Abstract
To improve health at the human, animal, and ecosystem interface, defined as One Health, training of researchers must transcend individual disciplines to develop a new process of collaboration. The transdisciplinary research approach integrates frameworks and methodologies beyond academic disciplines and includes involvement of and input from policy makers and members of the community. The authors argue that there should be a significant shift in academic institutions’ research capacity to achieve the added value of a transdisciplinary approach for addressing One Health problems. This Perspective is a call to action for academic institutions to provide the foundations for this salient shift. The authors begin by describing the transdisciplinary approach, propose methods for building transdisciplinary research capacity, and highlight three value propositions that support the case. Examples are provided to illustrate how the transdisciplinary approach to research adds value through improved sustainability of impact, increased cost-effectiveness, and enhanced abilities to mitigate potentially harmful unintended consequences. The authors conclude with three key recommendations for academic institutions: (1) a focus on creating enabling environments for One Health and transdisciplinary research, (2) the development of novel funding structures for transdisciplinary research, and (3) training of “transmitters” using real-world-oriented educational programs that break down research silos through collaboration across disciplines.
To improve health at the human, animal, and environment interface, defined in this Perspective as One Health, training of researchers must transcend individual disciplines to develop a new process of collaboration.1–3 The transdisciplinary research approach integrates frameworks and methodologies beyond traditional academic disciplines and involves policy makers and other members of the community.4 There is emerging evidence that the transdisciplinary approach will be vital in developing novel solutions for One Health issues.5,6 Indeed, complex problems like transmission of infectious agents through food and water supplies, air quality, climate change, and biodiversity loss require a deep understanding of the animal–human–ecosystem interface.7,8
To reach this potential, transdisciplinary approaches for One Health research must enhance collaboration among various disciplines and sectors of society9–13 and demonstrate added value14 by generating novel solutions to complex problems. To accomplish this, current silos must be broken down among clinical, biomedical, infectious disease, social sciences, population health, policy, and environmental health research.7 We contend that academic institutions should play a foundational role in breaking down these silos and facilitating transdisciplinary research initiatives.
The following institutional capacities have been identified as essential for facilitating transdisciplinary research: (1) the promotion of transdisciplinary education opportunities that include community-based methods, effective communication, and leadership; (2) reduction in conflict and perceived power differentials among disciplines; (3) improved transdisciplinary funding opportunities; and (4) restructuring how researchers are evaluated and rewarded within academic institutions.6,9 If these capacities are developed, One Health research using transdisciplinary approaches can lead to fundamentally new conceptualizations of scientific and social phenomena salient to generating sustainable solutions for One Health problems.10
This Perspective is a call to action for academic institutions to play a foundational role in transdisciplinary research capacity building. We begin by outlining key concepts and methods for building individual and institutional transdisciplinary capacity in order to highlight three value propositions that support the case for improved academic institution capacity for transdisciplinary One Health research. We conclude with three key recommendations to move academic institutions past “research as usual.”
The Transdisciplinary Approach
The terms multidisciplinary, interdisciplinary, and transdisciplinary research are often used interchangeably. However, there are significant differences between these research approaches and the outcomes they generate.15 Multidisciplinary research refers to a process in which researchers from different fields work independently or sequentially, each from their own disciplinary perspectives.9 In interdisciplinary research, researchers share more information and coordinate more closely with researchers from various fields, but their research is still guided by their own discipline-specific theories and frameworks. Transdisciplinary research, on the other hand, is a process in which researchers, community members, and policy makers work together using a shared vision and language that draws together scientific, experiential, and contextual knowledge to innovatively address a common complex problem.4 Although the application of a transdisciplinary research can vary throughout a project, depending on the activities undertaken at different stages along the research time frame, a congruent conceptual framework should guide the research from inception to knowledge translation.16
A Transdisciplinary Conceptual Framework
A conceptual framework provides a method for organizing ideas and approaches over the lifespan of a research project. Without a shared conceptual framework, members of the transdisciplinary team may take different paths in addressing research objectives, resulting in disjointed outcomes and extended research-to-action timeliness.6 Numerous examples of conceptual frameworks for transdisciplinary research exist in the literature,17,18 but an important unifying theme across frameworks is that transdisciplinary research is not hierarchical; rather, it is structured in its processes and phases. With this structure, the organization and momentum of collaborations in transdisciplinary research programs tend to change as the work proceeds. Further, more attention is paid to how research objectives and methods might need to be adapted over a project’s lifespan. Adaptation can be achieved through the inherent feedback loops that guide the transdisciplinary process.
