Abstract
A bezoar is a hard, and solid, foreign body located in the gastrointestinal tract that may recur. Bezoar is classified according to its origin. Pharmacobezoars develop in the gastrointestinal tract due to alterations in anatomical structure and/or intestinal motility. In this paper, a case, not yet defined in the literature, of a pharmacobezoar causing a mechanical obstruction that is accompanied by a malignancy in the colon is reported, with the aim of contributing to the literature.
Keywords: Pharmacobezoar, intestine, obstruction
INTRODUCTION
A bezoar is a stiff, solid, and recurrent foreign body that is located in the gastrointestinal tract. They are classified depending on the material of origin. A pharmacobezoar is foreign material that is formed by drugs (1–3). Pharmacobezoar is a very rare condition that may lead to complications (4). Moreover, it rarely results in obstruction. Pharmacobezoars develop in the gastrointestinal tract due to alterations in anatomical structure and/or intestinal motility (5). The diagnosis is usually difficult; therefore, pharmacobezoars are usually diagnosed during an operation or endoscopy. In this paper, a case, not yet defined in the literature, of a pharmacobezoar causing a mechanical obstruction that is accompanied by a malignancy in the colon is reported, with the aim of contributing to the literature.
CASE PRESENTATION
A 73-year-old male patient had complaints of stomach ache and vomiting for the past 2 weeks. His medical history revealed that he received hemodialysis 3 times a week (3/7) for chronic renal failure due to diabetic nephropathy. He had previous diagnoses of insulin-dependent diabetes mellitus and essential hypertension. Furthermore, there was a history of a left radical renal nephrectomy operation, which had been performed due to a left renal mass. To treat his systemic diseases, the patient had been taking nifedipin tab 2 × 30 mg, metildopa tab 4 × 250 mg, pantoprazole tab 1 × 1, telmisartan tab 1 × 1, acetylcysteine 600 effervescent tab 1 × 1, enoxaparin sodium 1 × 40 mg, ipratropium bromide- salbutamol inhaler 3 × 1, eprex epoetin alpha 3000 U 3/7, ascorbic acid amp. 1/7, L - carnitin amp. 1/7, multi vitamins amp. 1/15, calcium acetate tab 3 × 2, sucralfate tab 3 × 1, doxazosin mesylate 4 mg tab 1 × 1, enalapril maleate 10 mg tab 1 × 1, acetylsalisilic acid 100 mg tab 1 × 1, folic acid tab 1 × 1 and gabapentin 100 mg tab 1 × 1.
His physical examination revealed abdominal distension without defense or rebound. His laboratory blood results were as follows: white blood cell (WBC) 21,000/mm3, urea 52 mg/dL, creatinine 3.73 mg/dL, sodium (Na) 137 mmol/L, potassium (K) 4.5 mmol/L, hemoglobin (Hgb) 14.4 g/dL, and platelet (Plt) 419,000/mm3.
The left-nephrectomized patient’s abdominal computed tomography (CT) revealed atrophy in the size of the right kidney, significant dilatation and gas-fluid levels in the intestinal lumen, and dilatation extending from the cecum to the hepatic flexure of the ascending colon (8 cm at the widest area of the cecum) (Figure 1).
Figure 1.
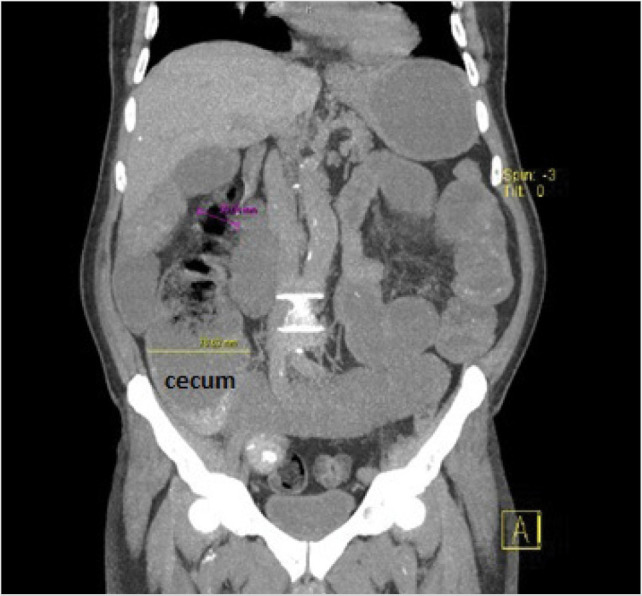
Cecal dilatation, normal segment distal to the obstruction, and intestinal dilatation in the coronary section
Informed consent was obtained from the patient. During the laparotomy, a small amount of ascites was observed, and a 3-cm mass was palpated in the ascending colon near the cecum. Drugs were found proximal to the tumor mass (Figure 2). With exploration, no other additional abdominal pathology was noted. Right hemicolectomy was performed. In the post-operative period, the patient had pneumonia and a wound infection, for which he was treated with suitable antibiotics and wound dressings.
