Abstract
Aim: The uterus with its size exceeds 12 weeks of gestation have been considered a relative contraindication to laparoscopic hysterectomy. With surgical techniques progressed and laparoscopic instruments improved, laparoscopic hysterectomy for large uteri have been performed safely and effectively. The aim of this study is to assess the feasibility and safety of laparoscopic hysterectomy on uterus more than 800 g using a three-trocar technique on 18 patients. Methods: From June 2011 to June 2013 a total of 18 consecutive patients underwent laparoscopic hysterectomy for benign gynaecological conditions. All of the 18 consecutive cases were successfully completed by laparoscopy with the instruction of the procedure. Results: All of the 18 cases were completed by laparoscopy without major complication. The average time of the surgery was 107 min (65-180), the average blood lost was 225 ml (50-800 ml), the average weight of the uterus was 1105 g (820-1880 g), and the average HGB drop was 0.9 g/dl (0.2-1.9 g/dl). Conclusion: Based on appropriate techniques and careful operate, Laparoscopic hysterectomies for large uteri using three-trocar is safe and feasible to most of the patients.
Keywords: Laparoscopic hysterectomy, large uterus, three-trocar technique
Introduction
Laparoscopic technique has been widely applied in gynecological surgery. It is a minimally invasive procedure with superior anatomic images due to magnification of video laparoscope, less blood loss, shorter hospitalization, faster recover, fewer complications, less adhesion formation and less scars [1-4]. With these advantages, it became a popular choice amongst women requiring hysterectomy for benign conditions. However, in rare cases the uterus can grow to a very large volume, thus present a big challenge for gynecological surgeon. A large uterus may lead to limited visibility, restrictive instrument range of motion and difficult removal of the specimen, and higher risk of complications such as hemorrhage, bowel and urinary injury [5-7]. Ferrari et al. [8] suggested that uteri weighing >500 g were difficult for laparoscopic hysterectomy. Similar results were reported by other studies and suggested that very large uteri should be treated by laparotomy [9,10].
With progressing surgical techniques and improved laparoscopic instruments, laparoscopic hysterectomy for large uteri have been performed safely and effectively [11,12], several studies have reported that they successfully performed laparoscopic hysterectomy on large uteri for more than 1000 g [13-16], all of which suggested that laparoscopic hysterectomy can be performed safely on well selected patient with large uterus.
In this article, we will report the experience of laparoscopic hysterectomy on large uteri more than 800 g using three-trocar technique, with the aim to assess the feasibility and safety of this technique.
Materials and methods
This is a retrospective review of 18 consecutive patients with enlarged uterus who underwent laparoscopic hysterectomy for benign gynaecological conditions using a three-trocar technique during the period of 2 years from June 2011 to June 2013 in Zhejiang provincial people’s hospital, China. Inclusion criteria were benign uterine disorders with uterine size of 16 weeks gestation or more and with a weight of more than 800 g. Women with malignancy or precancerosis or pelvic floor prolapse were excluded. Information collected including complete medical history, physical and gynecologic examination for the uterine size and mobility, laboratory examination, and ultrasound for the uterus. All patients had Liquid-based cytology and HPV test as well as endometrial sampling before there surgery. Two of the patients underwent total laparoscopic hysterectomy and the other of them underwent subtotal hysterectomy. Those who underwent subtotal hysterectomy should have high-risk HPV negative, previous three normal cervical smear and the willingness to continue on the cervical screening programme.
They were recommended to have a bowel preparation for a better visualization of the operative field and prophylactic antibiotic usage was performed half an hour before surgery. The procedure was completed by several seasoned associate chief physician and all patients received an informed consent before surgery. Approvals were obtained from the Ethics Committee of the Hospital.
