Abstract
BACKGROUND
Primary tumors of the spinal cord, spinal meninges, and cauda equina are relatively rare, and a paucity of population-based data exist on tumors in these sites. This study intends to augment the current literature by examining incidence of these tumors on a national level.
METHODS
Data from central cancer registries in the National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) programs for 2004–2007 (covering 99.2% of US population) and 1999–2007 (covering 89.4% of US population) were analyzed. Analyses for diagnosis years 2004–2007 included cases of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors. Descriptive statistics including estimated age-adjusted incidence rates standardized to the 2000 US standard population were conducted for both malignant and nonmalignant primary spinal tumors from cases diagnosed during 2004–2007 as well as trend analyses on malignant cases of primary spinal tumors (n = 5103) for cases diagnosed during 1999–2007 using SEER*Stat 6.6.2 software.
RESULTS
There were 2576 cases of malignant primary spinal tumors and 9136 cases of nonmalignant primary spinal tumors in 2004–2007. The incidence of malignant and nonmalignant primary spinal tumors combined differed by age, sex, race, and ethnicity. Results of trend analyses indicated that malignant primary spinal tumors have been stable throughout the 1999–2007 period.
CONCLUSIONS
This large population-based study adds new insights into the descriptive epidemiology of primary spinal cord, spinal meninges, and cauda equina tumors by providing in-depth analyses of the incidence of these tumors on a national level.
Keywords: spinal cord, spinal meninges, cauda equine, epidemiology, histology
INTRODUCTION
Primary tumors of the spinal cord, spinal meninges, and cauda equina (subsequently referred to as “spinal tumors”) are relatively rare,1–5 and there is a paucity of population-based data available on tumors in these sites.6 This is due, in large part, to the limited availability of cases ascertained with these tumors at single clinical settings.7 The rarity of these tumors has significant ramifications on patient outcomes, as it limits the level of research, treatment decisions, and health care planning. As a result, large population-based data sources are needed to provide accurate descriptive statistics on primary spinal tumors.7 With the institution of population-based cancer data sources, such as the Centers for Disease Control and Prevention (CDC) National Program of Cancer Registries (NPCR), the Central Brain Tumor Registry of the United States (CBTRUS), and the National Cancer Institute (NCI) Surveillance, Epidemiology, and End Results (SEER) Program, analyses can now be conducted on primary spinal tumors on a population-based level.7,8 Consequently, population-based incidence rates can be calculated, assisting in measuring the burden of primary spinal tumors in the population. Moreover, variations in these incidence patterns can help inform and stimulate research on primary spinal tumors.
On a national level, data collection of primary spinal tumors before 2004 in the United States focused on malignant behavior only. The exclusion of nonmalignant cases has restricted the ability to capture accurately the total burden of all primary spinal tumors in this population. However, there have been studies that have evaluated the incidence of nonmalignant spinal tumors in conjunction with malignant spinal tumors. CBTRUS has published data analyses on incident malignant and nonmalignant (benign and uncertain behavior) primary spinal cord tumors before the 2004 mandate to collect nonmalignant cases in conjunction with malignant cases in the United States.6,9
In January 2004, central cancer registries began collecting data on nonmalignant primary brain and central nervous system (CNS) tumors, including spinal tumors, as a result of the passage of Public Law 107–260, the Benign Brain Tumor Cancer Registries Amendment Act.10 Consequently, a more complete data set of the incidence of primary spinal tumors is available for study on a national level beginning with the 2004 diagnosis year. This study is intended to augment the current literature by analyzing data on primary spinal cord, spinal meninges, and cauda equina tumors. Specifically, these analyses focus on malignant and nonmalignant spinal tumor incidence by histology using the NPCR database in conjunction with the SEER program for diagnosis years 2004–2007 and also evaluate trends in primary malignant spinal tumors for diagnosis years 1999–2007.
MATERIALS AND METHODS
Incident malignant and nonmalignant primary spinal tumor cases were identified from population-based cancer registries that participated in CDC’s NPCR or NCI’s SEER program. NPCR supports central cancer registries in 45 states, the District of Columbia, Puerto Rico, and US Pacific Island jurisdictions, covering approximately 96% of the US population.8 Together, NPCR and SEER collect cancer incidence data for the entire US population.8,11 Cancer incidence data included those from the 2010 NPCR-Cancer Surveillance System submission and the November 2009 SEER submission. The study involved 2 separate analyses. The first analysis focused on a cross-sectional evaluation of incident primary malignant and nonmalignant spinal tumor cases diagnosed in the years 2004–2007 from central cancer registries in 49 states and the District of Columbia that met case ascertainment and quality criteria for all 4 years.11 These data cover approximately 99.2% of the US population during these 4 years. Data from 1 central cancer registry was excluded because it did not meet the case ascertainment and quality criteria for all 4 years. The second analysis focused on trends for data on incident primary malignant spinal tumor cases diagnosed in the years 1999–2007 from central cancer registries in 43 states that met case ascertainment and quality criteria for all 9 years.11 These data covered approximately 89.4% of the US population during the 9 years. Data from 7 states and the District of Columbia (8 CCRs) were excluded because case ascertainment and quality criteria standards were not met for the entire time period.
Primary spinal tumors in both sets of analyses were defined using the following topography codes (primary sites): C70.1 (spinal meninges), C72.0 (spinal cord), and C72.1 (cauda equina).12,13 Tumors were included regardless of the type of diagnostic confirmation (pathologically, radiographically, or clinically diagnosed) if they were the only primary tumor or the first of 2 or more independent primary tumors for a patient; 395 (3.3% of all spinal tumors) second or later primary tumors were excluded from the analyses as it was not always possible to determine whether these second or later primaries resulted from other CNS tumors. Separate analyses indicated that the study conclusions did not change with the exclusion of these tumors.
