Abstract
Background
The purpose of this study was to assess actual barriers to blood glucose control in patients with type 2 diabetes mellitus and to investigate barrier-related factors in an exploratory manner.
Methods
This cross-sectional study assessed patients with type 2 diabetes mellitus treated as outpatients at medical institutions within Fukuoka Prefecture, Japan. Barriers to blood glucose control were examined in patients with glycated hemoglobin ≥6.9% using a nine-item questionnaire. Answers were also obtained from physicians in charge of the patients for seven of nine questions.
Results
Seven hundred and thirteen patients answered the questionnaire. Many physicians and patients described barriers that involved difficulty in complying with diet therapy. For six of the seven barriers, patient awareness was lower than physician awareness. Patient-reported lack of concern for diabetes mellitus was more prevalent among patients with macrovascular complications. Patients who reported difficulty in compliance with exercise therapy and fear of hypoglycemia were more likely to suffer from microvascular complications.
Conclusion
For many of the barriers to blood glucose control, patients were less aware than physicians, suggesting that we need to take action to raise patient awareness. Of interest are the observations that the relevant barriers differed for macrovascular and microvascular complications and that the relationship between presence of macrovascular complications and lack of concern about diabetes mellitus.
Keywords: epidemiology, patient education, patient behavior, patient awareness, diabetic complications
Introduction
Drugs with a new mechanism of action, such as the dipeptidyl peptidase-4 inhibitors, glucagon-like peptide-1 receptor agonists, and sodium glucose cotransporter inhibitors, have been introduced and there are now more options for treatment of type 2 diabetes mellitus. The results of clinical studies using these new drugs are being published in rapid succession, and it is foreseeable that the algorithm for drug therapy for diabetes mellitus will become increasingly complex. In 2012, the American Diabetes Association and European Association for Study of Diabetes announced a new consensus statement in response to this issue, emphasizing a patient-centered approach.1 They propose that physicians set target blood glucose values for individual patients and discuss with the patient which therapy should be selected, taking into consideration not only the risk of hypoglycemia, disease duration, age (life expectancy), severity of complications, and the presence/absence of support, but also each patient’s attitude and expected treatment efforts (motivation, adherence, self-care capacity). Following this trend, we anticipate that it will become more important than ever for medical staff to understand the patient’s perspective.
In addition, as diet therapy and exercise therapy are the basis of diabetes therapy, a positive attitude, motivation, and self-management are essential patient attributes;2 it was reported that patient education was useful in achieving control of blood glucose and reducing the incidence of complications.3,4 When there is a barrier to blood glucose control, even optimal therapy proposed by a physician likely will not be carried through by the patient. In J-DOIT2 (the Japan Diabetes Outcome Intervention Trial 2), which tried to reduce the dropout rate from diabetes treatment, the rate was significantly reduced in the treatment-supported (intervention) group in comparison with the normal treatment (control) group (hazard ratio 0.367, P<0.0001).5,6 Concerning the question of how consistent awareness is between patients and physicians, Yoshioka et al reported that there were differences in awareness about insulin therapy (necessity of insulin therapy for the individual patient, limitation of life, and activities related to insulin therapy) between patients and physicians.7
In this study, we investigated the barriers to blood glucose control in patients who did not achieve the goal specified in the guidelines8 in order to elucidate whether there was a difference in awareness between the patient and the physician. We also analyzed the clinical significance of the presence or absence of barriers in an exploratory manner, focusing on their relationship with complications.
Subjects and methods
Study design and subjects
A cross-sectional observational study was conducted from April to September 2007 in outpatients with type 2 diabetes mellitus treated at medical institutions located in Fukuoka Prefecture, Japan. Inclusion criteria were: outpatients; type 2 diabetic patients aged ≥20 years; patients for whom the time of diagnosis of type 2 diabetes mellitus was clear (the year of diagnosis was sufficient); and patients from whom informed consent to participate in this study had been obtained. Among the eligible patients, those with glycated hemoglobin (HbA1c) ≥6.9% were included in the analysis.