Procedure
All patients were performed under general anaesthesia by endotracheal intubation in the lithotomy position with arms tucked at her sides. After catheterization and preparing the patient, a 10 mm trocar was inserted at the umbilicus point or upper umbilicus in the view of individual patient, pneumoperitoneum was established and a 30° laparoscope was then introduced through this port. After inspecting the abdomen and the pelvis, a uterine manipulator was inserted through the cervix under the supervision of laparoscope to accommodate the uterus as the procedure needs. Another 10mm trocar was placed according to the level where the adnexa located on after elevating the uterus. Usually the trocar was placed at the line between the left anterior superior iliac spine and umbilicus, 2 cm higher than the utero-ovarian ligaments after elevating the uterus. A 5 mm trocar was then placed on the contralateral side with the same rule (Figure 1A). With the aid of the manipulator, the uterus was then positioned at the opposite side as much as possible for a better exposure of the operative side. Transection with scissors was followed by bipolar forceps desiccation of the round ligament, the tubal isthmus and the utero-ovarian ligament, and then the peritoneum is opened on the anterior leaf of the broad ligament, the uterovesical fold was then opened and bladder reflected downwards(Figures 1B-D, 2A). After that, dissection was done to the posterior leaf of the broad ligament until uterine vessels revealed, loop ligature of the isthmus uteri or transfixion of the uterine vessels was followed by coagulating of the uterine vessels using bipolar current (Figure 2B-D). The uterus will become notably ischemic and undergoing a marked color change if devascularization is completed successfully. Then a 22 mm morcellator was used to remove the uterine specimen from the cavity, the endocervix was coagulated with bipolar diathermy, cervix stump was reinforced for two more loop ligation or interrupted suture based on the different disposition of uterine vessels (Figure 3A-C). For total hysterectomy, the uterosacral and cardinal ligaments are dessicated and cut following the extraction of the uterine corpus. The vaginal vault is opened thus the specimen is detached completely. The vaginal cuff was closed using interrupted or running suture relied on the operator’s preferences. The left side of the procedure was carried out in the left trocar and likewise the right side of the procedure was carried out in the right with pulling the uterus to the opposite side. Operative time was calculated from the insertion of the trocar to skin closure of the last port site. Blood loss was estimated by the waste irrigation fluid volume (ml) minus the volume of normal saline used for irrigation (ml).
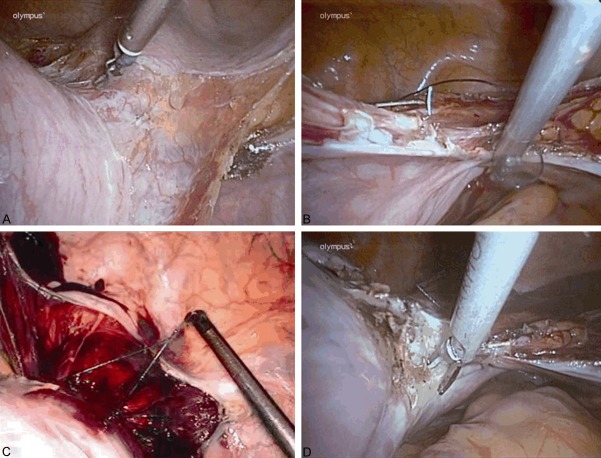
Figure 1.
A: The incision of the abdominal wall with the uterus weighing 1520 g; B: Laparoscopic subtotal hysterectomy for a uterus weighing 1082 g; C: Coagulation/section of the right utero-ovarian ligament using bipolar forceps. D: Opening the anterior/posterior leaf of the left broad ligament and the ascending branches of the uterus vessels can be seen clearly.
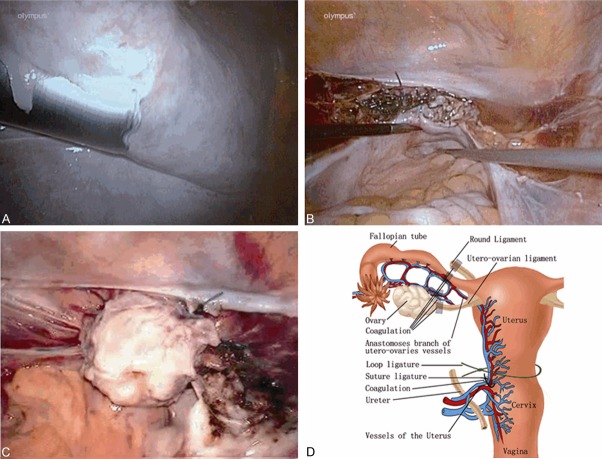
Figure 2.
A: Opening the uterovesical fold and dissecting the bladder from the cervix. B: Transfixion of the uterine vessels. C: Loop ligation of the isthmus uteri. D: Dissection of the uterine vessels and the uterus became notable color change.