Primary spinal tumor histological groupings were coded according to the version of the International Classification of Disease for Oncology (ICD-O) used at the time of diagnosis.12,13 As a result, primary spinal tumor cases diagnosed during 1999–2000 used the ICD-O second edition (ICD-O-2), whereas 2001–2007 cases used the ICD-O third edition (ICD-O-3); data from the 1999–2000 diagnosis years were converted to the ICD-O-3 codes. Fewer than 16 cases changed between ICD-O-2 and ICD-O-3 versions and were therefore excluded from this analysis. Nineteen invalid brain/CNS tumor cases were also excluded from the 2004–2007 analytic data set, and 5 invalid brain/CNS tumor cases were excluded from the 1999–2007 analytic data set. Invalid brain/CNS cases were defined as those histologies that appeared to be errors in coding. The histology categories used in this study were modeled after the classification scheme used for reporting of primary brain tumors, irrespective of behavior, in place since 1994 as developed by CBTRUS.14 These groupings are broadly based on the World Health Organization categories for brain tumors.15 The reader should be aware that histology 9383 has been used to identify both “other astrocytomas” and “ependymomas.” As both “other astrocytomas” and “ependymomas” represent primary glial neoplasms, and as these histologies in the spinal cord, especially the tanycytic histologic variant of ependymoma, are often confused with each other, the classification scheme does not influence the conclusions presented in this article. Table 1 shows the histology categories and ICD-O-3 codes used to define primary spinal tumors for diagnosis years 2004–2007 and diagnosis years 1999–2007. For completeness, 28 death certificate only cases were included in the 2004–2007 analytic data set, and 52 death certificate only cases were included in the 1999–2007 analytic data set.
Table 1.
Histology Categories and ICD-O-3 Codes Used to Define Primary Spinal Cord, Spinal Meninges, and Cauda Equina Tumors, 2004–2007 and 1999–2007
| Primary Spinal Tumor Histology Definitions |
ICD-O-3 Codes |
|---|---|
| Tumors of neuroepithelial tissue Ependymoma | 9391, 9392, 9393, 9394 |
| Pilocytic astrocytoma | 9421 |
| Other astrocytic tumors | 9410, 9420, 9401, 9411, 9383, 9384, 9424, 9400, 9440, 9441, 9442/3a |
| Tumors of spinal nerves | 9540, 9541, 9550, 9560, 9561, 9570, 9571, 9562 |
| Tumors of meninges Meningioma | 9530, 9531, 9532, 9533, 9534, 9537, 9538, 9539 |
| Hemangioblastoma | 9161, 9535 |
| Other mesenchymal | 8324, 8728, 8800, 8801, 8802, 8803, 8804, 8805, 8806, 8810, 8815, 8824, 8830, 8831, 8850, 8851, 8852,b 8854,b 8857, 8861, 8870,b 8890, 8897, 8900, 8910, 8920, 8990, 9040, 9150, 9170,b 9180, 9210, 9241, 9260, 9480, 9536b |
| Lymphomas | 9590, 9591, 9596, 9650, 9651, 9652, 9653, 9654, 9655, 9659, 9661, 9662, 9663, 9664, 9665, 9667, 9670, 9671, 9673, 9675, 9680, 9684, 9687, 9690, 9691, 9695, 9698, 9699, 9701, 9702, 9705, 9714, 9719,9727, 9728, 9729, 9731, 9733, 9734, 9740, 9741, 9750, 9755, 9756, 9757, 9758, 9766, 9826,b 9827, 9860,b, 9861, 9930, 9970 |
| Otherc | 8680, 8693, 8711, 8963, 9064, 9070,d 9071,d 9080, 9084, 9085, 9220, 9231, 9240, 9364, 9370, 9371, 9380, 9382, 9390, 9412, 9413, 9430,d 9450, 9451, 9470, 9473, 9490, 9492, 9500, 9501, 9503, 9505, 9506, 9508 |
| Unclassified tumors | 9120, 9121, 9122, 9123, 9125, 9130, 9131, 9133, 9140, 8000, 8001, 8002, 8003, 8004, 8005, 8010, 8013, 8021, 8452,b 8683, 8720, 8811, 8840, 8860, 8896, 8980, 9173, 9580, 9751, 9752, 9753, 9754, 9823, 9837, 9866 |
Abbreviations: CNS, central nervous system; ICD-O-3, International Classification of Disease for Oncology, 3rd edition, 2000 (World Health Organization, Geneva, Switzerland).
Twenty-eight death certificate only cases were included in the 2004–2007 data set, and 52 death certificate only cases were included in the 1999–2007 data set. Nineteen invalid brain/CNS tumor cases were excluded from the 2004–2007 data set, and 5 invalid brain/CNS tumor cases were excluded from the 1999–2007 data set. Invalid brain/CNS cases were defined as those histologies that appeared to be errors in coding.
Morphology 9442/3 only.
Histologies added in the 2009 revision of the Central Brain Tumor Registry of the United States histology grouping scheme as compared to the previous versions.
Other includes neuronal/glial, nonmalignant and malignant, chordoma/chondrosarcoma, embryonal/primitive/medulloblastoma, germ cell tumors and cysts, glioma malignant, not otherwise specified, mixed glioma, choroid plexus, oligodendroglioma, and anaplastic oligodendroglioma.
