Abstract
Objective
To assess the effects on overall self-rated health of the broad range of symptoms and impairments that are routinely asked about in national surveys.
Data
We use data from adults in the nationally representative Medical Expenditure Panel Survey (MEPS) 2002 with validation in an independent sample from MEPS 2000.
Methods
Regression analysis is used to relate impairments and symptoms to a 100-point self-rating of general health status. The effect of each impairment and symptom on health-related quality of life (HRQOL) is estimated from regression coefficients, accounting for interactions between them.
Results
Impairments and symptoms most strongly associated with overall health include pain, self-care limitations, and having little or no energy. The most prevalent are moderate pain, severe anxiety, moderate depressive symptoms, and low energy. Effects are stable across different waves of MEPS, and questions cover a broader range of impairments and symptoms than existing health measurement instruments.
Conclusions
This method makes use of the rich detail on impairments and symptoms in existing national data, quantifying their independent effects on overall health. Given the ongoing availability of these data and the shortcomings of traditional utility methods, it would be valuable to compare existing HRQOL measures to other methods, such as the one presented herein, for use in tracking population health over time.
Keywords: health measurement, health status, HRQOL, impairments, symptoms, weights, population health, quality of life
National surveys typically include a question asking respondents to rate their overall health on a scale from excellent or “best possible” to very poor, or “worst possible.” Such questions have been shown to accurately predict subsequent changes in functional status and mortality,1–3 and are related to a number of specific aspects of health, including physical functioning, pain, energy, and diagnoses.4–9 However, ratings of overall health do not provide detail on the extent to which a range of impairments and symptoms affect heath. For example, to what extent is mobility impairment or pain contributing to health related quality of life (HRQOL)?
Such an analysis is important because understanding why health is less than perfect requires knowing in which domains health is impaired, and the relative impact of these impairments. Although several studies have related specific diseases to overall health,7,10–15 detail on the symptoms and impairments experienced by those with specific diseases and risk factors is needed to understand what contributes to their health and how this changes over time.16 It is also important to account for the effects of co-occurring impairments and symptoms when examining their impacts on overall health.17
A broad range of symptoms and impairments that can affect HRQOL are asked about in ongoing national surveys, including pain, energy, emotion, cognition, and functioning in various domains, such as physical and sensory abilities. Some of these have been asked about as part of existing of health measurement instruments, including the SF-1218 and the Euroqol EQ-5D.19 However, the range of impairments and symptoms asked about in US national health surveil-lance data is broader than the set covered by any single existing instrument. Thus, measuring national health as a function of scores on a particular health measurement instrument fails to capitalize on the wealth of existing data. The objective of this article is to quantify the relative impact of different impairments and symptoms on self-rated overall health, maximizing the use of currently collected national data.
METHODS
Data and Measures
We use 2 independent samples of adults from the Medical Expenditure Panel Survey (MEPS),20,20a,20b a nationally representative survey of the US civilian noninstitutionalized population. Of all US national health surveys, the MEPS includes the widest array of questions on impairments and symptoms. Performing our analyses in the 2002 MEPS and replicating them in the 2000 MEPS enables out-of-sample predictions and tests the robustness of our findings.
MEPS contains questions about the presence and severity of specific impairments and symptoms (shown in the Appendix) and ratings of general overall health. A section on disability days asks about limitations in primary activity (work, school, or housework) and social activity, and a health section covers self care ability, cognitive status, vision, hearing, and physical abilities including walking, bending, and lifting. In addition, a mail-in questionnaire for adult respondents includes the SF-12, from which we obtain depressive symptoms, anxiety symptoms, and vitality limitations, and the EQ-5D, from which we obtain a measure of pain/discomfort. Levels of severity are available for these and other items, allowing the effect of different levels of impairment (such as limited versus no ability to perform primary role activity) to be examined separately. The 100-point rating scale (the visual analog scale from the EQ-5D), asks respondents to rate their current health on a scale from 100, as the best health imaginable, to 0, equivalent to the worst imaginable health state.
The sample sizes with complete data on impairments, symptoms, and health ratings are 22,589 (93% of respondents to both the in-person and mail-in questionnaires) in MEPS 2002, and 12,611 (82%) in MEPS 2000. Individuals missing data on one or more responses are excluded from analyses. A larger portion of those excluded were nonwhite and female in both surveys, and mean age was slightly higher in MEPS 2000 compared with those will full data. Statistical methods designed for survey data and sampling weights are used in SAS© (version 9 for UNIX, SAS Institute Inc., Cary, NC) to account for the MEPS sampling factors including stratification, clustering, oversampling of minorities, and nonresponse to the overall survey and the mail-in health questionnaire.
Analytic Approach
We estimate the health decrements of impairments and symptoms by using them to predict ratings of general overall health using regression analysis. To illustrate the methodology, we consider 2 symptoms or impairments, SI1 and SI2, with responses for each individual of SI1i and SI2i. Our OLS regression equations are of the form:
| (1) |
where Healthi is the rating of current health on a 0–1 scale (a simple transformation of the 100-point scale) and the βs are the estimates of the individual and joint effects of the symptoms or impairments (SI) on health. In interpreting coefficients for combinations of symptoms and impairments, a coefficient of β12 = 0 indicates an additive relationship, in which each symptom and impairment has a full independent effect. A negative coefficient (β12 <0) indicates that having both symptoms is synergistically worse than the sum of their individual effects. A positive interaction coefficient (β12 >0) indicates that the effect of adding a second symptom is not as bad as the effect of that symptom occurring alone.