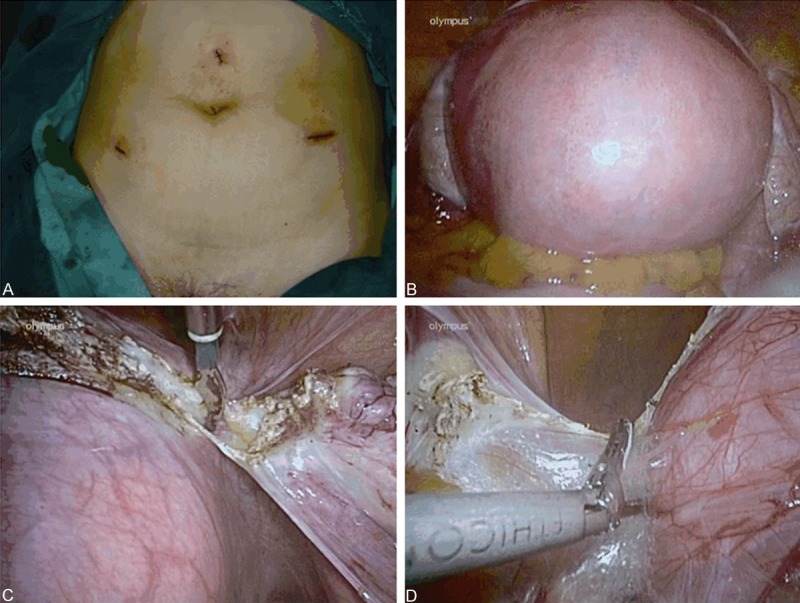
Figure 3.
A: Morcellation of the uterine specimen. B: The final look of the surgery by suturing. C: The final look of the surgery by loop ligation. D: Schematic diagram of the uterus and devascularization can be done in order according to the positions marked in the diagram.
Results
18 consecutive cases were included in the analysis (Table 1) and we didn’t have laparotomy on large uterus during the corresponding period. Mean age was 45.1±3.3 years (ranging from 39 to 53 years), mean BMI was 26.4±3.6 kg/m2 (ranging from 18.0 to 31.2 kg/m2), mean parity was 1.4±0.8 (ranging from 0 to 3). Previous surgeries included 5 cases of caesarean section and 1 case of adrenal surgery. There was an overlap of symptoms and the most common indication for hysterectomy was palpable mass in 55% (10/18) women, followed with menorrhagia in 45% (8/18) of women, urinary frequency was present in 28% (5/18) women; The mean time of the surgery was 107±29 min (ranging from 65 to180 min), the mean blood lost was 225±189 ml (ranging from 50 to 800 ml), the mean weight of the uterus was 1105±285 g (ranging from 820 to 1880 g), and the mean HGB drop was 0.9±0.5 g/dl (ranging from 0.2 to 1.9 g/dl). There was one patient who was midrange anemia before surgery bled as much as 800 ml intraoperatively and needed a blood transfusion; there was no bladder and ureter injury during the procedure, and none of them needed conversion to laparotomy (Table 2). Histopathological diagnosis included 14 cases of benign leiomyoma (14/18) and 4 cases of adenomyosis (4/18). All patients were followed up for at least six months after surgery and all recovered uneventfully.
Table 1.
Clinical characteristics of the 18 cases
| No. | Age (Y) | Parity (N) | Height (M) | BMI | Uterus size (W) |
|---|---|---|---|---|---|
| 1 | 43 | 1 | 1.53 | 24.7 | 18 |
| 2 | 39 | 0 | 1.58 | 22.0 | 20 |
| 3 | 46 | 2 | 1.60 | 19.5 | 18 |
| 4 | 43 | 1 | 1.53 | 27.7 | 20 |
| 5 | 53 | 1 | 1.68 | 18.0 | 22 |
| 6 | 50 | 3 | 1.56 | 24.6 | 24 |
| 7 | 45 | 2 | 1.54 | 28.2 | 22 |
| 8 | 46 | 1 | 1.55 | 31.2 | 26 |
| 9 | 43 | 1 | 1.60 | 29.6 | 18 |
| 10 | 44 | 1 | 1.52 | 25.1 | 22 |
| 11 | 47 | 2 | 1.58 | 30.0 | 24 |
| 12 | 42 | 1 | 1.55 | 27.0 | 20 |
| 13 | 48 | 3 | 1.59 | 25.3 | 24 |
| 14 | 43 | 2 | 1.53 | 29.9 | 24 |
| 15 | 42 | 1 | 1.55 | 29.1 | 22 |
| 16 | 46 | 1 | 1.62 | 28.1 | 22 |
| 17 | 47 | 1 | 1.56 | 26.7 | 20 |
| 18 | 43 | 1 | 1.60 | 28.5 | 26 |
| Mean ± SD | 45.1±3.3 | 1.4±0.8 | 1.57±0.04 | 26.4±3.6 | 21.7±2.6 |
BMI = body mass index.
