Abstract
Many existing and emerging cancer therapies have significant impact on the cardiovascular (CV) health of patients with cancer and cancer survivors. This manuscript examines current aspects of interdisciplinary cardio-oncology clinical care delivery and education in the United States and outlines how these data provide a platform for future development of the field. We present the results of the nationwide survey on cardio-oncology services, practices and opinions, conducted among Chiefs of Cardiology and Program Directors, that demonstrate ranges of clinical activities and identify significant interest for increased educational opportunities and expert training of CV physicians in this field. The survey respondents recognized clinical relevance, but emphasized lack of national guidelines, lack of funds, and limited awareness and infrastructure as the main challenges for development and growth of cardio-oncology. We discuss potential solutions to unmet needs through interdisciplinary collaboration and the active roles of professional societies and other stakeholders.
Keywords: cancer survivorship, cardio-oncology, cardiovascular risk prevention, cardiovascular toxicity
Evidence increasingly shows that cancer and heart disease are inextricably linked, whether through common risk factors, coexistence of both diseases in an aging population, or the deleterious effects of cancer treatments on cardiovascular (CV) health. Despite growing recognition of the importance and complexity of these relationships, the vast majority of CV professionals have little training or exposure to the many new advances in the field of cancer therapeutics and their possible adverse CV effects. There are substantial opportunities for CV specialists to advance partnership with oncologists in exploring new strategies to preserve and restore optimal CV health of patients with cancer and cancer survivors and for CV scientists to unravel the links between these disorders.
Due to significant College-wide interest, the American College of Cardiology's (ACC's) Early Career section has developed a working group to explore the potential in developing this new focus on cardio-oncology, including a potential new member section: Cardio-Oncology. In collaboration with ACC staff, this group has performed an environmental scan and conducted a nationwide survey of cardiologists regarding their views on cardio-oncology services, practices, and opinions to identify patient and professional needs in this growing field.
The aim of this paper is to summarize the key current aspects of interdisciplinary cardio-oncology clinical care delivery and education in the United States and outline how these data provide a platform for future development of the field. As part of the ACC's strategic mission to provide a professional home for CV specialists, we examine existing interests and expertise, as well as available forums and opportunities for education and knowledge exchange. This manuscript does not present a comprehensive review of the considerable clinical or research publications within cardio-oncology, but rather a snapshot of the needs and opportunities in patient care, training, and education in this field. We then discuss potential next steps to advance the field and interdisciplinary collaboration.
The origins of cardio-oncology or onco-cardiology
The terms cardio-oncology and onco-cardiology have both been used to describe this field, encompassing a continuum of CV risk stratification, prevention, and treatment that spans the timeline from cancer diagnosis into survivorship (Figure 1), and depends on close collaboration across cardiology and oncology specialties (1-3). The origins of the field date back to the late1960s when anthracylines, potent new antitumor compounds, were widely introduced into the therapeutic regimens of many cancers (4-6). Observations of their dose-dose dependent cardiotoxic effects not only led to critical modifications of anthracycline-based regimens with cumulative dose limits (7), but also spurred research directed towards the understanding, diagnosis, and prevention of cardiac toxicity. Anthracycline-induced cardiac injury became a prototype of what later was named Type-I cancer therapy-related cardiac dysfunction (CTRCD), characterized by ultrastructural evidence of necrosis, dose-dependence, and largely irreversible effects on cardiac muscle (8,9). In contrast, Type II CTRCD is associated with the use of molecularly-targeted cancer therapeutics whose effects are not dose related, do not have molecular evidence of necrosis, and are often reversible (8,9).
Figure 1. Continuum of Cardiovascular Care in Cardio-Oncology.
