Abstract
Introduction
There is paucity of data on Quality of Life (QOL) in non-psychotic mental disorders.
Aim
To assess the Quality of Life (QOL) in Obsessive Compulsive Disorder (OCD) and compare it with Dysthymic Disorder (DD).
Materials and Methods
This hospital based cross-sectional study was conducted in 30 patients each diagnosed to have OCD and DD during October 2009 to September 2011 in a medical institution in Davanagere, Karnataka, India. DSM-IV-TR (Diagnostic statistical manual-IV-Text Revised) criteria was used for diagnosis of OCD and DD. Yale Brown Obsessive Compulsive Scale (Y-BOCS) and WHO QOL BREF (brief form) scales were used. Data was analysed by independent sample t-test.
Results
Overall QOL score was 51.07(SD=11.47) and 50.91(SD=7.41) in OCD and DD groups respectively. QOL score was comparatively low in psychological domain with score of 44.12(SD=14.14) and 45.10(12.35) in OCD and DD respectively. There was no significant difference in the QOL score of the two groups with respect to socio demographic variables in OCD group, but it was different with respect to place of residence in DD group (p<0.05). In Q1(perception on quality of life) and Q2 (perception on quality of health) domain, QOL score was marginally higher than average in both the groups. In Y-BOCS scale, no statistical significant association was found between severity of OCD and QOL score in each of the domains (p>0.05).
Conclusion
Overall QOL score was average and there was no significant difference of QOL score between the OCD and DD groups implying that both these non-psychotic mental disorders may have same influence or effect on QOL of the subjects. Further analytical studies will explore the associated factors of QOL in OCD and DD.
Keywords: QOL score, WHO QOL BREF, Y-BOCS Scale
Introduction
According to World Health Organisation, Quality of Life (QOL) is an individual’s perception of their position in life in the context and value system in which they live and in relation to their goals, expectations, standards and concern [1]. QOL is impaired in Schizophrenia and in mood disorders such as major depression, DD, minor depression and anxiety disorders like generalized anxiety disorder, panic disorder and post traumatic stress disorder [2,3]. DD per se was associated with lesser impairment of QOL as compared to other mood disorders [3]. Alcohol use disorder is associated with lower levels of QOL as compared to general population [4]. OCD as a disorder has marked impact on QOL in mental health domains like social functioning, role limitation due to emotional problems and mental health comparable to depressive disorders [5]. In OCD, severity of obsessions and co morbid depression predict poor QOL [6]. But, Indian studies are lacking in this area.
There is paucity of Indian literature in the assessment of QOL in non psychotic illnesses. Hence the present study is planned to assess QOL in OCD and compare it with another non psychotic illness, DD.
Materials and Methods
Setting and Sample size
The present cross-sectional hospital based study was conducted from October 2009 to September 2011 in a medical institution in Davanagere, Karnataka, India. We selected 30 patients each diagnosed to have OCD and DD. Consecutive sampling method was used to select the study subjects.
Inclusion and Exclusion criteria
All the subjects between 18-45 y age group with duration of at least two years illness period were included in the study. Patients having co morbid Organic Brain Syndromes, Psychosis, BPAD (Bipolar affective Disorder), MDD, (Major Depressive Disorder) Alcohol and substance dependence, Personality disorder and Mental retardation, patients having concomitant chronic physical illness, past history of psychiatric illness and family history of psychiatric illness were excluded from the study.
Ethical issues
The study was approved by the ethical committee of the medical institution. Informed consent was obtained from the subjects after explaining the details to subject. In case the subject was unable to give consent, it was obtained from the guardian.
Study tools
1. DSM-IV-TR criteria was used for diagnosis of OCD and DD [7,8].
Obsessions as defined by following 4 criteria:
1. Recurrent and persistent thoughts, impulses or images that are experienced , at some time during the disturbance, as intrusive and inappropriate and that cause marked anxiety and distress.