We include interaction terms between all pairs of impairments and symptoms. We do not consider higher order interactions because of sample size issues and because of the lack of guidance in the literature regarding the relevant interactions to include. For variables such as pain that have more than 1 level of severity, we use a binary variable (“pain/no pain”) in interactions, to avoid the large number of additional interaction terms that would be required to interact each level of severity with every other impairment/symptom. Due to the large number of interactions, we test for potential overfitting of the data using an F test for full versus reduced models in MEPS 2002 and an out-of-sample prediction in MEPS 2000, and do not find evidence that it is a problem, as shown in the Appendix. Correlations between impairment and symptom variables are assessed using ϕ coefficients, and condition indices and standard errors are examined to assess for multicollinearity.
We then calculate weights for each impairment and symptom that are based not only on the coefficients for the main effects but also reflect the effects of interactions. To do this, we calculate mean predicted scores from the regressions first assuming that everyone reported the item (the worst case) and then assuming that no one reported the item (the best case). The difference between these mean predicted scores yields a weight capturing the broadest possible impact of having the symptom or impairment in light of the other symptoms and impairments that people have.
RESULTS
The prevalence of impairments and symptoms in MEPS 2002 is shown in Table 1. Those with the highest prevalence are moderate pain, anxiety symptoms, moderate depressive symptoms, and moderate vitality limitations.
TABLE 1.
Prevalence of Impairments and Symptoms in MEPS 2002*
| Proportion Reporting | |
|---|---|
| Primary role activity (limited) | 0.04 |
| Primary role activity (unable) | 0.04 |
| Secondary role activity | 0.05 |
| Self care | 0.01 |
| Walking (moderate) | 0.07 |
| Walking (severe) | 0.06 |
| Lift/bend/reach/stand/grasp | 0.08 |
| Depressive (moderate) | 0.15 |
| Depressive (severe) | 0.04 |
| Anxiety (moderate) | 0.12 |
| Anxiety (severe) | 0.18 |
| Vision | 0.05 |
| Hearing | 0.06 |
| Cognitive | 0.03 |
| Pain (moderate) | 0.31 |
| Pain (severe) | 0.03 |
| Vitality (moderate) | 0.14 |
| Vitality (severe) | 0.08 |
Definitions of impairments and symptoms provided in Appendix.
The ϕ coefficients used to assess correlations between impairment and symptom variables reveal that most of the relationships are below 0.45, with a few above 0.5, and 1 relatively high relationship of 0.84 (between severe walking and difficulty lifting/bending). Formal tests of multicollinearity (discussed in the Appendix) suggest no bias with main effects.
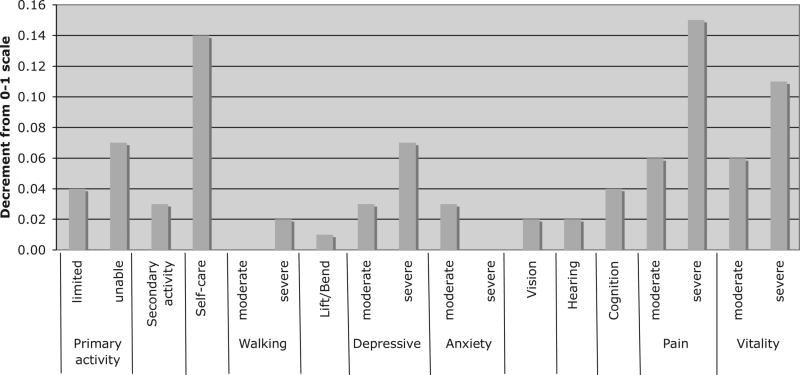
Regression results are shown in the Appendix (Table A1). Across the 2 MEPS surveys, very few impairments and symptoms have significantly different effects (as described in the Appendix), thus only weights derived from the larger 2002 sample are shown (Fig. 1, discussed below). All of the main effect coefficients are negative (symptoms predict worse health), and most of the impairments and symptoms are statistically significantly related to the rating of overall health.
FIGURE 1.
Weights for impairments and symptoms based on regression of 100-point ratings in MEPS 2002.
Many of the interaction terms are positive, indicating that a combination of multiple impairments is not as bad as a simple additive model would suggest. Instances of negative coefficients for interaction terms are also found, indicating that having both symptoms is synergistically worse than the sum of their individual effects.
Figure 1 shows the weights for impairments and symptoms that incorporate the effects of interactions. The symptoms or impairments with the worst estimated decrements to HRQOL across both surveys are severe pain, limitations in self-care, and vitality loss, with weights ranging from −0.11 to −0.15. Other items with substantial decrements are inability to perform primary role, severe depressive symptoms, moderate pain, and moderate vitality loss, with weights of −0.06 to −0.07.
DISCUSSION
This article lays out a method for quantifying the negative impact on health status of a broad range of impairments and symptoms which are consistently tracked by our national surveillance systems. Many of these, such as pain, vitality loss, depressive symptoms and anxiety are quite prevalent (affecting up to a third of the population) and have a substantial adverse impact on health and well-being in the United States.21,22
Regression methods have increasingly been used to assign weights to sets of chronic conditions, which enables accounting for complex interrelationships between them.7,11–13,15 We extend the regression methodology to assign weights to impairments and symptoms collected by one of our national health monitoring surveys. We demonstrate the robustness of our findings in 2 independent, nationally representative samples, finding similar weights and rankings of impairments and symptoms in each one. Our findings are consistent with evidence in the literature of factors negatively affecting self-rated health.4–6,8,9 Severe pain, limitations in self-care activity, and severe vitality impairments are the items with the greatest health decrements, each reducing HRQOL by −0.11 to −0.15.
