross D, Gabbert HE, Sarbia M. Association of NAD(P)H: quinone oxidoreductase 1 (NQO1) C609T polymorphism with esophageal squamous cell carcinoma in a German Caucasian and a northern Chinese population. Carcinogenesis. 2003;24:905–909. doi: 10.1093/carcin/bgg019. [DOI] [PubMed] [Google Scholar]
- 20.Mitrou PN, Watson MA, Loktionov AS, Cardwell C, Gunter MJ, Atkin WS, Macklin CP, Cecil T, Bishop DT, Primrose J, Bingham SA. Role of NQO1C609T and EPHX1 gene polymorphisms in the association of smoking and alcohol with sporadic distal colorectal adenomas: results from the UKFSS Study. Carcinogenesis. 2007;28:875–882. doi: 10.1093/carcin/bgl194. [DOI] [PubMed] [Google Scholar]
- 21.Zhang JH, Li Y, Wang R, Geddert H, Guo W, Wen DG, Chen ZF, Wei LZ, Kuang G, He M, Zhang LW, Wu ML, Wang SJ. NQO1 C609T polymorphism associated with esophageal cancer and gastric cardiac carcinoma in North China. World J Gastroenterol. 2003;9:1390–1393. doi: 10.3748/wjg.v9.i7.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marjani HA, Biramijamal F, Rakhshani N, Hossein-Nezhad A, Malekzadeh R. Investigation of NQO1 genetic polymorphism, NQO1 gene expression and PAH-DNA adducts in ESCC. A case-control study from Iran. Genet Mol Res. 2010;9:239–249. doi: 10.4238/vol9-1gmr693. [DOI] [PubMed] [Google Scholar]
- 23.di Martino E, Hardie LJ, Wild CP, Gong YY, Olliver JR, Gough MD, Bird NC. The NAD(P)H: quinone oxidoreductase I C609T polymorphism modifies the risk of Barrett esophagus and esophageal adenocarcinoma. Genet Med. 2007;9:341–347. doi: 10.1097/gim.0b013e3180654ccd. [DOI] [PubMed] [Google Scholar]
- 24.von Rahden BH, Stein HJ, Langer R, von Weyhern CW, Schenk E, Doring C, Siewert JR, Hofler H, Sarbia M. C609T polymorphism of the NAD(P)H: quinone oxidoreductase I gene does not significantly affect susceptibility for esophageal adenocarcinoma. Int J Cancer. 2005;113:506–508. doi: 10.1002/ijc.20576. [DOI] [PubMed] [Google Scholar]
- 25.Malik MA, Zargar SA, Mittal B. Role of NQO1 609C>T and NQO2-3423G>A polymorphisms in susceptibility to gastric cancer in Kashmir valley. DNA Cell Biol. 2011;30:297–303. doi: 10.1089/dna.2010.1115. [DOI] [PubMed] [Google Scholar]
- 26.Hlavata I, Vrana D, Smerhovsky Z, Pardini B, Naccarati A, Vodicka P, Novotny J, Mohelnikova-Duchonova B, Soucek P. Association between exposure-relevant polymorphisms in CYP1B1, EPHX1, NQO1, GSTM1, GSTP1 and GSTT1 and risk of colorectal cancer in a Czech population. Oncol Rep. 2010;24:1347–1353. doi: 10.3892/or_00000992. [DOI] [PubMed] [Google Scholar]
- 27.Sameer AS, Shah ZA, Syeed N, Rasool R, Afroze D, Siddiqi MA. NAD(P)H: quinone oxidoreductase 1 (NQO1) Pro187Ser polymorphism and colorectal cancer predisposition in the ethnic Kashmiri population. Asian Pac J Cancer Prev. 2010;11:209–213. [PubMed] [Google Scholar]
- 28.van der Logt EM, Bergevoet SM, Roelofs HM, Te Morsche RH, Dijk Y, Wobbes T, Nagengast FM, Peters WH. Role of epoxide hydrolase, NAD(P)H: quinone oxidoreductase, cytochrome P450 2E1 or alcohol dehydrogenase genotypes in susceptibility to colorectal cancer. Mutat Res. 2006;593:39–49. doi: 10.1016/j.mrfmmm.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 29.Harth V, Donat S, Ko Y, Abel J, Vetter H, Bruning T. NAD(P)H quinone oxidoreductase 1 codon 609 polymorphism and its association to colorectal cancer. Arch Toxicol. 2000;73:528–531. doi: 10.1007/s002040050004. [DOI] [PubMed] [Google Scholar]
