Abstract
Purpose
The National Breast and Cervical Cancer Early Detection Program through each state's administration serves millions of low-income and uninsured women aged 40–64. Our purpose was to assess whether cases screened through Georgia's Breast and Cervical Cancer Program (BCCP) were diagnosed at an earlier stage of disease and whether those who used the state's program regularly continued to obtain age-appropriate screens as they aged out of BCCP into Medicare between 2000 and 2005.
Methods
We used BCCP screening data to identify women with more than one screen and an interval of 18 months or less between screens as “regular” users of BCCP. Using the linked BCCP and Medicare enrollment/claims data, we tested whether women with any BCCP use (n = 3,134) or “regular” users (n = 1,590) were more likely than women not using BCCP (n = 10,086) to exhibit regular screening under Medicare. We used linked BCCP and Georgia Cancer Registry data to examine breast cancer incidence and stage at diagnosis of BCCP women compared to the Georgia population.
Results
Under Medicare, almost 63 % of women with any BCCP use were re-screened versus 51 % of non-BCCP users. The probability of being screened within 18 months of Medicare enrollment was 3.5 % points higher for any BCCP user and 17.7 points higher for “regular” BCCP users, compared to nonusers. Among Black non-Hispanics, the difference for any BCCP user was 13.7 % points and for regular users, 22.4 % points. A larger percentage of BCCP users were diagnosed at in situ or localized disease stage than overall.
Conclusions
The majority of women aging out of the GA BCCP 2000–2005 had used the program to obtain regular mammography. Regular users of GA BCCP continued to be screened within appropriate intervals once enrolled in Medicare due perhaps to educational and support components of BCCP.
Keywords: Mammography, NBCCEDP, Medicare
Introduction
The National Breast and Cervical Cancer Early Detection Program (NBCCEDP), established in 1990 and funded through the Centers for Disease Control and Prevention (CDC), provides important access to low-income women by providing free clinical breast examinations, mammograms, Pap tests, pelvic examinations, human papillomavirus (HPV) tests, diagnostic tests for abnormal results, and referrals to treatment [1]. NBCCEDP eligibility is generally extended to uninsured and underinsured women at or below 250 % of federal poverty level (FPL), but state income eligibility levels and other administrative details vary. While approximately 9–10 % of US women are eligible for NBCCEDP, it serves 8–12 % of these women due in part to limitations on funding [1].
Since 1995, Georgia has participated in the NBCCEDP with a program known as the “Breast and Cervical Cancer Program” or “BCCP.” Women can access BCCP services in all county public health clinics as well as in some private clinics that partner with the BCCP. The BCCP targets women aged 50–64 for breast cancer screening and those never/rarely screened. The BCCP considers a “rarely screened” woman as one who has not had a mammogram within the past 5 years. In addition to providing free clinical cancer screening services, the BCCP uses client navigators to offer support to BCCP case manager nurses and to conduct population-based education regarding breast, cervical, and colorectal cancers; a key goal is to encourage age-appropriate screening patterns. The BCCP began using client navigators in 2001, and their state partnership with the American Cancer Society (ACS) to operate this aspect of the program was established in 2011. Between 2008 and 2012, the BCCP served 40,071 women and provided 39,048 breast cancer screenings.
The NBCCEDP has been shown to be important for screening of low-income, uninsured women. As the NBCCEDP state programs matured in the latter 1990s, the percentage of all non-elderly women receiving Pap test, clinical breast examination (CBE), and mammography increased [2, 3]. Studies also indicate improvement over time within the NBCCEDP in reducing time to diagnosis [4, 5] and treatment [4] among NBCCEDP users with abnormal CBE or mammogram results. Newer studies indicate an association with reduced breast cancer mortality rate [6, 7]. Additionally, adding case management as a formal component in 2000 was perceived by state program managers to decrease the delay in follow-up and diagnostic services for women screened through the NBCCEDP [4, 8]. This result supports other studies that suggest the NBCCEDP case managers and other patient navigator programs can improve patients' timeliness to diagnosis, decrease patients' anxiety, and increase overall care satisfaction [5, 9]. The BCCP uses educational materials and consistent follow-up to encourage women to repeat screening at an interval of <18 or 24 months.
