Abstract
Postcholecystectomy bile duct injuries are a cause of significant morbidity and occasional mortality. Intraoperative recognition and repair of complete biliary transection with hepaticojejunostomy is the recommended treatment; however, it is possible only in few patients as either the injury is not recognized intraoperatively or the center is not geared up to perform an urgent hepaticojejunostomy in these patients with a nondilated duct. Retrospective analysis of data from a tertiary care referral center over a period of 10 years from January 2000 to December 2009 to report the feasibility and outcomes of prompt repair was done (defined as repair within 72 h of index operation) of postcholecystectomy bile duct injury. Ten patients of postcholecystectomy bile duct injury detected intraoperatively and referred early underwent prompt repair. All patients had a complete transection of the bile duct (type of injuries as per Strasberg classification: Type E V: 1, Type E III: 5, Type E II: 3 and Type E I: 1). The mean duration between injury and bile duct repair in the form of Roux-en-Y hepaticojejunostomy (RYHJ) was 22.7 (range 5–42) hours. The mean diameter of the anastomosis was 1.63 (range1–2.1) cm, and the anastomosis was stented in 7 patients. The mean duration of surgery was 4.6 +1.7 h. One patient developed bile leak on the first postoperative day, which settled by day 5. The mean duration of hospital stay was 5.1 (range 4–8) days. With a mean follow-up of 42 (range 24–110) months, all patients had excellent (70 %) or good outcome (30 %). Prompt RYHJ (within first 72 h) for postcholecystectomy biliary transection is an effective treatment and potentially limits the morbidity to the patient.
Keywords: Bile duct injury, Hepaticojejunostomy, Cholecystectomy, Biliary transection
Introduction
Biliary injury during cholecystectomy is a dreaded complication. If the injury is detected intraoperatively and appropriately managed, the associated morbidity is limited [1, 2]. Inadvertent biliary transection is best managed by performing a Roux –en-Y hepaticojejunostomy (RYHJ) by an expert team; however, it is possible in very few cases as only 25 %–32 % injuries are detected intraoperatively, and even when recognized, in most situations, the surgeon/center is not geared up to perform an RYHJ in a nondilated normal sized duct [3, 4]. Undetected intraoperatively, most of these cases present late with bile leak or its manifestations and are subsequently managed with a delayed bilioenteric bypass (RYHJ). Some injuries which are detected intraoperatively and are referred to a specialized center in time can be managed by prompt repair. The objective of this study was to report the feasibility and outcomes following prompt repair (within 72 h of the index surgery) of postcholecystectomy bile duct injuries with a transected bile duct referred to our center.
Methods