Histologies found only in the 1999–2007 National Program of Cancer Registries and Surveillance, Epidemiology, and End Results data set.
Race was categorized as white, black, American Indian/Alaska Native, Asian/Pacific Islander, and other/unknown race. To increase the accuracy of the American Indian/Alaska Native designation, linkages between the central cancer registries and the Indian Health Service database were completed before data submission to NPCR and SEER. Ethnicity was categorized as Hispanic or non-Hispanic. Race and ethnicity were not mutually exclusive.
Statistical Analysis
Frequencies by demographic and tumor characteristics for all primary spinal tumors were calculated. Age-adjusted incidence rates with 95% confidence intervals for all primary spinal tumors were calculated overall, and by behavior, sex, race/ethnicity, region, histology grouping, and diagnosis year. Rates were expressed per 100,000 persons and age-adjusted using the US 2000 population standard (19 age groups; Census P25-1130). The male to female rate ratios were calculated by dividing the age-adjusted incidence rates for male cases by those for female cases. Counts and rates based on <16 cases were not presented, to ensure rate stability and confidentiality. Moreover, annual percentage change and percentage change between years were calculated for malignant primary spinal tumors over time for diagnosis years 1999–2007. Annual percentage change was calculated using the weighted least squares method. All data analyses for this study were performed using SEER*Stat version 6.6.2.16
RESULTS
Table 2 shows demographic and tumor characteristics for all primary spinal tumors by behavior for cases diagnosed during the 2004–2007 period. Of the reported 11,712 primary spinal tumor incident cases diagnosed from 2004 to 2007, 2576 (22.0%) were malignant, and 9136 (78.0%) were nonmalignant (62.4% benign and 15.6% borderline). There were 1823 primary spinal tumors with borderline behavior, of which the most common histologic types were myxopapillary ependymomas (62%; includes ependymoma, not otherwise specified); hemangioblastoma (14%); and atypical, chordoid, and clear cell meningiomas (5%). Six percent of tumors with borderline behavior were “unclassified” (ie, nonspecific) tumors. The remaining 13% of these tumors were widely distributed among a variety of histological subtypes including “other astrocytic tumors,” “tumors of the cranial and spinal nerves,” “other mesenchymal tumors,” and other histologies (Table 1). The age-adjusted incidence rate for nonmalignant primary spinal tumors (0.76 per 100,000 persons) was significantly higher than the observed rate for malignant tumors (0.22 per 100,000 persons).
Table 2.
Description of Primary Spinal Cord, Spinal Meninges, and Cauda Equina Tumor Incidence by Selected Characteristics, United States, 2004–2007
| Characteristic | Total | Malignant | Nonmalignant | |||
|---|---|---|---|---|---|---|
| Counta (%) | Rateb [95% CI]c | Count (%) | Rate [95% CI] | Count (%) | Rate [95% CI] | |
| Total | 11,712 (100.0) | 0.97 [0.96–0.99] | 2576 (100.0) | 0.22 [0.21–0.22] | 9136 (100.0) | 0.76 [0.74–0.77] |
| Age at diagnosis, years | ||||||
| Birth-9 | 364 (3.1) | 0.23 [0.21–0.25] | 229 (8.9) | 0.14 [0.13–0.16] | 135 (1.5) | 0.09 [0.07–0.10] |
| 10–19 | 505 (4.3) | 0.30 [0.28–0.33] | 208 (8.1) | 0.13 [0.11–0.14] | 297 (3.3) | 0.18 [0.16–0.20] |
| 20–29 | 774 (6.6) | 0.47 [0.44–0.51] | 227 (8.8) | 0.14 [0.12–0.16] | 547 (6.0) | 0.34 [0.31–0.37] |
| 30–39 | 1277 (10.9) | 0.79 [0.75–0.83] | 331 (12.8) | 0.20 [0.18–0.23] | 946 (10.4) | 0.58 [0.55–0.62] |
| 40–49 | 2059 (17.6) | 1.15 [1.10–1.20] | 507 (19.7) | 0.28 [0.26–0.31] | 1552 (17.0) | 0.87 [0.82–0.91] |
| 50–59 | 2348 (20.0) | 1.57 [1.50–1.63] | 466 (18.1) | 0.31 [0.28–0.34] | 1882 (20.6) | 1.25 [1.20–1.31] |
| 60–69 | 1883 (16.1) | 2.01 [1.92–2.10] | 313 (12.2) | 0.33 [0.30–0.37] | 1570 (17.2) | 1.67 [1.59–1.76] |
