Abstract
Background
Chronic kidney disease (CKD) has become a significant part of the GP’s workload since the introduction of the National Institute for Health and Care Excellence guidelines in 2008. Patients with advanced CKD (stages G4 and G5) often have comorbidities, varied disease progression, and are likely to be older. GPs may experience difficulties with management decisions for patients with advanced CKD, including when to refer to nephrology.
Aim
To explore GPs’ views of managing patients with advanced CKD and referral to secondary care.
Design and setting
Qualitative study with GPs in four areas of England: London, Bristol, Birmingham, and Stevenage.
Method
Semi-structured interviews with 19 GPs. Transcribed interviews were thematically analysed.
Results
GPs had little experience of managing patients with advanced CKD, including those on dialysis or having conservative care (treatment without dialysis or a transplant), and welcomed guidance. Some GPs referred patients based on renal function alone and some used wider criteria including age and multimorbidity. GPs reported a tension between national guidance and local advice, and some had learnt from experience that patients were discharged back to primary care. GPs with more experience of managing CKD referred patients later, or sometimes not at all, if there were no additional problems and if dialysis was seen as not in the patient’s interests.
Conclusion
GPs want guidance on managing older patients with advanced CKD and comorbidities, which better incorporates agreement between local and national recommendations to clarify referral criteria. GPs are not generally aware of conservative care programmes provided by renal units, however, they appear happy to contribute to such care or alternatively, lead conservative management with input from renal teams.
Keywords: attitude of health personnel, chronic kidney disease, patient care management, primary health care, qualitative research
INTRODUCTION
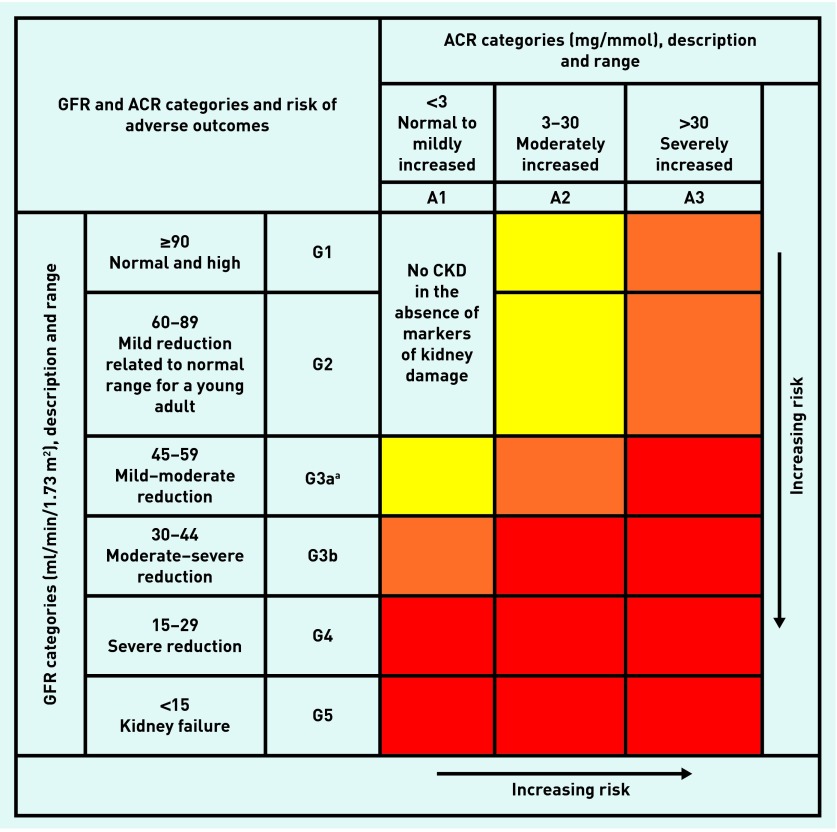
Diagnosis of chronic kidney disease (CKD) is common in primary care following the inclusion of CKD in national guidelines and the Quality and Outcomes Framework (QOF).1,2 CKD stage is based on the estimated glomerular filtration rate (eGFR) indicating the level of kidney function, classified from G1 to G5.1 The National Institute for Health and Care Excellence (NICE) also classifies CKD based on the combination of eGFR and albumin:creatinine ratio, giving the associated risk of adverse outcomes1 (Figure 1). Moderate-to-severe CKD (G3–G5) affects around 6% of the UK population, rising to around 30% of people aged >75 years.3 CKD is associated with poor clinical outcomes including mortality, cardiovascular disease, and progression to end-stage renal disease.4,5 Risk of poor clinical outcomes can be reduced by good blood pressure control, avoidance of nephrotoxic drugs, and appropriate use of renin–angiotensin–aldosterone system inhibitors.1
Figure 1.