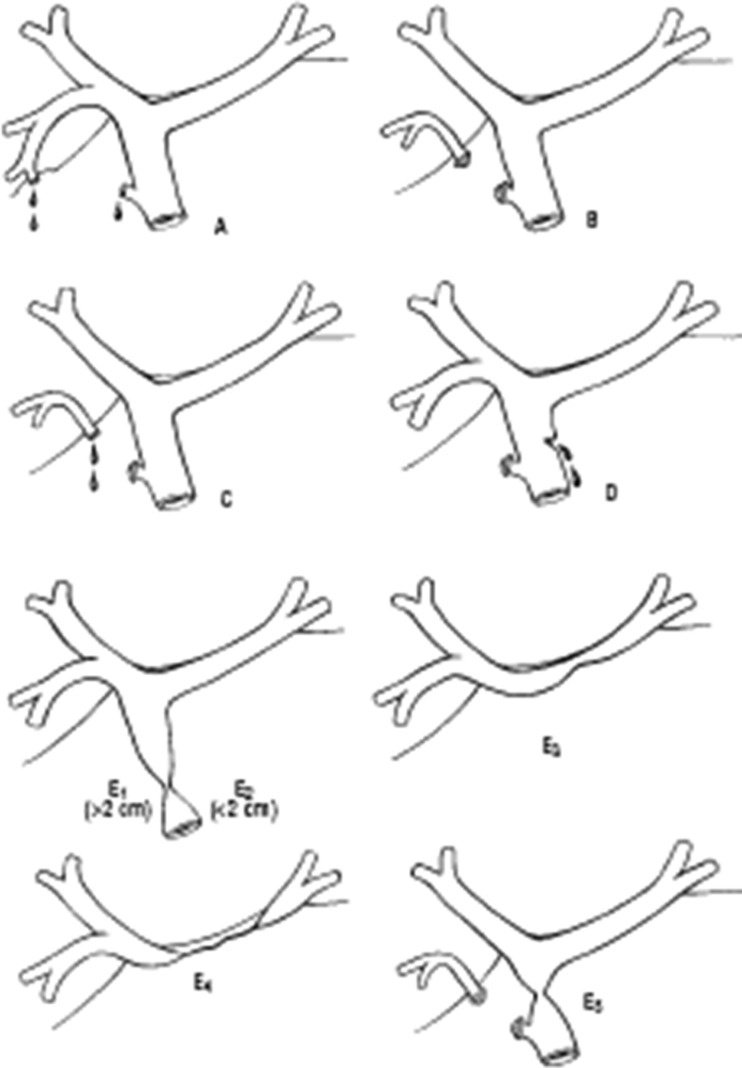
Retrospective analysis of prospectively collected data of bile duct injuries surgically managed at our center, a tertiary referral teaching center, between 2000 and 2009. The study group comprised 10 patients who had sustained a bile duct transection during cholecystectomy, which was recognized peroperatively and referred to our center with a drain in situ, within 72 h of injury. After admission, the patients were started on intravenous fluid and broad spectrum antibiotics. Blood investigations including hemogram, liver function tests, serum electrolytes and renal function tests were done and any abnormalities were corrected. A chest X-ray, bedside ultrasound of the abdomen and electrocardiogram were also done prior to surgery. Following this, the patients were taken up for prompt repair of the biliary injury. The surgical procedure was performed using an extended right subcostal incision. Any bile in the peritoneal cavity was suctioned out. By gentle dissection in the hepatoduodenal ligament, the magnitude of the biliary injury was ascertained and graded as per Strasberg classification (Fig. 1) [5]. In all cases, efforts were made to look for associated injuries including vascular injuries (especially of the right hepatic artery). In cases wherein the biliary anatomy was not clear, an intraoperative cholangiogram was done to ensure identification of all the major bile ducts. The repair was performed by anastomosing a well vascularized healthy proximal duct (with extension/filleting of the left duct) to a Roux loop of the jejunum (RYHJ, Fig. 2). Patients were followed up every 3 months for 1 year, 6 monthly for next 2 years and annually thereafter. A liver function test and ultrasound of the abdomen were done at each visit. A HIDA scan or MRCP was performed if needed. The outcome of surgery was graded as per the McDonald system (Table 1 and 2) [6].
Fig. 1.
Strasberg classification of bile duct injuries
Fig. 2.

Proximal bile duct prepared for hepaticojejunostomy – en-Y
Table 1.
Patient data
| S. no | Age | Sex | Interval between index surgery and repair (hours) | Type of injury | Surgery done | Duration of surgery (hours) | Anastomotic diameter (cm) | Stenting | Outcome McDonald grading |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 43 | M | 24 | E III | RYHJ | 5 | 2.1 | No | A |
| 2 | 24 | F | 32 | E III | RYHJ | 4.5 | 1 | Yes | B |
| 3 | 34 | F | 18 | EIII | RYHJ | 5 | 1.5 | Yes | A |
| 4 | 36 | F | 42 | EII | RYHJ | 3.6 | 2 | Yes | A |
| 5 | 56 | F | 30 | EII | RYHJ | 4 | 1 | Yes | A |
| 6 | 42 | F | 18 | EI | RYHJ | 3 | 2.1 | No | A |
| 7 | 40 | F | 24 | EII | RYHJ | 4.3 | 1.8 | Yes | A |
| 8 | 35 | M | 24 | EIII | RYHJ | 5.6 | 1.3 | yes | B |
| 9 | 30 | F | 5 | EV | RYHJ + Rt posterior sectoral duct anastomosis | 4 | 1.5 and 0.5 | Yes | A |
| 10 | 70 | F | 10 | EIII | RYHJ | 3 | 2 | No | B |
Table 2.