Repeat breast cancer screening is lowest among those with less than a college education, low income, and lack of insurance [10]. While older women (50+) are more likely than younger women to report screening within the past 2 years, a quarter of older women do not receive appropriate and timely mammography [11].
In this study, we examined the breast cancer screening patterns among women using the BCCP in GA and reaching Medicare age (65) between 2000 and 2005. Our goals were to assess whether, as they aged into Medicare coverage, their use of the BCCP influenced their screening behaviors compared to non-BCCP users of similar age, race/ethnicity, and similar geographic areas and in turn, whether it was associated with an earlier stage among those who did experience a breast cancer diagnosis.
Materials and methods
After obtaining institutional review board approval, we conducted a retrospective study focused on breast cancer screening and the incidence of breast cancer cases in Georgia for BCCP and non-BCCP women using several sources of data.
Data and linkage
We used data from: (1) BCCP enrollment and visit records; (2) Medicare Beneficiary Summary files (MBSF, BASF) and carrier claims files from the Centers for Medicare and Medicaid Services (CMS); and (3) Georgia Cancer Registry (GCR) in our analysis. We used the BCCP data to identify women who received at least one breast cancer screening or diagnostic procedure paid by the BCCP in Georgia and who turned 65 years of age between 2000 and 2007 and hence aged into Medicare in this period (n = 9,587); see Table 1 for a flowchart of full sample derivation.
Table 1.
Flowchart showing derivation of BCCP sample
| Category | n |
|---|---|
| BCCP aging out 2000–2008 | 9,587 |
| BCCP aging out 2000–2005 | 4,796 |
| BCCP aging out 2000–2005 | |
| Matched to Medicare beneficiary ID by Social Security Number | 3,858 |
| BCCP aging out 2000–2005 | |
| Matched to Medicare beneficiary ID by Social Security Number and date of birth | 3,666 |
| BCCP aging out 2000–2005 | |
| Matched to Medicare beneficiary ID by Social Security Number and date of birth and no HMO coverage in first 24 months of Medicare enrollment* | 3,134 |
A roster of IDs (Social Security Number (SSN), date of birth (DOB), and zip code) for these 9, 587 women was sent to CMS for linkage 2000–2007; CMS matched only on SSN and DOB so we would have data on women in the Medicare files 2000–2007 who had used the BCCP but may now reside elsewhere. We restricted our analytic sample to those aging out of the GA BCCP from 2000 to 2005 (n = 4,796) to observe their Medicare claims for at least 24 months. Of these women, we kept only those with: (1) SSN and exact DOB matching or (2) SSN and BCCP and Medicare DOB <1 week apart or same day/month but different years (n = 3,666). From this group, as well as the matched comparison group (discussed below), we excluded those with evidence of HMO enrollment in the first 24 months of Medicare enrollment since we only observe full claims experience for women in the Medicare fee-for-service sector; this sample included 3,134 BCCP women.
Since women can qualify for Medicare coverage before age 65 due to disability, we identified this group (9.7 % of BCCP women) and used the woman's actual Medicare start date if it occurred between 2000 and 2005. If the start date was before 2000 (2.7 % of BCCP women), we used the date they turned 65 as their Medicare start date for the purpose of this analysis. We control for disability status in our analysis.
Comparison group
CMS also provided data on non-BCCP women who aged into Medicare during 2000–2007 at the same time as BCCP women from similar GA zip codes; a comparison sample was drawn from these data. From the full CMS sample, we derived a random control sample of three Medicare enrolled women for each BCCP woman. We matched first based on race, year aging out, and zip code. While 85 % matched using these criteria, we subsequently found matches based on combinations of these factors and county in order to get three matches. There were five BCCP women without any available “matching” controls; they were still included in the BCCP analytic group. We derived the same dependent and independent variables for the BCCP group and the comparison group of women (n = 10,086), identifying all comparison women as non-BCCP users.
Regression variables
From the BCCP Enrollment and Patient Information, we used DOB, dates of each screening visit, type of screening visit (diagnostic, routine), screening results (normal, abnormal), age, race/ethnicity, and zip/county of residence for each woman in our study cohort. From the CMS two Beneficiary Annual Summary File (BASF), we derived data on evidence and indicators of 21 chronic conditions, Medicare coverage type (A, B, A/B, HMO), dates of birth and death, dates that their Medicare coverage started, and Medicare status code (disabled).
