Abstract
Background
Malocclusion, body posture, and breathing pattern may be correlated, but this issue is still controversial. The aim of the study was to examine the relationship between the type of malocclusion, body posture, and nasopharyngeal obstruction in children aged 7–14 years.
Material/Methods
The study group comprised 94 patients aged 7–14 years (mean±SD: 11.9±2.1 years); 44 (46.8%) males and 50 (53.2%) females. All patients passed an examination performed by the same orthodontist (study model and cephalometric radiograph analysis), orthopedic surgeon (body posture examined from the front, side, and back), and otorhinolaryngologist (anterior and posterior rhinoscopy and pharyngoscopy) in a blind manner.
Results
Postural disorders were observed in 72 (76.6%) patients. Hypertrophy of the adenoids was diagnosed in 54 (57.4%) patients, hypertrophy of the tonsils in 85 (90.3%), nasal septum deviation in 51 (54.3%), and allergic rhinitis in 19 (20.2%) patients. There was a statistically significant correlation between presence of kyphotic posture and a reduction in the SNB angle, representing sagittal position of the mandible. Also, there was a statistically significant association between kyphotic posture and nasopharyngeal obstruction (54.1% of patients with nasopharyngeal obstruction were kyphotic, compared with 25% of patients with no nasopharyngeal obstruction; p=0.02). Kyphotic posture and reduced SNB angle were more common among males.
Conclusions
We concluded that: 1) there was a significant association between the sagittal position of the mandible (SNB angle) and a kyphotic posture; 2) kyphotic posture was significantly more common among patients with nasopharyngeal obstruction.
Keywords: Malocclusion, Nasopharyngeal Diseases, Posture
Background
The stomatognathic system, an integral component of the upper body, may play an important role in postural control. Thus, changes in body posture may affect craniofacial development. Several studies suggest that spatial relationships between the jaws may influence the distal musculature and induce body postural adaptations [1,2]. However, Perinetti et al. concluded that mandibular position, asymmetric occlusion, and temporomandibular disorders do not appear to correlate with body sway or muscle activity in other parts of the body, including those responsible for maintaining posture, at a clinically relevant level [3,4].
Several studies have examined the relationship between malocclusion and parameters of body posture in the sagittal and frontal planes; the results identified a correlation between structural orthopaedic diseases and occlusal morphology [6,5]. Segatto et al. found that children with various spinal deformities have a high number of malocclusions [7], and Ben-Bassat et al. found that patients with idiopathic scoliosis showed more asymmetric features characteristic of malocclusion than a random control group [8]. Also, children with congenital hip dislocation are more predisposed to the development of a lateral cross-bite [9]. However, the results from studies looking at the correlation between poor body posture and dental occlusion are conflicting. For example, Lippold et al. examined 59 pre-school children and found statistically significant correlations between weak body posture and Class II malocclusion [6]. Also, Lippold et al. used rasterstereography to examine the sagittal profile of the spine in 53 adults with skeletal Class II and Class III malocclusions, and found a correlation between the vertical and sagittal position of the lower jaw and thoracic, lordotic, and pelvic inclination [10], and between the vertical and sagittal position of the lower jaw and pelvic rotation [11]. Thus, 2 different models of back shape were devised based on of the results on these studies: 1) a more distal and vertical craniofacial pattern is associated with an increase in the upper thoracic, lumbar-lordotic, and pelvic angles; and 2) a more mesial and horizontal craniofacial pattern is associated with smaller upper thoracic, lumbar-lordotic, and pelvic angles. Sinko et al. compared body posture in 29 Class II and Class III patients, and found that the apex of the thoracic kyphosis was more cranial in Class III patients than in Class II patients or healthy controls [12]. However, these studies are based on small samples. When Perillo et al. examined 703 children, they found no association between body posture and clinically assessed dental occlusion [13]. Silvestrini-Biavati et al. investigated association between malocclusion, poor posture, and ocular convergence disorders. They observed that about 14% of all patients had a pathological gait; among them, children demonstrated a higher prevalence of vertical occlusion anomalies [14]. Contradictory results of studies can arise because there was a large diversity among the studies with regard to the protocols used; some studies assessed body posture by physical examination while other studies used body photographs and rasterstereography.
There is also a correlation between body posture and breathing pattern. Enlarged tonsils and adenoids, allergic rhinitis, and chronic respiratory problems cause a mouth breathing syndrome, resulting in adaptive head and body postures [15], which also affects the development of the facial skeleton. It is generally accepted that anterior tilting of the head is the main postural change in such subjects, who push their heads forward and extend their neck to facilitate air flow through the mouth. An altered neck posture was observed in 80.0% of mouth-breathing children [15]. The forward position of the head causes protraction and rotation of the shoulders, elevation and abduction of the scapulae, depression of the thoracic anterior region, and forward displacement of the whole body. Unlike in nasal-breathing children, these postural changes in mouth-breathing children do not improve spontaneously once they are older (>8 years-of-age) [16]. Milanesi et al. demonstrated that adults who were mouth-breathers during childhood had a more anterior head posture and a larger lumbar lordosis angle than individuals in a control group [17].