McDonald grading system for outcome of surgical repair
| McDonald grade A | Asymptomatic patient, normal LFT |
| McDonald grade B | Asymptomatic patient, mild LFT derangement or occasional episodes of pain or fever |
| McDonald grade C | Pain, cholangitis and abnormal LFT |
| McDonald grade D | Requiring percutaneous dilatation or surgical revision |
Results
During the study period between 2000 and 2009, 406 patients of postcholecystectomy bile duct injuries were managed at our Department of Gastrointestinal Surgery. Of these, 10 patients were referred within 72 h of cholecystectomy with a biliary transection, which was detected intraoperatively. In all these patients, the injury was detected intraoperatively by the primary surgeon; a drain was placed and patients were referred to our center for further management. Of the 10 patients, there were 8 females and 2 males with a mean age of 41 (range 24–70) years. The types of injury (as per Strasberg classification) were Type E V: 1, Type E III: 5, Type E II: 3 and Type E1: 1. An RYHJ was done in all cases. The mean duration between index surgery (cholecystectomy) and bile duct repair (RYHJ) was 22.7 (range 5–42) hours. (Table 1) None of the patients had an associated vascular injury of the hepatic artery or portal vein. Nonviable tissue at the ends of the injured bile duct was excised in order to get a healthy duct for hepaticojejunostomy and to get wide anastomosis; extension onto/filleting of the left duct was done.
The mean diameter of the proximal duct was 0.75 (range 0.5–1.0) cm, and the mean anastomotic diameter was 1.63 (range 1–2.1) cm. Stented anastomosis was done in 7 patients as per the discretion of the operating surgeon. The mean duration of surgery was 4.6 ± 1.7 h and the mean blood loss was 185 (range 100–350) ml. There were no intraoperative complications or mortality. One patient developed postoperative bile leak on the first postoperative day, which settled by day 5. The mean hospital stay was 5.1 (range 4–8) days.
Follow up
All patients were followed up 3 monthly for 1 year, 6 monthly for next 2 years and annually thereafter. LFT and USG abdomen were done at each visit. A HIDA/MRCP was performed if needed. All 10 patients were followed up with mean follow up of 42 months (range 24–110 months). The outcome of surgery was graded as per the McDonald system. Seven patients (70 %) were asymptomatic and had normal LFT (McDonald Grade A), and three patients had mild derangement of LFT (elevated alkaline phosphatase and bilirubin) but were asymptomatic (McDonald Grade B). USG abdomen/MRI abdomen in these three patients did not reveal any IHBRD or segmental duct stricture. A HIDA performed showed normal bilioenteric flow with no hold up at the anastomotic site. None of the patients required any reintervention.
Discussion
The incidence of BDI during cholecystectomy has been reported to be 0.3 % to 0.6 % [7, 8], and most of these injuries are detected in the postoperative period. Only 25 %–32 % of bile duct injuries are recognized intraoperatively and an immediate repair in form of an RYHJ by an expert is the recommended approach [1, 2]. Unfortunately, the necessary technical expertise required to accomplish an RYHJ repair in these nondilated ducts is not always available at the center where the cholecystectomy has been performed and the injury detected. When the surgeon/center is not adept in performing such a procedure routinely, it is safer to drain the area and refer the patient to a specialized hepatobiliary center. Prompt repair of biliary transections has not gained universal acceptance because these repairs are technically challenging due to the small duct size, uncertainty about the vascularity of the ducts and presence of local inflammation and bile, which may make the repair difficult and less successful. Few of the earlier reports showed less than satisfactory results for early repair of biliary injuries [9–11]. In these series, however, early repair had included RYHJs done even beyond the first 72 h and up to 1–3 weeks. On the other hand, others [12, 13] have reported good to excellent outcomes following prompt repair, i.e. within 48–72 h. These varied results can be attributed to the lack of a uniform definition of early repair. In the present series, prompt repair was performed in only those patients in whom the injury was recognized intraoperatively by the operating surgeon and the patient was referred to our center within 72 h with a drain in situ. The rationale for performing such repairs is that there is limited inflammation in that area, infectious complications have not set in and in the long term, the morbidity and cost of treatment are decreased. A further delay (i.e. beyond 72 h) results in increased inflammation of the bile duct and the possibility of infection, increasing the chances of failure of the repair. In this situation, all efforts should be made to ensure adequacy of biliary drainage and control of any infection/sepsis. Therefore, the timing of repair is of importance when analyzing the results of these series. While the results of prompt repair (within the first 48–72 h) are comparable to that performed if the injury is detected during the cholecystectomy, a delay in repair to beyond 72 h may compromise the outcome [12].