Our weights may seem small relative to the impact that one would expect these problems to have on HRQOL. This highlights the fact that our weights for symptoms and impairments are to be considered as a group and not individually. The impact of a particular condition such as depression will occur through many impairments and symptoms. We include a broad array of these symptoms and impairments that are interrelated, which reduces the direct effect of each one individually, but provides a more comprehensive picture of their impact on health and identifies those with the worst independent effects. Also, at the aggregate level, the impact of an impairment or symptom on population health will be a product of its weight and its prevalence in the population. This means that an impairment or symptom associated with a relatively mild decrease in HRQOL in individuals can have a relatively large impact on population health if it occurs among a sizeable portion of the population. An example is moderate anxiety, which ranks near the bottom of the symptom list in terms of its impact on health (with an independent decrement of −0.02), but is one of the most prevalent symptoms, reported by 12% of the MEPS 2002 population. Conversely, impairments in self-care have a larger weight (−0.14, second only to severe pain in their impact on health), but are less prevalent (reported by only 1% of the MEPS 2002 population).
The particular importance of pain, low energy, and anxious/depressive symptoms in terms of prevalence and HRQOL impact suggests the possibility that targeting interventions to prevent and alleviate these symptoms could have a significant effect on health across a wide range of the population. To better understand the factors underlying impairments and symptoms and their change over time, future work could relate them to diseases and risk factors.
A number of well-validated existing summary health instruments are composed of questions about impairments and symptoms. The EQ-5D19 includes 5 broad questions on mobility, self care, usual activities, pain/discomfort, and anxiety/depression. The SF-1218 focuses on the ability to perform tasks, excluding information on specific abilities such as self-care, walking, bending, vision, hearing, and cognition. The Health Utilities Index (HUI),23,24 covers several of these impairments but excludes important questions on role activity. The SF-3625 and Quality of Well-Being Scale (QWB)26–28 are more comprehensive instruments; however, their length has precluded their inclusion in ongoing national health monitoring surveys.
Many existing measures assign scores to all possible combinations of impairments and symptoms based on elicitation of utilities or “preferences” for specific combinations of problems.19,23,29–31 For example, one EQ5D health state specifies having “no problems walking about,” “being unable to wash or dress self,” “having some problems with performing usual activities,” having “no pain or discomfort,” and being “moderately anxious or depressed.”32 Samples of community members are asked to imagine having a number of these specific combinations of health problems (each of which they may or may not have personally experienced) and rate them using a valuation method: standard gamble, time tradoff, or a 100-point rating scale.
Our regression method of assigning weights overcomes some of the limitations associated with the rating of hypothetical health scenarios, such as framing effects,33,34 focusing too narrowly on the potential negative life impact of the problem,35,36 and failing to anticipate adaptation to symptoms.35,37–41 The method we present does not require the direct rating of counterfactual health situations by either people with a condition or people without it, but rather asks people to rate only their current general health and to report their current symptoms and impairments.
Utility-based measures that incorporate risk and uncertainty via standard gambles or ask about trading off years of life are not designed to yield decrements for relatively minor health complaints. However, particularly in a healthy population, it is important to try to consider the full range of problems that can affect people—and that can potentially be alleviated through medical care. Our regression method using the 100-point rating scale as a dependent variable also avoids the cognitive challenges inherent in more formal utility elicitation using standard gamble and time-tradeoff techniques, the validity of which has been found to be subject to the numeracy of those surveyed.42
To account for interactions between specific impairments and symptoms, some preference-based scales use an additive model (ie, 15-D,43 SF-6D31), assuming scores on 1 item or domain are unaffected by scores on others. Others use a multiplicative model (HUI,24 AQOL44), or a combination of both (QWB,29 EQ5D19). Another approach, used in the SF measures (ie, SF-36,25 SF-1218) has been to use factor analysis to assign different weights to items based on their relative frequency and correlations with other items. However, this can inappropriately substitute variation in the prevalence of health problems for variation in the impact of these health problems on health, and can thus exclude items with important effects on health if they have a low correlation with others or occur infrequently.29
Our results underline the importance of allowing for flexible functional forms in relating symptoms and impairments to overall health, reinforcing previous findings of complex nonadditive effects.17 As demonstrated by the large number of positive interaction effects, having a combination of health problems is generally not as bad as having each one individually, but is worse than having only one of the problems.
Limitations
Our method examines the average effect of each impairment and symptom on self-rated HRQOL, taking into account other impairments and symptoms that people have. The severity of these problems will vary across individuals, and it is possible that not everyone uses the same frame of reference when rating their overall health.8,9 Our method assumes that people's interpretation of the same health state is independent of demographic and other factors. If certain groups differ systematically in what they consider to be a certain level of health (such as “perfect”), and those groups differ in symptom propensity, our measure will be biased. However, as noted in the Appendix, our weights are unchanged when controlling for sociodemographic variables, which provides some reassurance that our weights are not affected by this bias. Still, to test for differences in cut-points along the scale, we would need to compare self-ratings to objective measures of health, or use vignette questions that ask people to rate the health of others.45,46 These are important avenues for future research.
CONCLUSIONS
Our analyses provide valuable national-level estimates of the relative effects on HRQOL of the broad range of impairments and symptoms asked about in national data. The method presented here or a variant of it could potentially be used to monitor population health over time, in aggregate and for specific groups, providing policymakers with a means to understand what particular symptoms and impairments have the greatest effect on health and what is driving changes in population health and associated spending over time. Given the limitations of existing measures of population health, it would be valuable to compare them to alternative methods for use in tracking population health over time.
ACKNOWLEDGMENTS
The authors thank the Harvard Interfaculty Program for Health Systems Improvement and the Lasker foundation. The authors also thank Dennis Fryback, Daniel Kahneman, Emmett Keeler, Willard Manning, Milton Weinstein, and 3 anonymous reviewers for their comments on earlier versions of the manuscript and the methodology used. Finally, the authors thank Jean Roth of the NBER for statistical advice.