To date, no study has examined the association between malocclusion, body posture, and breathing pattern. The assessment of correlations between orthopedic, otorhinolaryngologic, and orthodontic findings derived from interdisciplinary studies appears to be of practical importance in diagnosis and prevention. Therefore, the aim of the present study was to examine the relationship between the type of malocclusion, body posture, and nasopharyngeal obstruction in children aged 7–14 years. The tested null hypotheses were that: 1) sagittal craniofacial skeletal morphology depends on the nasopharyngeal obstruction and body posture, and 2) vertical craniofacial skeletal morphology depends on the nasopharyngeal obstruction and body posture.
Material and Methods
The study sample was obtained from consecutive patients attending for orthodontic treatment at the Department of Orthodontics who agreed to participate in the study from September 2013 through May 2014. A full explanation of the study aims and procedures was provided to the parents of each patient and signed consent forms were obtained. The study was approved by the Regional Biomedical Research Ethics Committee (no. BE-2-48).
The study group comprised 94 patients aged 7–14 years (mean ±SD: 11.9±2.1 years). Forty-four were male (46.8%) and 50 were female (53.2%). All patients passed an examination performed by the same clinical team in a blinded manner. Power analysis was used to determine the sample size. Performing a power calculation, we anticipated changes in SNB angle by 2° (SD=2), α=0.05. In such circumstances, this study aimed to investigate 90 patients (n1=45, n2=45) to achieve 0.99 power. After investigation we concluded the study needed a power 0.802 (n1=49, n2=45; α=0.05; change in SNB angle 2.21) (SD=3.77).
The inclusion criteria into the study were as follows: age 7–14 years; no history of maxillofacial trauma or surgery, syndromes, clefts, or orthodontic treatment; no previous treatment for orthopedic disorders; and no previous injury to the pelvis, spine, or long bones.
Orthodontic examination
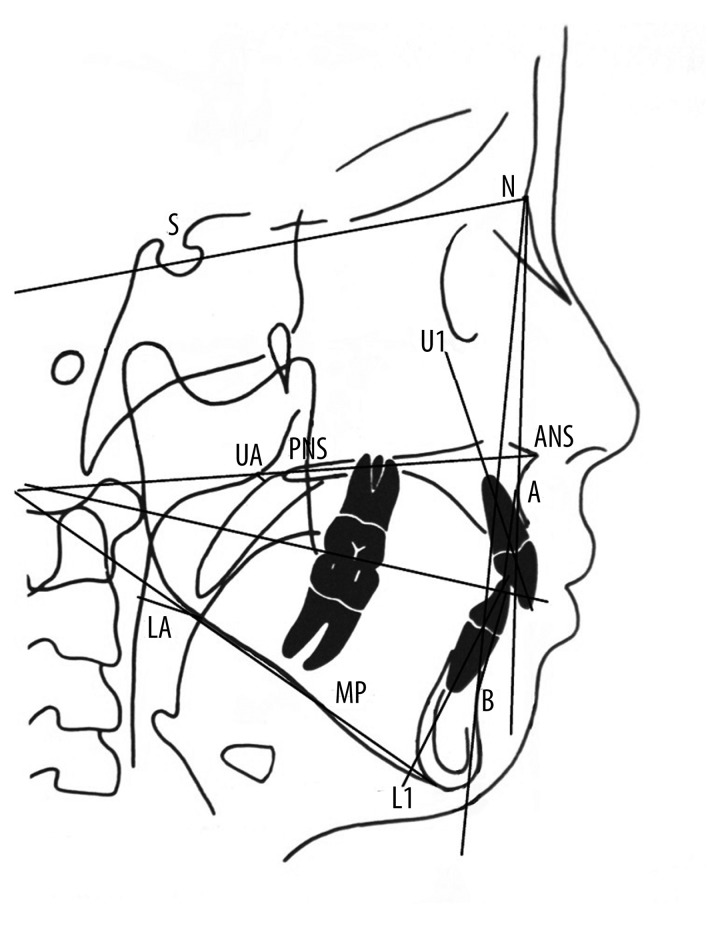
The orthodontic examination consisted of the study model and cephalometric radiograph analysis. The study model examination consisted of a transverse examination in which a posterior cross-bite was confirmed (at least 2 teeth showed a cross-relationship with the opposite teeth in the posterior segments of the dental arches. The cross-bite was categorized as unilateral or bilateral, and we performed a space analysis in which the difference between the available space and the necessary space in the dental arch was calculated. Crowding was categorized as mild (lack of space: 2–4 mm), moderate (5–9 mm), or severe (>9 mm). A standardized lateral cephalometric radiograph was taken for each patient (Kodak 8000C; enlargement factor 1.15; exposure: 12 mAs, 76–80 kV) and analyzed using Dolphin software (version 10.5). The sagittal position of the maxilla (SNA) and the mandible (SNB), the sagittal jaw relationship (ANB), the mandibular plane angle (MP-SN), and the inclination of the maxillary incisors and mandibular incisors (U1-ANS/PNS and L1-MP, respectively) were used to analyze the facial skull parameters. All measurements are shown in Figure 1.
Figure 1.
References and points used for this study. The sagittal position of the maxilla (SNA) and the mandible (SNB), the sagittal jaw relationship (ANB), the mandibular plane angle (MP-SN), the inclination of the maxillary incisors and mandibular incisors (U1-ANS/PNS and L1-MP).