We derived dependent variables that indicated whether the woman was screened (diagnostic or routine) within 18 or 24 months of her enrollment in Medicare by starting with her actual date of Medicare enrollment and examining claims to see whether the procedure codes noted below were observed with service dates in our follow-up periods. We report results for the 18-month period although the results are similar using the 24-month follow-up. Using the combination of the BCCP and Medicare claims data, we derived the time of screening since the woman first used BCCP, the time of screening since Medicare coverage began, the number of screens she received in BCCP and through Medicare, and the time between screens in each program, for those with multiple screens. The BCCP data denoted whether the screen was diagnostic or routine screening while procedure codes in the Medicare claims were used. Specifically, HCPCS procedure codes used to indicate diagnostic screens were 76090, 76091, 77051,77055, 77056, G0204, G0205, G0206,G0207, and 76082; HCPCS codes used to denote routine screens were 77052, 77057, G0202, G0203, 76092,76085, and 76083.
Our key independent variable was whether the woman was a BCCP user and if a user, a “regular” user. Since we observed a variety of screening patterns among women ever screened in the BCCP, we tested whether we would observe a sizeable number of women who were: (1) screened more than once and (2) if rescreened, the interval was less than 18 or 24 months. Those screened more than once and re-screened within 18 months were then categorized as “regular” users. We derived a categorical independent variable including: (1) any use of BCCP but not a “regular” user; (2) “regular” user of BCCP; and (3) non-BCCP user as the reference group.
To account for health status, we used CMS data for chronic conditions; these data include a yearly indicator and a first occurrence (1999 is earliest date) for 21 conditions. We collapsed their list into a subset based on prior literature and on significance levels. Other covariates in the model included: (1) race/ethnicity (Black non-Hispanic, Hispanic/other, and White non-Hispanic as reference group); (2) Medicare coverage during our follow-up period (Part A only, Part A and B non-continuous, Part A and B continuous as reference group); and (3) disabled (non-disabled as reference group). We note that women will receive screening services largely under Medicare Part B since this covers physician and outpatient service while Part A is largely for inpatient services. Finally, to control for unobserved time invariant county characteristics that may affect the woman's access to insurance and screening services, we used county indicators and estimate a fixed-effect model.
Logistic regressions were run for the full sample and for subsamples of women by race and by evidence of a breast cancer diagnosis as found in the Medicare comorbidity data, using Stata Statistical Software: Release 13. Marginal effects of each independent variable were estimated using the margins function within STATA. The sample for regression analysis excluded those women who died within 24 months of their Medicare start date; regression results were not affected by this exclusion.
Results
Descriptive: BCCP and non-BCCP women
Descriptive data for BCCP and matched non-BCCP women aging into Medicare 2000–2005 are shown in Table 2. Statistical significance is noted; there are no differences by race/ethnicity since the comparison group was matched on these characteristics. Data indicate that BCCP women are less likely to have only Part A coverage (1.9 vs. 4.0 %) and if covered by Part B, less likely to have non-continuous coverage (4.6 vs. 6.5 %). BCCP women are far less likely to be disabled (7.3 vs. 17.9 %); low-income disabled women would qualify for coverage under other public programs. Consistent with lower levels of disability, BCCP women were less likely to have any of the comorbidities listed with the exceptions of diabetes (17 % for both), breast cancer (1.4 vs. 1.8 %), colorectal (0.7 vs. 0.5 %), lung (0.4 vs. 0.3 %), and endometrial (0.3 for both) cancers. While almost 84 % of BCCP repeat users return within 18 months (see Table 3), and these women are identified as “regular” users of BCCP, this proportion drops to around 81 % (see Table 3) when they are under Medicare coverage. Yet, this is higher than non-BCCP users at 78 %. The first mammogram (diagnostic or screening) is received within 18 months of Medicare enrollment for less than half of non-BCCP users but for 60 % of BCCP users.
Table 2.