This work was supported by National Institute on Aging (NIA) research Grants: P01 AG17625, P30 AG12810, and R01 AG015911.
APPENDIX
Symptom/Impairment Question Wording
Primary Role Activity
Limited in ability or completely unable to work at a job, do housework, or go to school because of an impairment or a physical or mental health problem.
Other Role Activity
Besides the limitations we just talked about, limited in participating in social, recreational, or family activities because of an impairment or a physical or mental health problem.
Self-Care
Receive help or supervision with personal care such as bathing, dressing, or getting around the house.
Lifting/Bending
Difficulty bending or stooping, lifting 10 pounds, reaching over head, standing 20 minutes, or using fingers to grasp.
Walking
Moderate walking limitation: unable to or some/a lot of difficulty walking a mile and/or some difficulty walking 3 blocks. Severe walking limitation: unable or a lot of difficulty walking 3 blocks and/or unable or some/a lot of difficulty walking up 10 steps.
Pain
Moderate: have moderate pain or discomfort. Severe: have extreme pain or discomfort (EQ-5D).
Depressive Symptoms
Moderate: felt downhearted and blue some of the time or a good bit of the time during the past 4 weeks (vs. a little or none of the time); Severe: felt downhearted and blue most of the time or all of the time during the past 4 weeks (vs. a little or none of the time) (SF-12).
Anxiety Symptoms
Portion of the time person felt calm and peaceful during the past 4 weeks (vs. most or all of the time). Moderate: a good bit of the time; Severe: some, a little, or none of the time (SF-12).
Vitality
Portion of the time person had a lot of energy during the past 4 weeks (vs. most or all of the time). Moderate: a good bit of the time or some of the time; Severe: a little or none of the time (SF-12).
Vision
Difficulty seeing (with glasses or contacts, if used): no difficulty versus some difficulty seeing or cannot read ordinary newspaper print or cannot recognize familiar people standing 2 or 3 feet away or blind.
Hearing
Difficulty hearing (with hearing aid, if used): no difficulty versus some difficulty hearing or cannot hear some or most things people say or deaf.
Cognition
Experience confusion or memory loss such that it interferes with daily activities, have problems making deci sions to the point that it interferes with daily activities, or require supervision for own safety.
Additional Detail on Methods and Results
Comparison of MEPS Surveys in 2002 and 2000
Only 2 coefficients significantly differ between MEPS waves when accounting for everything else in the model: severe depressive symptoms and severe pain (P = 0.02). A few interaction effects also differ significantly across waves in regressions involving both scales. The resulting weights are worse in 2002 by 0.03 for severe depressive symptoms, and better in 2002 by 0.04 for severe pain.
Tests for Overfitting of the Regression Model
Two models were fit in MEPS 2002: a more complete model including all possible two-way interactions between impairments and symptoms and a smaller model including terms for only those interactions with an N of 500 or more (37 of the 66 possible interactions). An F-test for full versus reduced models showed that the explanatory power was significantly greater with the 29 additional interactions (F = 4.91, P = 0.00000). As an additional test, predicted health scores were calculated in MEPS 2000, based on results of regressions in MEPS 2002. The mean-squared error in this out-of-sample prediction did not differ between models (0.0170 for both). As a result, we use the model with more interactions. That said, the correlation between predicted health ratings for the 2 models was very high: 0.997. Thus in practical terms, the issue of overfitting is not particularly important.
Tests of Multicollinearity
Formal tests of multicollinearity indicate that it is present in our analyses only with the inclusion of interaction effects. The highest condition index associated with our full regression model is 54.0, whereas in an alternate model including only the main effects, the highest condition index is 6.6, below the level at which weak dependencies between coefficients may begin to affect regression estimates. However, even in the larger model, standard errors were not inflated, with most well below 0.04.
Effects of Sociodemographic Factors
Our main analyses include all impairments and symptoms, but no sociodemographic variables. We chose not to control for such factors as age, gender, race, and socioeconomic status with the belief that these affect health primarily via specific impairments and symptoms, and that their coefficients would primarily reflect aspects of health that were inadequately captured by our symptom and impairment variables. However, we present a second set of analyses controlling for age, gender, interactions between age and gender, and race (white vs. black and other nonwhite), in the middle column of Appendix Table A1. Although demographic variables are significant predictors of the level of self-rated health, the effects of impairments and symptoms on self-rated health are essentially unchanged when controlling for these demographic factors, indicating that they do not materially affect impairment and symptom weights. The coefficients for demographic variables could reflect either real (unmeasured) health differences or differences in reporting. However, differences in reporting have been in the opposite direction from our findings in studies that have compared self-ratings to ratings of vignettes or controlled for measures of objective function (such as performance tests). In these studies, older adults,46 men,45 and nonwhites45 were less likely to report impairment, whereas we find worse reported health with age and among men and nonwhites. This suggests that our de mographic coefficients primarily reflect differences in actual health that are not captured by our symptoms and impairments. The male coefficient is negative, which is not consistent with known differences in health by gender. However, this occurs only because these analyses control for a broad range of impairments and symptoms. When not controlling for these, men had better self-rated health (not shown in table). This indicates that the worse rating among women was explained by the impairments and symptoms in our model.
APPENDIX TABLE A1.