The error margins for the study models and lateral cephalometric analysis were determined by repeatedly measuring the 6 variables on 10 randomly selected models and radiographs at 2-week intervals. Measurements were made by the same operator (MS). Parametric data were subjected to a paired-samples t-test and non-parametric Wilcoxon signed ranks test, which showed that there was no significant difference between the data sets.
Orthopedic examination
The examination was performed in a quiet classroom without external interference. The patient was examined in a relaxed standing posture: subjects were asked to stand in an upright position, barefoot, without moving, looking straight ahead, with relaxed shoulders and arms resting at their sides for a natural head and body position. A standard routine examination from the front, side, and back was performed for each patient. Degrees of severity cannot be differentiated with adequate precision by manual orthopedic diagnostics; therefore, the findings were graded either as normal or abnormal. Patients were first examined from the side and the thoracic kyphosis was evaluated. If an increased, but adjustable, asymptomatic curvature of the thoracic spine was observed, the posture was classed as kyphotic. All patients underwent tests to rule out Scheuermann’s disease and ankylosing spondylitis; briefly, each patient was asked to stand upright and pull back the shoulders to induce thoracic extension. In cases of postural kyphosis, an increased curvature, which is regular and mobile, was found. Next, patients were examined from the front, and the position of shoulders, the symmetry of the waist triangles, and the horizontal alignment of the upper iliac crests were noted. Finally, patients were examined from the back, and the position of the shoulders, the scapular height, and the symmetry of the waist triangles, iliac crests, and thoracic rib hump were noted. Differences between the left and right sides were interpreted as asymmetry. All the patients underwent testing to rule out scoliosis. Briefly, patients were asked to bring their chin to their chest, relax the hands, and flex the hips with the knees extended. The examiner then looked for the emergence of a paravertebral muscle roller in the lumbar region or a rib hump in the thoracic region. If a rib prominence hump was present (>1 cm), then full-length frontal and lateral spinal radiographs were obtained to evaluate the degree of spinal deformation (by measuring the Cobb’s angle) (Figure 2).
Figure 2.
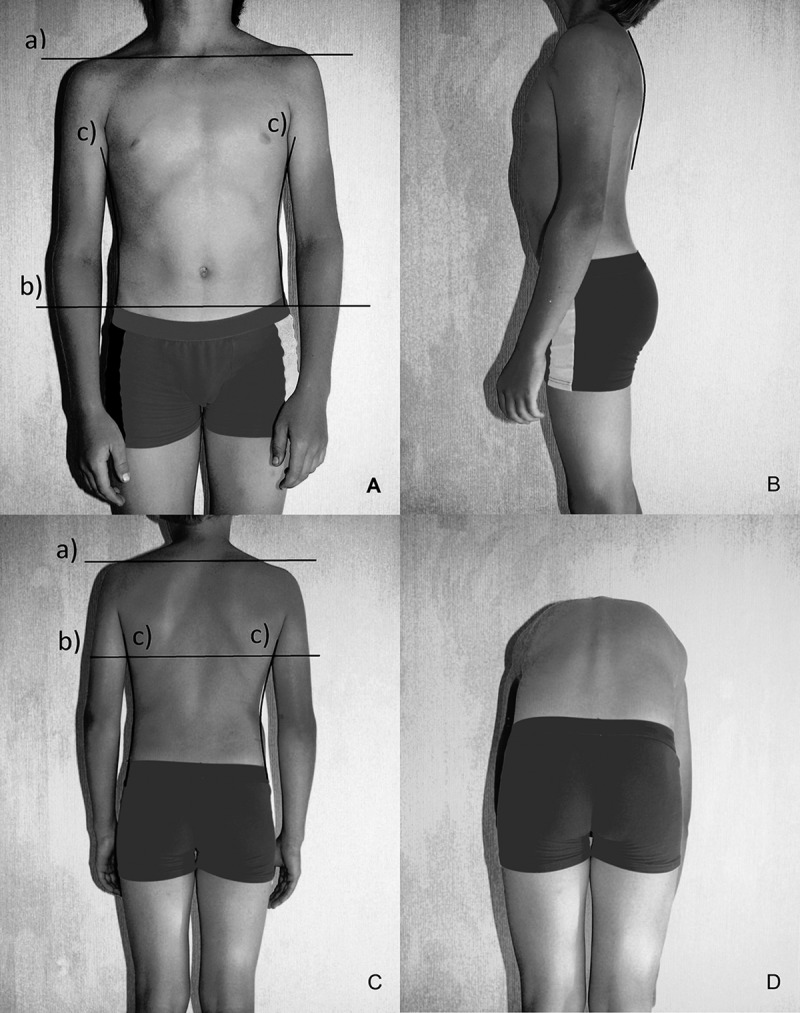
Orthopedic examination: (A) Evaluation from the front: a) symmetry of the shoulders; b) symmetry of the waist triangles; c) horizontality of frontal upper iliac crests. (B) Thoracic kyphosis has to be evaluated from the side. (C) Evaluation from the back: a) symmetry of the shoulders; b) the scapular height; c) symmetry of the waist triangles. (D) Test to confirm or rule out scoliosis. It has to be observed if the paravertebral muscle roller emerges in the lumbar region and the rib hump in the thoracic region.