Characteristics of sample, BCCP, and non-BCCP users aging into Medicarea, 2000–2005
| Demographic and clinical characteristics | Full sample n = 13,320 | Non-BCCP users n = 10,086 | BCCP users n = 3,134 |
|---|---|---|---|
| Race | |||
| Non-Hispanic Black (%) | 39.5 | 39.5 | 39.2 |
| Non-Hispanic White | 56.4 | 56.3 | 56.7 |
| Other | 4.1 | 4.1 | 4.1 |
| Medicare coverage (first 24 months)b | |||
| Part A only | 3.5 | 4.0 | 1.9*** |
| Part A with non-continuous part B | 6.0 | 6.5 | 4.6 |
| Part A and B | 90.4 | 89.5 | 93.5 |
| Disabled | 15.4 | 17.9 | 7.3*** |
| Died within 24 months of Medicare start | 3.0 | 3.2 | 2.1*** |
| Comorbiditiesc | |||
| Cardiovascular disease (CVD) | 15.2 | 16.5 | 11.0*** |
| Dementia | 1.6 | 1.9 | 0.8*** |
| Osteoporosis/arthritis/hip fracture | 16.7 | 17.8 | 13.3*** |
| Cataract/glaucoma | 18.1 | 19.1 | 14.7*** |
| Chronic kidney disease | 3.5 | 4.0 | 1.8*** |
| Chronic obstructive pulmonary disease | 6.3 | 6.9 | 4.4*** |
| Diabetes | 17.1 | 17.1 | 17.0 |
| Depression | 9.0 | 9.6 | 7.2*** |
| Stroke/transient ischemic attack | 3.0 | 3.5 | 1.5*** |
| Breast cancer | 1.7 | 1.8 | 1.4 |
| Colorectal cancer | 0.5 | 0.5 | 0.7 |
| Lung cancer | 0.4 | 0.4 | 0.3 |
| Endometrial cancer | 0.2 | 0.2 | 0.2 |
p < 0.001;
p < 0.01;
p < 0.05
Any woman with at least one month of HMO coverage observed within the first 24 months of Medicare enrollment following their 65th birthdate is excluded from the sample
For some women (n = 1,561), their Medicare start date was before age 65; for these women, their 65th birthdate was used as their Medicare start date for purposes of the regression analysis. Almost all of these women are classified as disabled in the Medicare beneficiary files
Data on comorbidities are taken from the Medicare Chronic Condition Warehouse. Comorbidities are derived based on clinical codes found in claims data and first date of service
Table 3.
Breast cancer screening patterns among BCCP and non-BCCP users aging into Medicarea, 2000–2005
| Screening patterns | Full sample n = 13,320 | Non-BCCP users n = 10,086 | BCCP users n = 3,134 |
|---|---|---|---|
| Mammogramsb and intervals under BCCP | |||
| Only 1 | 39.4 % | – | 39.4 % |
| ≥2 | 60.6 | – | 60.6 |
| Pattern for those with ≥2 | n = 1,900 | n = 1,900 | |
| ≤12 months | 17.5 | – | 17.5 |
| 13–18 months | 66.2 | – | 66.2 |
| 19–24 months | 8.7 | – | 8.7 |
| >24 months | 7.6 | – | 7.6 |
| Mammogramsc and intervals under Medicare | |||
| No mammogram | 30.7 | 34.0 | 19.9*** |
| Only 1 | 15.6 | 15.1 | 17.4 |
| ≥2 | 53.7 | 50.9 | 62.7 |
| Pattern for those with ≥2 | n = 7,096 | n = 5,130 | n = 1,966 |
| ≤12 months | 24.6 | 24.7 | 24.2** |
| 13–18 months | 54.4 | 53.6 | 56.6 |
| 19–24 months | 10.9 | 10.8 | 11.2 |
| >24 months | 10.1 | 10.9 | 8.0 |
| Timing of mammogramsc under Medicare | |||
| Within 18 months of Medicare start | 50.3 | 47.1 | 60.4*** |
| Within 24 months of Medicare start | 56.2 | 52.7 | 67.4*** |
| Timing of screening mammogramsc under Medicare | |||
| Within 18 months of Medicare start | 44.5 | 41.7 | 53.5*** |
| Within 24 months of Medicare START | 50.7 | 47.5 | 60.9*** |
p < 0.001;
p < 0.01;
p < 0.05
Any woman with at least one month of HMO coverage observed within the first 24 months of Medicare enrollment following their 65th birthdate is excluded from the sample
Mammograms include diagnostic or screening mammograms and are identified directly in the BCCP data
Diagnostic mammograms are identified in the Medicare data with HCPCS procedure codes: “76090,” “76091,” “77051,” “77055,” “77056,” “G0204,” “G0205,” “G0206,” “G0207,” “76082”; screening mammograms are identified in the Medicare data with HCPCS procedure codes: “77052,” “77057,” “G0202,” “G0203,” “76092,” “76085,” “76083”
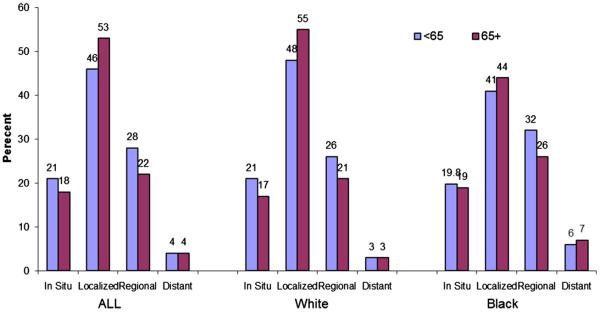