| 70–79 | 1601 (13.7) | 2.53 [2.41–2.66] | 197 (7.6) | 0.31 [0.27–0.36] | 1404 (15.4) | 2.22 [2.10–2.34] |
| ≥80 | 901 (7.7) | 2.09 [1.96–2.23] | 98 (3.8) | 0.23 [0.18–0.28] | 803 (8.8) | 1.87 [1.74–2.00] |
| Sex | ||||||
| Male | 4791 (40.9) | 0.83 [0.81–0.86] | 1312 (50.9) | 0.23 [0.21–0.24] | 3479 (38.1) | 0.61 [0.59–0.63] |
| Female | 6921 (59.1) | 1.09 [1.06–1.11] | 1264 (49.1) | 0.21 [0.20–0.22] | 5657 (61.9) | 0.88 [0.86–0.91] |
| Race | ||||||
| White | 10,128 (86.5) | 1.01 [0.99–1.03] | 2207 (85.7) | 0.23 [0.22–0.24] | 7921 (86.7) | 0.79 [0.77–0.80] |
| Black | 885 (7.6) | 0.63 [0.59–0.68] | 228 (8.9) | 0.15 [0.13–0.18] | 657 (7.2) | 0.48 [0.44–0.52] |
| American Indian/Alaska Native | 67 (0.6) | 0.64 [0.49–0.82] | 18 (0.7) | 0.14 [0.08–0.23] | 49 (0.5) | 0.50 [0.36–0.67] |
| Asian/Pacific Islander | 386 (3.3) | 0.76 [0.68–0.84] | 79 (3.1) | 0.15 [0.11–0.18] | 307 (3.4) | 0.61 [0.54–0.69] |
| Other unspecified/unknown race | 246 (2.1) | d | 44 (1.7) | d | 202 (2.2) | d |
| Ethnicitye | ||||||
| Hispanic | 1002 (8.6) | 0.77 [0.72–0.83] | 300 (11.6) | 0.20 [0.18–0.23] | 702 (7.7) | 0.57 [0.52–0.62] |
| Non-Hispanic | 10,710 (91.4) | 1.00 [0.98–1.02] | 2276 (88.4) | 0.22 [0.21–0.23] | 8434 (92.3) | 0.78 [0.77–0.80] |
| Region | ||||||
| Northeast | 2724 (23.3) | 1.18 [1.13–1.22] | 529 (20.5) | 0.23 [0.21–0.26] | 2195 (24.0) | 0.94 [0.90–0.98] |
| Midwest | 2442 (20.9) | 0.90 [0.87–0.94] | 530 (20.6) | 0.20 [0.18–0.22] | 1912 (20.9) | 0.70 [0.67–0.74] |
| South | 4178 (35.7) | 0.95 [0.92–0.98] | 918 (35.6) | 0.21 [0.20–0.22] | 3260 (35.7) | 0.74 [0.72–0.77] |
| West | 2368 (20.2) | 0.91 [0.88–0.95] | 599 (23.3) | 0.23 [0.21–0.25] | 1769 (19.4) | 0.69 [0.66–0.72] |
| Microscopic confirmation, %f | 10,600 (90.5) | d | 2421 (94.0) | d | 8179 (89.5) | d |
| Primary site | ||||||
| Spinal meninges | 4219 (36.0) | 0.35 [0.34–0.36] | 154 (6.0) | 0.01 [0.01–0.02] | 4065 (44.5) | 0.34 [0.33–0.35] |
| Spinal cord | 7082 (60.5) | 0.59 [0.58–0.61] | 2337 (90.7) | 0.20 [0.19–0.20] | 4745 (51.9) | 0.40 [0.39–0.41] |
| Cauda equina | 411 (3.5) | 0.03 [0.03–0.04] | 85 (3.3) | 0.01 [0.01–0.01] | 326 (3.6) | 0.03 [0.02–0.03] |
| Histology | ||||||
| Ependymoma | 2478 (21.2) | 0.21 [0.20–0.22] | 1320 (51.2) | 0.11 [0.10–0.12] | 1158 (12.7) | 0.10 [0.09–0.10] |
| Pilocytic astrocytoma | 194 (1.7) | 0.02 [0.02–0.02] | 194 (7.5) | 0.02 [0.02–0.02] | 0 (0.0) | 0.00 [0.00-0.00] |
| Other astrocytic tumors | 336 (2.9) | 0.03 [0.03–0.03] | 310 (12.0) | 0.03 [0.02–0.03] | 26 (0.3) | 0.00 [0.00-0.00] |
| Tumors of spinal nerves | 3125 (26.7) | 0.26 [0.25–0.27] | 59 (2.3) | 0.01 [0.00–0.01] | 3066 (33.6) | 0.25 [0.25–0.26] |
| Meningioma | 3820 (32.6) | 0.32 [0.31–0.33] | 63 (2.4) | 0.01 [0.00–0.01] | 3757 (41.1) | 0.31 [0.30–0.32] |
| Hemangioblastoma | 269 (2.3) | 0.02 [0.02–0.03] | g | g | g | 0.02 [0.02–0.03] |
| Other mesenchymal | 179 (1.5) | 0.02 [0.01–0.02] | g | 0.00 [0.00-0.00] | g | 0.01 [0.01–0.02] |
| Lymphomas | 306 (2.6) | 0.03 [0.02–0.03] | 306 (11.9) | 0.03 [0.02–0.03] | 0 (0.0) | 0.00 [0.00-0.00] |
| Other | 470 (4.0) | 0.04 [0.04–0.04] | 227 (8.8) | 0.02 [0.02–0.02] | 243 (2.7) | 0.02 [0.02–0.02] |
| Unclassified tumors | 535 (4.6) | 0.04 [0.04–0.05] | 67 (2.6) | 0.01 [0.00–0.01] | 468 (5.1) | 0.04 [0.04–0.04] |
| Diagnosis year | ||||||
| 2004 | 2820 (24.1) | 0.96 [0.92–0.99] | 670 (26.0) | 0.23 [0.21–0.25] | 2150 (23.5) | 0.73 [0.70–0.76] |
| 2005 | 2995 (25.6) | 1.00 [0.97–1.04] | 671 (26.0) | 0.23 [0.21–0.24] | 2324 (25.4) | 0.78 [0.75–0.81] |
| 2006 | 2998 (25.6) | 0.99 [0.95–1.03] | 622 (24.1) | 0.21 [0.19–0.22] | 2376 (26.0) | 0.78 [0.75–0.82] |
| 2007 | 2899 (24.8) | 0.95 [0.91–0.98] | 613 (23.8) | 0.20 [0.19–0.22] | 2286 (25.0) | 0.74 [0.71–0.77] |
Counts pertain to 99.2% of the US population covered by eligible cancer registries. Data from 1 central cancer registry are not included. Percentages may not add to 100% because of rounding.