Examination
Patient background (age, sex, body mass index, duration of diabetes), HbA1c, therapy, presence or absence of hypertension, dyslipidemia, and complications were assessed. In those patients who did not achieve the goal in terms of blood glucose control (HbA1c <6.9%), barriers to blood glucose control were also examined with a nine-item questionnaire (see Figure 1 for the question items). Answers were also obtained from the physicians in charge of the patients, in order to investigate whether there are differences between patients and physicians regarding awareness of barriers. Two items were answered only by patients since it was considered difficult for physicians to evaluate, ie, “it was difficult to periodically visit the hospital/clinic” and “hypoglycemia was scary”. We selected the most recent HbA1c values within 6 months of the day the patient responded to the questionnaire.
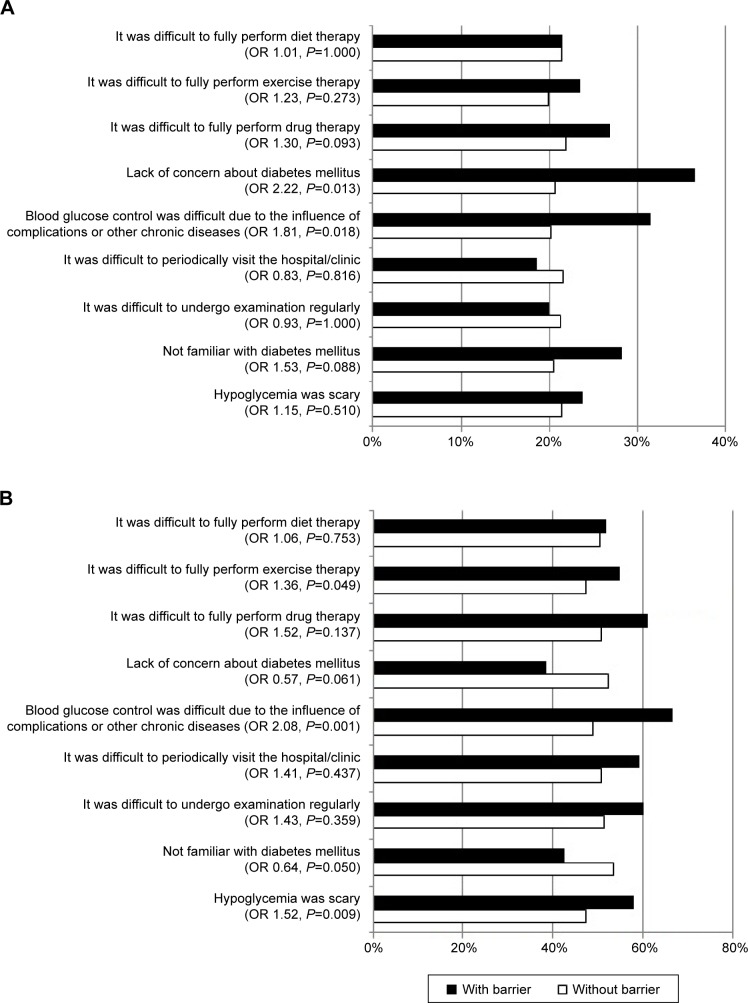
Figure 1.
Prevalence of complications among patients with or without barriers to blood glucose control. (A) Prevalence of macrovascular complications. (B) Prevalence of microvascular complications.
Notes: OR, versus patient group without a barrier. The P-value was calculated with the Fisher’s exact test (two-sided). Macrovascular complication included any one of angina pectoris, myocardial infarction, arteriosclerosis obliterans, or cerebrovascular disease. Microvascular complication included any one of diabetic nephropathy, diabetic retinopathy, or diabetic neuropathy.
Abbreviation: OR, odds ratio.
The presence or absence of hypertension, dyslipidemia, and complications, as determined by common criteria, was not re-evaluated in this study; we simply compiled the diagnoses made by each physician. In a case where angina pectoris, myocardial infarction, arteriosclerosis obliterans, or cerebrovascular disease was diagnosed, “a macrovascular complication” was considered present, and where diabetic nephropathy, diabetic retinopathy, or diabetic neuropathy was diagnosed, “a microvascular complication” was similarly considered present.