Otorhinolaryngological examination
Anterior and posterior rhinoscopy and pharyngoscopy were performed to assess nasal and pharyngeal status. The following diagnoses were made based on the findings: hypertrophy of the adenoids (Grade 2–3) was diagnosed when up to 2/3 of the choana was compromised; hypertrophy of the palatal tonsils (Grade 2–4) was diagnosed when there was <50% of normal space between tonsillar pillars; nasal septum deviation was diagnosed when the nasal septum was severely shifted away from the midline; and allergic rhinitis was diagnosed when the patient showed typical allergy symptoms (nasal congestion, runny nose, sneezing, and watery eyes) and skin-prick test results were positive. Nasopharyngeal obstruction was determined when hypertrophy of the adenoids (2nd degree or higher) and/or hypertrophy of the tonsils (2nd degree or higher), and/or nasal septum deviation and/or allergic rhinitis was diagnosed for the patient.
The orthopedic and otorhinolaryngological examination was performed by expert investigators (EC and RP). To assess the method error of clinical investigation, prior to the survey, the investigators calibrated and standardized their procedures by repeating examinations of 10 patients at 2 different times (measuring agreement was calculated by kappa; kappa values were >0.8).
Statistical analysis
All statistical analyses were performed using the statistical software package SPSS 20.0 for Windows. To compare the mean values, the Student’s t test was used if the distribution of data was normal. In case of non-normal data, the Mann-Whitney U test was used. Hypotheses of interrelations between characteristics were verified using the χ2 criterion method and Spearman correlation coefficients (r). The most specific predictors of the decrease in the SNB angle were assessed using logistic regression analysis and receiver operating characteristic (ROC) curve analysis. A p-value of <0.05 was considered statistically significant.
Results
The orthodontic, orthopedic, and otorhinolaryngological characteristics of the patients are described in Table 1.
Table 1.
The orthodontic, orthopedic, and otorhinolaryngological characteristics of the study group.
| Characteristic | Patients n (%) | |
|---|---|---|
| Orthodontic characteristics: | ||
| Skeletal sagittal relationship | Class I (ANB angle 1–3°) | 26 (27.7%) |
| Class II (ANB angle ≥4°) | 60 (63.8%) | |
| Class III (ANB angle ≤0°) | 8 (8.5%) | |
| Postural characteristics | ||
| Kyphotic posture | 45 (47.9%) | |
| Asymmetry of shoulder line | 23 (24.5%) | |
| Asymmetry of position of scapulae | 23 (24.5%) | |
| Asymmetry of waist triangles | 5 (5.3%) | |
| Rib hump | 48 (51.1%) | |
| Otorhinolaryngological characteristics | ||
| Hypertrophy of adenoids | Grade 1 | 24 (25.5%) |
| Grade 2 | 30 (31.9%) | |
| Hypertrophy of tonsils | Grade 1 | 46 (48.9%) |
| Grade 2 | 32 (34%) | |
| Grade 3 | 7 (7.4%) | |
| Nasal septum deviation | 51 (54.3%) | |
| Allergic rhinitis | 19 (20.2%) |
Postural disorders were observed in 72 (76.6%) patients. Structural orthopedic anomaly (scoliosis) was observed in 1 patient. Kyphotic posture was more common among males (26; 59.1%) than females (19; 38%) (p=0.01). There was no statistically significant association between sex and the occurrence of transverse orthopedic pathology. The relationships between malocclusion, sex, and sagittal orthopaedic pathology are presented in Table 2.
Table 2.
The relationship between orthodontic variables, sex, and sagittal orthopaedic parameters (thoracic kyphosis).
| Orthodontic variables | Female | p | Male | p | Total | p | |||
|---|---|---|---|---|---|---|---|---|---|
| n=50 | n=44 | n=94 | |||||||
| Thoracic kyphosis | Thoracic kyphosis | Thoracic kyphosis | |||||||
| Normal | Kyphotic posture | Normal | Kyphotic posture | Normal | Kyphotic posture | ||||
| n=31 | n=19 | n=18 | n=26 | n=49 | n=45 | ||||
| Mean, SD | Mean, SD | Mean, SD | Mean, SD | Mean, SD | Mean, SD | ||||
| Sagittal position of the maxilla (SNA°) | 82.03±3.61 | 81.28±3.08 | 0.46 | 82.50±3.47 | 80.88±2.9 | 0.1 | 82.2±3.53 | 81.05±2.95 | 0.91 |
| Sagittal position of the mandible (SNB°) | 78.58±3.78 | 77.21±2.76 | 0.17 | 79.00±3.99 | 76.02±3.74 | 0.02* | 78.73±3.08 | 76.52±3.38 | 0.01* |
| Sagittal jaw relationship (ANB°) | 3.35±2.8 | 3.97±1.58 | 0.39 | 3.60±2.78 | 4.75±3.35 | 0.24 | 3.44±2.76 | 4.42±2.75 | 0.23 |
| Mandibular plane angle (MP-SN°) | 32.59±5.02 | 35.00±4.47 | 0.92 | 31.90±6.60 | 33.12±6.27 | 0.54 | 32.34±5.59 | 33.91±5.60 | 0.18 |
| Inclination of maxillary incisors (U1-ANS/PNS) | 107.74±8.41 | 106.89±7.62 | 0.72 | 107.33±10.8 | 106.94±9.44 | 0.9 | 107.59±9.29 | 106.92±8.62 | 0.72 |
| Inclination of mandibular incisors (L1-MP°) | 91.71±9.22 | 93.63±6.79 | 0.44 | 92.36±8.2 | 93.40±6.44 | 0.64 | 91.95±8.78 | 93.50±6.51 | 0.34 |
| Overjet (mm) | 3.37±2.64 | 3.86±1.2 | 0.42 | 3.39±3.27 | 5.15±3.34 | 0.09 | 3.38±2.85 | 4.62±2.71 | 0.03* |
| Overbite (mm) | 3.78±2.39 | 4.05±2.04 | 0.67 | 3.50±2.35 | 5.19±2.15 | 0.02* | 3.68±2.36 | 4.71±2.16 | 0.03* |
There was a statistically significant correlation between presence of kyphotic posture and a reduction in the SNB angle (statistically significant in males but not significant in females).