Rates are per 100,000 persons and age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130), except age-specific rates, which were not age-adjusted.
Ninety-five percent confidence intervals (CIs) were calculated using the Tiwari modification.
Race and ethnicity are not mutually exclusive.
Indicates that rates could not be calculated or not applicable.
Indicates that percentage microscopic confirmation includes positive histology, positive exfoliative cytology; no positive histology, and positive microscopic confirm; method not specified.
Indicates that the count was <16 for 2004–2007 and was suppressed or that the number was complementarily suppressed for 2004–2007 to ensure patient privacy and confidentiality.
Age-specific rate patterns were similar for total and nonmalignant primary spinal tumors. That is, rates gradually increased with advancing age groups, peaking at 70 to 79 years of age and declining slightly at ≥80 years. However, for malignant primary spinal tumors, rates peaked at 60 to 69 years of age and declined at 70 to 79 years of age. The age-specific incidence rate for malignant and nonmalignant primary spinal tumors combined was lowest in children aged 0 to 9 years (0.23 per 100,000 persons) and was highest in adults aged 70 to 79 years (2.53 per 100,000 persons). The total age-specific incidence rate in children (0–19 years) was 0.27 per 100,000 persons and in adults (≥20 years) the total age-specific incidence rate was 1.27 per 100,000 persons.
Differences in primary spinal tumors by behavior and sex were also noted. Among malignant cases, the frequency was distributed almost equally by sex, whereas among nonmalignant cases approximately 60% were diagnosed in women compared with 40%inmen. The total and nonmalignant primary spinal tumor age-adjusted rates in women were significantly greater than those observed for men, but no significant difference was seen in a comparison of malignant age-adjusted rates by sex.
Among total, malignant, and nonmalignant cases, the predominant race group was white (approximately 85%) distantly followed by black race. Age-adjusted rates for total and nonmalignant primary spinal tumors were significantly greater for white cases than black, American Indian/Alaska Native, or Asian/Pacific Islander cases. Malignant age-adjusted rates were significantly higher among white cases than black or Asian/Pacific Islander race groups but not for cases of American Indian/Alaska Native race. With respect to ethnicity, non-Hispanics accounted for approximately 90% of the reported cases and were observed to have significantly higher total and nonmalignant age-adjusted rates than Hispanic cases, but the malignant primary spinal tumor rates were not significantly different between the 2 ethnicity groups.
The geographic region with the largest proportion of cases in the cohort (approximately 35%) was observed to be the South, with about 20% to 25% of the remaining cases distributed in each of the remaining 3 regions (Northeast, Midwest, and West). However, the region with the highest total and nonmalignant incidence rates for primary spinal tumors was the Northeast, and these rates were significantly greater than those observed for the Midwest, South, and West regions. Malignant rates among the 4 geographic regions were not significantly different.
Proportionately, the distribution of cases by primary spinal tumor site was similar for total, malignant, and nonmalignant behavior groups. The largest numbers of cases were diagnosed in the spinal cord, followed by the spinal meninges, and then cauda equina, which had the smallest number of cases. However, the distribution within behavior groups varied considerably, as did differences in the magnitudes of age-adjusted incidence rates.
Overall, the most common primary spinal tumor histological types were meningiomas, tumors of spinal nerves, and ependymomas. For malignant behavior cases, ependymoma was most common, whereas meningioma was predominant among nonmalignant cases. The magnitude of histology-specific age-adjusted incidence rates paralleled these observed frequency patterns.
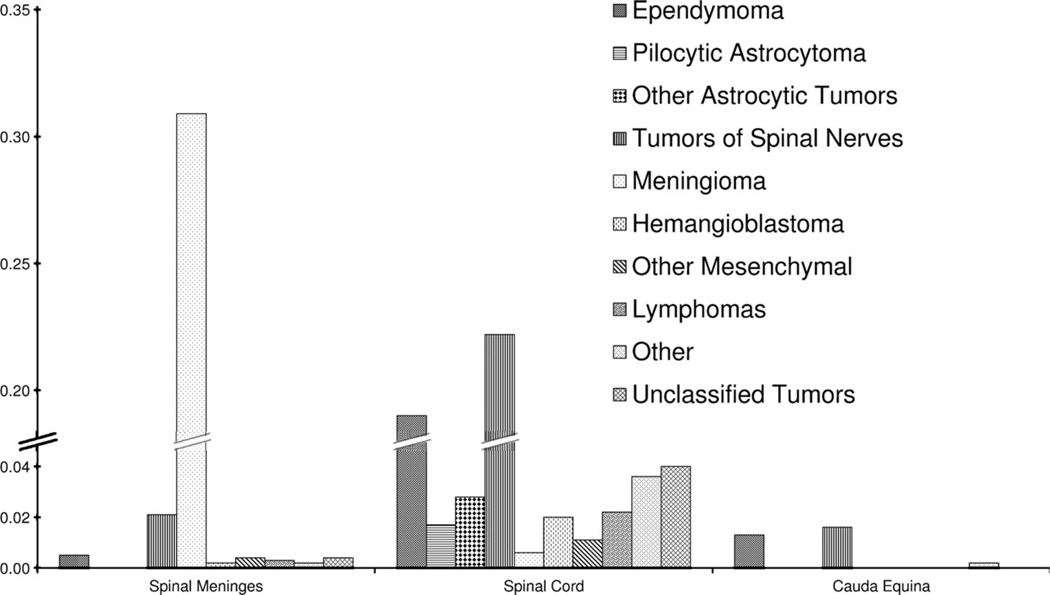
Figure 1 presents combined malignant and nonmalignant primary spinal tumor incidence rates by primary site and histology. Generally, the spinal meninges had the highest incidence rate of meningiomas, whereas the spinal cord had the highest incidence rate of tumors of spinal nerves followed closely by ependymomas. For cauda equina, tumors of spinal nerves were the most common, followed closely by ependymomas.