Classification of chronic kidney disease, considering estimated GFR and ACR. aConsider using eGFRcystatinC for people with CKD G3aA1 (see recommendations 1.1.14 and 1.1.15 of the NICE guidelines). ACR = albumin:creatinine ratio. CKD = chronic kidney disease. GFR = glomerular filtration rate. Yellow = moderately increased risk. Orange = high risk. Red = very high risk. Adapted with permission from Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013; 3(1): 1–150.
Patients who progress to advanced CKD (G4 and G5), are commonly referred to secondary care following NICE guideline recommendations (Box 1).1 Studies indicate, however, that this may be delayed for some patients, meaning they have less specialist care before starting renal replacement therapy (RRT).6 Timely referral to secondary care allows patients to be educated about their management options to aid informed decision making at a later stage.7 Once under nephrology care, guidelines recommend starting RRT for symptomatic patients with advanced CKD G5 and for patients with an eGFR <6 ml/min/1.73 m2 even if asymptomatic.8,9 Therefore, patients need to be aware of their RRT options if their illness progresses. However, studies indicate that for some older adults, with frailty and comorbidities, the balance of benefit versus burden may favour non-dialysis/conservative care.10–12 As a result, conservative care pathways within nephrology services have been developed.13 Under such pathways patients may continue to be seen in secondary care or may be referred back to primary care. It is unknown whether GPs are aware of such conservative renal pathways and whether they are managing patients under such pathways. Exploring GPs’ awareness and views of such programmes may contribute to understanding GPs’ decision making regarding referrals.
Box 1. Summary of National Institute for Health and Care Excellence guideline recommendations on referral of patients with chronic kidney disease.1.
Take into account the individual’s wishes and comorbidities when considering referral.
People with chronic kidney disease (CKD) in the following groups should normally be referred for specialist assessment:
Glomerular filtration rate (GFR) <30 ml/min/1.73 m2 (GFR category G4 or G5), with or without diabetes
Albumin:creatinine ratio (ACR) ≥70 mg/mmol, unless known to be caused by diabetes and already appropriately treated
ACR ≥30 mg/mmol (ACR category A3) together with haematuria
Sustained decrease in GFR of ≥25%, and a change in GFR category or sustained decrease in GFR of ≥ 15 ml/min/1.73 m2 within 12 months
Hypertension that remains poorly controlled despite the use of at least four antihypertensive drugs at therapeutic doses
Known or suspected rare or genetic causes of CKD
Suspected renal artery stenosis.
Consider discussing management issues with a specialist by letter, email, or telephone in cases where it may not be necessary for the person with CKD to be seen by the specialist.
Once a referral has been made and a plan jointly agreed, it may be possible for routine follow-up to take place at the patient’s GP surgery rather than in a specialist clinic. If this is the case, criteria for future referral or re-referral should be specified.
To date, qualitative studies have explored GPs’ experiences of identifying and managing CKD G3 in primary care.14,15 They have shown that GPs experienced difficulties diagnosing CKD, explaining the diagnosis to patients without causing undue distress, and had concerns about overdiagnosing CKD.14,15 Studies concluded that general practice was likely to be missing opportunities for health promotion and prevention of disease progression and/or complications.14–16
How this fits in
Chronic kidney disease (CKD) is commonly diagnosed in primary care and GPs are encouraged to manage and refer patients according to guidelines. Previous studies have explored GPs’ views of managing moderate CKD (G3) but have not explored views of managing advanced CKD (G4 and G5). This study indicates that there is variation when GPs decide to refer patients to secondary care depending on kidney function, patient’s age, and comorbidity; GPs’ previous experience of managing CKD; and referrals back from secondary care. GPs require detail on how local recommendations fit with national guidelines in order to inform referrals, as well as guidance on the management of patients with multimorbidity.
No qualitative study has focused on the management of patients with advanced CKD in primary care. Therefore, this study aimed to explore GPs’ views and experiences of managing patients with advanced CKD and their knowledge of conservative care pathways to identify reasons for referral or non-referral of patients to secondary care.