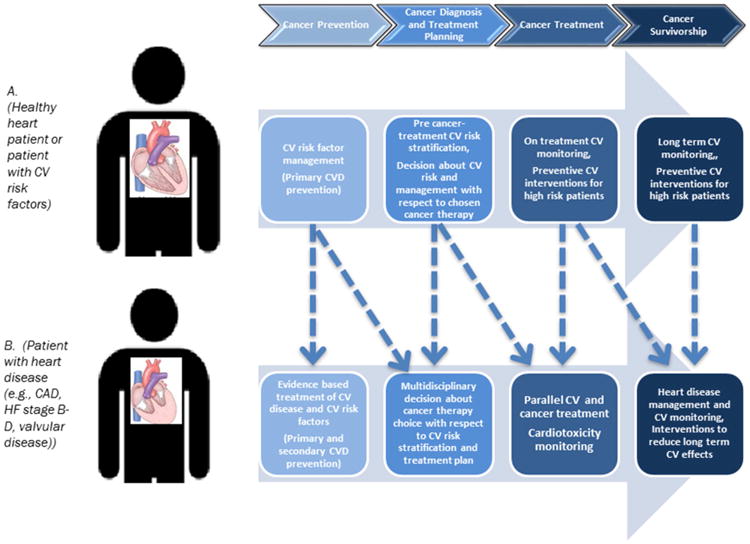
An example of the continuum of cardiovascular care on a timeline of cancer diagnosis, treatment, and survivorship. Patient A represents a patient with no existing cardiovascular disease and patient B represents a patient with a pre-existing cardiovascular condition.
Since these early clinical and pathological observations, our knowledge about cardiotoxicity has seen an impressive growth fueled by molecular investigations of traditional and numerous new cancer therapeutics (10-12), translational research using biomarkers and imaging for CV prediction and risk stratification (13-18), clinical trials evaluating the effects of cardioprotective strategies (19-22), as well as epidemiologic investigations into the burden of these diseases (23-26). In addition to cardiac dysfunction and heart failure, the spectrum of cardiovascular effects related to cancer therapies (spanning many cancer therapeutics and radiation treatments) includes, but is not limited to arrhythmias, valvular heart disease, accelerated atherosclerosis, and pericardial disease. The reader is invited to in-depth reviews of these broad investigational areas (27-33).
The growth of research and clinical activities, evidenced by an exponential increase in the number of publications in the field (Figure 2), has set the foundation for a new discipline, aimed not only at screening, preventing, and treating CV effects of cancer therapies, but also at forming a partnership in providing comprehensive CV care for patients with cancer and cancer survivors (1-3).
Figure 2. PubMed Citations in “Cardio-Oncology”.
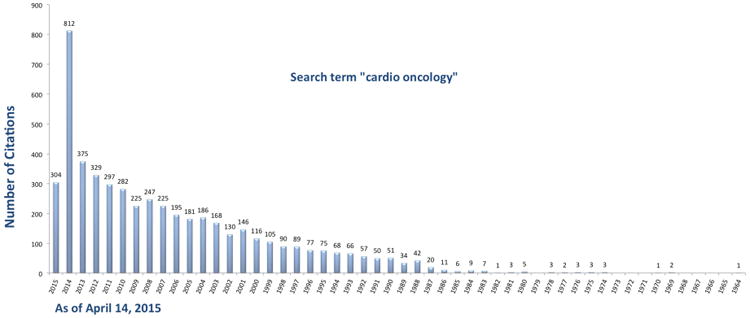
Number of PubMed citations using search term “cardio oncology” by year.
Existing cardio-oncology programs–a vanguard?
Growing clinical demand has resulted in the emergence of dedicated cardio-oncology programs across the United States, frequently at tertiary/quaternary referral centers with both comprehensive cancer centers and dedicated heart failure programs. The MD Anderson Cancer Center, Memorial Sloan Kettering Cancer Center, Vanderbilt-Ingram Cancer Center, University of Pennsylvania Abramson Cancer Center, and Dana-Farber Cancer Institute have pioneered these programs, and set critical groundwork in the field. However, these programs have formed in isolation, as currently there is no coordinating professional association to guide and bridge their development. Despite this lack of external recognition, experience suggests that rapid growth in CV services occurs once a dedicated service is introduced: in 2000, the Department of Cardiology at MD Anderson Cancer Center had 4 general cardiologists managing 1,300 new consults, 3,700 inpatients, and 3,900 echocardiograms and electrocardiograms yearly (C. Iliescu, personal communication, December 2014). Since that time, this group has grown into a comprehensive CV service, including interventional, electrophysiology, and advanced heart failure services, with 2,500 new consults, 8,600 inpatient follow-up visits and 75,000 imaging tests and CV procedures in 2014 (17,000 echocardiographic studies, 55,000 electrocardiograms, 2,000 cardiac catheterization and electrophysiology procedures, and 1,000 vascular and nuclear medicine studies). Cardiomyopathy and cardiotoxicity represent 20% to 30% of the practice, with the remainder comprised of pre-cancer therapy risk stratification and management, acute coronary syndromes, cardiac dysrhythmias, pericardial disease, and cardiac tumors.