For the purposes of this Perspective, we put forth the framework outlined by Lang and colleagues,19 which conceptualizes transdisciplinary research as an interface practice, whereby the interface allows for real-world problems to trigger scientific inquiry and mutual and joint learning between science and society. According to this framework, transdisciplinary research is a flexible and adaptive process that requires continual shifting between full transdisciplinary collaboration and reductionist approaches to solve component pieces of the puzzle.
Developing Competencies for Transdisciplinary Approaches
Academic institutions worldwide have the potential to play crucial roles in creating enabling environments for transdisciplinary research: They are by default designed to integrate education and research, they have disciplinary experts who are on the cutting edge of their fields, they exist as part of national and international collaborative networks, and they are linked into national and international funding systems. Above all, academic institutions are focal points for change and innovation.
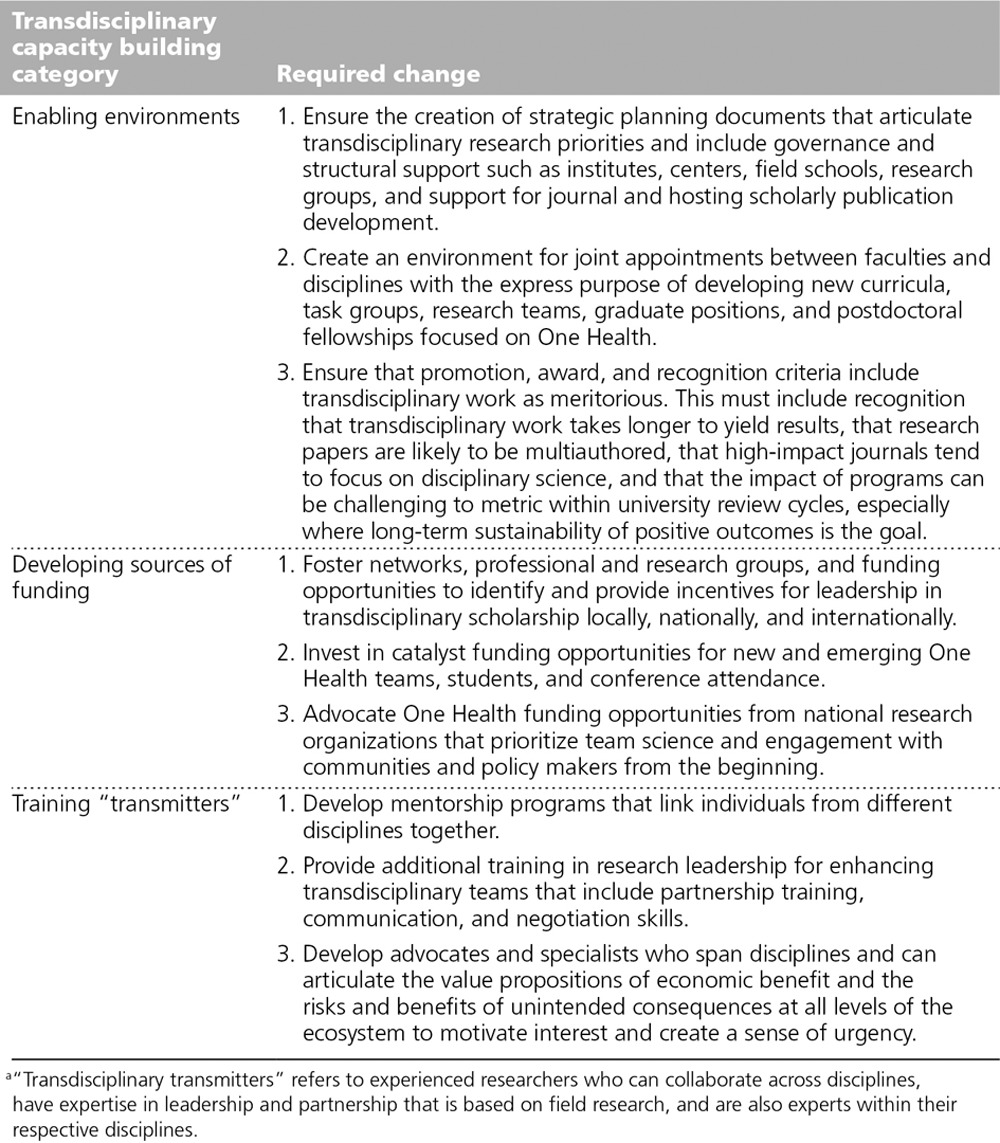
Despite this potential for creating innovative environments and One Health knowledge platforms, transdisciplinary approaches cannot compete alongside traditional research approaches unless there is a dramatic shift in the design, management, organization, and funding of university research. Without such a shift, One Health risks merely being a rebranding exercise of current siloed approaches that will likely fail to deliver on its goal of improving animal, human, and ecosystem health systems. In the sections below we outline steps that could be taken to improve enabling environments and funding for transdisciplinary research as well as the importance of developing “transmitters” who have the expertise to lead transdisciplinary teams (Table 1).