Proportion Reporting Items and Coefficients From OLS Regression of the 100-Point Rating Scale (Transformed to a 0-1 Scale) on Impairments and Symptoms in MEPS 2002 and MEPS 2000
| Domains and Symptoms/Impairments | Proportion Reporting | Main Model MEPS 2002 | P | Model Including Age, Sex, Race in MEPS 2002 | P | Main Model MEPS 2000 | P |
|---|---|---|---|---|---|---|---|
| Social activity | 0.08 | ||||||
| Limited major role activity | 0.04 | –0.04 | 0.003 | –0.04 | 0.0007 | –0.06 | 0.02 |
| Unable to perform major role activity | 0.04 | –0.07 | <.0001 | –0.06 | <0.0001 | –0.10 | 0.00 |
| Limited in other/secondary role activity | 0.05 | –0.03 | 0.10 | –0.02 | 0.145 | –0.08 | 0.05 |
| Physical activity | 0.09 | ||||||
| Self-care limitations | 0.01 | –0.14 | 0.002 | –0.13 | 0.002 | –0.06 | 0.23 |
| Bending/lifting/standing/reaching/fingers | 0.08 | –0.01 | 0.71 | 0.00 | 0.90 | –0.03 | 0.47 |
| Moderate walking limitation | 0.07 | –0.00 | 0.98 | 0.01 | 0.75 | –0.03 | 0.42 |
| Severe walking limitation | 0.06 | –0.03 | 0.19 | –0.02 | 0.34 | –0.07 | 0.10 |
| Pain | 0.28 | ||||||
| Moderate pain | 0.31 | –0.05 | <.0001 | –0.04 | <0.0001 | –0.05 | <0.0001 |
| Severe pain | 0.03 | –0.17 | <.0001 | –0.16 | <0.0001 | –0.20 | <0.0001 |
| Mental health | 0.12 | ||||||
| Moderate depressive symptoms | –0.03 | <0.0001 | –0.03 | <0.0001 | –0.02 | <0.0001 | |
| Severe depressive symptoms | 0.08 | –0.07 | <.0001 | –0.07 | <0.0001 | –0.03 | 0.0005 |
| Moderate anxiety symptoms | –0.02 | <.0001 | –0.02 | <0.0001 | –0.01 | 0.0144 | |
| Severe anxiety symptoms | 0.08 | –0.04 | <.0001 | –0.04 | <0.0001 | –0.04 | <0.0001 |
| Vitality | 0.22 | ||||||
| Have a lot of energy a little/none of time | 0.14 | –0.05 | <0.0001 | –0.05 | <0.0001 | –0.04 | <0.0001 |
| Have a lot of energy only some of time | 0.08 | –0.12 | <0.0001 | –0.11 | <0.0001 | –0.11 | <0.0001 |
| Senses | 0.10 | ||||||
| Vision impairment | 0.05 | –0.03 | 0.0002 | –0.02 | 0.001 | –0.01 | 0.50 |
| Hearing impairment | 0.06 | –0.02 | 0.0005 | –0.01 | 0.15 | –0.02 | 0.09 |
| Cognitive impairment | 0.03 | –0.03 | 0.10 | –0.02 | 0.19 | –0.08 | 0.00 |
| Interactions | |||||||
| Primary and secondary activity limitations | 0.04 | 0.00 | 0.79 | 0.00 | 0.87 | 0.01 | 0.83 |
| Primary activity and self-care limitations | 0.01 | 0.03 | 0.51 | 0.03 | 0.44 | 0.06 | 0.25 |
| Primary activity and walking limitations | 0.04 | 0.01 | 0.78 | 0.01 | 0.75 | –0.03 | 0.51 |
| Primary activity and bending/lifting limitations | 0.05 | 0.03 | 0.30 | 0.03 | 0.29 | 0.08 | 0.03 |
| Primary activity limitation and depressive symptoms | 0.02 | 0.04 | 0.03 | 0.04 | 0.03 | –0.02 | 0.36 |
| Primary activity limitation and anxiety symptoms | 0.02 | 0.03 | 0.05 | 0.03 | 0.05 | –0.01 | 0.74 |
| Primary activity limitation and vision impairment | 0.01 | –0.02 | 0.23 | –0.02 | 0.24 | –0.02 | 0.55 |
| Primary activity limitation and hearing impairment | 0.01 | 0.00 | 0.89 | 0.00 | 0.87 | 0.03 | 0.25 |
| Primary activity limitation and cognitive impairment | 0.02 | –0.01 | 0.66 | –0.01 | 0.69 | 0.02 | 0.53 |
| Primary activity limitation and pain | 0.05 | –0.04 | 0.00 | –0.03 | 0.01 | –0.01 | 0.59 |
| Primary activity limitation and vitality loss | 0.05 | –0.01 | 0.34 | –0.02 | 0.28 | –0.01 | 0.70 |
| Secondary activity and self-care limitations | 0.01 | –0.03 | 0.20 | –0.03 | 0.20 | 0.03 | 0.50 |
| Secondary activity and walking limitations | 0.03 | –0.03 | 0.37 | –0.03 | 0.38 | –0.03 | 0.35 |
| Secondary activity and bending/lifting limitations | 0.03 | 0.02 | 0.48 | 0.02 | 0.45 | 0.11 | 0.00 |
| Secondary activity and depressive symptoms | 0.01 | –0.01 | 0.50 | –0.02 | 0.43 | –0.05 | 0.22 |
| Secondary activity limitation and anxiety symptoms | 0.01 | –0.04 | 0.06 | –0.04 | 0.05 | –0.01 | 0.75 |
| Secondary activity limitation and vision impairment | 0.01 | 0.02 | 0.36 | 0.02 | 0.39 | 0.02 | 0.46 |
| Secondary activity limitation and hearing impairment | 0.01 | –0.02 | 0.30 | –0.02 | 0.28 | –0.06 | 0.07 |
| Secondary activity and cognitive impairment | 0.01 | –0.01 | 0.68 | –0.01 | 0.73 | 0.01 | 0.70 |
| Secondary activity limitation and pain | 0.03 | 0.02 | 0.42 | 0.02 | 0.43 | 0.00 | 0.90 |
| Secondary activity limitation and vitality loss | 0.03 | 0.03 | 0.10 | 0.04 | 0.05 | 0.02 | 0.52 |