Though these few, highly-specialized CV centers are likely to provide excellent care for this patient cohort, the vast majority of patients with cancer and survivors are cared for in community-based practices, rather than in academic settings. In such settings, the volume is expected to be much lower, affording physicians less experience in managing cardio-oncology concerns. Indeed, recent reports suggest patients with cancer may be undertreated with regards to their CV risk compared to similar cancer-free cohorts (34,35). These observations have raised controversy and point to the need for better understanding and attention to the delivery of CV care for this heterogeneous patient population across diverse practice settings.
National cardio-oncology survey
In order to evaluate the current state of cardio-oncology services, practices, and opinions within the wider ACC community, we conducted a nationwide online survey of 444 adult and pediatric Cardiology Division Chiefs and CV Fellowship Program Training Directors. The rationale for focusing on division chiefs and training directors was because of their likely knowledge of existing clinical and educational cardio-oncology activities, as well as our working group's interest in their perception of the needs and potential barriers for development of cardio-oncology services, education, and training. While the choice of this target population biased our sample in favor of academic institutions and limited representation of community awareness and efforts in our results, it provides an important insight into potential future opportunities for cardio-oncology knowledge dissemination from tertiary CV training centers into the community. The survey was conducted from May 5 to May 28, 2014, with reminders sent on May 13 and May 20. A total of 106 CV specialists completed the survey for an overall response rate of 24%. The majority of participants were Cardiology Fellowship Training Directors (44%) or Cardiology Division Chiefs (25%) working at academic medical centers (76%). (All results are shown as Survey Results Supplements). Over half described their Heart Failure program as involving transplant (56%) and their Oncology program as representing a NCI-designated Comprehensive Cancer Center (53%).
Perceived importance of CV care in patients with cancer
The majority of respondents (>70%) felt that CV implications of cancer treatment were a very important consideration in the continuum of treatment of patients with cancer, and two-thirds (65%) thought that access to consultants with specialized training would provide an advantage in caring for patients who suffer CV complications from anticancer treatments. In the majority of centers, the estimated number of CV imaging tests for oncology patients was between 100 and 500 per year, with somewhat lower estimated numbers of CV consults.
Current cardio-oncology programs and training
In 35% of centers, cardio-oncology activities fall within pre-operative consultation services managed by general cardiology, while 27% of centers reported having an established, specialized cardio-oncology service with multiple clinicians. Sixteen percent of respondents reported relying on a single cardiologist with expertise in the area and 12% currently offer no cardio-oncology services, but plan to add them within the next year.
Perceived level of understanding among fellow specialists
A significant number of the participants (39%) did not feel confident in dealing with CV care specific to patients with cancer, and participants gave themselves an average rating when asked about their level of understanding of the impact of holding or stopping anticancer treatment on cancer outcomes. At the same time, cardiologists gave their peer oncologists an average rating about their understanding of the impact of slow or inadequate cardiology assessment on the development of CV complications in oncology patients. Over half (52%) of respondents agreed (vs. 9% who disagreed) that a cardio-oncology service or a dedicated clinician would improve the care of patients with cancer.
Barriers to establishment or expansion of cardio-oncology services
Lack of national guidelines and lack of funding were the most frequently cited barriers to the establishment of a cardio-oncology service (both cited by 44%), followed by limited interest (38%) and infrastructure (36%), and limited educational opportunities (29%). Only 7% felt there were no barriers. Many programs reported having no formal training in cardio-oncology (43%), with some institutions offering exposure during regular clinical rotations (43%), and a small number including lectures in cardio-oncology as part of the Core Curriculum (11%). Importantly, 70% of respondents reported that they would be likely to use educational material for their fellows and staff, if those were available.