2. The thoughts, impulses or images are not simply excessive worries about real life problems.
3. The person attempts to ignore or suppress such thoughts, impulses or images or to neutralize them with some other thought or action.
4. The person recognizes that the obsessional thoughts, impulses or images are a product of his or her own mind.
Compulsions as defined by following two criteria
1. Repetitive behaviour (e.g. hand washing, ordering, checking) or mental acts (eg:- praying, counting, repeating words silently) that the person feels driven to perform in response to an obsession, or according to rules that must be applied rigidly.
2. The behaviours or mental acts are aimed at preventing or reducing distress or preventing some dreaded event or situation; however , these behaviours or mental acts either are not connected in a realistic way with what they are designated to neutralize or prevent or are clearly excessive.
DSM-IV-TR criteria for Dysthymic Disorder [7].
Depressed mood for most of the day, for more days than not, as indicated either by subjective account or observation by others, for at least two years. In children and adolescents, mood can be irritable and duration must be at least one year.
2. WHO QOL-BREF [9]: It was used to assess the QOL in OCD and DD. It consists of four domains namely physical, psychological, social relationship and environmental. Each domain consists of 7, 3, 6 and 8 questions respectively with a total of 24 questions. The mean score of items within each domain is used to calculate the domain score. Total score for each domain after transformation ranges from 1 to 100. Overall total average score and Standard Deviation of physical, psychological, social relationship and environmental domains was calculated. There are also two single question items that are examined separately. Q1 is about an individual’s overall perception of quality of life and Q2 is about his perception of overall quality of health. It is easy to administer and this questionnaire was translated to Kannada and back translated to English by independent experts to assess the reliability of the instrument. Pilot-test was done before the survey. Domain scales are scaled in positive direction i.e, higher scores denotes higher quality of life.
3. Y Y-BOCS scale [10]: It was used to assess the Obsession and compulsion and categorized into mild, moderate and severe with scores of 0-13, 14-26, 27-40 respectively. The Y-BOCS scale ratings do not depend on specific types of symptoms like washing, checking or counting, but are instead based on aspects of those symptoms as reported by the patient during the interview like duration, interference, degree of resistance. The scale is divided into two parts of five questions each, the Obsessions subscale and the Compulsions subscale. On each subscale five aspects of pathology are rated on scales ranging from 0 (no symptoms) to 4 (extreme symptoms): (1) time spent, (2) degree of interference, (3) distress, (4) resistance, and (5) perceived control over the symptom. Unlike some other OCD measures, the YBOCS assigns lower scores to greater resistance as an indicator of health. Scores obtained from the subscales are summed to yield a YBOCS total score.
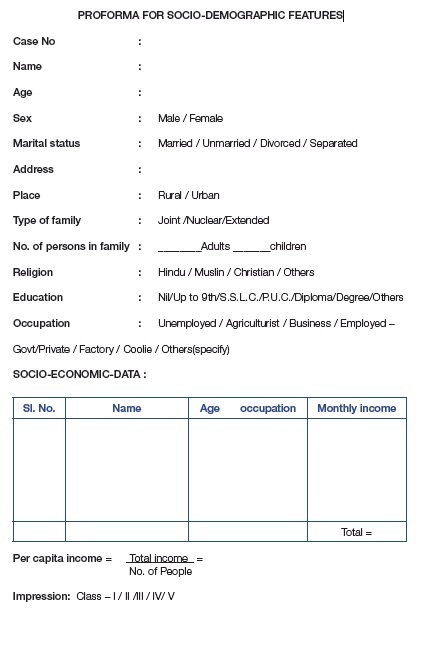
Method of data collection
The data was collected from the study subjects regarding socio-demographic details like age, sex, urban/rural, address, type of family, number of persons in the family, education, occupation, and income of family from all sources by interviewing the patient using a standard structured questionnaire. Socio economic status was assessed by modified Prasad classification scale [11,12]. This was followed by the administration of WHO QOL BREF scale and Y-BOCS scale.