Table 1.
Recommendations for Building Enabling Environments for Transdisciplinary Research That Will Facilitate Successful Funding and the Development of Transdisciplinary “Transmitters”a
Enabling environments and funding
To create an enabling environment for transdisciplinary approaches to address One Health problems, institutions must conduct a capacities assessment to identify and address gaps in the supportive knowledge platforms and organizational environments. For example, the lack of an academic performance reward structure for transdisciplinary research at academic institutions often discourages team-focused research.4,13 Furthermore, historically there has been limited funding for transdisciplinary research projects as many national and international funding agencies preclude allocating money to addressing linkages between disciplines and overly specialized problems.20
Moving forward, researchers need to be engaged with funders as partners, educating them about and promoting the value of transdisciplinary approaches as an intentional phase of research development. Faculty with transdisciplinary interests should be encouraged to sit on advisory and review granting boards, heightening awareness of the value of the approach. Further, developing internal university peer review teams with transdisciplinary expertise will help new research teams take advantage of these emerging opportunities. Teams also need to be creative in identifying alternate funding sources for transdisciplinary research projects.21 Recently, Tri Council granting agencies in Canada have made efforts to support team grant and meeting applications, which can be leveraged to bring transdisciplinary teams together.22 Furthermore, the Eco Health movement and the United Nations Foundation grants, which are inherently transdisciplinary, have highlighted the transdisciplinary approach as a necessary component in addressing complex One Health issues.23
The lack of existing structures in academic institutions to support transdisciplinary research may require teams to spend more time in collaborative dialogue with various funding bodies. This can result in a heightened awareness of the unique constraints, timeliness, and needs for long-term support.9,24 For most academic institutions, mechanisms to build transdisciplinary curricula, learning environments, mentorship, and leadership are still in their infancy. Incentives and recognition for educational scholarship in One Health curriculum development will help to create an environment in which new ways of working together are systematically taught and evaluated for their effectiveness.
The transdisciplinary “transmitter”
We define “transmitters” as experienced researchers who can collaborate across disciplines, have expertise in leadership and partnership that is based on field research, and are also experts within their respective disciplines. We introduce the term to emphasize the importance of developing “real-world” experienced transdisciplinary workers who will guide and advocate transdisciplinary practice in research. Previously naïve collaborators can become additional transmitters and help transdisciplinary One Health approaches become mainstream alongside traditional disciplines. Transmitters are not a new breed of generalists. Rather, they have the unique ability to lead a transdisciplinary team in real-world settings with one overarching conceptual framework that unites individual disciplines for research on a common complex problem.
Current academic programs generally focus on the development of a skill set in one specific discipline and define excellence as mastery of a narrow area. Although individuals’ discipline expertise is essential to the success of a transdisciplinary team, leaders must also be able to appreciate and understand what other disciplines can contribute, including alternative methodologies essential for addressing research objectives. As a result, different leadership styles may be required at different points along the project timeline. During the transdisciplinary research process, from the preconception phase throughout the research and knowledge translation stages, a rotating-role, multileadership model emerges in which the corresponding skill types are used according to what is required at a specific stage during the research project.25 During the initial development stages, research transmitters need to take a leadership role in championing the ideas and values of the transdisciplinary approach and developing shared conceptual frameworks. As the research progresses over time, the leadership role may require someone with a different skill set. The research transmitters should have the knowledge, skills, and attitudes developed through real-world experiences and expert mentoring to facilitate these multileadership changes.