METHOD
The study was carried out as part of the Conservative Kidney Management Assessment of Practice Patterns Study (CKMAPPS). It was one of three qualitative studies exploring the views of nephrologists, patients with CKD, and GPs on the management of advanced CKD. The views of nephrologists and patients are reported elsewhere.17,18
CKMAPPS included nine renal units, selected based on their variation in management of advanced CKD, as indicated in a previous survey, and location in England.19 The current study identified general practice surgeries in four regions, in the catchment areas of four of these nine renal units (London, Bristol, Birmingham, and Stevenage). Surgeries were identified from the QOF database.
All participants were GPs currently practising in England. One GP from each surgery was invited to take part in the study by post. Purposive sampling was undertaken, seeking variation in relation to the key criteria of relevance for the topic, years in practice, number of GPs in practice, and location (rural, suburban, or urban). If a GP declined or did not respond after 8 weeks, a second GP from the same surgery was invited. GPs returned a reply slip and signed a consent form by post to indicate they were happy to participate and were contacted by the research team to arrange an interview.
An experienced non-clinical researcher carried out telephone interviews. Interviews followed a semi-structured guide that explored GPs’ previous experience of managing CKD (Appendix 1). GPs were paid £40 for participating in the study. Interviews continued until data indicated saturation.20 Interviews were audiorecorded, transcribed verbatim, and transcripts were checked by the interviewer before analysis.
Data were analysed following an inductive thematic analysis process.21 This approach minimised the influence of the researchers’ preconceptions, ensuring that analysis was grounded in the data. Analysis began as soon as the first transcript was received, and subsequent data collection and analysis were conducted concurrently. The same researcher who carried out the interviews led analysis. Data were read and re-read to aid familiarity. Initial transcripts were coded by identifying each segment of text which represented a meaningful unit of data in relation to the main research question. Codes were named to represent the original data as closely as possible. Existing codes were used in later transcripts where similar data were identified. NVivo (version 9) was used to organise data and facilitate coding. Once 10 transcripts had been analysed codes were grouped into initial themes and sub-themes, based on their similarities, to represent the main emerging topics coming from the data. The remaining transcripts were coded according to these initial themes. Any data that did not fit under existing themes were coded under a new label to ensure analysis was open to emerging issues not previously anticipated or identified during earlier analysis. Themes and supporting quotations were discussed with a second researcher and revised to produce a consensus thematic framework. Final themes were discussed with the wider research team and were renamed to enhance validity and clarity until a consensus was reached.
RESULTS
A total of 25 GPs from a pool of 353 invited to the study responded to say they were interested in participating. It was not possible to obtain information on non-responders or reasons for refusal. Six GPs were unable to take part in an interview because of a lack of availability. Nineteen interviews were completed, with three to six GPs interviewed in each region. The responders reflected diversity across key characteristics (Table 1). Interviews were carried out between January and August 2013.
Table 1.
Characteristics of participating GPs (n = 19)
| GP characteristics | Mean | Range |
|---|---|---|
| Age, years | 46 | 31–60 |
|
| ||
| Years in practice | 16 | 3–32 |
|
| ||
| Number of GPs in practice | 5 | 2–12 |
|
| ||
| n | % | |
|
| ||
| Male sex | 12 | 63 |
|
| ||
| Location of practice | ||
| Urban | 3 | 16 |
| Suburban | 11 | 58 |
| Rural | 5 | 26 |
|
| ||
| GP subject of interest | ||
| Renal | 2 | 11 |
| Renal-related disease (for example, diabetes) | 8 | 42 |
| Neither | 9 | 47 |
Five themes were identified, as outlined below. These themes were derived based on a comprehensive analysis of all interviews.
Experiences of managing advanced CKD
Most GPs reported that they did not feel confident managing patients who had advanced CKD without input from specialists. While GPs reported that they had several patients diagnosed with CKD G3, most reported that they had limited experience of managing patients with advanced CKD because there were small numbers of such patients:
‘I know some Birmingham areas they have a lot of patients on dialysis because they are from different [ethnic] backgrounds, we don’t have that, we have one or two maximum on dialysis in our practice. So it’s not that frequent to go into that stage.’
(GP8, Birmingham, suburban location, 10 years in practice)
Interviewer (I): ‘What about when you are referring someone, what sort of stage would you want to refer them?’