Statistical Analysis
The data was entered in Statistical Package for Social Sciences (SPSS) version 16. For Continuous data, independent sample t-test was used. Information was depicted in proportion, mean score value and its standard deviation (SD) and 95% confidence interval. P-value less than 0.05 was considered as significant.
Results
QOL measured in the domains of Q1, Q2, physical, psychological, social and environmental domains and total QOL score did not differ between the OCD and the DD group. But psychological domain score was low in both the groups compared to other domain scores. Total QOL score was found to be average in both OCD and DD [Table/Fig-1].
[Table/Fig-1]:
Comparison of QOL Score in OCD and DD
| WHOQOL-BREF Domains | OCD (SD), N=30 | DD(SD), N=30 | t-value, p-value |
|---|---|---|---|
| Q1 | 3.10(1.09) | 3.03 (0.99) | 0.246, 0.806 |
| Q2 | 3.13(0.97) | 2.83(0.79) | 1.310, 0.195 |
| Physical | 55.60(11.59) | 52.0(10.67) | 1.252, 0.216 |
| Psychological | 44.12(14.14) | 45.10(12.35) | 0.272, 0.786 |
| Social | 49.63(17.85) | 55.63(14.09) | 1.445, 0.154 |
| Environmental | 54.87(12.57) | 50.90(10.34) | 1.335, 0.187 |
| Total average QOL score (Excluding Q1 and Q2) | 51.07(11.47) | 50.91(7.41) | 0.063, 0.958 |
p-value less than 0.05 is considered as significant
There was no significant difference in the QOL of the two groups with respect to socio demographic variables [Table/Fig-2]. In DD, place of residence was associated with QOL score [Table/Fig-3]. The QOL in the Y-BOCS scale has not shown statistically significant difference in the domains of QOL [Table/Fig-4].
[Table/Fig-2]:
Comparison of socio-demographic features and QOL transformed score in OCD
| Socio-demographic Features in OCD | Mean Score (SD) | t-value, p-value | |
|---|---|---|---|
| Age | ≤30 years (n=22) | 51.11 (10.65) | 0.037, 0.971 |
| >30 years (n=8) | 50.94 (14.31) | ||
| Sex | Male(n=14) | 52.38 (9.99) | 0.577, 0.568 |
| Female (n=16) | 49.92 (12.84) | ||
| Place | Urban (n=23) | 50.93 (10.74) | 0.112, 0.911 |
| Rural (n=7) | 51.50 (14.58) | ||
| Education | ≤10th class(n=10) | 47.50 (6.95) | 1.214, 0.235 |
| >10th class (n=20) | 52.85 (12.96) | ||
| Marital Status | Married (n=15) | 49.10 (12.88) | 0.937, 0.357 |
| Unmarried (n=15) | 53.03 (9.91) | ||
| Socio Economic Class | Higher Class: Catagory 1 and 2 (n=11) | 52.61 (14.03) | 0.555, 0.583 |
| Lower class -Category 3,4 and 5 (n=19) | 50.17 (10.02) | ||
p-value less than 0.05 is considered as significant
[Table/Fig-3]:
Comparison of socio-demographic features and QOL transformed score in DD
| Socio-demographic Features | Mean Score (SD) | t-value, p-value | |
|---|---|---|---|
| Age | ≤30 years (n=16) | 51.23(8.61) | 0.253, 0.802 |
| >30 years (n=14) | 50.54(6.06) | ||
| Sex | Male (n=12) | 52.73(6.68) | 1.102, 0.280 |
| Female (18) | 49.69(7.81) | ||
| Place | Urban (n=16) | 53.39(7.76) | 2.068, 0.048* |
| Rural (n=14) | 48.07(6.08) | ||
| Education | ≤10th class | 49.85(6.22) | 1.310, 0.201 |
| >10th class (n=20) | 53.81(9.92) | ||
| Marital Status | Married (n=21) | 49.92(6.37) | 1.124, 0.270 |
| Unmarried(n=9) | 53.22(9.45) | ||
| Socioeconomic Status in OCDD | Higher Class- Category 1 and 2 (n=7) | 46.89(7.08) | 1.688, 0.103 |
| Lower class-Category 3,4 and 5 (n=23) | 52.13(7.22) | ||
*p-value less than 0.05 is considered as significant
[Table/Fig-4]:
Severity of illness in OCD and QOL score