Statistical analysis
McNemar’s test was used to compare the differences between patients’ and physicians’ responses. The Student’s t-test and Fisher’s exact test were used to assess the differences in background factors between patients with one or fewer different responses and two or more different responses, when compared with physicians. Exploratory investigations examined how the presence or absence of barriers was related to the presence or absence of complications, and what background factors were associated with the presence or absence of barriers. Fisher’s exact test was used to assess the difference in prevalence of complications (macrovascular, microvascular) between patients with and without barriers. The Student’s t-test and Fisher’s exact test were used to assess the differences in background factors between patients with and without a barrier to blood glucose control related to the presence of complications. Statistical analyses were performed using R version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria). All probability values were two-sided and the significance level was set at P<0.05.
Ethical considerations
This study was conducted in accordance with the Ethical Guidelines for Epidemiological Research (issued by the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labour and Welfare) and the Declaration of Helsinki after approval from the ethics committee of Kyushu University. Written informed consent to inclusion in this study was obtained from all subjects.
Results
Characteristics of subjects
Eleven hundred and two patients with type 2 diabetes were screened from 40 institutions. Seven hundred and thirteen patients with HbA1c ≥6.9% and answers about barriers to blood glucose control obtained from both the patient and the physician were included in the analysis. The proportion of patients with HbA1c ≥6.9% was 67.1% (519/773) in hospitals and 59.0% (194/329) in clinics. Table 1 shows the backgrounds of these subjects.
Table 1.
Subject background factors
| n=713 | |
|---|---|
| Institution (hospital/clinic) | 519/194 |
| Physician’s specialty (Japan Diabetes Society specialist/other) | 417/296 |
| Age (years) | 63.7±10.6 |
| Male/female (%) | 55.9/44.1 |
| BMI (kg/m2) | 24.3±3.9 |
| Diabetes duration (years) | 11.6±8.6 |
| HbA1c(NGSP) (%) | 8.1±1.2 |
| Using hypoglycemic drug (%) | 93.3 |
| Number of oral hypoglycemic drugs | 1.4±1.0 |
| Using insulin (%) | 25.0 |
| Complicated by hypertension (%) | 54.0 |
| Complicated by dyslipidemia (%) | 58.9 |
| Macrovascular complications (%) | 21.5 |
| Presence of angina pectoris (%) | 9.3 |
| Presence of myocardial infarction (%) | 3.6 |
| Presence of arteriosclerosis obliterans (%) | 5.3 |
| Presence of cerebrovascular disease (%) | 9.8 |
| Microvascular complications (%) | 51.5 |
| Presence of diabetic nephropathy (%) | 24.5 |
| Presence of diabetic retinopathy (%) | 31.1 |
| Presence of diabetic neuropathy (%) | 32.4 |
Note: Values are expressed as the mean ± standard deviation (age, BMI, diabetes duration, HbA1c, and number of oral hypoglycemic drugs), number (institution and physician’s specialty), or frequency (other factors).
Abbreviations: BMI, body mass index; HbA1c, glycated hemoglobin; NGSP, National Glycohemoglobin Standardization Program.
The proportions of patients with risks for macrovascular complications were as follows. Of the patients with macro-vascular complications and microvascular complications, 51.6% and 48.5%, respectively, had smoking experience. Of ex-smokers, 64.6% were patients with macrovascular complications and 52.2% were patients with microvascular complications. Hypertension afflicted 73.9% of patients with macrovascular complications and 60.5% of those with microvascular complications. Of patients with macrovascular complications and microvascular complications, 66.7% and 60.8%, respectively, had dyslipidemia.