Table 3 shows the relationship between orthodontic anomalies, sex, and nasopharyngeal obstruction.
Table 3.
The relationship between orthodontic variables, sex, and nasopharyngeal obstruction.
| Orthodontic variables | Female | p | Male | p | Total | p | |||
|---|---|---|---|---|---|---|---|---|---|
| n=50 | n=44 | n=94 | |||||||
| Nasopharyngeal obstruction | Nasopharyngeal obstruction | Nasopharyngeal obstruction | |||||||
| Absent | Present | Absent | Present | Absent | Present | ||||
| n=12 | n=38 | n=8 | n=36 | n=20 | n=74 | ||||
| Mean, SD | Mean, SD | Mean, SD | Mean, SD | Mean, SD | Mean, SD | ||||
| Sagittal position of the maxilla (SNA°) | 81.92±3.55 | 81.69±3.40 | 0.85 | 82.25±5.01 | 81.39±2.74 | 0.5 | 82.05±4.07 | 81.55±3.08 | 0.56 |
| Sagittal position of the mandible (SNB°) | 79.08±3.80 | 77.74±3.34 | 0.25 | 78.13±4.26 | 77.04±4.07 | 0.5 | 78.70±3.91 | 77.40±3.71 | 0.17 |
| Sagittal jaw relationship (ANB°) | 2.74±3.30 | 3.85±2.04 | 0.17 | 4.13±1.64 | 4.32±3.41 | 0.88 | 3.30±2.79 | 4.08±2.78 | 0.48 |
| Mandibular plane angle (MP-SN°) | 32.17±3.33 | 33.93±5.27 | 0.28 | 30.85±6.65 | 33.01±6.32 | 0.39 | 31.64±4.81 | 33.48±5.79 | 0.2 |
| Inclination of maxillary incisors (U1- ANS/PNS) | 107.83±9.07 | 107.29±7.83 | 0.84 | 103.38±12.55 | 107.93±9.26 | 0.25 | 106.05±10.52 | 107.60±8.50 | 0.49 |
| Inclination of mandibular incisors (L1-MP°) | 92.67±10.54 | 92.37±7.71 | 0.92 | 93.88±5.67 | 92.78±7.48 | 0.7 | 93.15±8.75 | 92.57±7.55 | 0.77 |
| Overjet (mm) | 3.08±2.58 | 3.72±2.09 | 0.39 | 4.31±2.75 | 4.46±3.55 | 0.91 | 3.58±2.65 | 4.08±2.90 | 0.48 |
| Overbite (mm) | 3.21±1.83 | 4.10±2.35 | 0.24 | 4.19±2.20 | 4.57±2.42 | 0.68 | 3.60±1.99 | 4.33±2.38 | 0.21 |
There was no significant association between the presence of transverse orthopedic pathology and orthodontic or otorhinolaryngologic pathology. Also, there was no relationship between crowding, posterior cross-bite, and orthopedic or otorhinolaryngologic parameters.
The findings evaluating the relationship between nasopharyngeal obstruction and sagittal orthopedic pathology indicated that kyphotic posture was significantly more common among patients with nasopharyngeal obstruction – 54.1% patients with nasopharyngeal obstruction were kyphotic, compared with 25% patients with no nasopharyngeal obstruction (Spearman’s correlation coefficient=0.24; p=0.02).