We also used GCR and linked BCCP data to examine the overall incidence of breast cancer in the Georgia population and differences in the stage at diagnosis of BCCP cases and non-BCCP women. As shown in Fig. 1, older women with a breast cancer diagnosis in Georgia tend to be diagnosed at localized or in situ compared to younger women (71 vs. 67 %), and large disparities exist across races regardless of age. The data in Fig. 2 indicate that the stage at diagnosis for women who ever used the BCCP, regardless of whether the diagnosis was before or after age 65 and Medicare coverage, I, is more likely localized or in situ than those actually diagnosed during a BCCP screening; this also holds when comparing BCCP women to all GA breast cancer cases.
Fig. 1.
Georgia breast cancer cases by age, race, and stage at diagnosis
Fig. 2.
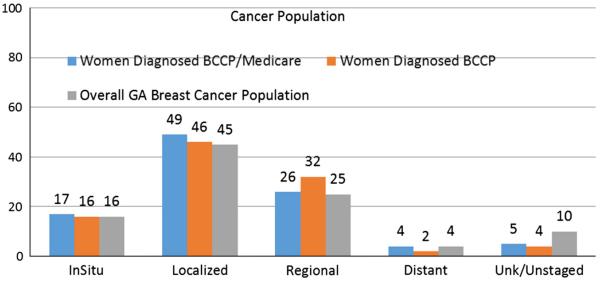
Stage at diagnosis among women diagnosed with BCCP screen, women diagnosed with BCCP screen or under Medicare and overall GA breast
Regression results
The results in Table 4 are marginal effects and can be interpreted, for example, as the difference in the probability of being screened (diagnostic or routine) within 18 months of Medicare enrollment for any BCCP user and “regular” BCCP users, versus non-BCCP users, controlling for Part A/B coverage, disability status, and the presence of comorbidities.
Table 4.
Marginal effects of use of BCCP on the probability of (any) breast cancer screening under medicare in first 18 months of enrollment by evidence of breast cancer and race/ethnicity
| Independent variables for full samplea | Marginal effect: all women Full sample | Marginal effect: White non-Hispanics | Marginal effect: Black non-Hispanics |
|---|---|---|---|
| Any user BCCPb | 0.035** | −0.024 | 0.137*** |
| Regular user BCCP | 0.177*** | 0.156*** | 0.224*** |
| Part A onlyc | −0.506*** | −0.410*** | −0.307*** |
| Part A, non-continuous part Bd | −0.226*** | ||
| Disabled | −0.145*** | −0.157*** | −0.142*** |
| Comorbidities | |||
| Cardiovascular disease (CVD) | 0.005 | −0.012 | 0.025 |
| Dementia | −0.111*** | −0.165** | −0.064 |
| Osteoporosis/arthritis/hip fracture | 0.113*** | 0.128*** | 0.107*** |
| Cataract/glaucoma | 0.120*** | 0.098*** | 0.145*** |
| Chronic kidney disease | −0.042 | −0.021 | −0.050 |
| Chronic obstructive pulmonary disease | −0.073*** | −0.076** | −0.053 |
| Diabetes | 0.020 | 0.001 | 0.046** |
| Depression | −0.010 | −0.027 | 0.038 |
| Stroke/transient ischemic attack | −0.046 | −0.034 | −0.049 |
| Breast cancer | 0.297*** | 0.321*** | 0.264*** |
| Colorectal cancer | 0.086 | 0.042 | 0.171 |
| Lung cancer | −0.084 | −0.000 | −0.347 |
| Endometrial cancer | 0.152 | 0.324 | −0.006 |
| Observations | 12,827 | 7,256 | 5,022 |
p < 0.001;
p < 0.01;
p < 0.05
The sample excludes those women who died within 24 months of their Medicare start date. Additional covariates for the full sample include race and year aging into Medicare
Reference group is women who are non-BCCP users. Regular user is defined as BCCP users with more than one screen and a re-screening within 18 months
Reference group is women with Part A and B continuous coverage over the 24 months
Part A only and Part A/Some B coverage were combined into one category due to small sample sizes
Results indicate that women who had any BCCP use were 3.5 % points more likely than non-BCCP users to be screened within 18 months of Medicare enrollment while “regular” users were even more likely to be screened, almost 18 % points, within that time frame than non-BCCP users. While White non-Hispanic women who ever used the BCCP showed no difference in the probability of screening, both ever and regular users among Black non-Hispanics had significantly higher probabilities (13.7–22.4 % points) than Blacks who never used the BCCP.