- 30.Sachse C, Smith G, Wilkie MJ, Barrett JH, Waxman R, Sullivan F, Forman D, Bishop DT, Wolf CR. A pharmacogenetic study to investigate the role of dietary carcinogens in the etiology of colorectal cancer. Carcinogenesis. 2002;23:1839–1849. doi: 10.1093/carcin/23.11.1839. [DOI] [PubMed] [Google Scholar]
- 31.Begleiter A, Hewitt D, Maksymiuk AW, Ross DA, Bird RP. A NAD(P)H: quinone oxidoreductase 1 polymorphism is a risk factor for human colon cancer. Cancer Epidemiol Biomarkers Prev. 2006;15:2422–2426. doi: 10.1158/1055-9965.EPI-06-0661. [DOI] [PubMed] [Google Scholar]
- 32.Bartsch H, Malaveille C, Lowenfels AB, Maisonneuve P, Hautefeuille A, Boyle P. Genetic polymorphism of N-acetyltransferases, glutathione S-transferase M1 and NAD(P)H: quinone oxidoreductase in relation to malignant and benign pancreatic disease risk. The International Pancreatic Disease Study Group. Eur J Cancer Prev. 1998;7:215–223. doi: 10.1097/00008469-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Mohelnikova-Duchonova B, Marsakova L, Vrana D, Holcatova I, Ryska M, Smerhovsky Z, Slamova A, Schejbalova M, Soucek P. Superoxide dismutase and nicotinamide adenine dinucleotide phosphate: quinone oxidoreductase polymorphisms and pancreatic cancer risk. Pancreas. 2011;40:72–78. doi: 10.1097/MPA.0b013e3181f74ad7. [DOI] [PubMed] [Google Scholar]
- 34.Hamajima N, Matsuo K, Iwata H, Shinoda M, Yamamura Y, Kato T, Hatooka S, Mitsudomi T, Suyama M, Kagami Y, Ogura M, Ando M, Sugimura Y, Tajima K. NAD(P)H: quinone oxidoreductase 1 (NQO1) C609T polymorphism and the risk of eight cancers for Japanese. Int J Clin Oncol. 2002;7:103–108. doi: 10.1007/s101470200013. [DOI] [PubMed] [Google Scholar]
- 35.Gujral DM, Bhattacharyya S. Cardiac manifestations of gastrointestinal carcinoid tumor. Future Cardiol. 2013;9:479–488. doi: 10.2217/fca.13.24. [DOI] [PubMed] [Google Scholar]
- 36.Lin L, Qin Y, Jin T, Liu S, Zhang S, Shen X, Lin Z. Significance of NQO1 overexpression for prognostic evaluation of gastric adenocarcinoma. Exp Mol Pathol. 2014;96:200–205. doi: 10.1016/j.yexmp.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 37.Phillips RM, Basu S, Brown JE, Flannigan GM, Loadman PM, Martin SW, Naylor B, Puri R, Shah T. Detection of (NAD(P)H: quinone oxidoreductase-1, EC 1.6. 99.2) 609C→T and 465C→T polymorphisms in formalin-fixed, paraffin-embedded human tumour tissue using PCR-RFLP. Int J Oncol. 2004;24:1005–1010. [PubMed] [Google Scholar]
- 38.Liu K, Tian H, Yu KZ, Shen WY, Mao ZC, Jin CH, Pan HB, He JX. Association between NQO1 Pro187Ser polymorphism and esophageal cancer: a meta-analysis. Tumour Biol. 2014;35:2063–2068. doi: 10.1007/s13277-013-1273-2. [DOI] [PubMed] [Google Scholar]
- 39.Lienhart WD, Gudipati V, Uhl MK, Binter A, Pulido SA, Saf R, Zangger K, Gruber K, Macheroux P. Collapse of the native structure caused by a single amino acid exchange in human NAD(P)H: quinone oxidoreductase(1) FEBS J. 2014;281:4691–4704. doi: 10.1111/febs.12975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang H, Neely L, Lundgren K, Yang YC, Lough R, Timple N, Burrows F. BIIB021, a synthetic Hsp90 inhibitor, has broad application against tumors with acquired multidrug resistance. Int J Cancer. 2010;126:1226–1234. doi: 10.1002/ijc.24825. [DOI] [PubMed] [Google Scholar]
- 41.Zhang J, Yin L, Liang G, Liu R, Pu Y. Detection of quinone oxidoreductase 1 (NQO1) single-nucleotide polymorphisms (SNP) related to benzene metabolism in immortalized B lymphocytes from a Chinese Han population. J Toxicol Environ Health A. 2010;73:490–498. doi: 10.1080/15287390903523436. [DOI] [PubMed] [Google Scholar]