GP: ‘Ooo, again, I probably would look it up. I think that ... no, I’m not going to answer that because I would look it up to be honest because I’m so unfamiliar at the moment that I wouldn’t guess.’
(GP3, Bristol, inner-city location, 13 years in practice)
Other GPs with a particular interest in renal disease or associated conditions described feeling knowledgeable about how best to manage patients with CKD.
Increased confidence also applied to GPs with older patient populations who saw CKD more often:
‘I’ve got an older population. Nine per cent of my population have got an eGFR below 60. That’s nine per cent. Which is why it’s an area, shall I say, I do quite a lot of work in.’
(GP1, Bristol, rural location, 32 years in practice)
Communicating about CKD with patients
Most GPs made reference to the asymptomatic nature of CKD and the difficulty of explaining a diagnosis to patients as a result:
‘ [Patients] don’t understand what [CKD] actually means. Especially those who don’t really have symptoms, there are lots of people with CKD 5 that don’t have symptoms ... it’s “life’s all fine, how can my kidneys be failing? I feel fine” ... I think because they don’t have symptoms, often they don’t really understand the importance of it.’
(GP4, Stevenage, suburban location, 10 years in practice)
GPs reported that patients did not commonly know about kidney disease. GPs said that they tried to decrease patients’ anxiety about diagnosis by giving information over several consultations, explaining a diagnosis at an earlier stage of CKD, and avoiding certain terminology such as ‘chronic kidney disease’. GPs reported feeling that this wording was too strong and some felt it could lead to patients being overly anxious about their diagnosis. Instead GPs stated that the kidneys were not ‘working as well as they should be’ or that the kidneys were ‘ageing faster than you’:
‘It’s like other things, if you use the word “kidney failure” or “heart failure” people instantly think “oh my goodness, I’m going to drop dead tomorrow”.’
(GP2, Bristol, inner-city location, 3 years in practice)
GPs felt that some patients with moderate, stable CKD would not know of their clinical diagnosis and that this may be a result of avoiding such terminology. GPs did feel, however, that patients with advanced CKD would know of their diagnosis and all reported that they would inform such patients.
Getting advice on managing advanced CKD
All GPs had previously contacted a renal unit for advice about how to manage patients with advanced CKD and most were satisfied with the ease of communication. Some GPs knew nephrology staff well and a smaller number had received training from their local unit. One example was educational outreach sessions:
‘ [The consultant nephrologist] has been proactive, he’s come out and given talks to us, come to the practice and he’s also given talks to postgraduate meetings.’
(GP9, Birmingham, suburban location, 8 years in practice)
GPs described two specific areas where they felt they needed guidance. These were how to optimise referral decisions and the management of patients with advanced CKD when it was deemed too early to refer them. Particular patient populations were seen as more complex than others:
‘If you are a young person with [CKD] four and five it’s much more clear cut as to what you are treating and how you manage it compared to an elderly person when there is all this comorbidity, you know, they have all got diabetes, they have all got ischaemic heart disease, very few of them have just got renal disease. The care is much more complicated.’
(GP14, London, suburban location, 32 years in practice)
Referring patients with CKD to secondary care
There appeared to be variation in when GPs referred patients to secondary care. Two key referral practices were identified:
referral of all patients based on eGFR; and
referral driven by individual patient factors.
GPs with less experience of CKD management, or more uncertainty about management, tended to refer all patients with advanced CKD. A decline in the eGFR, rather than the exact value, was most often the key factor:
‘I think [referral] depends on rate of decline [of eGFR], I think it depends on other features, I mean if there are other things that we think might be causing it, particularly diabetes, difficult hypertension, yeah, I think rate of decline.’
(GP6, Bristol, rural location, 20 years in practice)
A referral approach shaped by individual patient factors, including patient preference, indicated the importance of multimorbidity, age, and travel time to the nearest renal unit. GPs were more likely to refer patients with advanced CKD who had particular management problems, such as poorly-controlled hypertension or proteinuria. Some said they avoided referring very older patients unless their CKD was causing them problems:
‘I mean if they are sort of over 75, over 80, I think each case is on its own merit in terms of stage 4 really, you know, have we got well-controlled hypertension? Is it recently developed? Is it rapidly declining? And if there is a lot of proteinuria as well we would refer that particular stage 4, but otherwise some stage 4s in the quite elderly, we might just be sort of keeping an eye on.’