Results indicate that enrollment in only Medicare Part A markedly reduces the probability of being screened (50 % points) and having non-continuous Part B coverage and the probability by almost 23 % points relative to having Part A and continuous Part B coverage. Women with disability, regardless of race, are less likely to be screened.
Having certain comorbidities (dementia and COPD) reduce the probability of screening while others (osteoporosis/arthritis/hip fracture; cataract/glaucoma and breast cancer) are associated with increased probabilities of screening. To assess whether these patterns hold for women without a history of breast cancer, we tested models (available upon request) omitting that group; patterns are largely stable overall and across races.
Discussion
This study adds to the literature on the NBCCEDP by focusing on older, low-income women using the NBCCEDP in a state, which has incorporated a specific component, client navigators, to assist BCCP clients in overcoming obstacles to screening such as cost, lack of knowledge about guidelines, lack of information about screening locations, language, and transportation. Many older women use the BCCP for regular screening before aging into Medicare, and the program's targeted outreach and education appear to promote significantly higher levels of regular and timely screening as they age out of the BCCP. Whether due to the client navigator component or unobserved characteristics of women who are BCCP users, we find that Georgia women who use this state's NBCCEDP are more likely than other Medicare enrollees to obtain breast screening soon after aging into Medicare. The effects found here were stronger for non-Hispanic Black women who were regular users of BCCP, an important finding given continued racial disparities in stage at time of diagnosis. [12].
The results presented here suggest there may be a long-term benefit of the BCCP to former participants through instilling and promoting positive screening behaviors that result in cancers detected at an earlier stage than those detected among women who never participated in the BCCP. Our finding that women diagnosed during BCCP screenings are diagnosed at earlier stages, however, may simply reflect that these diagnoses occur at a younger age since women aged 65+ are not eligible to be screened under BCCP if they have Part B coverage. Our finding that BCCP women diagnosed at any time are also diagnosed at earlier stages of disease suggests that their continued screening patterns under Medicare may lead to earlier detection. We also note that the largest absolute differences between the groups analyzed are with respect to the incidence of regional disease, with BCCP rates higher than those covered by Medicare and the Georgia population in general. It is hard to draw conclusions from this finding in the absence of information regarding grade, or receptor status. Receptor status, however, is a better indicator of possible treatment outcomes and which tumors would respond better to which treatments. We are not addressing any treatment options or outcomes in this paper.
A limitation of the study is that it is only for one state's NBCCEDP. While we included women who lived in Georgia while using the BCCP, we also included women who may have resided in other states once enrolled in Medicare. Since Medicare is a national program with uniform coverage, we can still assess their usage. There may be a small percentage of women who moved from one county to another within Georgia, but they would still have access to a BCCP site within each county largely through their local public health departments, which may not hold in other states. The BCCP maintains a roughly 2 % loss to follow-up rate for diagnostic completion among those women who are recommended for breast follow-up after their screening, which minimizes this concern. For women actually diagnosed with breast cancer in the BCCP, the number refusing treatment or who are lost prior to start of treatment is virtually zero.