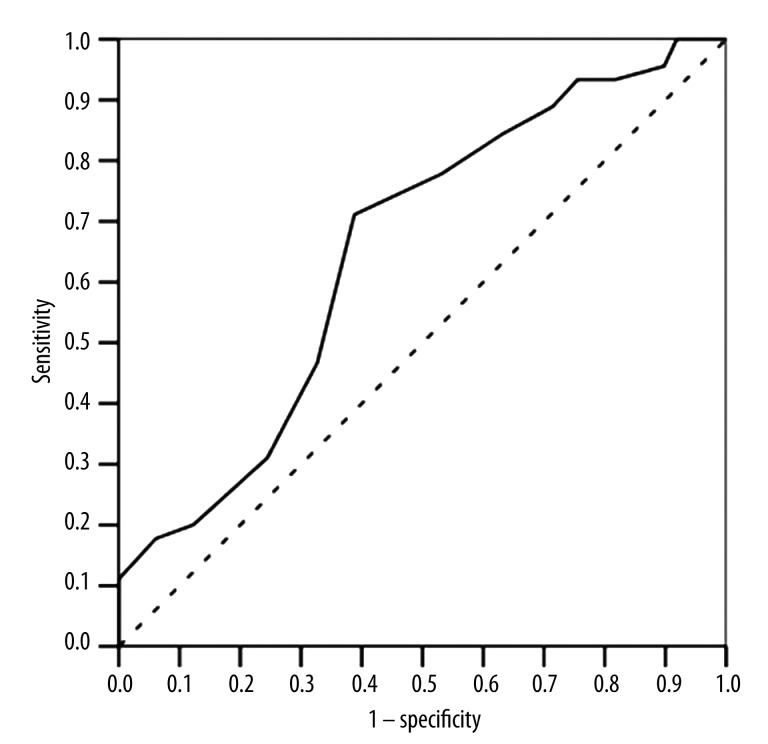
Because we identified a significant decrease in the SNB angle in patients with kyphotic posture and nasopharyngeal obstruction, we performed logistic regression analysis to evaluate the risk of a decrease in the SNB angle. The critical value of the SNB angle was determined using ROC curve analysis (Figure 3). The threshold of 77° was crucial for the SNB angle (sensitivity 71.1%; specificity, 69.8%; p=0,002). We found that among patients with SNB angle <77°, kyphotic posture was found in 71.1% of patients and normal thoracic kyphosis was found in 38.8%.
Figure 3.
Receiver operating characteristic (ROC) curve analysis for prediction of the critical values of the SNB angle. Area under the receiver operating characteristic curve=65.2%.
Therefore, we performed binary logistic regression analysis, which revealed that kyphotic posture increases odds ratio of the SNB<77° angle by 3.887 (95% CI; 1.639–9.218). This calculation adjusted with nasopharyngeal obstruction indicated odds ratio of the SNB<77° angle by 4.037 (95% CI; 1.652–9.861).
Discussion
Malocclusion has a multifactorial etiology; several of these factors, including oral habits and breathing mode, play an important role in pathogenesis. Changes in body posture may also influence craniofacial development. An improved understanding of the mechanism underlying normal craniofacial development is needed for the accurate diagnosis and appropriate treatment of malocclusion. The present study was based on the hypothesis that body posture, breathing pattern, and the type of malocclusion are inter-dependent.
The study group comprised consecutive orthodontic patients aged 7–14 years (the age during which transition from primary to permanent dentition occurs). This age range of patients was also selected on the basis of growth peculiarities. A healthy child assumes a normal spinal curvature at around 7 years of age. The rate of spinal growth is not constant – there is a period of accelerated growth between 10.5 and 15.5 years of age, and peak height velocity occurs at an average of 12.2 years in girls and 13.9 years in boys [18]. During this period, any postural defects may be either spontaneously corrected or become worse [19]. We detected a high prevalence of orthopedic anomalies in the study group, the most common being kyphotic posture (47.9%) and a thoracic rib hump (51.1%). This is in agreement with the findings of other studies. For example, Lippold et al. reported orthopedic pathological findings in 52% of pre-school children [6], and Hagner et al. identified poor body posture in 65.71% of 10-year-old and 54.29% of 13-year-old non-orthodontic children [19]. Nasopharyngeal pathology also was a common finding in the present study. According to the literature, hypertrophy of the adenoids and tonsils, which causes mouth breathing, is common in children (varying from 40% to 60%) [20]. The present study identified hypertrophy of the adenoids in 57.4% and of the tonsils in 90.3% of subjects; these high levels may be due to the selection of the specific group of patients.
Overall, the results showed that sagittal body posture was related to sagittal craniofacial parameters. Patients with a kyphotic posture had an increased overjet and lower SNB angle. This was significant in males, but was only a tendency in females. Such a difference could occur because kyphotic posture was more common among males (59.1%) than females (38%) (p=0.01). This is in agreement with the results of Lippold et al., who identified correlations between the sagittal position of the lower jaw and thoracic inclination [10]. Lippold et al. also reported that the position of the maxilla does not correlate with spinal curvature [10,11], which also agrees with our results. However, we found no relationship of the vertical position of the lower jaw and thoracic inclination, which is in contrast to the results of Lippold et al. [10]. The results of our study show that the facial angle (MP-SN) tended to be increased in patients with a kyphotic posture; however, this difference was not significant. Silvestrini-Biavati et al. reported that about 13% of children 8.5±2.3 years old showed a pathological gait, and among them there was a higher prevalence of patients with a deep bite and open bite. The authors also suggested that vertical malocclusions are correlated to the dominant eye [14]. In our study we found that dental overjet and overbite were statistically significantly greater in patients with a kyphotic posture; however, skeletal vertical parameters (angle MP-SN) did not differ in groups with normal or kyphotic posture.
According to our results, craniofacial parameters were not associated with nasopharyngeal pathology. Previous studies showed that nasopharyngeal pathology causes changes in the growth of the mandible (which rotates downward and backward), and an increase in the height of the lower face [21,22]. We also found that a kyphotic posture was statistically significantly more common among patients with nasopharyngeal pathology; however, Neiva et al. did not find an increase in thoracic kyphosis in mouth-breathing subjects [23].