Intraoperative detection of biliary injuries has been reported to be possible in only 25 %–32 % [14]. Even when detected by the operating surgeon, there is often a delay in referring the patient to an appropriate surgeon/center. This is exemplified in our data, as of the total 406 cases of postcholecystectomy BDI managed in 10 years (January 2000 to December 2009), only 10 cases were referred early enough to be taken up for prompt repair. All these were recognized intraoperatively by the operating surgeon; all had a major bile duct injury (Strasberg Type E) without any other associated injury, and all of them were in a good clinical condition for definitive repair. The mean interval between cholecystectomy and repair was 22.7 h (range 5–42 h), mean ductal diameter was 0.75 cm and mean anastomotic diameter was 1.63 cm. To achieve a wide and well vascularized anastomosis, any nonviable tissue was excised and the left duct was included in anastomosis. All but three cases (70 %) had transanastomotic stent placed, which was removed at 6–8 weeks. One patient had a minor controlled bile leak, which settled spontaneously by the fifth postoperative day. The mean hospital stay was 5.1 days. All of our patients had excellent (70 %) or good (30 %) outcome without any restricture at a mean follow-up of 42 months.
In one of our patients, the operating surgeon contacted us after realizing (during the cholecystectomy) that an injury (transection) had occurred. He was advised to terminate the procedure with no further attempt to remove the gall bladder from the bed and refer the patient after putting a drain in the right subhepatic region. This not only prevents further proximal extension of the injury, but also facilitates the subsequent repair. The referral center can prepare healthy proximal duct after completing cholecystectomy and transecting the duct at an appropriate level. Therefore, if during the index surgery (cholecystectomy) the operating surgeon realizes that a transaction has occurred and he is not geared up to perform an immediate repair, he should not do any further dissection or attempt to remove the gall bladder.
At the time of repair, it is prudent to identify and ascertain the extent of injury. In such a situation, performing intraoperative cholangiogram can be extremely valuable in defining the anatomy. The repair is performed by anastomosing (duct mucosa) the bile duct with a Roux limb of the jejunum. Any nonviable tissue at the ends of the injured bile duct should be excised in order to get a healthy duct. It is also important to assess the integrity of the right hepatic artery as its injury is a known risk factor for development of a delayed anastomotic stricture if an early repair is performed [15]. Early repair following a concomitant biliovascular injury (especially injury to the right hepatic artery) has been reported as a risk factor for the development of ischemic anastomotic strictures. This is especially important in more proximal biliary injuries involving the hilum. In experienced centers, a simultaneous vascular repair can be attempted during prompt surgery for biliary injury; however, long-term outcomes following such repairs are not known. However, this is a feasible option only when detected on table. After a time gap, a vascular repair is not usually recommended. In the present series, none of the patients had an associated vascular injury.
An anastomosis at the hilum with extension onto the left duct obviates the ill effects of an associated vascular injury. The incision on the bile duct is further extended onto the left duct to achieve wider anastomosis. While some may argue that such an extension may result in a higher stricture should the anastomosis narrow, the current literature suggests that such an approach used while performing a hepaticojejunostomy as a part of early repair may actually decrease the incidence of stricture formation [13]. For small ducts, fine catheters are used to stent the anastomosis.
The efficacy of delayed repair is well established. Chapman et al. [16] reported excellent or good outcomes in 87 % cases (of 110 patients) following a delayed repair. Similar results were also shown by Sikora et al. [17] and Murr et al. [18].
Excellent results obtained in our experience are due to the good patient selection (time interval of <72 h, absence of peritonitis and sepsis) and strict adherence to the principles of high anastomosis with extension to left duct. Good patient selection is paramount for success of this approach. Presence of severe peritonitis, bilioma or systemic sepsis will render the patient unsuitable for prompt repair and drainage and control of sepsis is prudent before attempting any repair in such cases. We take 72 h as a cut off for attempting prompt repair because presence of bile and surgical trauma beyond that point incite sever inflammatory response and also increase chances of colonization of bile, leaving unhealthy and inflamed tissues less suitable to repair [12], which may explain poor results obtained in some series attempting repair beyond this point. A universal approach of high repair with extension to left duct safe guards against progression of ischemia which is responsible for majority of restrictures in the early repair group. On the basis of our results, we propose a prompt repair in a selective group of patients which are referred to an expert center within 72 h and are not associated with peritonitis or sepsis.
Conclusion
Prompt RYHJ for biliary transection (within first 72 h) for postcholecystectomy biliary transection is an effective treatment and potentially limits the morbidity to the patient. Good patient selection with a controlled biliary fistula and no evidence of sepsis, and sound surgical technique can help achieve results comparable to delayed or on table repair.