| WHOQOL-BREF Domains | Y-BOCS Moderate (n=15) | Y-BOCS Severe (n=15) | t-value, p-value |
|---|---|---|---|
| Q1 | 3.47(0.99) | 2.73(1.10) | 1.919, 0.065 |
| Q2 | 3.00(0.85) | 3.27(1.10) | 0.745, 0.463 |
| Physical | 56.80(13.09) | 54.40(10.19) | 0.560, 0.580 |
| Psychological | 45.67(15.44) | 42.67(13.07) | 0.574, 0.570 |
| Social | 55.07(18.13) | 44.20(16.37) | 1.723, 0.096 |
| Environmental | 55.93(12.50) | 53.80(12.98) | 0.458, 0.650 |
| Total average QOL score (Excluding Q1 and Q2) | 53.37(12.22) | 48.77(10.59) | 1.102, 0.280 |
Not significant when p-value > 0.05
Discussion
In the present study QOL measured in the domains of Q1, Q2, physical, psychological, social and environmental domains that did not differ between the OCD and the DD group in a statistically significant manner. There is paucity of literature in this area. But there are studies reported on assessment of QOL conducted among OCD and DD subjects separately as discussed below [13-25].
In OCD, QOL in psychological and social domain could be relatively more affected than other domains because of the internal distress caused by obsessions and compulsions similar to another Indian study [13], which showed the QOL mean score as Physical-51.84 (SD=19.9), Psychological- 35.60 (SD=14.9), Social-39.53(SD=16.3), and Environmental-59.74 (SD=12.2). Here, psychological and social domains were more affected than our study. Environmental domain of QOL was not impaired much because OCD being a non-psychotic disorder, there is not much difficulty in meeting ordinary demands of life. Studies have shown the poor QOL in OCD patients across a wide range of domains in particularly social and mental health aspects [14].
Our study did not find the relation of obsession and compulsion with QOL. Evidence is less regarding the relation of obsession and compulsion on QOL although it is strongly correlated with some studies [14]. It has shown that compulsions reduced patient’s QOL in the physical, psychological and environmental domains, whereas obsessions did not have any impact on QOL ratings [15]. Also, it was found that compared with that of the general population, the QOL of relatives of patients with OCD was significantly lower in the domains physical and psychological well-being, and social relationship [16].
A study has shown that multiple factors were associated with poor QOL in subjects with OCD like depression, severity of obsession symptoms, perceived low social support, severe adverse effects of medication, combined use of mood stabilizers and low social status [17]. Thus different domains of QOL may be differently affected by OCD. Studies which used SF-36 showed that the severity of the obsessive-compulsive disorder was correlated with QOL [18,19]. A study showed that severity of obsessions and depressive symptoms were significant predictors of impairment in QOL in contrast to our study [20]. This may be because of other influencing factors. It was shown that QOL scores were significantly lower for the OCD patients both before and after treatment, but improved significantly during treatment [21]. The severity of impairment of QOL in OCD equalled that of impairment in schizophrenia [22,23]. Also, individuals who are in remission have improved levels of QOL and functioning, whereas individuals with OCD are significantly impaired, and individuals with OCD and comorbid disorders are the most impaired [21].