Unfortunately, training programs and mentors experienced in transdisciplinary One Health at academic institutions designed to create these types of cross-discipline transmitters are generally absent. We call for the development and implementation of interprofessional, cross-disciplinary educational programs and research projects through which transmitters can gain experience. Key areas for transmitter training include how to facilitate foundational disciplinary knowledge of the One Health approach to complex health challenges at the animal–human–ecosystem interface, collaborative processes, stakeholder mapping, conflict resolution, cross-cultural and cross-disciplinary communication, knowledge translation and exchange, team building, and management.
Added Value of the Transdisciplinary Approach
To drive capacity building for the development of enabling environments, unique funding opportunities, and transmitter training, the added value of the transdisciplinary approach needs to be explicit. Below we add to the current body of knowledge on how transdisciplinary research adds value through improved sustainability of impact, increased cost-effectiveness, and the enhanced potential for mitigating harmful outcomes.
Improving sustainability of impact
We adopt a broad concept of impact sustainability—namely, that One Health approaches should aim to produce positive outcomes that are resilient, productive, and endure over time. These kinds of challenges are more generally addressed by the emerging discipline of Sustainability Science. Lang and colleagues19 describe three key arguments supporting transdisciplinary research as a foundational strategy to address impact sustainability: (1) The constructive input from various communities of knowledge, relevant disciplines, communities, and governmental levels is incorporated; (2) goals, norms, and visions of the affected communities need to inform intervention strategies; and (3) collaboration between researchers and nonacademic stakeholders increases legitimacy, ownership, and accountability for the identified problem as well as the potential solutions.
Sustainability challenges require the integration of new ways of thinking, producing, and implementing knowledge. The involvement of key stakeholders from outside the academic community is a central component of transdisciplinary research and provides unique and important insights on the appropriateness of potential One Health solutions. Generating sustainable solutions will initially involve a high level of transdisciplinary collaboration in order to define the problem and identify the required approaches. On the basis of pragmatism, individual researchers may then use discipline-specific methods to resolve components of the problem. The transdisciplinary team then integrates all of the discipline-specific information under the overarching conceptual framework to develop sustainable solutions. An example of this emerging approach is the International Livestock Research Institute’s (ILRI) “Reto-o-Reto” project in Kenya.26 This work exemplifies the kind of discipline-boundary-crossing collaborations that we advocate and it demonstrates hybrid local-scientific knowledge generation and application, with a focus on sustainability of outcomes (impact). We propose this approach should be mainstream and fostered by academic institutions.
Increasing cost-effectiveness
Transdisciplinary research capacity will facilitate the investigation of the benefits of cost sharing (allocating costs of the intervention among different sectors according to the proportional benefits)27 among disciplines during the process of developing, adapting, and evaluating One Health interventions20,28 This is especially true for disease control and health promotion efforts in low- to middle-income countries where zoonotic diseases affect food security, household vulnerability, wealth saving, and gender equality as well as the country’s broader economy.14 Transdisciplinary research capacity would facilitate estimating the extent and potential spread of diseases; the cost of zoonotic diseases on livelihood outcomes, national economies, and environments; and identifying factors that prevent the adoption of cost-effective strategies.14 This type of research would not be possible without academic institutions creating centers of excellence, institutes, or research groups that bring together individuals with the competencies to conduct transdisciplinary research and innovative funding strategies to initiate and maintain research programs over time.
The Human and Animal Health research unit of the Swiss Tropical and Public Health Institute (Swiss TPH) is an exemplary case study for transdisciplinary research. Using a transdisciplinary approach, work in this research unit focuses on the health of mobile populations and zoonosis control in low- to middle-income countries.10 Researchers are examining the synergistic potential of closer cooperation between the human health and animal health sectors and integration of various levels of knowledge including the added value of indigenous expertise and engaging communities as co-researchers. Particular attention is paid to the added value of human and animal health, the financial savings, and the environmental benefits from collaboration among all involved sectors. This includes the knowledge, goals, and vision of the local community.
Zinsstag and colleagues5 describe a few cases where the Swiss TPH used transdisciplinary approaches to address One Health problems. For example, Roth et al27 showed that if the costs of vaccinating livestock against brucellosis were allocated to all sectors in proportion to the benefits, the intervention might be profitable and cost-effective for the agricultural and health sectors. In Chad, Zinsstag and colleagues1 showed that the combination of both postexposure treatment of rabies-infected human patients and a dog vaccination campaign broke even with cost-effectiveness of postexposure treatment alone after five years, and was more cost-effective after seven years. Schelling and colleagues29 reported on the success and cost savings of joint vaccination campaigns for livestock and people among nomadic pastoralists. They demonstrated that cooperation between public health, veterinary services, and the community increases accountability, ownership, and legitimacy of these interventions and also results in expanded coverage for essential health interventions for people and livestock in remote rural areas. Throughout these projects, transdisciplinary research skills are institutionalized in the Swiss TPH’s learning environment and facilitate the creation of transdisciplinary transmitters.