Table 2.
Intra-and-postoperative data of the 18 cases
| No. | Operative time (min) | Blood loss (ml) | Resected Weight (g) | HGB Drop (g/dl) | I I | PHS (day) | HD | TS |
|---|---|---|---|---|---|---|---|---|
| 1 | 90 | 50 | 835 | 0.2 | 0 | 4 | Leiomyoma | LSH |
| 2 | 80 | 100 | 868 | 0.2 | 0 | 4.5 | Adenomyosis | LSH |
| 3 | 100 | 100 | 820 | 0.5 | 0 | 4 | Leiomyoma | LSH |
| 4 | 95 | 200 | 875 | 0.7 | 0 | 4 | Leiomyoma | LSH |
| 5 | 125 | 150 | 972 | 0.6 | 0 | 4 | Leiomyoma | LSH |
| 6 | 135 | 350 | 1200 | 1.1 | 0 | 4.5 | Adenomyosis | TLH |
| 7 | 105 | 200 | 1271 | 0.9 | 0 | 5 | Leiomyoma | LSH |
| 8 | 140 | 800 | 1880 | 1.9 | Bleeding | 6 | Leiomyoma | LSH |
| 9 | 87 | 50 | 880 | 0.6 | 0 | 4 | Leiomyoma | LSH |
| 10 | 140 | 250 | 1044 | 1.0 | 0 | 4.5 | Leiomyoma | LSH |
| 11 | 95 | 200 | 1082 | 1.2 | 0 | 4 | Leiomyoma | LSH |
| 12 | 70 | 50 | 822 | 0.9 | 0 | 4 | Adenomyosis | LSH |
| 13 | 120 | 200 | 1380 | 1.1 | 0 | 5 | Leiomyoma | LSH |
| 14 | 125 | 350 | 1344 | 1.2 | 0 | 5 | Adenomyosis | LSH |
| 15 | 87 | 300 | 1100 | 1.5 | 0 | 4 | Leiomyoma | LSH |
| 16 | 95 | 150 | 1039 | 0.5 | 0 | 4 | Leiomyoma | LSH |
| 17 | 65 | 50 | 965 | 0.4 | 0 | 4 | Leiomyoma | LSH |
| 18 | 180 | 500 | 1520 | 1.7 | 0 | 6 | Adenomyosis | TLH |
| Mean ± SD | 107±29 | 225±189 | 1105±285 | 0.9±0.5 | 4.5±0.6 |
No. = Number; I I = Introperative incident; PHS = Postoperative hospital stay; HD = Histopathological diagnosis; TS = Type of surgery; LSH = laparoscopic subtotal hysterectomy; TLH = total laparoscopic hysterectomy.
Discussion
The uterus is usually considered large when its size exceeds 12 weeks of gestation (280 g on average) [17]. Cases of large uteri have been considered a relative contraindication to laparoscopic hysterectomy due to limited visibility and access to uterine vascular associated with the high risk of complications such as hemorrhage, bowel and urinary injury, difficulty in extracting the uterus and extended duration of the procedure as well as highly occurrence of conversion to laparotomy [14]. As such, most studies set an upper limit of laparoscopic hysterectomy for 15 to 16 weeks gestation.
With the improvements of laparoscopic techniques and the advent of morcellators in the latest years, clinical feasibility and practicality of laparoscopic surgery to remove enlarged uteri has been demonstrated. But there are few articles in the literature to addressing laparoscopic hysterectomy for uteri more than 800g, and most of these literatures had some limitations, such as long operative time as much as 6 hours, pelvic cellulitis, intraoperative bleeding that needs converting to open surgery, bladder or bowel injury [13-15]. These procedures usually need at least 4 ports during the surgery and some of the procedures were laparoscopically assisted vaginal hysterectomy. The size of the uterus seems to be an important factor for the occurrence of intraoperative hemorrhage and intra-and-postoperative complications during laparoscopic hysterectomy, especially when performed on uterus larger than 500 g. In our opinion, there are three key points to consider to performing such surgery successfully.