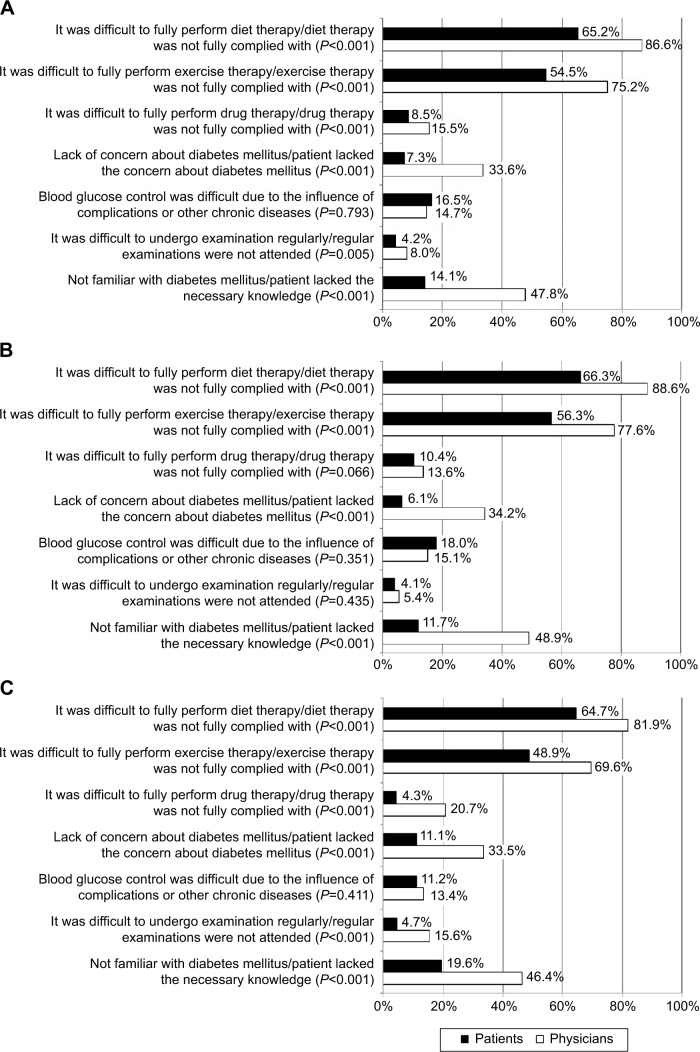
Barriers to blood glucose control
Common answers from physicians regarding barriers to blood glucose control were: diet therapy was not fully complied with (86.6%); exercise therapy was not fully complied with (75.2%); and patients lacked the necessary knowledge (47.8%). Common answers from patients regarding barriers to blood glucose control were: it was difficult to fully comply with diet therapy (65.2%); it was difficult to fully perform exercise therapy (54.5%); and blood glucose control was difficult due to the influence of complications or other chronic diseases (16.5%). Among the seven questions asked of both physicians and patients, there were significant differences (P<0.05) between physicians and patients regarding all questions except “blood glucose control was difficult due to the influence of complications or other chronic diseases”. The patients’ awareness was lower for the other six questions (Figure 2A).
Figure 2.
Barrier to blood glucose control (proportion of responders who said the barrier was present; a comparison between physicians and patients). (A) Total, (B) patients who visited hospitals, and (C) patients who visited clinics.
Note: P-value was calculated with McNemar’s test with the continuity correction.
Subgroup analysis in patients who visited hospitals and clinics was performed (Figure 2B and C). For the following two questions, although a significant difference was not observed between patients who visited hospitals and their physicians, a significant difference was observed between patients who visited clinics and their physicians, ie, it was difficult to achieve medication compliance and it was difficult to undergo examination regularly.
Background factors were compared to determine whether or not there were significant differences in the number of items showing inconsistency between physician’s answers and patient’s answers (≥2 or <2), and there were no significant differences between the two groups (Table 2).
Table 2.
Background factors according to the number of discrepancies in response among physicians and patients
| ≤1 item (n=391) | ≥2 items (n=322) | P-value* | |
|---|---|---|---|
| Age (years) | 64.1±10.1 | 63.2±11.2 | 0.285 |
| Sex: proportion of females (%) | 44.6 | 43.5 | 0.762 |
| BMI (kg/m2) | 24.1±3.8 | 24.6±4.0 | 0.066 |
| Diabetes duration (years) | 11.4±8.3 | 11.9±8.9 | 0.491 |
| HbA1c (NGSP) (%) | 8.0±1.2 | 8.1±1.2 | 0.409 |
| Using hypoglycemic drug (%) | 92.8 | 94.4 | 0.655 |
| Number of oral hypoglycemic drugs | 1.4±1.0 | 1.5±1.0 | 0.397 |
| Using insulin (%) | 23.8 | 26.4 | 0.435 |
| Complicated by hypertension (%) | 57.0 | 50.3 | 0.082 |
| Complicated by dyslipidemia (%) | 58.8 | 59.0 | 1.000 |
| Macrovascular complications (%) | 22.0 | 20.8 | 0.715 |
| Microvascular complications (%) | 48.3 | 55.3 | 0.071 |
Notes: Values are expressed as the mean ± standard deviation (age, BMI, diabetes duration, HbA1c, and number of oral hypoglycemic drugs), or frequency (other factors);
Student’s t-test for continuous variables, Fisher’s exact test (two-sided) for proportions.