Over one-quarter (27%) of respondents (N = 29) offered additional comments to express needed support in the field of cardio-oncology, specifically the need for educational materials and dedicated meetings (25%), training and curriculum (22%), clinical relevance and growth (19%), and the development of guidelines (13%). Two respondents (6%) listed concerns about excessive splitting of the CV specialty into subspecialties.
Roadmap to the Next Level
The survey results document a widespread appreciation of the importance of CV concerns in patients with cancer and a recognized need to improve the care of these patients through provision of specialized services. However, the survey also notes significant barriers. Plans to develop cardio-oncology must recognize both the opportunities and the potential hurdles. The ACC's recognition of the importance of this area and dedication to its advancement is manifest by the recent creation of a member section in cardio-oncology, a major step forward.
In planning for this section, the Cardio-Oncology working group considered current and future opportunities in broad areas of best clinical practices, research, education, and training (Table 1). The activities listed represent an arbitrary and narrow sample that is evolving rapidly (and will be outdated soon), but aim to give an insight into successful seminal efforts that now need to be broadened. For example, our survey identified a need for training in cardio-oncology that presently exists only at few comprehensive cancer centers that possess a critical concentration of expert faculty, clinical volume, and complexity. Expansion of these efforts is necessary to meet the growing demand for trained CV specialists. The establishment of the key competencies within cardio-oncology and the tools necessary to assess training and establish progress, following the Core Cardiovascular Training Statement (COCATS) recommendations (36), will be required to allow further successful growth of the field. Similarly, within broad areas of research and clinical standards in cardio-oncology, there is a need for critical validation and integration of the data from single academic institutions, further development of methods and standards, and strategic implementation and dissemination of knowledge.
Table 1. Current and Future Opportunities in Advancing CV Care in Patients With Cancer and Cancer Survivors.
| Cardio-Oncology Area | Examples of Recent and Current Activities | Possible Future Steps |
|---|---|---|
| Best clinical care practices |
|
|
| Research |
|
|
| Education |
|
|
| Training |
|
|
| Collaborations of stakeholders |
|
|
ACC = American College of Cardiology; ASCO = American Society of Clinical Oncology; ASE = American Society of Echocardiography; CME = Continuing Medical Education; COCATS = Core Cardiovascular Training Statement; CV = cardiovascular; EACVI = European Association of Cardiovascular Imaging; ICOS = International CardiOncology Society; NCI = National Cancer Institute; NCCN = National Comprehensive Cancer Network; NHLBI = National Heart Lung and Blood Institute; SCAI = Society of Cardiac Angiography and Interventions.
The Cardio-Oncology member section will serve as a professional home for the growing number of specialists and allow them to share best practices, develop educational tools and practice standards, design training programs, advocate for cardio-oncology, as well as collaborate with oncology specialists. It is through these advancements and critical partnerships within cardiology and across specialties that a value-based proposition of improved patient care and outcomes will be fulfilled.
Supplementary Material
Respondent Composition
Current Clinical Cardio-Oncology Services
Cardiovascular Consults for Oncology Patients
Oncology Cardiovascular Imaging Requests
Current Cardio-Oncology Educational Programs
Importance of Cardiovascular Consideration
Advantages of Specific Training
Confidence in providing CV Care for Patients with Cancer
Perceived level of understanding by cardiologists and oncologists
Likelihood to Use Educational Materials
Barriers to establishment or expansion of cardio-oncology services
Cardio-Oncology Service Improves Care
Central Illustration. Overview of the Spectrum Of Cardio-Oncology: Bench to Bedside to Community.