The first is to choose a suitable site to place the trocar. Suitable trocar position provides sufficient view of operation field and adequate range of motion for instruments which help to facilitate the operation. Kai-Yun Wu, et al [18], suggested that the higher the first trocar is, the better the operation field, and the primary trocar should be placed at least 8 cm higher than the uterus fundus, which is different from ours. According to our experience, for those fundus which were at the level below or equal to the umbilicus, we choose the umbilicus as the first site, and for those above the umbilicus, the first site was located in median line 3-6 cm higher than the umbilicus in light of individual patient for a sufficient view of operation field. The distance between the umbilicus and the xiphoid bone is about 10-12 cm, for those fundus which were at the level above the umbilicus, there were almost nowhere to place the trocar if at least 8 cm higher than the uterus fundus should be maintained. In addition, the distant first site made it difficult in dealing with the uterus vessels and cervix. As for the assistant trocars, the position was depended on the level where the adnexa located on after elevating the uterus. Usually, 2 cm higher than the level helps to facilitate coagulating the utero-ovarian vessels, round ligament and the tube.
The second key point for such surgery should be how to reduce intraoperative blood loss. In regarding to this, two aspects should be concerned. Firstly, it requires exposing and maintaining an as good as possible operation field. Large uterus take up most of the pelvic volume, which make visibility limited and instrument range of motion restrictive. Good exposure not only reduced blood lost but also the operation time and thus in return reduces the likelihood of intra-and-post operation complications. Usually, a 30 degree laparoscope may help seeing around so that important structures and vascular pedicles can be visualized and dealt with. And when perform the surgery, the left side of the procedure should be carried out in the left trocar, with a grasp clamp help pulling the uterus to the right side and the patient was leaned to the right side to facilitate exposure the left field, and likewise the right side. Additional trocars usually couldn’t provide more help for the procedure on account of limited space. Secondly, complete devascularization, mechanical or pharmacologic methods can be used to prevent or decrease the bleeding. Large uterus usually got obvious thickening vessels. Once the veins are broken, it is difficulty to stop bleeding by electric coagulation, so the critical step for devascularization is elaborative dissection and blocking of the vessels. As the picture shows (Figure 3D), the blood supply to the uterus originates from the uterine artery. Bilateral anastomoses branch of the uterine and the ovarian arteries supply to the tube and tubal part of the uterus. Thus the vessels mentioned above were the key points of devascularization, especially the anastomoses branch of the uterus and the ovarian arteries. They were surrounded by round ligament, ovarian ligament and fallopian tubes which often form generous structure that is not conducive to direct coagulation of the vessels. Prior to dealing with the anastomoses branch, bipolar desiccation and dissecting of the round ligament, the tubal isthmus and part of the utero-ovarian ligament was more conducive to avoid bleeding. The good deal of the anastomoses branch is a prerequisite for the clear field of the following surgery. For exact devascularization of the Utero-ovaries anastomoses branch using coagulation, cut the vessels far away from the uterus side as possible, and then open the anterior and posterior leaf of the peritoneum. Care should be taken to avoid broking the ascending branch of the uterus vessels. The uterovesical fold was then opened and bladder reflected downwards, so that the paracervical vascular bundles could be exposed clearly, and devascularization can be completed by loop ligation or suture. Should the major vessels bleeding during the procedure, the most important thing is to dissect and separate the paracervix fast and followed with loop ligation, while coagulation is usually ineffective. Some studies also reported that selective coagulation of the uterine artery at its origin avoids unexpected perioperative hemorrhage and allows safe laparoscopic hysterectomy in enlarged uterus [19]. However, this is usually not easy to operate especially in uterus larger than 16 gestational weeks.