Abbreviations: BMI, body mass index; HbA1c, glycated hemoglobin; NGSP, National Glycohemoglobin Standardization Program.
Relationship between barriers and complications/between barriers and background factors
Patients with barriers to blood glucose control are thought to be at risk for development and progression of complications. The odds ratios for complications (macrovascular, microvascular) are shown in Figure 1 stratified by the presence or absence of each barrier as the independent variable. The prevalence of macrovascular complications (21.5% overall) was higher in the patients who answered “yes” to the question related to “lack of concern for diabetes mellitus” or “blood glucose control was difficult due to the influences of complications or other chronic diseases”. The prevalence of microvascular complications (51.5% overall) was higher in patients who answered “yes” to the questions related to “it was difficult to fully perform exercise therapy”, “blood glucose control was difficult due to the influences of complications or other chronic diseases”, or “hypoglycemia was scary.”
Table 3 shows background factors according to the presence or absence of barriers to blood glucose control. The proportion of patients who answered “yes” to the item “it was difficult to fully perform exercise therapy” differed significantly depending on body mass index, use of a hypoglycemic drug, use of insulin, and the presence of hypertension as a complication. The proportion of patients who answered “yes” to the item “lack of concern for diabetes mellitus” was not significantly different depending on background factors. The proportion of patients who answered “yes” to the item “hypoglycemia was scary” was significantly different depending on age, sex, and whether they were using insulin.
Table 3.
Background factors according to the presence or absence of barriers to blood glucose control
| Compliance with exercise therapy
|
Concern for diabetes mellitus
|
Fear of hypoglycemia
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Feasible compliance (n=314) | Difficult compliance (n=373) | P-value* | With concern (n=645) | Without concern (n=52) | P-value* | Absence of fear (n=308) | Presence of fear (n=320) | P-value* | |
| Age (years) | 64.4±11.0 | 63.4±10.2 | 0.222 | 63.5±10.6 | 65.9±11.5 | 0.148 | 62.1±11.1 | 65.4±10.2 | <0.001 |
| Sex: proportion of females (%) | 43.3 | 44.9 | 0.700 | 44.3 | 36.5 | 0.311 | 37.8 | 52.5 | <0.001 |
| BMI (kg/m2) | 23.8±3.5 | 24.8±3.9 | <0.001 | 24.3±3.8 | 24.9±4.2 | 0.330 | 24.4±3.9 | 24.2±3.9 | 0.510 |
| Diabetes duration (years) | 12.0±8.7 | 11.7±8.5 | 0.651 | 11.5±8.4 | 12.9±10.4 | 0.333 | 11.3±8.9 | 12.5±8.6 | 0.075 |
| HbA1c (NGSP) (%) | 8.0±1.1 | 8.1±1.2 | 0.438 | 8.0±1.2 | 8.2±1.1 | 0.384 | 8.2±1.2 | 8.0±1.2 | 0.160 |
| Using hypoglycemic drugs (%) | 90.8 | 95.7 | 0.013 | 93.6 | 88.5 | 0.151 | 92.5 | 94.3 | 0.420 |
| Number of oral hypoglycemic drugs | 1.5±1.0 | 1.4±1.0 | 0.215 | 1.5±1.0 | 1.3±1.0 | 0.394 | 1.5±1.0 | 1.4±1.0 | 0.229 |
| Using insulin (%) | 21.0 | 29.5 | 0.014 | 26.0 | 15.4 | 0.098 | 23.7 | 31.3 | 0.040 |
| Complicated by hypertension (%) | 49.4 | 58.4 | 0.021 | 53.8 | 53.8 | 1.000 | 53.6 | 53.4 | 1.000 |
| Complicated by dyslipidemia (%) | 56.7 | 61.1 | 0.244 | 60.2 | 50.0 | 0.186 | 58.4 | 61.3 | 0.515 |
Notes: Values are expressed as the mean ± standard deviation (age, BMI, diabetes duration, HbA1c, and number of oral hypoglycemic drugs), or frequency (other factors).
Student’s t-test for continuous variables, Fisher’s exact test (two-sided) for proportions.