| Self-care and walking limitations | 0.01 | 0.03 | 0.81 | 0.03 | 0.80 | 0.08 | 0.52 |
| Self-care and bending/lifting limitations | 0.01 | 0.07 | 0.56 | 0.07 | 0.57 | –0.05 | 0.69 |
| Self-care limitations and depressive symptoms | 0.005 | –0.03 | 0.24 | –0.04 | 0.21 | 0.00 | 0.93 |
| Self-care limitations and anxiety symptoms | 0.005 | 0.02 | 0.62 | 0.02 | 0.63 | 0.04 | 0.35 |
| Self-care limitations and vision impairment | 0.004 | 0.01 | 0.76 | 0.01 | 0.76 | –0.02 | 0.74 |
| Self-care limitations and hearing impairment | 0.004 | –0.01 | 0.54 | –0.01 | 0.55 | 0.04 | 0.27 |
| Self-care limitations and cognitive impairment | 0.01 | 0.03 | 0.30 | 0.03 | 0.34 | 0.00 | 0.92 |
| Self-care limitations and pain | 0.01 | –0.01 | 0.91 | 0.00 | 0.93 | –0.07 | 0.19 |
| Self-care limitations and vitality loss | 0.01 | –0.05 | 0.34 | –0.05 | 0.29 | –0.06 | 0.24 |
| Walking and bending/lifting limitations | 0.06 | –0.02 | 0.16 | –0.02 | 0.18 | 0.01 | 0.84 |
| Walking limitations and depressive symptoms | 0.02 | 0.02 | 0.58 | 0.02 | 0.67 | 0.03 | 0.51 |
| Walking limitations and anxiety symptoms | 0.02 | –0.01 | 0.61 | –0.01 | 0.72 | –0.04 | 0.08 |
| Walking limitations and vision impairment | 0.01 | –0.02 | 0.42 | –0.02 | 0.53 | 0.04 | 0.32 |
| Walking limitations and hearing impairment | 0.02 | 0.01 | 0.84 | 0.01 | 0.74 | 0.02 | 0.49 |
| Walking limitations and cognitive impairment | 0.02 | 0.01 | 0.70 | 0.01 | 0.72 | 0.01 | 0.92 |
| Walking limitations and pain | 0.06 | 0.02 | 0.38 | 0.02 | 0.42 | 0.03 | 0.45 |
| Walking limitations and vitality loss | 0.05 | –0.02 | 0.35 | –0.02 | 0.36 | 0.02 | 0.41 |
| Bending/lifting limitations and depressive symptoms | 0.02 | –0.03 | 0.39 | –0.03 | 0.46 | –0.02 | 0.53 |
| Bending/lifting limitations and anxiety symptoms | 0.02 | 0.01 | 0.46 | 0.01 | 0.51 | 0.06 | 0.02 |
| Bending/lifting limitations and vision impairment | 0.02 | 0.02 | 0.27 | 0.02 | 0.36 | –0.02 | 0.55 |
| Bending/lifting limitations and hearing impairment | 0.02 | 0.02 | 0.48 | 0.02 | 0.47 | –0.03 | 0.38 |
| Bending/lifting limitations and cognitive impairment | 0.02 | 0.01 | 0.84 | 0.01 | 0.78 | 0.01 | 0.90 |
| Bending/lifting limitations and pain | 0.07 | –0.01 | 0.51 | –0.01 | 0.66 | –0.02 | 0.67 |
| Bending/lifting limitations and vitality loss | 0.06 | –0.01 | 0.55 | –0.01 | 0.51 | –0.01 | 0.58 |
| Depressive and anxiety symptoms | 0.03 | –0.02 | 0.05 | –0.02 | 0.03 | –0.05 | <0.0001 |
| Depressive symptoms and vision impairment | 0.01 | 0.00 | 0.88 | 0.00 | 0.97 | 0.02 | 0.52 |
| Depressive symptoms and hearing impairment | 0.01 | 0.02 | 0.17 | 0.02 | 0.15 | 0.01 | 0.58 |
| Depressive symptoms and cognitive impairment | 0.01 | –0.04 | 0.03 | –0.04 | 0.04 | –0.02 | 0.46 |
| Depressive symptoms and pain | 0.05 | –0.02 | 0.04 | –0.02 | 0.05 | 0.02 | 0.12 |
| Depressive symptoms and vitality loss | 0.05 | 0.01 | 0.25 | 0.02 | 0.13 | 0.02 | 0.13 |
| Anxiety symptoms and vision impairment | 0.01 | 0.00 | 0.67 | 0.00 | 0.74 | 0.00 | 0.91 |
| Anxiety symptoms and hearing impairment | 0.01 | 0.00 | 0.76 | 0.00 | 0.93 | –0.02 | 0.05 |
| Anxiety symptoms and cognitive impairment | 0.01 | –0.02 | 0.32 | –0.02 | 0.30 | 0.00 | 0.95 |
| Anxiety symptoms and pain | 0.05 | 0.00 | 0.87 | 0.00 | 0.67 | 0.00 | 0.71 |
| Anxiety symptoms and vitality loss | 0.05 | –0.01 | 0.02 | –0.01 | 0.03 | –0.01 | 0.01 |
| Vision and hearing impairments | 0.01 | 0.01 | 0.41 | 0.01 | 0.37 | 0.01 | 0.53 |
| Vision and cognitive impairments | 0.01 | 0.03 | 0.14 | 0.03 | 0.13 | –0.01 | 0.72 |
| Vision impairment and pain | 0.03 | 0.01 | 0.18 | 0.01 | 0.17 | –0.02 | 0.31 |
| Vision impairment and vitality loss | 0.03 | –0.02 | 0.16 | –0.02 | 0.14 | –0.01 | 0.64 |
| Hearing and cognitive impairments | 0.01 | 0.01 | 0.48 | 0.01 | 0.52 | 0.00 | 0.88 |
| Hearing impairment and pain | 0.04 | 0.00 | 0.89 | 0.00 | 0.93 | 0.01 | 0.62 |
| Hearing impairment and vitality loss | 0.03 | –0.01 | 0.15 | –0.02 | 0.09 | –0.01 | 0.71 |
| Cognitive impairment and pain | 0.03 | 0.00 | 0.98 | 0.00 | 0.97 | 0.00 | 0.97 |
| Cognitive impairment and vitality loss | 0.03 | 0.00 | 0.96 | 0.00 | 0.89 | 0.02 | 0.57 |
| Pain and vitality loss | 0.15 | –0.05 | <.0001 | –0.05 | 0.0001 | –0.04 | <0.0001 |
| Age | — | –0.00 | <0.0001 | — | |||
| Male | — | –0.01 | <0.0001 | — | |||