(GP9, Birmingham, suburban location, 27 years in practice)
Interviewees gave several reasons for trying not to refer unless absolutely necessary. There appeared to be a widely-held view that it was better for patients to be treated in primary care where possible and GPs perceived that patients preferred this:
‘ [Our] kidney service is fine but it’s a pressurised service. And I don’t like sending people we could have managed better in the community or managed better locally, down to a service which is pushed. But at the same time if needs do, hey, I work with them.’
(GP1, Bristol, rural location, 32 years in practice)
One GP reported that his/her practice preferred not to refer older patients with CKD to secondary care because they had other comorbidities that were being actively treated which might conflict with CKD management:
‘Well, to be honest, we don’t send the older [patients] because, as I say, it is all about their other morbidities. [Later in interview] Because usually [older patients] have got something else, they have got a coronary disease or something else which kind of overrides what is happening in their kidneys ... what will frequently happen is the cardiologist will start the medication that makes the renal function deteriorate but the cardiologist will say, “Never mind the renal function, take it.” They then get to the renal physicians who say, “Absolutely not, they can’t be taking this”, and they stop it. And so you’ve gone round in a big circle and nobody has benefited. That frequently happens.’
(GP14, London, suburban location, 32 years in practice)
GP accounts invoked a tension between national guidelines to refer all patients with advanced CKD and personal experience of renal units immediately referring patients back to primary care when referrals were deemed to be ‘too early’ or inappropriate. Such experience had led GPs to revise how they made subsequent referral decisions:
‘That is the dilemma, as an ex-colleague of mine said “I didn’t want to refer all my patients with CKD 4 because one of the nephrologists said ‘we’re not going to do a great deal anyway’.” So even though the guidance says refer everybody with stage 4 [GPs] don’t particularly.’
(GP7, Bristol, rural location, 20 years in practice)
‘I think if they are going to discharge more and more people back to GPs there has to be clear guidelines as to when you refer them back [to nephrology].’
(GP4, Stevenage, suburban location, 10 years in practice)
Managing patients by conservative and palliative care
GPs reported that they had little involvement with patients after they had been referred because patients commonly started dialysis. GPs maintained care for patients for whom referral was perceived to be inappropriate and occasionally managed patients who had chosen not to have dialysis (conservative care).
GPs identified patients who they thought they would be unlikely to refer as they thought they would be unlikely to benefit from dialysis, for instance, because of low life expectancy from another cause, or very poor quality of life. These were very specific groups of patients for whom palliative care was thought to be the most appropriate option. GPs most often gave examples of patients already receiving palliative care for a non-renal condition, patients with advanced dementia, and/or patients who were in nursing homes. In most cases GPs said they would not alert nephrology to such patients, although interviewees differed, with some wanting to check their non-referral decision with specialists:
GP:’ [I wouldn’t refer a] palliative care patient, with cancer, or a patient who is in a nursing home, or who has severe dementia and therefore is in a nursing home.’
I: ‘Ok. And what would your reasons be for not referring those?’
GP: ‘Purely what quality of life would they have? Because they are not mobile and it’s not fair.’
(GP12, Stevenage, suburban location, 13 years in practice)
GPs were not familiar with conservative care of kidney disease and few had experience of such patients. GPs felt comfortable with the idea of conservative care if patients could be treated as palliative care patients, that is, the patient had made an informed decision not to pursue dialysis. However, some GPs worried about patients changing their mind:
GP: ‘We have had [patients receiving conservative care]. I’m not sure whether they are still with us or not. But, yes, there have been situations where they have declined dialysis.’
I: ‘And how do you feel about managing those patients?’
GP: ‘Well, again I suppose it is trying to do it as best you can. I mean obviously with the patients being under the care of the secondary care services at least you feel that there is communication going on and if there is a change of heart on the side of the patient or a deterioration then you have got someone to call on to and give you some further advice and support.’
(GP10, Birmingham, suburban location, 19 years in practice)
DISCUSSION
Summary
Most GPs reported having limited experience of managing patients with advanced CKD, including those on dialysis and having conservative care, and subsequently needed guidance from specialists. GPs felt they required guidance on when to refer patients and how to manage patients before referral; in particular, older adults and those with comorbidities. While GPs reported that it was sometimes difficult to explain a diagnosis of CKD, they believed that patients with advanced CKD would be aware of their condition. There was variation about when GPs decided to refer patients and they emphasised the importance of a decline in kidney function as a prompt for referral. GPs highlighted a tension between national guidelines and local advice. There was a perception among all GPs that managing patients in primary care was preferable where possible and some GPs postponed referrals or did not refer patients who they perceived to be unlikely to benefit from dialysis. Lastly, while GPs were largely unaware that all four renal units offered conservative care, they said they would be happy to care for such patients if this was an informed decision.