Figure 2.
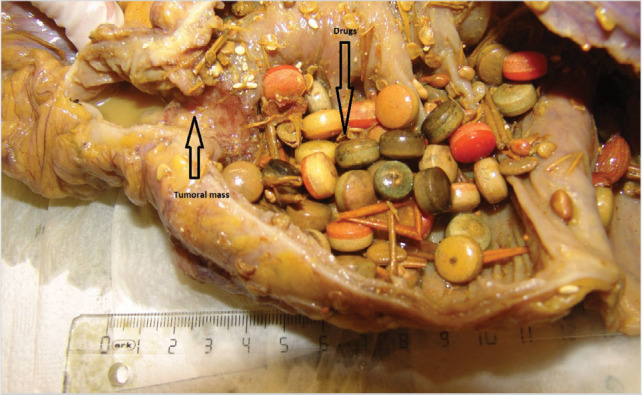
Drugs and tumoral mass that led to obstruction and a proximal pharmacobezoar
The pathology results were as follows: a grade 2 adenocarcinoma of the ascending colon, where 16 pericolic lymph nodes were tumor-negative, and 1 pericolic lymph node that was positive for carcinoma metastasis, and an appendix with normal mucosa. Thus, the tumor grade was reported as being pT4N1. There were no malignant cells in the abdominal fluid.
DISCUSSION
Although bezoars are known to be one of the post-gastrectomy/post-vagotomy complications that cause gastric outlet and intestinal obstruction, there are not enough publications on bezoars. The majority of bezoars is located in the stomach; however, bezoars may be encountered in the whole gastrointestinal tract, including the esophagus and rectum. Four different types of bezoars have been determined in the gastrointestinal tract: 1. phytobezoars (hortobezoars), 2. trichobezoars (pilobezoars, hairball), 3. stone-like foreign bodies in the stomach, and 4. pharmacobezoars (drug-induced). There is not a sufficient number of publications on pharmacobezoars. A search on Pubmed revealed only 26 published articles. The majority of published cases was related to pharmacobezoars that were located in the stomach. We did not come across any publications of pharmacobezoars that coexisted with colon carcinoma.
CONCLUSION
Pharmacobezoars are rarely seen, and their diagnosis is difficult. Suspecting its presence is important for the diagnosis. Pharmacobezoars should be included in the differential diagnosis of older patients who have anatomical and functional diseases of the colon. Moreover, pharmacobezoars should be considered in patients who use a variety of drugs and have clinical symptoms of mechanical intestinal obstruction.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.E.; Design - F.A.; Supervision - M.Ç.; Funding - S.R.; Data Collection and/or Processing - F.A.; Analysis and/or Interpretation - M.Ç.; Literature Review - A.E.; Writer - A.E.; Critical Review - H.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Simpson SE. Pharmacobezoars described and demystified. Clin-Toxicol (Phila) 2011;49:72–89. doi: 10.3109/15563650.2011.559472. http://dx.doi.org/10.3109/15563650.2011.559472. [DOI] [PubMed] [Google Scholar]
- 2.Islek A, Sayar E, Yılmaz A, Boneval C, Artan R. A rare outcome of iron deficiency and pica: Rapunzel syndrome in a 5-year-old child iron deficiency and pica. Turk J Gastroenterol. 2014;25:100–102. doi: 10.5152/tjg.2014.4051. http://dx.doi.org/10.5152/tjg.2014.4051. [DOI] [PubMed] [Google Scholar]
- 3.Kement M, Ozlem N, Colak E, Kesmer S, Gezen C, Vural S. Synergistic effect of multiple predisposing risk factors on the development of bezoars. World J Gastroenterol. 2012;18:960–964. doi: 10.3748/wjg.v18.i9.960. http://dx.doi.org/10.3748/wjg.v18.i9.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor JR, Streetman DS, Castle SS. Medication bezoars: a literature review and report of a case. Ann Pharmacother. 1998;32:940–946. doi: 10.1345/aph.17420. http://dx.doi.org/10.1345/aph.17420. [DOI] [PubMed] [Google Scholar]
- 5.Black T, Philips G, Burbridge R. Pharmacobezoar in a patient on an oral phosphate binder. Gastrointest Endosc. 2013;77:511–512. doi: 10.1016/j.gie.2012.11.002. http://dx.doi.org/10.1016/j.gie.2012.11.002. [DOI] [PubMed] [Google Scholar]