Figure 1.
Malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumor incidence rates are shown by primary site and histology, for the United States, 2004–2007. Rates pertain to 99.2% of U.S. population covered by eligible cancer registries. Data from 1 central cancer registry is not included. Rates are per 100,000 persons and age-adjusted to the 2000 U.S. standard population (19 age groups - Census P25-1130). “Other” includes neuronal/glial, nonmalignant and malignant, chordoma/chondrosarcoma, embryonal/primitive/medulloblastoma, germ cell tumors and cysts, glioma malignant, not otherwise specified, mixed glioma, choroid plexus, oligodendroglioma, and anaplastic oligodendroglioma.
Table 3 shows male to female age-adjusted rate ratios for histologic-specific primary spinal tumors for diagnosis years 2004–2007. Statistically significant differences in rates by histology type between sexes were found for ependymomas (male:female rate ratio 1.15), tumors of spinal nerves (male:female rate ratio 1.11), meningiomas (male:female rate ratio 0.28), and lymphomas (male:female rate ratio 1.76). Men had significantly higher rates than women for ependymomas, tumors of spinal nerves, and lymphomas, but lower rates than women for meningiomas.
Table 3.
Malignant and Nonmalignant Primary Spinal Cord, Spinal Meninges, and Cauda Equina Tumor Histology Male-Female Rate Ratio, United States, 2004–2007a
| Sex | Total | Male | Female | Male-Female Rate Ratio (95% CI)c |
|||
|---|---|---|---|---|---|---|---|
| Histology | Count | Rateb | Count | Rate | Count | Rate | |
| Ependymoma | 2478 | 0.21 | 1299 | 0.22 | 1179 | 0.19 | 1.15 (1.06–1.24)d |
| Pilocytic astrocytoma | 194 | 0.02 | 110 | 0.02 | 84 | 0.02 | 1.28 (0.95–1.72) |
| Other astrocytic tumors | 336 | 0.03 | 178 | 0.03 | 158 | 0.03 | 1.15 (0.92–1.43) |
| Tumors of spinal nerves | 3125 | 0.26 | 1590 | 0.27 | 1535 | 0.25 | 1.11 (1.04–1.20)d |
| Meningioma | 3820 | 0.32 | 723 | 0.13 | 3097 | 0.47 | 0.28 (0.26–0.30)d |
| Hemangioblastoma | 269 | 0.02 | 141 | 0.02 | 128 | 0.02 | 1.15 (0.89–1.47) |
| Other mesenchymal | 179 | 0.02 | 93 | 0.02 | 86 | 0.01 | 1.14 (0.84–1.55) |
| Lymphomas | 306 | 0.03 | 184 | 0.03 | 122 | 0.02 | 1.76 (1.39–2.24)d |
| Other | 470 | 0.04 | 243 | 0.04 | 227 | 0.04 | 1.10 (0.91–1.32) |
| Unclassified tumors | 535 | 0.04 | 230 | 0.04 | 305 | 0.05 | 0.86 (0.72–1.03) |
Counts pertain to 99.2% of the US population covered by eligible cancer registries. Data from 1 central cancer registry are not included.
Rates are per 100,000 persons and age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130).
Ninety-five percent confidence intervals (CIs) were calculated using the Tiwari modification.
Indicates that the male rate is significantly different from the female rate (P < 0.05) as calculated by the rate ratio.
Table 4 shows the change in incidence rates over time for all malignant primary spinal tumors diagnosed during 1999–2007. Rates of malignant primary spinal tumors did not change significantly during this time period.
Table 4.
Trends in Malignant Primary Spinal Tumor Annual Age-Adjusted Incidence Rates, Male and Female, United States, 1999–2007a
| Year | All Malignant Spinal Tumors | ||
|---|---|---|---|
| Count | Rateb (95% CI)c |
Percentage Change |
|
| 1999 | 531 | 0.21 (0.20–0.23) | |
| 2000 | 552 | 0.22 (0.20–0.24) | 4.8 |
| 2001 | 548 | 0.22 (0.20–0.23) | 0.0 |
| 2002 | 544 | 0.21 (0.19–0.23) | −4.5 |
| 2003 | 571 | 0.22 (0.20–0.24) | 4.8 |
| 2004 | 602 | 0.23 (0.21–0.25) | 4.5 |
| 2005 | 610 | 0.23 (0.21–0.25) | 0.0 |
| 2006 | 578 | 0.21 (0.20–0.23) | −8.7 |
| 2007 | 567 | 0.21 (0.19–0.23) | 0.0 |
| Annual percentage changed | 0.03 (−1.02–1.10) | ||
| Total percentage change | −2.66 | ||
Counts pertain to 89.4% of the US population covered by eligible cancer registries. Data from 8 central cancer registries are not included.
Rates are per 100,000 persons and age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130).
Ninety-five percent confidence intervals (CIs) were calculated using the Tiwari modification.