Mitigation of harmful unintended outcomes
Research and interventions to address One Health problems occur in complex social and ecological systems. As such, there are likely to be harmful unintended outcomes due to the interplay of action and the context of that action.30 Harmful, unintended outcomes are by their very nature unpredictable, and strategies for mitigation must be based on pairing scientific and contextual knowledge. Transdisciplinary research provides an approach for improving the synthesis of scientific and contextual knowledge, leading to improved consideration and mitigation of harmful unintended outcomes that are known to potentially occur in a variety of areas: physical, psychosocial, economic, environmental, and cultural.31
Health impact assessment (HIA) provides an example of the importance of transdisciplinary research when planning and implementing policies and interventions. HIA is a means of evidence-based decision making to promote positive outcomes and reduce the potential harm of policies that do not have improvements in human health as a primary objective.32–34 The transdisciplinary research process brings scientific, experiential, and contextual evidence to the table. One Health issues such as air pollution and food contamination scares have driven the need for transdisciplinary collaboration to both understand these complex issues and to generate novel approaches to addressing the immediate health threat without generating harmful unintended outcomes.35 Holistic methods of HIA that are based on a transdisciplinary framework are required to adequately address health, social, and cultural impacts on indigenous communities that are affected by industrialization.36
Examples of well-meaning interventions generating harmful unintended outcomes include arsenic groundwater contamination in Bangladesh and West Bengal due to a lack of water safety testing37 and spread of hepatitis C infection following antischistosomal therapy in Egypt that failed to incorporate emerging knowledge of the importance of needle sterilization.38 Transdisciplinary research approaches would have facilitated the inclusion of wider scientific and contextual knowledge during planning and the continued monitoring of these interventions, which may have led to the mitigation of these long-term harmful unintended outcomes.
Recommendations and Conclusion
To achieve the added value of transdisciplinary approaches for One Health problems, we provide three key recommendations for academic institutions that build on previous work in translational and transdisciplinary research. Translational research, or the idea of “bench to bedside,” has been facilitated through programs such as the Clinical and Translational Science Awards. The intent of these awards is threefold: (1) captivate, advance, and nurture a cadre of well-trained multi- and interdisciplinary investigators and research teams; (2) create an incubator for innovative information technologies and research tools; and (3) synergize translational research to promote the application of new knowledge and techniques in clinical practice.39 Transdisciplinary research requires the development of centers of excellence, such as the Swiss TPH, which have developed a culture of One Health through unique training opportunities and practical collaboration.7
Our recommendations build on these successes by focusing on creating enabling environments for One Health and transdisciplinary research, training transmitters using real-world-oriented educational programs that break down silos through collaboration across disciplines and nonacademic stakeholders, and the development of novel funding structures for One Health transdisciplinary research. On the basis of these recommendations, we conclude that without a significant shift in academic research capacity and approaches, we run the risk of simply rebranding our current activities as transdisciplinary and, ultimately, failing to achieve the significant added value of transdisciplinary One Health research addressing complex global health challenges evolving at animal–human–ecosystem interfaces.
Acknowledgments: The authors would like to thank those who attended the transdisciplinary workshop at the University of Calgary for brainstorming and initial conceptualization of this manuscript.
