Abstract
Surgical literature defines the case of acute appendicitis in a sac of femoral hernia as de Garengeot’s hernia. The diagnosis remains a very hard challenge for surgeon because the symptoms are aspecific and the most effective tools for preoperative evaluation (as abdominal computed tomography and abdominal ultrasound scan) can often be indeterminate or misinterpreted. We report the case of an 85-year-old white male admitted to our unit complaining of a 1-day history of vague abdominal pain, nausea, vomiting, and painful swelling in the right groin. Preoperatively, an incarcerated right femoral hernia was supposed and patient underwent surgery via oblique inguinal incision. The intraoperative finding was a de Garengeot’s hernia and an appendectomy with hernia repair was performed. Patient had a regular course and was discharged on the second postoperative day.
Keywords: de Garengeot’s hernia, Incarceration, Appendicitis, Femoral hernia
Introduction
The femoral hernias account for less than 3 % of all hernias, have a rate of incarceration ranging between 5 and 20 %, and their content is typically omentum [1].
In anecdotal cases, the contents include other organs such as Meckel’s diverticulum, stomach, ovary, small bowel, and appendix [2, 3].
The case of acute appendicitis in a sac of femoral hernia is defined as de Garengeot’s hernia [1–8]. In fact, in 2005, Akopian and Alexander proposed to name this condition by Rene Jacques Croissant de Garengeot, the Parisian surgeon who first described an appendix without inflammation signs in a femoral hernia in 1731 [8].
In 1785, Hevin was the first to describe an appendectomy for acute appendicitis in a femoral hernia; only about 100 cases are reported to date [3, 5, 8].
Case Report
An 85-year-old white male was admitted to our unit complaining of vague abdominal pain, nausea, vomiting, and painful swelling in the right groin for 1 day. The medical history of patient reported hypertension, bladder papillomatosis, right inguinal hernia repair, and no previous abdominal surgery. The abdominal medical examination revealed only a painful and irreducible lump in the right inguino-crural region, the rectal examination found a normal empty ampulla, the white blood cells count was in the normal range, and the abdominal X-ray showed signs of bowel obstruction. An incarcerated right femoral hernia was diagnosed, although a recurrent inguinal hernia remained suspected. The hernia was reduced by taxis and the abdominal pain resolved. Clinical conditions were reassuring and an early elective surgery was preferred instead of urgent operation.
Patient remained hospitalized to undergo other preoperative examinations.
Three days after admission, immediately following a colonoscopy (resulted negative), an urgent surgery became mandatory because of another episode of hernia incarceration, this time irreducible.
Open surgery was performed because our center has not yet experienced the hernia approach by laparoscopy. We made an inguinal oblique incision approximately 1 cm above the inguinal ligament in order to be able to manage both a crural and an inguinal hernia.
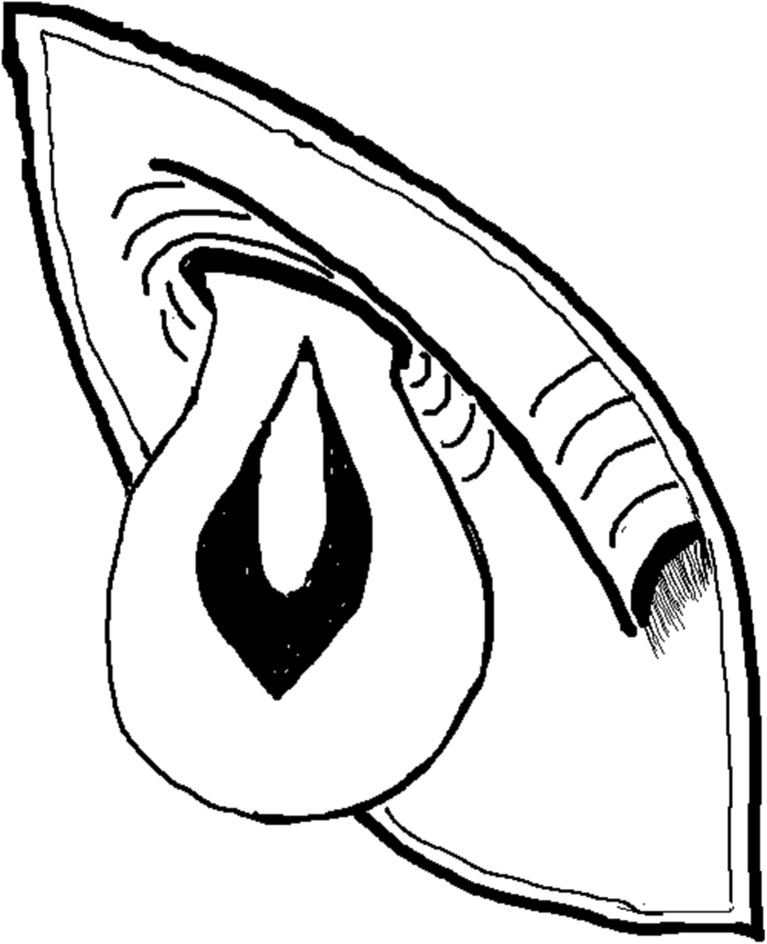
The intraoperative finding was an incarcerated femoral hernia with an inflamed appendix in its sac (Fig. 1).
Fig. 1.
The image shows the inflamed appendix in the crural hernia sac
The appendix was removed and the stump was secured by ligature and invaginating suture.
The hernia repair was performed by suturing the iliopubic tract to Cooper’s ligament with absorbable suture materials after sac removal.
Absorbable suture were used to prevent postoperative neuropathic pain attributable to nerve entrapment and prosthetic devices were avoided because of the high risk of infection.
The histological examination confirmed a catarrhal appendicitis.