The BCCP and other states' NBCCEDP provide important access to breast cancer screening and early detection among low-income women. How the NBCCEDP relates to Medicare and Medicaid is important for access to continued screening and if needed, treatment. The NBCCEDP has been linked to Medicaid through the Breast and Cervical Cancer Prevention and Treatment Act (BCCPTA), and evidence for Georgia [13] suggests that this linkage is critical for reducing time to enrollment/treatment among women with a cancer diagnosis. It is important that states maintain and improve their capacity to use surveillance and linked data systems to monitor screening, Medicare and Medicaid enrollment, and related outcomes for poor and near-poor women. In Georgia and other states that have opted out of the Patient Protection and Affordable Care Act (ACA), the NBCCEDP and BCCPTA will continue to be critical for addressing the needs of underserved women.
The NBCCEDP can be especially important to women as they get close to Medicare age; on average, women in our study cohort were 62 when they entered BCCP, perhaps when they lost connection to the work force and employer-sponsored insurance. Educational materials could make these women more aware of Medicare coverage in general and in particular, the “Welcome to Medicare” benefit. This is the first and free visit provided to new Medicare enrollees (within the first 12 months of enrollment in Medicare Part B) and includes an evaluation of preventive screenings, including cancer screening [14]. Only 3 % of new Medicare enrollees were found to use this benefit in 2006, and the key reason was lack of knowledge about it [15]. Salloum et al. [16] report that newly enrolled Medicare eligible women did not take advantage of this benefit, and hence, mammography percentages among this group did not increase. Of newly enrolled women aged 65–66 without a history of breast cancer, 25 % reported a screening compared to 35 % of those aged 67–68 [16].
As women age, the presence of multiple chronic conditions can also influence their screening patterns. Moreover, guidelines do not recommend screening in women with limited life expectancies. Evidence indicates that older women, those in nursing homes and in particular, those with evidence of cognitive impairment are less likely to receive mammograms [17–19]. The presence of other comorbidities, such as rheumatoid arthritis, has not been associated with lower screening percentages [20]. Our results confirm the effect of dementia on lower probability of screening along with other prevalent conditions, such as COPD. Both physicians and their patients will need to make well-informed decisions regarding the benefits of continued screening among older women with and without comorbidities.
Acknowledgments
The funding for this research was provided by the Centers for Disease Control, Division of Cancer Prevention and Control under a Cooperative Agreement SIP11-043: Feasibility of Linking the Georgia Breast and Cervical Cancer Screening Program (BCCP) with the Georgia Cancer Registry (GCR) and Medicare. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.National Breast and Cervical Cancer Early Detection Program (NBCCEDP) [Accessed 25 Feb 2015];About the program. 2014 http://www.cdc.gov/cancer/nbccedp/about.htm.
- 2.Adams E, Florence C, Thorpe K, Becker E, Joski P. Preventive care: female cancer screening, 1996–2000. Am J Prev Med. 2003;25(4):301–307. doi: 10.1016/s0749-3797(03)00216-2. doi:10.1016/S0749-3797(03)00216-2. [DOI] [PubMed] [Google Scholar]
- 3.Adams E, Breen N, Joski P. Impact of the National Breast and Cervical Cancer Early Detection Program on mammography and Pap test utilization among white, Hispanic, and African American women: 1996–2000. Cancer Spec Suppl. 2007;109(2):348–358. doi: 10.1002/cncr.22353. doi:10.1002/cncr.22353. [DOI] [PubMed] [Google Scholar]