Annual percent change was calculated using weighted least squares method.
DISCUSSION
Our analyses add new insights into the descriptive epidemiology of primary spinal tumors and provide a more complete understanding of the incidence of these tumors on a national level. This study complements a recent study published by Engelhard et al that reported the clinical presentation, histology, and treatment of 430 patients with primary tumors of the spinal cord, spinal meninges, and cauda equina.4 Together, these studies provide a comprehensive perspective of the epidemiology of primary spinal tumors.
In our study, the most common site of all primary spinal tumors combined was the spinal cord (60.5%), followed by spinal meninges (36.0%), and then cauda equina (3.5%). This result is similar to a study by Schellinger et al (spinal cord, 70.0%; spinal meninges, 26.0%; cauda equina, 4.0%).6 However, our results differ from a study in Norway that found equal proportions of spinal cord and spinal meninges, and a study in Croatia finding that >½ of the tumors diagnosed in this population were located in the spinal meninges.17,18 Possible explanations for these differences may be attributed to small sample size or population differences within the Norway and Croatia data sets.
Results from our analyses confirm previous findings of frequencies of histology types and sex differences.6 Schellinger et al reported that the most common spinal tumor histologic types were meningiomas (29%), nerve sheath tumors (24%), and ependymomas (23%), which closely matches our findings (meningiomas, 33%; tumors of spinal nerves, 27%; ependymomas, 21%).6 In addition, a study in Croatia had similar findings.18 Moreover, a population-based study conducted in Los Angeles also found that ependymoma was the most prevalent type of glioma, which is similar to the findings of this study.19 Lastly, a study using the National Cancer Database by Engelhard et al found that the most common tumor types were meningioma (24.4%), ependymoma (23.7%), and schwannoma (21.2%).4
The overall incidence of spinal tumors (malignant and nonmalignant combined) found in our study (0.97 per 100,000 persons) is lower than that found in France (1.20 per 100,000 persons),3 Croatia (1.60 per 100,000 persons),18 or Rochester, Minnesota (2.50 per 100,000 persons),20 but is higher than that observed in a study by Schellinger et al (0.74 per 100,000 persons)6 or Estonia (0.80 per 100,000 persons).5 Sample size and population differences may explain differences found in France, Croatia, Minnesota, and Estonia. The collection of nonmalignant tumors in the United States improved substantially with diagnosis year 2004, and given that the Schellinger study was conducted before 2004, the differences in rates between that study and the current study may be explained simply by completeness in reporting. However, there still remains the potential for continued underreporting of nonmalignant spinal meninges in the United States. As a result, continued surveillance of the descriptive epidemiology of spinal tumors is important. With regard to sex differences, Schellinger et al found that the overall incidence rate among men was 0.70 per 100,000 persons, whereas women had an incidence rate of 0.77 per 100,000 persons,6 which is similar to our findings of sex differences, although the incidence rates between men and women were greater in our study. This difference is likely because of better collection of nonmalignant meningiomas and nonmalignant tumors in general.6 Similarly to our study, Schellinger et al found that incidence rates were lowest in children aged 0 to 19 years and highest in adults aged 75 to 84 years.6 Likewise, similar age-specific rate patterns were also found in South Korea and Estonia.2,5
Since the passage of Public Law 107–260, the Benign Brain Tumor Cancer Registries Amendment Act, incident cases of nonmalignant brain and CNS tumors have been collected beginning with diagnosis year 2004. Our analyses revealed that 78.0% of primary spinal tumors were nonmalignant, accounting for the majority of incident cases for diagnosis years 2004–2007. Nonmalignant spinal tumors are space occupying lesions, and as such are associated with weakness, paresthesias, and paralysis. Omission of these nonmalignant cases in past data collections may have resulted in an underestimation of the incidence of primary spinal tumors, and consequently, may have inadvertently created a perception of a lower burden of disease on the population.21 As a result of mandating, by public law, the collection of nonmalignant primary spinal tumors in conjunction with malignant primary spinal tumors in 2004, population-based surveillance of cancer is able to capture the burden of this disease more completely in the US population.
Our findings should be considered in light of several limitations. We did not account for reporting delays in the data. It is likely that reporting delays are larger for nonmalignant tumors than for malignant tumors, as they are less likely to be diagnosed and/or reported from the traditional reporting sources for malignant tumors. There have also been changes in the multiple primary rules, which could affect the magnitude of the numerators in the calculation of incidence rates. Moreover, the variability in incidence rates between states is much larger for nonmalignant than for malignant tumors, suggesting that there still may be some data collection issues with regard to completeness of the data for the nonmalignant tumors. In registry data, there is a possibility of misclassification or miscoding, especially with rare tumors. Taking this into account, reasoned assumptions have been made with the analyses. For example, nerve sheath tumors coded to meninges may not be accurately coded, but likely represent true tumors in the region under study. In addition, data were not available for 1 central cancer registry in the 2004–2007 analytic data set, and data were not available for 8 central cancer registries in the 1999–2007 analytic data set. The exclusion of these central cancer registries may have influenced the precision of the observed incidence rates.
Conclusions
This study provides the first comprehensive population-based analysis of primary spinal cord, spinal meninges, and cauda equina tumor incidence, covering approximately 99.2% of the US population for the 2004–2007 period. These analyses contribute to a more detailed understanding of age, sex, and race/ethnicity by primary spinal tumor incidence on a national level in the United States. More importantly, the incidence rates for malignant and nonmalignant primary spinal tumors by site, histology, and sex are assessed separately and provide further insight into the descriptive epidemiology of primary spinal tumor incidence in the United States.