When we evaluated body posture in the transverse plane, we identified any association between asymmetric posture and orthodontic parameters. The malocclusion most likely to be related to asymmetric orthopaedic anomalies should be a posterior cross-bite. Korbmacher et al. examined 55 children referred to an orthopedic center and found that those with a unilateral cross-bite were more likely to have an oblique shoulder, oblique pelvis, functional leg length differences, and scoliosis than children with dental symmetry [24]. Mouth breathing is also associated with narrowing of the upper dental arch and a posterior cross-bite. However, we did not find any relationship between body posture, nasopharyngeal pathology, and a posterior cross-bite. Michelotti et al. also failed to demonstrate a significant association between a posterior cross-bite and postural stability or transverse orthopedic pathology [25]. Here, we found no relationship between crowding of the dental arches and body posture or nasopharyngeal pathology. This is in contrast to the findings of Pachi et al. and Solow and Sonnesen, who reported that crowding was associated with craniocervical posture [26,27]. The discrepancy between the results reported herein and those of others can be explained, at least in part, by differences in study design (e.g., type of orthopedic evaluation), specific patient groups (e.g., orthodontic/non-orthodontic patients), different age groups, and different sample sizes.
In summary, the results of the present study suggest that there is a significant association between a decrease in the SNB angle, kyphotic posture, and nasopharyngeal pathology. The presence of kyphotic posture, especially together with a nasopharyngeal obstruction, increases the possibility of the mandibular retrusion. The null hypotheses were tested: 1) sagittal craniofacial skeletal morphology depended on the nasopharyngeal obstruction and body posture; and 2) vertical craniofacial skeletal morphology did not depend on the nasopharyngeal obstruction and body posture. However, the question of causality remains. Which of these morphologic changes are primary and which are consequential? To answer this question, we looked at a few studies that evaluated changes in body posture after the correction of malocclusion. Lippold et al. conducted a randomized clinical trial in a juvenile population with a unilateral posterior cross-bite and found that early orthodontic treatment had no effect on postural parameters [28]. Sinko et al. found that there was no significant difference between body posture before orthognathic surgery and at 1 year after surgery [12]. Tecco et al. suggest that improvements in nasopharyngeal airway adequacy after rapid maxillary expansion were only mildly associated with changes in the craniocervical angle and tipping of the head [29], and a review by Michelotti et al. concluded that even if there is an association between occlusal factors and postural alterations, there is not enough scientific evidence to support a cause-effect relationship [30]. Therefore, although it is reasonable to suppose that the stomatognathic system can affect cervical region function, its overall relevance to body posture is still unclear. This lack of scientific evidence in the literature of a cause-effect relationship between occlusion, nasopharyngeal pathology, and postural disorders makes this question difficult to answer. Further studies with correct methods are needed to clarify these cause-effect relationships.
Conclusions
The present study has 2 main findings: 1) there was a significant association between the sagittal position of the mandible (SNB angle) and a kyphotic posture; and 2) based on study results, kyphotic posture was significantly more common among patients with nasopharyngeal obstruction.
Footnotes
Source of support: Departmental sources
References
- 1.Bracco P, Deregibus A, Piscetta R. Effects of different jaw relations on postural stability in human subjects. Neurosci Lett. 2004;356:228–30. doi: 10.1016/j.neulet.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 2.Tardieu C, Dumitrescu M, Giraudeau A, et al. Dental occlusion and postural control in adults. Neurosci Lett. 2009;450:221–24. doi: 10.1016/j.neulet.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Perinetti G, Primožič J, Manfredini D, et al. The diagnostic potential of static body-sway recording in orthodontics: a systematic review. Eur J Orthod. 2013;35:696–705. doi: 10.1093/ejo/cjs085. [DOI] [PubMed] [Google Scholar]
- 4.Perinetti G, Turp JC, Primožič J, et al. Associations between the masticatory system and muscle activity of other body districts. A meta-analysis of surface electromyography studies. J Electromyogr Kinesiol. 2011;21:877–84. doi: 10.1016/j.jelekin.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Ikemitsu H, Zeze R, Yuasa K, Izumi K. The relationship between jaw deformity and scoliosis. Journal Oral Radiology. 2006;22:14–17. [Google Scholar]
- 6.Lippold C, van den Bos L, Hohoff A, et al. Interdisciplinary study of orthopedic and orthodontic findings in pre-school infants. J Orofac Orthop. 2003;64:330–40. doi: 10.1007/s00056-003-0236-4. [DOI] [PubMed] [Google Scholar]