Patient had a regular course and was discharged on the second postoperative day.
In our case, we suppose de Garengeot’s hernia is owing to the appendix migration in the hernia sac because of pelvic localization of caecum, afterwards the rigid femoral ring strangulated it.
Discussion
The de Garengeot’s hernia is a femoral hernia with an acute appendicitis in its sac and accounts for 0.08–0.13 % of all femoral hernias. It is more common in women (6:1) in order the higher incidence of femoral hernias in this sex, mainly affects the elderly population [1, 3–6].
Similar but different condition is Amyand’s hernia, i.e., acute appendicitis in an inguinal hernia, named after the English surgeon Claudius Amyand, who first performed appendectomy in an inguinal hernia sac in 1735 [1, 8].
The migration of appendix in the femoral hernia may be attributed to its abnormal anatomic position. It may depend on abnormal intestinal rotation during embryological development, anatomic variations in the mobility of the ceacum, or variations in caecal attachments [1, 5, 6].
Two theories are debated about the physiopathology of the appendix inflammation in the hernia sac. According to the first theory, the inflammation is owing to an intraluminal obstruction due to an appendicolith or a hypertrophy of appendiceal lymphatic tissue; according to the second theory, the inflammation is an ischemic necrosis due to the appendix strangulation by the narrow neck of the femoral canal [1, 2, 4, 6].
The most common clinical symptoms include vague abdominal pain, painful swelling, and erythema of the right groin [1–8].
The differential diagnosis must be done with inguinal hernia, adenitis, varix node, ectasia of the vena saphena magna, lipomas or other soft tissue tumors, lymphomas, and hypostatic abscesses in retroperitoneal processes [5].
Abdominal computed tomography can reveal a low-positioned caecum and a fluid-filled tubular structure with thick walls extending from the base of the caecum into the herniated sac. Ultrasound abdominal scan can identify bowel contents in the hernia sac [1, 5, 7].
Nevertheless, the diagnosis remains an intraoperative finding because clinical signs and instrumental exams can be not specific [1–8].
The treatment of choice for de Garengeot’s hernia is the emergency appendicectomy and femoral hernia repair.
In the case of not gangrenous or perforated appendix, the appendectomy via hernia sac is adequate by inguinal oblique incision; if perforation signs are found or it is difficult to reach the base of appendix, the laparotomic approach is mandatory [1, 4].
In the case of evident contamination of surgical field, the hernia repair by only suturing (herniorrhaphy) is more safe to prevent postoperative infections; otherwise, a prosthetic device can be used [4, 5].
Laparoscopic approach is an available and effective therapeutic option limited by the risk of expansion of the infection originating from the appendix. When practicable, it has the social advantages of laparoscopic treatment (shorter hospital stay, earlier return to work, less need for pain killers). In surgical literature, this topic is still debated though various small series confirm the feasibility [7].
The prognosis is excellent and the most frequent complication is the wound infection, which occurs in 14–29 % of cases and resolves successfully. More rare and serious reported complications are necrotising fasciitis and death due to sepsis, typical in cases of very old patients and/or delayed treatment [1, 6].
In conclusion, the de Garengeot’s hernia is a rare disease for which the preoperative diagnosis remains a very difficult challenge for the surgeon, in that:
There are no typical signs or symptoms.
Imaging studies can often be indeterminate or misinterpreted.
It is not very likely that a surgeon considers this condition in course of differential diagnosis because it is a rare disease.
Despite all the difficulties of the previous points, the timely diagnosis and the appropriate surgical treatment is the key to having a successful outcome.
We claim that it is essential to spread the knowledge of this pathology among the medical community in order to include it in the differential diagnosis of pain in the right lower quadrant.
Acknowledgments
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Salkade PR, Chung AY, Law YM. De Garengeot’s hernia: an unusual right groin mass two to acute appendicitis in an incarcerated femoral hernia. Hong Kong Med J. 2012;18(5):442–445. [PubMed] [Google Scholar]
- 2.Weir CD, Doan SJ, Lughlin V, Diamond T. Strangulation of the appendix in a femoral hernia sac. Ulster Med J. 1994;63(1):114–115. [PMC free article] [PubMed] [Google Scholar]
- 3.Erdas E, Sias L, Licheri S, Secci L, Aresu S, Barbarossa M, Pomata M. De Garengeot hernia with acute appendicitis. G Chir. 2013;34(3):86–89. [PubMed] [Google Scholar]
- 4.Ebisawa K, Yamazaki S, Kimura Y, Kashio M, Kurito K, Yasumuro S, Nishida S, Takayama T. Acute appendicitis in an incarcerated femoral hernia: a case of De Garengeot Hernia. Case Rep Gastroenterol. 2009;3(3):313–317. doi: 10.1159/000250821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piperos T, Kalles V, Al Ahwal Y, Konstantinou E, Skarpas G, Mariolis-Sapsakos T. Clinical significance of de Garengeot’s hernia: a case of acute appendicitis and review of the literature. Int J Surg Case Rep. 2012;3(3):116–117. doi: 10.1016/j.ijscr.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen ET, Komenaka IK. Strangulated femoral hernia containing a perforated appendix. Can J Surg. 2004;47(1):68–69. [PMC free article] [PubMed] [Google Scholar]
- 7.Comman A, Gaetzschmann P, Hanner T, Behrend M. DeGarengeot hernia: transabdominal preperitoneal hernia repair and appendectomy. JSLS. 2007;11(4):496–501. [PMC free article] [PubMed] [Google Scholar]
- 8.Akopian G, Alexander M. de Garengeot Hernia: appendicitis within a femoral hernia. Am Surg. 2005;71(6):526–527. [PubMed] [Google Scholar]