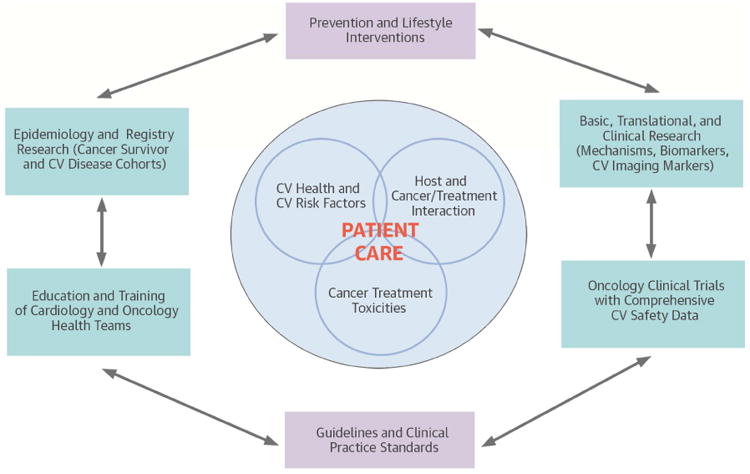
Partnerships across and within the disciplines of cardiology and oncology in the areas of research (basic, translational, clinical, and population science), education and clinical training, and guidelines and clinical documents development as a potential solution to unmet needs and advancement in patient care.
Acknowledgments
The authors thank Kristin West and Amalea Hijar from the American College of Cardiology for their assistance in the preparation of the manuscript. This work was in part supported by NIH/5KL2TR000102-04 to A.B.
Disclosures: Dr. Barac has received research support from the NIH, research support and honoraria for lectures from Genentech, Inc., and consultancy fees from Cell Therapeutics, Inc. Dr. Ky has received research support from Pfizer, the NIH, and PA Cure Health. Dr. Mayer has received research support from Pfizer, Eisai and Myriad. Dr. Douglas has received research grants from the NCI and the University of South Florida.
Abbreviations
- ACC
American College of Cardiology
- ASCO
American Society of Clinical Oncology
- COCATS
Core Cardiology Training Symposium
- CTRCD
cancer therapy-related cardiac dysfunction
- CME
continuing medical education
- CV
cardiovascular
- EACVI
European Association of Cardiovascular Imaging
- NCCN
National Comprehensive Cancer Network
- NCI
National Cancer Institute
- NHLBI
National Heart, Lung and Blood Institute
Footnotes
Disclaimer: The views expressed in this paper by the American College of Cardiology's (ACC) Prevention of Cardiovascular Disease Section do not necessarily reflect the views of JACC or the ACC.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Albini A, Pennesi G, Donatelli F, et al. Cardiotoxicity of anticancer drugs: the need for cardio-oncology and cardio-oncological prevention. J Natl Cancer Inst. 2010;102:14–25. doi: 10.1093/jnci/djp440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minotti G, Salvatorelli E, Menna P. Pharmacological foundations of cardio-oncology. J Pharmacol Exp Ther. 2010;334:2–8. doi: 10.1124/jpet.110.165860. [DOI] [PubMed] [Google Scholar]
- 3.Yeh ET. Onco-cardiology: the time has come. Tex Heart Inst J. 2011;38:246–47. [PMC free article] [PubMed] [Google Scholar]
- 4.Ewer MS, Ali MK, Mackay B, et al. A comparison of cardiac biopsy grades and ejection fraction estimations in patients receiving Adriamycin. J Clin Oncol. 1984;2:112–7. doi: 10.1200/JCO.1984.2.2.112. [DOI] [PubMed] [Google Scholar]
- 5.Ewer MS, Von Hoff DD, Benjamin RS. A historical perspective of anthracycline cardiotoxicity. Heart Fail Clin. 2011;7:363–72. doi: 10.1016/j.hfc.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Lefrak EA, Pitha J, Rosenheim S, et al. A clinicopathologic analysis of adriamycin cardiotoxicity. Cancer. 1973;32:302–14. doi: 10.1002/1097-0142(197308)32:2<302::aid-cncr2820320205>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 7.Von Hoff DD, Layard MW, Basa P, et al. Risk factors for doxorubicin-induced congestive heart failure. Ann Intern Med. 1979;91:710–7. doi: 10.7326/0003-4819-91-5-710. [DOI] [PubMed] [Google Scholar]
- 8.Ewer MS, Vooletich MT, Durand JB, et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol. 2005;23:7820–6. doi: 10.1200/JCO.2005.13.300. [DOI] [PubMed] [Google Scholar]
- 9.Khouri MG, Douglas PS, Mackey JR, et al. Cancer therapy-induced cardiac toxicity in early breast cancer: addressing the unresolved issues. Circulation. 2012;126:2749–63. doi: 10.1161/CIRCULATIONAHA.112.100560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duran JM, Makarewich CA, Trappanese D, et al. Sorafenib cardiotoxicity increases mortality after myocardial infarction. Circ Res. 2014;114:1700–12. doi: 10.1161/CIRCRESAHA.114.303200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jay SM, Murthy AC, Hawkins JF, et al. An engineered bivalent neuregulin protects against doxorubicin-induced cardiotoxicity with reduced proneoplastic potential. Circulation. 2013;128:152–61. doi: 10.1161/CIRCULATIONAHA.113.002203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang S, Liu X, Bawa-Khalfe T, et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med. 2012;18:1639–42. doi: 10.1038/nm.2919. [DOI] [PubMed] [Google Scholar]