- 4.Richardson L, Royalty J, Howe W, Helsel W, Kammerer W, Benard V. Timeliness of breast cancer diagnosis and initiation of treatment in the National Breast and Cervical Cancer Early Detection Program, 1996–2005. Am J Prev Med. 2010;100(9):1769–1776. doi: 10.2105/AJPH.2009.160184. doi:10.1089/jwh.2011.3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lobb R, Allen J, Emmons K, Ayanian J. Timely care after an abnormal mammogram among low-income women in a public breast cancer screening program. Arch Intern Med. 2010;170(6):521–528. doi: 10.1001/archinternmed.2010.22. doi:10.1001/archinternmed.2010.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howard D, Ekwueme D, Gardner J, Tangka F, Li C, Miller J. The impact of a national program to provide free mammograms to low-income, uninsured women on breast cancer mortality rates. Cancer. 2010;116(19):4456–4462. doi: 10.1002/cncr.25208. doi:10.1002/cncr.25208. [DOI] [PubMed] [Google Scholar]
- 7.Hoerger T, Ekwueme D, Miller J, Uzunangelov V, Hall I, Segel J, Royalty J, Gardner J, Smith J, Li C. Estimated effects of the National Breast and Cervical Cancer Early Detection Program on breast cancer mortality. Am J Prev Med. 2011;40(4):397–404. doi: 10.1016/j.amepre.2010.12.017. doi:10.1016/j.amepre.2010.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lantz P, Keeton K, Romano L, et al. Case management in public health screening programs: the experience of the National Breast and Cervical Cancer Early Detection Program. J Public Health Manag Pract. 2004;10(6):545–555. doi: 10.1097/00124784-200411000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Basu M, Linebarger J, Gabram S, Patterson S, Amin M, Ward K. The effect of nurse navigation on timeliness of breast cancer care at an academic comprehensive cancer center. Cancer. 2013;119:2524–2531. doi: 10.1002/cncr.28024. doi:10.1002/cncr.28024. [DOI] [PubMed] [Google Scholar]
- 10.Rakowski W, Breen N, Meissner H, Rimer B, Vernon S, Clark M, Freedman A. Prevalence and correlates of repeat mammography among women aged 55–79 in the year 2000 National Health Interview Survey. Prev Med. 2004;39:1–10. doi: 10.1016/j.ypmed.2003.12.032. doi:10.1016/j.ypmed.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 11.Miller J, King J, Joseph D, Richardson L. [Accessed 25 Feb 2015];Breast cancer screening among adult women-behavioral risk factor surveillance systems, US, 2010. 2012 61(02):46–50. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6102a8.htm. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Vital signs: racial disparities in breast cancer severity—United States, 2005–2009. MMWR Morb Mortal Wkly Rep. 2012;2012(61):922–926. [PubMed] [Google Scholar]
- 13.Adams EK, Chien LN, Florence CS, Raskind-Hood C. The breast and cervical cancer prevention and treatment act in Georgia: effects on time to medicaid enrollment. Cancer. 2009;115(6):1300–1309. doi: 10.1002/cncr.24124. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services (CMS) [Accessed 25 Feb 2015];Your welcome to medicare visit. 2015 http://www.medicare.gov/people-like-me/new-to-medicare/welcome-to-medicare-visit.html.
- 15.Petroski C, Regan J. Use and knowledge of the new enrollee “Welcome to Medicare” physical examination benefit. Health Care Fin Rev. 2009;30(3):71–76. [PMC free article] [PubMed] [Google Scholar]
- 16.Salloum R, Jensen G, Biddle A. The “Welcome to Medicare” visit: a missed opportunity for cancer screening among women? J Women's Health. 2013;22(1):19–25. doi: 10.1089/jwh.2012.3777. doi:10.1089/jwh.2012.3777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Legg J, Clement D, White K. Are women with self-reported cognitive limitations at risk for underutilization of mammography? J Health Care Poor Underserved. 2004;15(4):688–702. doi: 10.1353/hpu.2004.0066. doi:10.1353/hpu.2004.0066. [DOI] [PubMed] [Google Scholar]
- 18.Mehta K, Fung K, Kistler C, Chang A, Walter L. Impact of cognitive impairment on screening mammography use in older US women. Am J Pub Health. 2010;100(10):1917–1923. doi: 10.2105/AJPH.2008.158485. doi:10.2105/AJPH.2008.158485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marwill S, Freund K, Barry P. Patient factors associated with breast cancer screening among older women. J Am Geriatr Soc. 1996;44(10):1210–1214. doi: 10.1111/j.1532-5415.1996.tb01371.x. [DOI] [PubMed] [Google Scholar]
- 20.Kim S, Sheneeweiss S, Myers J, Liu J, Solomon D. No differences in cancer screening rates in patients with rheumatoid arthritis compared to the general population. Arthritis Rheum. 2012;64(10):3076–3082. doi: 10.1002/art.34542. doi:10.1002/art.34542. [DOI] [PMC free article] [PubMed] [Google Scholar]