References
- 1.Olsen D. Bile duct injuries during laparoscopic cholecystectomy. Surg Endosc. 1997;11(2):133–138. doi: 10.1007/s004649900315. [DOI] [PubMed] [Google Scholar]
- 2.Carroll BJ, Birth M, Phillips EH. Common bile duct injuries during laparoscopic cholecystectomy that result in litigation. Surg Endosc. 1998;12(4):310–314. doi: 10.1007/s004649900660. [DOI] [PubMed] [Google Scholar]
- 3.Jarnagin WR, Blumgart LH. Operative repair of bile duct injuries involving the hepatic duct confluence. Arch Surg. 1999;134:769. doi: 10.1001/archsurg.134.7.769. [DOI] [PubMed] [Google Scholar]
- 4.Mercado MA. Early versus late repair of bile duct injuries. Surg Endosc. 2006;20:1644–1647. doi: 10.1007/s00464-006-0490-9. [DOI] [PubMed] [Google Scholar]
- 5.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 6.McDonald MI, Farnell MB, Nagorney D, et al. Benign biliary strictures: repair and outcome with a contemporary approach. Surgery. 1995;118:582–591. doi: 10.1016/S0039-6060(05)80022-4. [DOI] [PubMed] [Google Scholar]
- 7.Calvete J, Sabater L, Camps B, et al. Bile duct injury during laparoscopic cholecystectomy: myth or reality of the learning curve? Surg Endosc. 2000;14:608–611. doi: 10.1007/s004640000103. [DOI] [PubMed] [Google Scholar]
- 8.Flum DR, Cheadle A, Prela C, et al. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290:2168–2173. doi: 10.1001/jama.290.16.2168. [DOI] [PubMed] [Google Scholar]
- 9.Bergman JJ, van den Brink GR, Rauws EA, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996;38(1):141–147. doi: 10.1136/gut.38.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walsh RM, Henderson JM, Vogt DP, Brown N. Long-term outcome of biliary reconstructionfor bile duct injuries from laparoscopic cholecystectomies. Surgery. 2007;142(4):456–457. doi: 10.1016/j.surg.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Goykhman Y, Kory I, Small R, et al. Long-term outcome and risk factors of failure after bile duct injury repair. J Gastrointest Surg. 2008;12(8):1412–1417. doi: 10.1007/s11605-008-0538-3. [DOI] [PubMed] [Google Scholar]
- 12.Sahajpal AK, Chow SC, Dixon E. Bile duct injuries associated with laparoscopic cholecystectomy. Timing of repair and long-term outcomes. Arch Surg. 2010;145(8):757–763. doi: 10.1001/archsurg.2010.153. [DOI] [PubMed] [Google Scholar]
- 13.Mercado MA, Chan C, Orozco H, Tielve M, Hinojosa CA. Acute bile duct injury. The need for a high repair. Surg Endosc. 2003;17(9):1351–1355. doi: 10.1007/s00464-002-8705-1. [DOI] [PubMed] [Google Scholar]
- 14.Lau WY, Lai ECH, Lau SHY. Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg. 2010;80:75–81. doi: 10.1111/j.1445-2197.2009.05205.x. [DOI] [PubMed] [Google Scholar]
- 15.Gupta N, Solomon H, Fairchild R, Kaminski DL. Management and outcome of patients with combined bile duct and hepatic artery injuries. Arch Surg. 1998;133:176–18. doi: 10.1001/archsurg.133.2.176. [DOI] [PubMed] [Google Scholar]
- 16.Chapman WC, Havely A, Blumgart LH, Benjamin IS. Postcholecystectomy bile duct strictures: management and outcome in 130 patients. Arch Surg. 1995;130:597–604. doi: 10.1001/archsurg.1995.01430060035007. [DOI] [PubMed] [Google Scholar]
- 17.Sikora SS, Pottakkat B, Srikanth G, Kumar A, Saxena R, Kapoor VK. Postcholecystectomy benign biliary strictures—long-term results. Dig Surg. 2006;23(5–6):304–312. doi: 10.1159/000097894. [DOI] [PubMed] [Google Scholar]
- 18.Murr MM, Gigot JF, Nagorney DM, Harmsen WS, Ilstrup DM, Farnell MB. Long term results of biliary reconstruction after laparoscopic bile duct injuries. Arch Surg. 1999;134(6):604–610. doi: 10.1001/archsurg.134.6.604. [DOI] [PubMed] [Google Scholar]