- 13.Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109:2749–54. doi: 10.1161/01.CIR.0000130926.51766.CC. [DOI] [PubMed] [Google Scholar]
- 14.Cardinale D, Colombo A, Torrisi R, et al. Trastuzumab-induced cardiotoxicity: clinical and prognostic implications of troponin I evaluation. J Clin Oncol. 2010;28:3910–6. doi: 10.1200/JCO.2009.27.3615. [DOI] [PubMed] [Google Scholar]
- 15.Jordan JH, D'Agostino RB, Jr, Hamilton CA, et al. Longitudinal assessment of concurrent changes in left ventricular ejection fraction and left ventricular myocardial tissue characteristics after administration of cardiotoxic chemotherapies using T1-weighted and T2-weighted cardiovascular magnetic resonance. Circ Cardiovasc Imaging. 2014;7:872–9. doi: 10.1161/CIRCIMAGING.114.002217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in patients with breast cancer treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol. 2014;63:809–16. doi: 10.1016/j.jacc.2013.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawaya H, Sebag IA, Plana JC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging. 2012;5:596–603. doi: 10.1161/CIRCIMAGING.112.973321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thavendiranathan P, Poulin F, Lim KD, et al. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63:2751–68. doi: 10.1016/j.jacc.2014.01.073. [DOI] [PubMed] [Google Scholar]
- 19.Bosch X, Rovira M, Sitges M, et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies) J Am Coll Cardiol. 2013;61:2355–62. doi: 10.1016/j.jacc.2013.02.072. [DOI] [PubMed] [Google Scholar]
- 20.Cardinale D, Colombo A, Sandri MT, et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006;114:2474–81. doi: 10.1161/CIRCULATIONAHA.106.635144. [DOI] [PubMed] [Google Scholar]
- 21.Kalay N, Basar E, Ozdogru I, et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006;48:2258–62. doi: 10.1016/j.jacc.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 22.Seicean S, Seicean A, Plana JC, et al. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J Am Coll Cardiol. 2012;60:2384–90. doi: 10.1016/j.jacc.2012.07.067. [DOI] [PubMed] [Google Scholar]
- 23.Bowles EJ, Wellman R, Feigelson HS, et al. Pharmacovigilance Study Team. Risk of heart failure in breast cancer patients after anthracycline and trastuzumab treatment: a retrospective cohort study. J Natl Cancer Inst. 2012;104:1293–305. doi: 10.1093/jnci/djs317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–98. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 25.Ezaz G, Long JB, Gross CP, et al. Risk prediction model for heart failure and cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Heart Assoc. 2014;3:e000472. doi: 10.1161/JAHA.113.000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsai HT, Isaacs C, Fu AZ, et al. Risk of cardiovascular adverse events from trastuzumab (Herceptin) in elderly persons with breast cancer: a population-based study. Breast Cancer Res Treat. 2014;144:163–70. doi: 10.1007/s10549-014-2836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen MH, Colan SD, Diller L. Cardiovascular disease: cause of morbidity and mortality in adult survivors of childhood cancers. Circ Res. 2011;108:619–28. doi: 10.1161/CIRCRESAHA.110.224519. [DOI] [PubMed] [Google Scholar]
- 28.Force T, Kerkela R. Cardiotoxicity of the new cancer therapeutics--mechanisms of, and approaches to, the problem. Drug Discov Today. 2008;13:778–84. doi: 10.1016/j.drudis.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ky B, Vejpongsa P, Yeh ET, et al. Emerging paradigms in cardiomyopathies associated with cancer therapies. Circ Res. 2013;113:754–64. doi: 10.1161/CIRCRESAHA.113.300218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lal H, Kolaja KL, Force T. Cancer genetics and the cardiotoxicity of the therapeutics. J Am Coll Cardiol. 2013;61:267–74. doi: 10.1016/j.jacc.2012.05.066. [DOI] [PubMed] [Google Scholar]