Footnotes
Funding/Support: The University International Grants Committee at the University of Calgary funded this work. The Vanier Canada Graduate Scholarship funds L.K. Allen-Scott for her PhD work.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
References
- 1.Zinsstag J, Dürr S, Penny MA, et al. Transmission dynamics and economics of rabies control in dogs and humans in an African city. Proc Natl Acad Sci U S A. 2009;106:14996–15001. doi: 10.1073/pnas.0904740106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zinsstag J, Schelling E, Waltner-Toews D, Tanner M. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev Vet Med. 2011;101:148–156. doi: 10.1016/j.prevetmed.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mazet JA, Clifford DL, Coppolillo PB, Deolalikar AB, Erickson JD, Kazwala RR. A “one health” approach to address emerging zoonoses: The HALI project in Tanzania. PLoS Med. 2009;6:e1000190. doi: 10.1371/journal.pmed.1000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenfield PL. The potential of transdisciplinary research for sustaining and extending linkages between the health and social-sciences. Soc Sci Med. 1992;35:1343–1357. doi: 10.1016/0277-9536(92)90038-r. [DOI] [PubMed] [Google Scholar]
- 5.Zinsstag J, Meisser A, Schelling E, Bonfoh B, Tanner M. From “two medicines” to “One Health” and beyond. Onderstepoort J Vet Res. 2012;79:492. doi: 10.4102/ojvr.v79i2.492. [DOI] [PubMed] [Google Scholar]
- 6.Min B, Allen-Scott LK, Buntain B. Transdisciplinary research for complex One Health issues: A scoping review of key concepts. Prev Vet Med. 2013;112:222–229. doi: 10.1016/j.prevetmed.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Shomaker TS, Green EM, Yandow SM. One Health: A compelling convergence. Acad Med. 2013;88:49–55. doi: 10.1097/ACM.0b013e31827651b1. [DOI] [PubMed] [Google Scholar]
- 8.Choffnes ER, Relman DA, Olsen L, Hutton R, Mack A. Improving Food Safety Through a One Health Approach: Workshop Summary. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 9.Stokols D. Toward a science of transdisciplinary action research. Am J Community Psychol. 2006;38:63–77. doi: 10.1007/s10464-006-9060-5. [DOI] [PubMed] [Google Scholar]
- 10.Schelling E, Wyss K, Diguimbaye C, et al. Towards integrated and adapted health services for nomadic pastoralists. In: Hirsch Hadorn G, Hoffmann-Reim H, Biber-klemm S, et al., editors. In: Handbook of Tansdisciplinary Research. Heidelberg, Germany: Springer; 2007. pp. 277–291. [Google Scholar]
- 11.Gehlert S, Murray A, Sohmer D, McClintock M, Conzen S, Olopade O. The importance of transdisciplinary collaborations for understanding and resolving health disparities. Soc Work Public Health. 2010;25:408–422. doi: 10.1080/19371910903241124. [DOI] [PubMed] [Google Scholar]
- 12.Stokols D, Harvey R, Gress J, Fuqua J, Phillips K. In vivo studies of transdisciplinary scientific collaboration: Lessons learned and implications for active living research. Am J Prev Med. 2005;28(2 suppl 2):202–213. doi: 10.1016/j.amepre.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Stokols D, Fuqua J, Gress J, et al. Evaluating transdisciplinary science. Nicotine Tob Res. 2003;5(suppl 1):S21–S39. doi: 10.1080/14622200310001625555. [DOI] [PubMed] [Google Scholar]
- 14.Narrod C, Zinsstag J, Tiongco M. A one health framework for estimating the economic costs of zoonotic diseases on society. Ecohealth. 2012;9:150–162. doi: 10.1007/s10393-012-0747-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aagaard-Hansen J, Ouma JH. Managing interdisciplinary health research—Theoretical and practical aspects. Int J Health Plann Manage. 2002;17:195–212. doi: 10.1002/hpm.671. [DOI] [PubMed] [Google Scholar]
- 16.Herweg K, Schäfer N, Zimmermann A. Guidelines for Integrative Training in Inter- and Transdisciplinary Research Settings: Hints and Tools for Trainers of Trainers. Bern, Switzerland: Geographica Bernensia; 2012. [Google Scholar]
- 17.Wiek A, Walterand AI. A transdisciplinary approach for formalized integrated planning and decision-making in complex systems. Eur J Oper Res. 2009;197:360–370. [Google Scholar]
- 18.Carew AL, Wickson F. The TD wheel: A heuristic to shape, support and evaluate transdisciplinary research. Futures. 2010;42:1146–1155. [Google Scholar]
- 19.Lang DJ, Wiek A, Bergmann M, et al. Transdisciplinary research in sustainability science: Practice, principles, and challenges. Sustain Sci. 2012;7:25–43. [Google Scholar]
- 20.Parkes MW, Bienen L, Breilh J, et al. All hands on deck: Transdisciplinary approaches to emerging infectious disease. Ecohealth. 2005;2:258–272. [Google Scholar]
- 21.Harper SL, Edge VL, Cunsolo Willox A. “Changing climate, changing health, changing stories” profile: Using an EcoHealth approach to explore impacts of climate change on inuit health. Ecohealth. 2012;9:89–101. doi: 10.1007/s10393-012-0762-x. [DOI] [PubMed] [Google Scholar]
- 22.Natural Sciences and Engineering Research Council of Canada. Collaborative Health Research Projects. 2013. http://www.nserc-crsng.gc.ca/Professors-Professeurs/grants-subs/CHRP-PRCS_eng.asp. Accessed November 14, 2014.