Strengths and limitations
Although few GPs responded to the invitation to participate, the use of purposive sampling and interviewing until data indicated saturation meant that findings are likely transferable to GPs across the UK. This is limited somewhat by the fact that the sample included a number of GPs with an interest in renal disease or a related condition, which was to be expected.
Interviews rather than focus groups were chosen for data collection because the research question focused on the experiences and knowledge of individuals rather than exploring primary care culture or social norms.22 Telephone interviews allowed GPs to participate easily from four locations in England, which reduced time spent on data collection and travel costs. Invitations to participate in focus groups risked obtaining fewer responses because of the greater time commitment required for such a study.
Unlike previous studies, GPs were recruited from practices from a range of areas of England, rather than from practices that were taking part in a larger study, and were not required to take part in other aspects of the CKMAPPS project.14,15 This avoided recruiting only from practices who were research focused and added to the relevance of findings to GPs in general.
Finally, interviews were carried out before the introduction of new NICE guidelines in July 2014 and the results should be viewed in light of this.1
Comparison with existing literature
There were similarities between this study, on advanced CKD, and previous research looking at GP management of moderate CKD.14,15 Results indicated that GPs experienced concern in telling patients with moderate stage CKD of their diagnosis and used specific terminology to avoid patients becoming distressed.14 GPs also had difficulty explaining moderate CKD to patients because of the lack of public awareness of kidney disease.15 While GPs reported that not all patients with CKD G3 would be aware of their diagnosis, they believed that patients with advanced CKD would be aware, indicating they viewed stages G4 and G5 differently. No qualitative literature has explored GPs’ views of managing advanced CKD in practice.
Implications for research and practice
Most patients with advanced CKD have multiple morbidities and frailty, with the condition being particularly common among older patients.23 Some GPs highlighted a conflict between treatment for CKD and treatment for other chronic conditions, and others felt unsure about referring older adults because of their complex comorbidities. Contrasting advice from specialists meant that there may be a preference to keep patients in primary care. While this approach may avoid anxiety and multiple hospital appointments for patients, there may be missed opportunities to offer specialist education to patients about renal disease and support informed decision making about treatment options.
Guidelines that focus on single conditions are particularly problematic in CKD where so many patients have comorbidities and further advice on managing common comorbidities would be helpful for GPs.24 GPs in the current study made little reference to patient preferences, possibly because they had limited examples of advanced CKD to draw on, however, patient preference was implicit to discussions around choosing management options that were easier for patients. Guidelines that emphasise shared decision making may contribute to patients making informed decisions about their care and help acknowledge decisions based on patient preference.
GPs appreciated input from their local renal units, in the form of local guidelines or educational meetings, and these appeared to have offered clarity on when to refer patients. Reporting systems that highlight patients with CKD whose renal function is declining could play an important role.25 GPs occasionally made decisions about whether patients would be likely to benefit from dialysis and postponed referral or did not refer at all. GPs, often being unaware of current conservative care programmes in renal units, are happy to provide conservative care to renal patients and could be better involved in delivering such care, focused on symptom management and maintaining quality of life. Recent research indicates that forming better relationships between primary care and nephrology services is perceived as a priority need by renal unit staff.13
Acknowledgments
We thank the GPs who volunteered to take part in this study for giving their time, Dr Lynn Josephs, a GP and researcher, for providing comments on this manuscript, and two reviewers for their useful suggestions
Appendix 1. The interview guide used for telephone interviews with GPs
- Managing patients with CKD in practice
- 1. Can you tell me what experience you have in managing patients who have chronic kidney disease? And patients who have kidney failure?
-
2. Can you tell me a little bit about patients with chronic kidney disease stage 5 that you currently look after or that you have looked after most recently?Prompts: age, comorbidities, frequency of consults, presenting complaint.
- 3. For patients with kidney failure, where are they in terms of management? (for example, transplant, on dialysis, likely to be on dialysis in the future, conservative care)
- 4. How often would you/your practice tend to see patients with CKD 5?