| Black | — | –0.01 | 0.0002 | — | |||
| Nonwhite, Nonblack | — | –0.02 | <0.0001 | — | |||
| Intercept | 0.92 | 0.96 | 0.90 | <0.0001 | |||
| Summary statistics | |||||||
| N | 22,589 | 22,589 | 12,611 | ||||
| R2 | 0.536 | 0.542 | 0.470 |
Footnotes
Previous versions of this work were presented at the biennial meeting of the American Society of Health Economists (June 2006, Madison, WI), the biennial meeting of the International Society for Health Economics (July 2005, Barcelona, Spain), the National Bureau of Economic Research Summer Institute Aging Workshop (July 2005, Cambridge, MA), and the annual meeting of the Society for Medical Decision Making, (October 2004, Atlanta, GA).
REFERENCES
- 1.DeSalvo KB, Bloser N, Reynolds K, et al. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21:267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 3.Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995;50:S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- 4.Fylkesnes K, Forde OH. The Tromso Study: predictors of self-evaluated health— has society adopted the expanded health concept? Soc Sci Med. 1991;32:141–146. doi: 10.1016/0277-9536(91)90053-f. [DOI] [PubMed] [Google Scholar]
- 5.Fylkesnes K, Forde OH. Determinants and dimensions involved in self-evaluation of health. Soc Sci Med. 1992;35:271–279. doi: 10.1016/0277-9536(92)90023-j. [DOI] [PubMed] [Google Scholar]
- 6.Meurer LN, Layde PM, Guse CE. Self-rated health status: a new vital sign for primary care? WMJ. 2001;100:35–39. [PubMed] [Google Scholar]
- 7.Cutler D, Richardson E. Measuring the health of the U.S. population. In: Winston C, Baily MN, Reiss PC, editors. Brookings Papers on Economic Activity, Microeconomics: 1997. Brookings Institution Press; Washington, DC: 1998. pp. 217–272. [Google Scholar]
- 8.Kaplan G, Baron-Epel O. What lies behind the subjective evaluation of health status? Soc Sci Med. 2003;56:1669–1676. doi: 10.1016/s0277-9536(02)00179-x. [DOI] [PubMed] [Google Scholar]
- 9.Krause NM, Jay GM. What do global self-rated health items measure? Med Care. 1994;32:930–942. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Brauer CA, Rosen AB, Greenberg D, et al. Trends in the measurement of health utilities in published cost-utility analyses. Value Health. 2006;9:213–218. doi: 10.1111/j.1524-4733.2006.00116.x. [DOI] [PubMed] [Google Scholar]
- 11.Franks P, Hanmer J, Fryback DG. Relative disutilities of 47 risk factors and conditions assessed with seven preference-based health status measures in a national U.S. sample: toward consistency in cost-effectiveness analyses. Med Care. 2006;44:478–485. doi: 10.1097/01.mlr.0000207464.61661.05. [DOI] [PubMed] [Google Scholar]
- 12.Flanagan W, McIntosh CN, Le Petit C, et al. Deriving utility scores for co-morbid conditions: a test of the multiplicative model for combining individual condition scores. Popul Health Metr. 2006;4:13. doi: 10.1186/1478-7954-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saarni SI, Harkanen T, Sintonen H, et al. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Qual Life Res. 2006;15:1403–1414. doi: 10.1007/s11136-006-0020-1. [DOI] [PubMed] [Google Scholar]
- 14.Schultz SE, Kopec JA. Impact of chronic conditions. Health Rep. 2003;14:41–53. [PubMed] [Google Scholar]
- 15.Sullivan PW, Lawrence WF, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Med Care. 2005;43:736–749. doi: 10.1097/01.mlr.0000172050.67085.4f. [DOI] [PubMed] [Google Scholar]
- 16.Revicki DA. National health preference data: a useful resource for health services research. Med Decis Making. 2006;26:310–312. doi: 10.1177/0272989X06291334. [DOI] [PubMed] [Google Scholar]
- 17.Kopec JA, Willison KD. A comparative review of four preference-weighted measures of health-related quality of life. J Clin Epidemiol. 2003;56:317–325. doi: 10.1016/s0895-4356(02)00609-1. [DOI] [PubMed] [Google Scholar]
- 18.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Brooks R, Rabin RE, de Charro F, editors. The measurement and valuation of health status using EQ-5D: a European perspective. Kluwer Academic Publishers; Dordrecht: 2003. [Google Scholar]
- 20. [May 29, 2007];Medical Expenditure Panel Survey Background. Available at: http://www.meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.