The third is to remove the specimen effectively. Usually most of the time was spent on the removal of the large specimen. It is important to use a big cannula diameter morcellator for morcellation, and if available, 20-mm or more will be preferred. As for total hysterectomy, specimen can be first morcellated for volume reduction, and removed through the trocar, after cervix stump excision, the rest specimen can be removed through the vagina. Some studies reports that small fragment may be dispersed throughout the peritoneal cavity during morecellation, which it seems a negative impact on the prognosis of patients, especially on those who are presenting with undetected leiomyosarcoma [20,21]. This prompted the FDA to issue a warning about potential risks associated with morecellation. Uterine leiomyosarcoma is a particular subtype of uterine sarcoma which is more likely to affect perimenopausal women around 50 years. Because there are no specific clinical or paraclinical pre-operative signs to evoke uterine leiomyosarcoma, these tumors usually are identified incidentally after review of the surgical specimen [22]. Three large series found that the rates of incidental leiomyosarcoma in patients undergoing surgery for presumed leiomyomas is extremely low, ranging from 0.08% to 0.49% [23-25]. And thus in our opinion, the concern about leiomyosarcoma, especially in young patients, should not be a criterion to avoid less invasive non-laparotomic surgical route, and alternative methods such as the usage of endoscopic bag and routine endometrial sampling may help reducing the risk.
The main difference with previous studies is that we only used three trocars to perform the surgery safely. All of the 18 consecutive cases were successfully completed by laparoscopy. There was no major complication such as bladder and ureter injury during the procedure, and none of them needed conversion to laparotomy. Potential weaknesses of this study were the small number of the patients and the retrospective nature of the study. According to our studies, based on appropriate techniques and careful operation, Laparoscopic hysterectomies for large uteri using three-trocar is safe and feasible if the strategies mentioned above were strictly followed to most of the patients.
Acknowledgements
We are grateful to Suneng Fu for his excellent work in English proofreading.
Disclosure of conflict of interest
None.
References
- 1.Donnez J, Nisolle M. Laparoscopic supracervical (subtotal) hysterectomy (LASH) J Gynecol Surg. 1993;9:91–4. doi: 10.1089/gyn.1993.9.91. [DOI] [PubMed] [Google Scholar]
- 2.Kovac SR. Hysterectomy outcomes in patients with similar indications. Obstet Gynecol. 2000;95:787–93. doi: 10.1016/s0029-7844(99)00641-9. [DOI] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists. ACOG Committee Opinion. Number 311, April 2005. Appropriate use of laparoscopically assisted vaginal hysterectomy. Obstet Gynecol. 2005;105:929–30. doi: 10.1097/00006250-200504000-00059. [DOI] [PubMed] [Google Scholar]
- 4.Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, van Voorst S, Mol BW, Kluivers KB. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;8:CD003677. doi: 10.1002/14651858.CD003677.pub4. [DOI] [PubMed] [Google Scholar]
- 5.Köhler C, Hasenbein K, Klemm P, Tozzi R, Schneider A. Laparoscopic-assisted vaginal hysterectomy with lateral transsection of the uterine vessels. Surg Endosc. 2003;17:485–90. doi: 10.1007/s00464-002-9091-4. [DOI] [PubMed] [Google Scholar]
- 6.Hillis SD, Marchbanks PA, Peterson HB. Uterine size and risk of complications among women undergoing abdominal hysterectomy for leiomyomas. Obstet Gynecol. 1996;87:539–43. doi: 10.1016/0029-7844(95)00478-5. [DOI] [PubMed] [Google Scholar]
- 7.Unger JB. Vaginal hysterectomy for the woman with a moderately enlarged uterus weighing 200 to 700 grams. Am J Obstet Gynecol. 1999;180:1337–44. doi: 10.1016/s0002-9378(99)70016-5. [DOI] [PubMed] [Google Scholar]