- Referring patients with CKD to secondary care
- 5. How would your practice normally identify patients with chronic kidney disease or kidney failure? What is the most common way kidney disease is identified?
- 6. If you identified a patient with new CKD 5 what action(s) would you/your practice routinely take?
- 7. Can you tell me about a time when you told someone they had chronic kidney disease? How did you tell them? What words did you use?
- 8. What questions do patients have about CKD? What do they think of when they are told?
- 9. What proportion of the patients, with CKD 5, on your practice list do you think get referred to secondary care?
- What are the reasons for referral?
- What are the reasons for non-referral?
- Do you have any guidelines about when to refer? National or local?
- 10. How is referral to secondary care discussed with the patient? How is non-referral to secondary care discussed with the patient?
- 11. Do you notify the renal unit about patients who are not being referred? How? What is their reaction?
- 12. If a patient is not referred, how is this recorded in their notes? (for example, secondary care if admitted to hospital).
- Managing patients with CKD 5
- 13. What role do you as a GP play in the management of patients with CKD 5 who are under nephrology?
- 14. Do you have a systematic approach to following up patients with chronic kidney disease?
- 15. What are the components of patient care if they are not under nephrology?
- 16. How do you feel about patients with CKD 5 being referred back to primary care if they opt not to have active treatment/opt for conservative care?
- 17. What agencies/healthcare professions are involved in CKD management/treatment? How were those connections made?
- 18. How are the palliative care needs of patients with CKD 5 addressed?
- 19. Do you have any concerns about managing patients with CKD? Do you think you need any training in managing CKD? Would you like any training?
- 20. What, in an ideal world, would you like to see happen with the management of these patients? What role would GPs play? What are the barriers to achieving this?
Conclusion
21. Are there any other relevant issues we haven’t covered that you would like to mention?
22. Are there any questions you that would like to ask me?
Demographic questions
Sex:
Age:
Years in practice:
Years in current surgery:
Special interests (for example, kidney disease, palliative care, care of the elderly):
Funding
This project was funded by the National Institute of Health Research (NIHR) Health Services and Delivery Research Programme (project number 09/2000/36) and has been published in full in Health Services and Delivery Research.18 Dr Leydon was funded by an NIHR Personal Fellowship Award during the time of this study. This study was sponsored by the University of Southampton. The study sponsor did not have any role in the study design, data collection or analysis, writing of the final manuscript, or the decision to submit this manuscript for publication. This report presents independent research commissioned by the NIHR. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, CCF, NETSCC, the Health Services Research programme or the Department of Health.
Ethical approval
This work was granted ethical approval by the NRES Committee West Midlands – South Birmingham (REC reference: 11/WM/0240).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.National Institute for Health and Care Excellence . Chronic kidney disease: early identification and management of chronic kidney disease in adults in primary and secondary care CG182. London: NICE; 2014. [PubMed] [Google Scholar]
- 2.NHS Employers 2015/16 General Medical Services (GMS) contract Quality and Outcomes Framework (QOF) http://bma.org.uk/practical-support-at-work/contracts/independent-contractors/qof-guidance (accessed 23 Apr 2015).