- 20a.Cohen J. MEPS Methodology Report No. 1. Agency for Healthcare Policy and Research; Rockville, MD: 1997. [June 24, 2008]. Design and Methods of the Medical Expenditure Panel Survey Household Component. AHCPR Pub. No. 97-0026. Available at: http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr1/mr1.shtml. [Google Scholar]
- 20b.Ezzati-Rice TM, Rohde F, Greenblatt J. Methodology Report No. 22. Agency for Healthcare Research and Quality; Rockville, MD: Mar, 2008. [June 24, 2008]. Sample Design of the Medical Expenditure Panel Survey Household Component, 1998–2007. Available at: http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr22/mr22.pdf. [Google Scholar]
- 21.Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92:195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horsman J, Furlong W, Feeny D, et al. The Health Utilities Index (HUI(R)): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torrance GW, Feeny DH, Furlong WJ, et al. Multiattribute utility function for a comprehensive health status classification system. Health utilities index mark 2. Med Care. 1996;34:702–722. doi: 10.1097/00005650-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Ware JJ, Kosinski M, Gandek B. Sf-36 Health Survey: Manual & Interpretation Guide. QualityMetric Inc.; Lincoln, RI: 2000. [Google Scholar]
- 26.Andresen EM, Rothenberg BM, Kaplan RM. Performance of a self-administered mailed version of the Quality of Well-Being (QWB-SA) questionnaire among older adults. Med Care. 1998;36:1349–1360. doi: 10.1097/00005650-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan R, Anderson J. The general health policy model: an integrated approach. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. Lippincott-Raven; Philadelphia, PA: 1996. pp. 309–322. [Google Scholar]
- 28.Kaplan RM, Bush JW. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1:61–80. [Google Scholar]
- 29.Kaplan RM, Bush JW, Berry CC. Health status: types of validity and the index of well-being. Health Serv Res. 1976;11:478–507. [PMC free article] [PubMed] [Google Scholar]
- 30.McDowell I, Newell C. Measuring health: a guide to rating scales and questionnaires. Oxford University Press; New York, NY: 1996. [Google Scholar]
- 31.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 32.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095–1108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Tversky A, Kahneman D. Rational choice and framing of decisions. J Business. 1986;59:S251–S278. [Google Scholar]
- 34.McNeil BJ, Pauker SG, Sox HC, Jr, et al. On the elicitation of preferences for alternative therapies. N Engl J Med. 1982;306:1259–1262. doi: 10.1056/NEJM198205273062103. [DOI] [PubMed] [Google Scholar]
- 35.Ubel PA, Loewenstein G, Jepson C. Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Qual Life Res. 2003;12:599–607. doi: 10.1023/a:1025119931010. [DOI] [PubMed] [Google Scholar]
- 36.Kahneman D, Tversky A, editors. Choices, Values and Frames. Cambridge University Press; Cambridge, UK: 2000. [Google Scholar]
- 37.Sackett DL, Torrance GW. The utility of different health states as perceived by the general public. J Chronic Dis. 1978;31:697–704. doi: 10.1016/0021-9681(78)90072-3. [DOI] [PubMed] [Google Scholar]
- 38.Slevin ML, Stubbs L, Plant HJ, et al. Attitudes to chemotherapy: comparing views of patients with cancer with those of doctors, nurses, and general public. BMJ. 1990;300:1458–1460. doi: 10.1136/bmj.300.6737.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Epstein AM, Hall JA, Tognetti J, et al. Using proxies to evaluate quality of life. Can they provide valid information about patients’ health status and satisfaction with medical care? Med Care. 1989;27:S91–S98. [PubMed] [Google Scholar]
- 40.Gilbert DT, Pinel EC, Wilson TD, et al. Immune neglect: a source of durability bias in affective forecasting. J Pers Soc Psychol. 1998;75:617–638. doi: 10.1037//0022-3514.75.3.617. [DOI] [PubMed] [Google Scholar]
- 41.Wilson TD, Wheatley T, Meyers JM, et al. Focalism: a source of durability bias in affective forecasting. J Pers Soc Psychol. 2000;78:821–836. doi: 10.1037//0022-3514.78.5.821. [DOI] [PubMed] [Google Scholar]
- 42.Woloshin S, Schwartz LM, Moncur M, et al. Assessing values for health: numeracy matters. Med Decis Making. 2001;21:382–390. doi: 10.1177/0272989X0102100505. [DOI] [PubMed] [Google Scholar]
- 43.Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33:328–336. doi: 10.3109/07853890109002086. [DOI] [PubMed] [Google Scholar]
- 44.Hawthorne G, Richardson J, Osborne R. The Assessment of Quality of Life (AQoL) instrument: a psychometric measure of health-related quality of life. Qual Life Res. 1999;8:209–224. doi: 10.1023/a:1008815005736. [DOI] [PubMed] [Google Scholar]
- 45.Iburg KM, Salomon JA, Tandon A, et al. Global Programme on Evidence for Health Policy Discussion Paper. World Health Organization; Geneva: 2001. Cross-population comparability of self-reported and physician-assessed mobility levels: evidence from the Third National Health and Nutrition Examination Survey. [Google Scholar]
- 46.Salomon JA, Tandon A, Murray CJ. Comparability of self rated health: cross sectional multi-country survey using anchoring vignettes. BMJ. 2004;328:258. doi: 10.1136/bmj.37963.691632.44. [DOI] [PMC free article] [PubMed] [Google Scholar]