But, in DD subjects, QOL in physical domain could be relatively more impaired compared to OCD because of the somatic preoccupation in DD where in the patients perceives the somatic symptoms as being physical in origin which interfere in leading and experiencing a normal life. A study highlighted that different domains of QOL are differently affected by depressive disorders and depressive subjects had poorer QOL on the physical, psychological and social relationship domains than the non-depressive control group [24]. Subjects with bipolar disorder in remission had similarly poor levels of QOL in all four domains as those subjects with schizophrenia in remission [25]. In view of the above finding, it is important to look for all the contextual factors affecting the QOL in DD.
The present study has got its own limitations. Hospital based study may not represent the homogeneity of the population in the community. Contextual factors affecting OCD and DD were not collected and analysed due to feasibility constraints. In spite of these limitations, it gives valuable information on the comparison of QOL scores in all the domains and certain associated factors. Further analytical studies will explore the different factors associated with QOL in OCD and DD.
Conclusion
Overall QOL score was average and there was no significant difference of QOL score between OCD and DD groups implying that both these non-psychotic mental disorders may have same influence or effect on QOL of the subjects. Further analytical multi-centric studies will help in understanding the associated factors of QOL in OCD and DD.
Annexure-II
Annexure-II.
Financial or Other Competing Interests
None.
References
- [1].S Saxena. New Delhi: Byword Viva Publishersl; 2005. Functioning disability and quality of life assessment in mental health. ]in: Bhugra D, Ranjith G, Patel V(Eds.) Handbook of Psychiatry: a South Asian perspective. [Google Scholar]
- [2].RK Solanki, P Singh, A Midha, K Chugh. Schizophrenia: Impact of quality life. Indian J Psychiatry. 2008;50:181–86. doi: 10.4103/0019-5545.43632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].RL Spitzer, K Kroenke, M Linzer, SR Hahn, BW Williams, FV De Gruy, et al. Health Related Quality Of Life In Primary care patients with mental disorders. JAMA. 1995;274:1511–17. [PubMed] [Google Scholar]
- [4].D Donovan, ME Mattson, RA Cisler, R Longbaugh, A Zweben. Quality of life as an outcome measure in alcoholism treatment research. J Stud Alcohol Suppl. 2005;15:119–39. doi: 10.15288/jsas.2005.s15.119. [DOI] [PubMed] [Google Scholar]
- [5].LM Koran, ML Thienemann, R Davenportn. Quality of life for patients with obsessive- compulsive disorder. Am J Psychiatry. 1996;153:783–88. doi: 10.1176/ajp.153.6.783. [DOI] [PubMed] [Google Scholar]
- [6].M Masellis, N A Rector, MA Richter. Quality of life in OCD: Differential Impact of Obssession, Compulsions and Depression Comorbidit. Can J Psychiatry. 2003;48:72–77. doi: 10.1177/070674370304800202. [DOI] [PubMed] [Google Scholar]
- [7]. IV-TR Mood Disorders Available from: http://www.ncbi.nlm.nih.gov/[7]books/NBK64063/
- [8]. Diagnostic Criteria for 300.3 Obsessive-Compulsive Disorder. Available from: http://behavenet.com/node/21592.
- [9]. WHO QOL BREF- Field Trial Version December 1996. Available from http://www.who.int/mental_health/media/en/76.pdf.