Acknowledgments
We thank the Central Cancer Registry staff, who collected the data used in this study. These data were provided by the central cancer registries participating in either the National Program of Cancer Registries (NPCR) and were submitted to CDC in November 2009 data submission or the Surveillance, Epidemiology, and End Results (SEER) Program in the November 2009 submission. The dataset includes data for diagnosis years 1998–2007 (excluding SEER-Metro Registry data).
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
FUNDING SOURCES
No specific funding was disclosed.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
REFERENCES
- 1.Central Brain Tumor Registry of the United States. Hinsdale, IL: CBTRUS; 2005. CBTRUS Statistical Report: Primary Brain Tumors in the United States, 1998–2002. [Google Scholar]
- 2.Chi J, Khang SK. Central nervous system tumors among Koreans—a statistical study on 697 cases. J Korean Med Sci. 1989;4:77–90. doi: 10.3346/jkms.1989.4.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elia-Pasquet S, Provost D, Jaffre A, et al. Incidence of central nervous system tumors in Gironde, France. Neuroepidemiology. 2004;23:110–117. doi: 10.1159/000075953. [DOI] [PubMed] [Google Scholar]
- 4.Engelhard H, Villano J, Porter K, et al. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. J Neurosurg Spine. 2010;13:67–77. doi: 10.3171/2010.3.SPINE09430. [DOI] [PubMed] [Google Scholar]
- 5.Liigant A, Asser T, Kulla A, Kaasik AE. Epidemiology of primary central nervous system tumors in Estonia. Neuroepidemiology. 2000;19:300–311. doi: 10.1159/000026269. [DOI] [PubMed] [Google Scholar]
- 6.Schellinger KA, Propp JM, Villano JL, McCarthy BJ. Descriptive epidemiology of primary spinal cord tumors. J Neurooncol. 2008;87:173–179. doi: 10.1007/s11060-007-9507-z. [DOI] [PubMed] [Google Scholar]
- 7.Davis FG, McCarthy BJ, Berger MS. Centralized databases available for describing primary brain tumor incidence, survival, and treatment: Central Brain Tumor Registry of the United States (CBTRUS); Surveillance, Epidemiology, and End Results (SEER); and National Cancer Data Base (NCDB) Neuro Oncol. 1999;1:205–211. doi: 10.1093/neuonc/1.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC), Division of Cancer Prevention and Control (DCPC), Cancer Surveillance Branch (CSB), National Program of Cancer Registries (NPCR) About the Program. [Accessed January 14, 2011]; Available at: http://www.cdc.gov/cancer/npcr/about.htm.
- 9.Central Brain Tumor Registry of the United States. Hinsdale, IL: CBTRUS; 2009. 2009–2010 CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in Eighteen States in 2002–2006. [Google Scholar]
- 10.Senate and House of Representatives of the United States. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention; 2002. Public Law 107–260. Benign Brain Tumor Cancer Registries Amendment Act. Diseases. Health and Health Care. [Google Scholar]
- 11.Centers for Disease Control and Prevention, Division of Cancer Prevention and Control, Cancer Surveillance Branch, National Program of Cancer Registries. United States Cancer Statistics Publication Standards. [Accessed January 14, 2011]; Available at: ( http://www.cdc.gov/cancer/npcr/uscs/2005/technical_notes/criteria.htm.
- 12.2nd ed. Geneva, Switzerland: World Health Organization; 1990. International Classification of Diseases for Oncology. [Google Scholar]
- 13.3rd ed. Geneva, Switzerland: World Health Organization; 2000. International Classification of Diseases for oncology. [Google Scholar]
- 14.Central Brain Tumor Registry of the United States. Hinsdale, IL: CBTRUS; 2011. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2004–2007. [Google Scholar]
- 15.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK. 4th ed. Lyon, France: IARC Press; 2007. World Health Organization Classification of Tumours of the Central Nervous System. [Google Scholar]
- 16.Surveillance Research Program. National Cancer Institute SEER*- Stat software, version 6.6.2. Available at: www.seer.cancer.gov/seerstat.
- 17.Johannesen TB, Angell-Andersen E, Tretli S, Langmark F, Lote K. Trends in incidence of brain and central nervous system tumors in Norway, 1970–1999. Neuroepidemiology. 2004;23:101–109. doi: 10.1159/000075952. [DOI] [PubMed] [Google Scholar]
- 18.Materljan E, Materljan B, Sepcic J, Tuskan-Mohar L, Zamolo G, Erman-Baldini I. Epidemiology of central nervous system tumors in Labin area, Croatia, 1974–2001. Croat Med J. 2004;45:206–212. [PubMed] [Google Scholar]
- 19.Preston-Martin S. Descriptive epidemiology of primary tumors of the spinal cord and spinal meninges in Los Angeles County, 1972–1985. Neuroepidemiology. 1990;9:106–111. doi: 10.1159/000110757. [DOI] [PubMed] [Google Scholar]
- 20.Kurland LT. The frequency of intracranial and intraspinal neoplasms in the resident population of Rochester, Minnesota. J Neurosurg. 1958;15:627–641. doi: 10.3171/jns.1958.15.6.0627. [DOI] [PubMed] [Google Scholar]
- 21.Davis FG, Kupelian V, Freels S, McCarthy B, Surawicz T. Prevalence estimates for primary brain tumors in the United States by behavior and major histology groups. Neuro Oncol. 2001;3:152–158. doi: 10.1093/neuonc/3.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]