- 8.Ferrari MM, Berlanda N, Mezzopane R, Ragusa G, Cavallo M, Pardi G. Identifying the indications for laparoscopically assisted vaginal hysterectomy: a prospective, randomised comparison with abdominal hyster-ectomy in patients with symptomatic uterine fibroids. BJOG. 2000;107:620–5. doi: 10.1111/j.1471-0528.2000.tb13303.x. [DOI] [PubMed] [Google Scholar]
- 9.Salmanli N, Maher P. Laparoscopically-assisted vaginal hysterectomy for fibroid uteri weighing at least 500 grammes. Aust N Z J Obstet Gynaecol. 1999;39:182–4. doi: 10.1111/j.1479-828x.1999.tb03367.x. [DOI] [PubMed] [Google Scholar]
- 10.Switala I, Cosson M, Lanvin D, Querleu D, Crepin G. Is vaginal hysterectomy important for large uterus of more than 500 g? Comparison with laparotomy. J Gynecol Obstet Biol Reprod (Paris) 1998;27:585–92. [PubMed] [Google Scholar]
- 11.Pelosi MA, Kadar N. Laparoscopically assisted hysterectomy for uteri weighing 500 g or more. J Am Assoc Gynecol Laparosc. 1994;1:405–9. doi: 10.1016/s1074-3804(05)80808-4. [DOI] [PubMed] [Google Scholar]
- 12.Wang CJ, Yen CF, Lee CL, Tashi T, Soong YK. Laparoscopically assisted vaginal hysterectomy for large uterus: a comparative study. Eur J Obstet Gynecol Reprod Biol. 2004;115:219–23. doi: 10.1016/j.ejogrb.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 13.Demir RH, Marchand GJ. Safe laparoscopic removal of a 3200 gram fibroid uterus. JSLS. 2010;14:600–2. doi: 10.4293/108680810X12924466008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walid MS, Heaton RL. Laparoscopic extirpation of a 3-kg uterus. Arch Gynecol Obstet. 2009;279:607–8. doi: 10.1007/s00404-008-0827-9. [DOI] [PubMed] [Google Scholar]
- 15.Walid MS, Heaton RL. Total laparoscopic hysterectomy for uteri over one kilogram. JSLS. 2010;14:178–82. doi: 10.4293/108680810X12785289143837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kondo W, Bourdel N, Marengo F, Botchorishvili R, Pouly JL, Jardon K, Rabischong B, Mage G, Canis M. Is laparoscopic hysterectomy feasible for uteri larger than 1000 g? Eur J Obstet Gynecol Reprod Biol. 2011;158:76–81. doi: 10.1016/j.ejogrb.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 17.Daraï E, Soriano D, Kimata P, Laplace C, Lecuru F. Vaginal hysterectomy for enlarged uteri, with or without laparoscopic assistance: randomized study. Obstet Gynecol. 2001;97:712–6. [PubMed] [Google Scholar]
- 18.Wu KY, Lertvikool S, Huang KG, Su H, Yen CF, Lee CL. Laparoscopic hysterectomies for large uteri. Taiwan J Obstet Gynecol. 2011;50:411–4. doi: 10.1016/j.tjog.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Roman H, Zanati J, Friederich L, Resch B, Lena E, Marpeau L. Laparoscopic hysterectomy of large uteri with uterine artery coagulation at its origin. JSLS. 2008;12:25–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Kho KA, Nezhat CH. Evaluating the risks of electric uterine morcellation. JAMA. 2014;311:905–6. doi: 10.1001/jama.2014.1093. [DOI] [PubMed] [Google Scholar]
- 21.Park JY, Park SK, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol. 2011;122:255–9. doi: 10.1016/j.ygyno.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 22.Leung F, Terzibachian JJ. Re: “The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma”. Gynecol Oncol. 2012;124:172–3. doi: 10.1016/j.ygyno.2011.08.035. [DOI] [PubMed] [Google Scholar]
- 23.Parker WH, Fu YS, Berek JS. Uterine sarcoma in patients operated on for presumed leiomyoma and rapidly growing leiomyoma. Obstet Gynecol. 1994;83:414–8. [PubMed] [Google Scholar]
- 24.Leung F, Terzibachian JJ, Gay C, Chung Fat B, Aouar Z, Lassabe C, Maillet R, Riethmuller D. Hysterectomies performed for presumed leiomyomas: should the fear of leiomyosarcoma make us apprehend non laparotomic surgical routes? Gynecol Obstet Fertil. 2009;37:109–14. doi: 10.1016/j.gyobfe.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 25.Leibsohn S, d’Ablaing G, Mishell DR Jr, Schlaerth JB. Leiomyosarcoma in a series of hysterectomies performed for presumed uterine leiomyomas. Am J Obstet Gynecol. 1990;162:968–74. doi: 10.1016/0002-9378(90)91298-q. [DOI] [PubMed] [Google Scholar]