- 23.Yacoob M, Hetzler B, Langer R. The ecohealth system and the community engagement movement in foundations: A case study of mutual benefits from grants funded by the United Nations Foundation. Nat Resour Forum. 2004;28:133–143. [Google Scholar]
- 24.Abrams DB. Applying transdisciplinary research strategies to understanding and eliminating health disparities. Health Educ Behav. 2006;33:515–531. doi: 10.1177/1090198106287732. [DOI] [PubMed] [Google Scholar]
- 25.Konig B, Diehl K, Tscherning K, Helming K. A framework for structuring interdisciplinary research management. Res Policy. 2013;2:261–272. [Google Scholar]
- 26.Reid RS, Nkedianye D, Said MY, et al. Knowledge Systems for Sustainable Development Special Feature Sackler Colloquium: Evolution of models to support community and policy action with science: Balancing pastoral livelihoods and wildlife conservation in savannas of East Africa [published online November 3, 2009]. Proc Natl Acad Sci U S A. http://www.pnas.org/content/early/2009/11/02/0900313106.abstract. Accessed December 3, 2014. [DOI] [PMC free article] [PubMed]
- 27.Roth F, Zinsstag J, Orkhon D, et al. Human health benefits from livestock vaccination for brucellosis: Case study. Bull World Health Organ. 2003;81:867–876. [PMC free article] [PubMed] [Google Scholar]
- 28.Rashid JR, Spengler RF, Wagner RM, et al. Eliminating health disparities through transdisciplinary research, cross-agency collaboration, and public participation. Am J Public Health. 2009;99:1955–1961. doi: 10.2105/AJPH.2009.167932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schelling E, Wyss K, Béchir M, Moto DD, Zinsstag J. Synergy between public health and veterinary services to deliver human and animal health interventions in rural low income settings. BMJ. 2005;331:1264–1267. doi: 10.1136/bmj.331.7527.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merton RK. The unanticipated consequences of purposive social action. Am Sociol Rev. 1936;1:894–904. [Google Scholar]
- 31.Allen-Scott LK, Hatfield JM, McIntyre L. A scoping review of unintended harm associated with public health interventions: Towards a typology and an understanding of underlying factors. Int J Public Health. 2014;59:3–14. doi: 10.1007/s00038-013-0526-6. [DOI] [PubMed] [Google Scholar]
- 32.Lock K. Health impact assessment. BMJ. 2000;320:1395–1398. doi: 10.1136/bmj.320.7246.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mindell JS, Boltong A, Forde I. A review of health impact assessment frameworks. Public Health. 2008;122:1177–1187. doi: 10.1016/j.puhe.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 34.Wise M, Harris P, Harris-Roxas B, Harris E. The role of health impact assessment in promoting population health and health equity. Health Promot J Austr. 2009;20:172–179. doi: 10.1071/he09172. [DOI] [PubMed] [Google Scholar]
- 35.Joffe M, Mindell J. A framework for the evidence base to support health impact assessment. J Epidemiol Community Health. 2002;56:132–138. doi: 10.1136/jech.56.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kryzanowski JA, McIntyre L. A holistic model for the selection of environmental assessment indicators to assess the impact of industrialization on indigenous health. Can J Public Health. 2011;102:112–117. doi: 10.1007/BF03404158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chowdhury UK, Biswas BK, Chowdhury TR, et al. Arsenic groundwater contamination and sufferings of people in West Bengal-India and Bangladesh. Trace Elements Man Animals. 2000;10:645–650. [Google Scholar]
- 38.Frank C, Mohamed MK, Strickland GT, et al. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet. 2000;355:887–891. doi: 10.1016/s0140-6736(99)06527-7. [DOI] [PubMed] [Google Scholar]
- 39.Dankwa-Mullan I, Rhee KB, Stoff DM, et al. Moving toward paradigm-shifting research in health disparities through translational, transformational, and transdisciplinary approaches. Am J Public Health. 2010;100(suppl 1):S19–S24. doi: 10.2105/AJPH.2009.189167. [DOI] [PMC free article] [PubMed] [Google Scholar]