- [10].Woody Sheila R , Steketee Gail, Chambless Dianne L. Reliability and validity of the Yale Brown Obsessive Compulsive scale. Behav. Res. Ther. 1995;33(5):597–605. doi: 10.1016/0005-7967(94)00076-v. [DOI] [PubMed] [Google Scholar]
- [11].BG Prasad. Social classification of Indian families. J Indian Med Assoc. 1970;55:98–199. [PubMed] [Google Scholar]
- [12].AK Agarwal. Social Classification: The need to update in the present scenario. Indian J Community Med. 2008;33:50–51. doi: 10.4103/0970-0218.39245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].GP Gururaj, SB Math, JY Reddy, CR Chandrashekar. Family burden, quality of life and disability in obsessive compulsive disorder: an Indian perspective. J Postgrad Med. 2008;54:91–97. doi: 10.4103/0022-3859.40773. [DOI] [PubMed] [Google Scholar]
- [14].SA Moritz. Review on quality of life and depression in obsessive-compulsive disorder. CNS Spectr. 2008;13(9 Suppl 14):16–22. doi: 10.1017/s1092852900026894. [DOI] [PubMed] [Google Scholar]
- [15].K Stengler-Wenzke, M Kroll, S Riedel-Heller, H Matschinger, MC Angermeyer. Quality of life in obsessive–compulsive disorder: the different impact of obsessions and compulsions. Psychopathology. 2007;40:282–89. doi: 10.1159/000104744. [DOI] [PubMed] [Google Scholar]
- [16].K Stengler-Wenzke, M Kroll, H Matschinger, MC Angermeyer. Quality of life of relatives of patients with obsessive-compulsive disorder. Psychiatry. 2006;47:523–27. doi: 10.1016/j.comppsych.2006.02.002. [DOI] [PubMed] [Google Scholar]
- [17].SY Hou, CF Yen, MF Huang, PW Wang, YC Yeh. Quality of life and its correlates in patients with obsessive-compulsive disorder. Kaohsiung J Med Sci. 2010;26:397–407. doi: 10.1016/S1607-551X(10)70065-6. [DOI] [PubMed] [Google Scholar]
- [18].B Rodriguez-Salgado, H Dolengevich-Segal, M Arrojo-Romero, P Castelli-Candia, M Navio-Acosta , MM Perez-Rodriguez, et al. Perceived quality of life in obsessive-compulsive disorder: related factors. BMC Psychiatry. 2006;6:20. doi: 10.1186/1471-244X-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].U Albert, G Maina, F Bogetto, A Chiarle, D Mataix-Cols. Clinical predictors of health- related quality of life in obsessive-compulsive. Compr Psychiatry. 2010;51:193–200. doi: 10.1016/j.comppsych.2009.03.004. [DOI] [PubMed] [Google Scholar]
- [20].Eisena Jane L , Manceboa Maria A , Pintoa Anthony, Colesb Meredith E, Paganoa Maria E, Stouta Robert. Impact of obsessive-compulsive disorder on quality of life. Comprehensive Psychiatry. 2006;47:270–75. doi: 10.1016/j.comppsych.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].JD Huppert, HB Simpson, KJ Nissenson, MR Liebowitz, EB Foa. Quality of life and functional impairment in obsessive-compulsive disorder: a comparison of patients with and without comorbidity, patients in remission, and healthy controls. Depress Anxiety. 2009;26:39–45. doi: 10.1002/da.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].A Bystritsky, RP Liberman, S Hwang, CJ Wallace, T Vapnik, K Maindment, et al. Social functioning and quality of life comparisons between obsessive- compulsive and schizophrenic disorders. Depress Anxiety. 2001;14:214–18. doi: 10.1002/da.1069. [DOI] [PubMed] [Google Scholar]
- [23].J Bobes, MP González, C Bascarán, MT Arango, M Sáiz, PA Bousoño. Quality of life and disability in patients with obsessive-compulsive disorder. Compr Psychiatry. 2010;51:193–200. doi: 10.1016/j.comppsych.2009.03.004. [DOI] [PubMed] [Google Scholar]
- [24].CF Yen, CP Cheng, CF Huang, JY Yen, CH Ko, CS Chen. Quality of life and its association with insight, adverse effects of medication and use of atypical antipsychotics in patients with bipolar disorder and schizophrenia in remission. Bipolar Disord. 2008;10:617–24. doi: 10.1111/j.1399-5618.2007.00577.x. [DOI] [PubMed] [Google Scholar]
- [25].CF Yen, CC Chen, Y Tang, TC Ko, CH Yen. Association between quality of life and self-stigma, insight, and adverse effects of medication in patients with depressive disorders. Depress Anxiety. 2009;26:1033–39. doi: 10.1002/da.20413. [DOI] [PubMed] [Google Scholar]