- 31.Shelburne N, Adhikari B, Brell J, et al. Cancer treatment-related cardiotoxicity: current state of knowledge and future research priorities. J Natl Cancer Inst. 2014;106:dju232. doi: 10.1093/jnci/dju232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vejpongsa P, Yeh ET. Prevention of anthracycline-induced cardiotoxicity: challenges and opportunities. J Am Coll Cardiol. 2014;64:938–45. doi: 10.1016/j.jacc.2014.06.1167. [DOI] [PubMed] [Google Scholar]
- 33.Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53:2231–47. doi: 10.1016/j.jacc.2009.02.050. [DOI] [PubMed] [Google Scholar]
- 34.Ammon M, Arenja N, Leibundgut G, et al. Cardiovascular management of cancer patients with chemotherapy-associated left ventricular systolic dysfunction in real-world clinical practice. J Card Fail. 2013;19:629–34. doi: 10.1016/j.cardfail.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 35.Yoon GJ, Telli ML, Kao DP, et al. Left ventricular dysfunction in patients receiving cardiotoxic cancer therapies are clinicians responding optimally? J Am Coll Cardiol. 2010;56:1644–50. doi: 10.1016/j.jacc.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Halperin JL, Williams ES, Fuster V, et al. ACC 2015 Core Cardiovascular Training Statement 4 (COCATS 4) (Revision of COCATS 3) J Am Coll Cardiol. 2015;65:1721–3. [Google Scholar]
- 37.NCCN Guidelines Version 1.2015 Survivorship: Anthracycline-Induced Cardiac Toxicity. National Comprehensive Cancer Network; Feb 27, 2015. [Accessed May 4, 2015]. Available at: http://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. [Google Scholar]
- 38.Lancellotti P, Nkomo VT, Badano LP, et al. European Society of Cardiology Working Groups on Nuclear Cardiology and Cardiac Computed Tomography and Cardiovascular Magnetic Resonance and the American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, and Society of Cardiovascular Computed Tomography. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2013;14:721–40. doi: 10.1093/ehjci/jet123. [DOI] [PubMed] [Google Scholar]
- 39.Plana JC, Galderisi M, Barac A, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27:911–39. doi: 10.1016/j.echo.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 40.MD Anderson Cancer and the Heart. MD Anderson Cancer Center. [Accessed May 4, 2015]; Available at: http://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/cardiology/cancer-and-the-heart/index.html.
- 41.International CardiOncology Society. [Accessed May 4, 2015]; Available at: http://icosna.org.
- 42.Ewer MS, Yeh ET. Cancer and the Heart. 2nd. Shelton, CT: People's Medical Publishing House; 2013. [Google Scholar]
- 43.Makari-Judon G, Mayer EL. ASCO University, Learning module; 2013. [Accessed May 4, 2015]. 2013 Oncology Literature Reviews Breast Cancer— Fourth Quarter. Available at: http://university.asco.org/2013-oncology-literature-reviews-breast-cancer-fourth-quarter. [Google Scholar]
- 44.Ruddy K, Moslehi J. ASCO University, Learning module; 2014. [Accessed May 4, 2015]. Cardiac Complications of Cancer Therapy. Available at: http://university.asco.org/cardiac-complications-cancer-therapy. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Respondent Composition
Current Clinical Cardio-Oncology Services
Cardiovascular Consults for Oncology Patients
Oncology Cardiovascular Imaging Requests
Current Cardio-Oncology Educational Programs
Importance of Cardiovascular Consideration
Advantages of Specific Training
Confidence in providing CV Care for Patients with Cancer
Perceived level of understanding by cardiologists and oncologists
Likelihood to Use Educational Materials
Barriers to establishment or expansion of cardio-oncology services
Cardio-Oncology Service Improves Care