- 3.Roderick P, Roth M, Mindell J. Prevalence of chronic kidney disease in England: findings from the 2009 Health Survey for England. J Epidemiol Community Health. 2011;65:A12. [Google Scholar]
- 4.Astor BC, Matsushita K, Gansevoort RT, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with mortality and end-stage renal disease. A collaborative meta-analysis of kidney disease population cohorts. Kidney Int. 2011;79(12):1331–1340. doi: 10.1038/ki.2010.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gansevoort RT, Matsushita K, van der Velde M, et al. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int. 2011;80(1):93–104. doi: 10.1038/ki.2010.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smart NA, Titus TT. Outcomes of early versus late nephrology referral in chronic kidney disease: a systematic review. Am J Med. 2011;124(11):1073–1080.e2. doi: 10.1016/j.amjmed.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 7.Jones C, Roderick P, Harris S, Rogerson M. Decline in kidney function before and after nephrology referral and the effect on survival in moderate to advanced chronic kidney disease. Nephrol Dial Transplant. 2006;21(8):2133–2143. doi: 10.1093/ndt/gfl198. [DOI] [PubMed] [Google Scholar]
- 8.The Renal Association . Clinical practice guidelines: planning, initiation and withdrawal of dialysis. 6th edn. Petersfield: Renal Association; 2014. [Google Scholar]
- 9.Tattersall J, Dekker F, Heimbürger O, et al. When to start dialysis: updated guidance following publication of the Initiating Dialysis Early and Late (IDEAL) study. Nephrol Dial Transplant. 2011;26(7):2082–2086. doi: 10.1093/ndt/gfr168. [DOI] [PubMed] [Google Scholar]
- 10.Murtagh FE, Marsh JE, Donohoe P, et al. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol Dial Transplant. 2007;22(7):1955–1962. doi: 10.1093/ndt/gfm153. [DOI] [PubMed] [Google Scholar]
- 11.Da Silva-Gana M, Wellsted D, Greenshields H, et al. Quality of life and survival in patients with advanced kidney failure managed conservatively or by dialysis. Clin J Am Soc Nephrol. 2012;7(12):2002–2009. doi: 10.2215/CJN.01130112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hussain JA, Mooney A, Russon L. Comparison of survival and palliative care involvement in patients aged over 70 years choosing conservative management or renal replacement therapy in advanced chronic kidney disease. Palliat Med. 2013;27(9):829–839. doi: 10.1177/0269216313484380. [DOI] [PubMed] [Google Scholar]
- 13.Okamoto I, Tonkin-Crine S, Rayner HC, et al. Conservative care for end-stage kidney failure in the UK: a national survey. Clin J Am Soc Nephrol. 2015;10(1):120–126. doi: 10.2215/CJN.05000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blakeman T, Protheroe J, Chew-Graham C, et al. Understanding the management of early-stage chronic kidney disease in primary care: a qualitative study. Br J Gen Pract. 2012 doi: 10.3399/bjgp12X636056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crinson I, Gallagher H, Thomas N, de Lusignan S. How ready is general practice to improve quality in chronic kidney disease? A diagnostic analysis. Br J Gen Pract. 2010;60(575):403–409. doi: 10.3399/bjgp10X502100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blakeman T, Harding S, O’Donoghue D. Acute kidney injury in the community: why primary care has an important role. Br J Gen Pract. 2013;63(609):173–174. doi: 10.3399/bjgp13X664207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tonkin-Crine S, Okamoto I, Leydon GM, et al. Understanding by older patients of dialysis and conservative management for chronic kidney failure. Am J Kidney Dis. 2015;65(3):443–450. doi: 10.1053/j.ajkd.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roderick P, Rayner HC, Tonkin-Crine S, et al. A national study of practice patterns in UK renal units in the use of dialysis and conservative kidney management to treat people aged 75 years and over with chronic kidney failure. Health Serv Deliv Res. 2015;3(12) [PubMed] [Google Scholar]
- 19.Castledine C, Gilg J, Rogers C, et al. UK Renal Registry 13th Annual Report (December 2010): Chapter 15: UK renal centre survey results 2010: RRT incidence and use of home dialysis modalities. Nephron Clin Pract. 2011;119(Suppl 2):c255–c267. doi: 10.1159/000331783. [DOI] [PubMed] [Google Scholar]
- 20.Hamberg K, Johansson E, Lindgren G, Westman G. Scientific rigour in qualitative research: examples from a study of women’s health in family practice. Fam Pract. 1994;11(2):176–181. doi: 10.1093/fampra/11.2.176. [DOI] [PubMed] [Google Scholar]
- 21.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 22.Kitzinger J. Qualitative research. Introducing focus groups. BMJ. 1995;311(7000):299–302. doi: 10.1136/bmj.311.7000.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stevens LA, Li S, Wang C, et al. Prevalence of CKD and comorbid illness in elderly patients in the United States: results from the Kidney Early Evaluation Program (KEEP) Am J Kidney Dis. 2010;55(3 Suppl 2):S23–S33. doi: 10.1053/j.ajkd.2009.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reeve J, Blakeman T, Freeman GK, et al. Generalist solutions to complex problems: generating practice-based evidence–the example of managing multimorbidity. BMC Fam Pract. 2013;14:112. doi: 10.1186/1471-2296-14-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kennedy DM, Chatha K, Rayner HC. Laboratory database population surveillance to improve detection of progressive chronic kidney disease. J Ren Care. 2013;39(Suppl 2):23–29. doi: 10.1111/j.1755-6686.2013.12029.x. [DOI] [PubMed] [Google Scholar]