- 7.Segatto E, Lippold C, Végh A. Craniofacial features of children with spinal deformities. BMC Musculoskelet Disorders. 2008;9:169–79. doi: 10.1186/1471-2474-9-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ben-Bassat Y, Yitschaky M, Kaplan L, Brin I. Occlusal patterns in patients with Idiopathic scoliosis. Am J Orthod Dentofacial Orthop. 2006;130:629–33. doi: 10.1016/j.ajodo.2005.01.032. [DOI] [PubMed] [Google Scholar]
- 9.Harila V, Valkama M, Sato K, Tolleson S. Occlusal asymmetries in children with congenital hip dislocation. Eur J Orthod. 2012;34:307–11. doi: 10.1093/ejo/cjr004. [DOI] [PubMed] [Google Scholar]
- 10.Lippold C, Danesha G, Schilgen M, et al. Relationship between thoracic, lordotic, and pelvic inclination and craniofacial morphology in adults. Angle Orthodontist. 2006;76:779–85. doi: 10.1043/0003-3219(2006)076[0779:RBTLAP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Lippold C, Danesha G, Hoppe G, et al. Trunk inclination, pelvic tilt and pelvic rotation in relation to the craniofacial morphology in adults. Angle Orthodontist. 2007;77:29–35. doi: 10.2319/121205-434R.1. [DOI] [PubMed] [Google Scholar]
- 12.Sinko K, Grohs JG, Millesi-Schobel G, et al. Dysgnathia, orthognathic surgery and spinal posture. Int J Oral Maxillofac Surg. 2006;35(4):312–17. doi: 10.1016/j.ijom.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Perillo L, Signoriello G, Ferro F, et al. Dental occlusion and body posture in growing subjects. A population-based study in 12-year-old Italian adolescents. International Dentistry SA. 2008;10:46–52. [Google Scholar]
- 14.Silvestrini-Biavati A, Migliorati M, Demarziani E, et al. Clinical association between teeth malocclusions, wrong posture and ocular convergence disorders: an epidemiological investigation on primary school children. BMC Pediatrics. 2013;13:12. doi: 10.1186/1471-2431-13-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okuro RT, Morcillo AM, Sakano E, et al. Exercise capacity, respiratory mechanics and posture in mouth breathers. Braz J Otorhinolaryngol. 2011;77:656–62. doi: 10.1590/S1808-86942011000500020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krakauer LH, Guilherme A. Relationship between mouth breathing and postural alterations of children: a descriptive analysis. Int J Orofacial Myology. 2000;26:13–23. [PubMed] [Google Scholar]
- 17.Milanesi JM, Borin G, Correa ECR, et al. Impact of the mouth breathing occurred during childhood in the adult age: Biophotogrammetric postural analysis. Int J Pediatr Otorhinolaryngol. 2011;75:999–1004. doi: 10.1016/j.ijporl.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 18.Largo RH, Gasser T, Prader A, et al. Analysis of the adolescent growth spurt using smoothing spline functions. Ann Hum Biol. 1978;5:421–34. doi: 10.1080/03014467800003071. [DOI] [PubMed] [Google Scholar]
- 19.Hagner W, Bąk D, Hagner-Derengowska M. Changes in body posture in children between the 10th and 13th years of age. Polish Annals of Medicine. 2011;18:76–81. [Google Scholar]
- 20.Abreu RR, Rocha RL, Lamounier JA, Guerra AFM. Prevalence of mouth breathing among children. J Pediatr (Rio J) 2008;84:529–35. doi: 10.2223/JPED.1806. [DOI] [PubMed] [Google Scholar]
- 21.Cuccia AM, Lotti M, Caradonna D. Oral breathing and head posture. Angle Orthod. 2008;78:77–82. doi: 10.2319/011507-18.1. [DOI] [PubMed] [Google Scholar]
- 22.Ucar FI, Uysal T. Comparision of orofacial airway dimensions in subject with different breathing pattern. Prog Orthod. 2012;13:210–17. doi: 10.1016/j.pio.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Neiva PD, Kirkwood RN, Godinho R. Orientation and position of head posture, scapula and thoracic spine in mouth-breathing children. Int J Pediatr Otorhinolaryngol. 2009;73:227–36. doi: 10.1016/j.ijporl.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Korbmacher H, Koch L, Eggers-Stroeder G, Kahl-Nieke B. Associations between orthopaedic disturbances and unilateral crossbite in children with asymmetry of the upper cervical spine. Eur J Orthod. 2007;29:100–4. doi: 10.1093/ejo/cjl066. [DOI] [PubMed] [Google Scholar]
- 25.Michelotti A, Farella M, Buonocore G, et al. Is unilateral posterior crossbite associated with leg length inequality? Eur J Orthod. 2007;29:622–26. doi: 10.1093/ejo/cjm071. [DOI] [PubMed] [Google Scholar]
- 26.Pachi F, Turla R, Checchi AP. Head posture and lower arch dental crowding. Angle Orthod. 2009;79:873–80. doi: 10.2319/060708-595.1. [DOI] [PubMed] [Google Scholar]
- 27.Solow B, Sonnesen L. Head posture and malocclusions. Eur J Orthod. 1998;20:685–93. doi: 10.1093/ejo/20.6.685. [DOI] [PubMed] [Google Scholar]
- 28.Lippold C, Moiseenko T, Drerup B, et al. Spine deviations and orthodontic treatment of asymmetric malocclusions in children. BMC Musculoskeletal Disord. 2012;13:151–58. doi: 10.1186/1471-2474-13-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tecco S, Festa F, Tete S, et al. Changes in head posture after rapid maxillary expansion in mouth-breathing girls: a controlled study. Angle Orthod. 2005;75:171–76. doi: 10.1043/0003-3219(2005)075<0167:CIHPAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Michelotti A, Buonocore G, Manzo P, et al. Dental occlusion and posture: an overview. Prog Orthod. 2011;12:53–58. doi: 10.1016/j.pio.2010.09.010. [DOI] [PubMed] [Google Scholar]