Abbreviations: BMI, body mass index; HbA1c, glycated hemoglobin; NGSP, National Glycohemoglobin Standardization Program.
Discussion
To analyze the clinical significance of barriers to blood glucose control, we investigated the relationship between barriers and complications. A remarkable finding was that even after the onset of macrovascular complications, some patients reported lack of concern about diabetes mellitus.
In this study, significant differences in awareness were seen between physicians and patients regarding six of the seven items related to barriers to blood glucose control (Figure 2). For all items with a significant difference, the awareness level was lower for patients than for physicians. Since this study was a cross-sectional, it included patients newly diagnosed with type 2 diabetes and patients with a long-term treatment history. Differences in awareness between physicians and patients were also observed in the Diabetes Attitudes, Wishes and Needs Japan study conducted in 148 patients with type 2 diabetes mellitus for whom insulin therapy was recommended. In 13 of 16 questions about insulin therapy asked of patients and physicians, a significant difference was seen, and it was suggested that patients lack knowledge of the significance of insulin therapy and the limitations accompanying insulin therapy.5 In a strategic study to reduce the dropout rate from diabetes treatment (J-DOIT2), the rate was significantly reduced in the treatment-supported (intervention) group in comparison with the normal treatment (control) group.4 This finding also suggests that it would be useful to check the awareness level in patients and educate/instruct them if their awareness was insufficient or there was misunderstanding.
We investigated whether patients with low awareness of barriers to blood glucose control (the patients who provided answers that differed markedly from those of their physicians) can be identified from patient background factors. The background factors were compared between patients for whom the number of items showing inconsistency between physician’s answers and patient’s answers was large (≥2 questions) and those for whom the number was small (≤1 question), but no background factors showed a significant difference (Table 2). It was therefore considered difficult to use background factors to predict whether patients are sufficiently aware of barriers to blood glucose control, and we considered it necessary to check the awareness level of each patient.
We next investigated whether the presence of barriers to blood glucose control was correlated with complications (macrovascular or microvascular). When the odds ratios of macrovascular and microvascular complications were compared in patients with a barrier to blood glucose control, concern about diabetes mellitus tended to be low in patients with macrovascular complications and tended to be high in patients with microvascular complications (Figure 1). Other researchers report similar findings, ie, that the level of awareness of complications in patients with diabetes was higher for microvascular than for macrovascular complications. In a 2008 survey conducted by Boston Scientific Japan K.K. and the Japan Association for Diabetes Education and Care investigating 680 diabetes patients aged ≥40 years who were members of the Japan Association for Diabetes Education and Care, the level of awareness of diabetic complications was 92% for retinopathy, 88% for neuropathy, and 87% for nephropathy, but just 71% for ischemic heart disease and 75% for cerebral infarction; awareness was lower for macrovascular complications as compared with microvascular complications.9 Mori et al reported that when 611 diabetes patients were asked about the organs affected by diabetic complications, the awareness level was 97% for eyes, about 80% for kidneys, and about 67% for nerves, but about 50% for the brain and heart.10
Past concern about diabetes was not investigated in our cross-sectional study; however, we thought that poor blood glucose control had occurred and resulted in complications in patients who were not concerned about their diabetes. On the other hand, some patients became more concerned about diabetes after the onset of complications. In the case of macrovascular complications, comprehensive management is important, including not only blood glucose but also other risk factors, such as smoking, obesity, blood pressure, and lipids. We think that concern about diabetes mellitus tends to increase following microvascular complications, but other risk factors tend to cause concern where macrovascular complications occur. The possibility that the patient group with macrovascular complications was more concerned about these risks was suggested by the data concerning smoking, hypertension, and dyslipidemia in this study. The proportion of ex-smokers among patients with smoking experience was higher by 12.4 points in the patients with macrovascular complications than in the patients with microvascular complications. The prevalence of hypertension was higher by 13.4 points and the prevalence of dyslipidemia was higher by 5.9 points in patients with macrovascular complications than in those with microvascular complications. We did not investigate past body mass index. In six of the seven questionnaire items related to barriers, the awareness level was lower in patients than in physicians, but regarding “influences of complications or other chronic diseases”, the awareness level was slightly higher in the patients (Figure 2A). It is possible that even when the major cause of failure to achieve the goal of blood glucose control was insufficient concern or knowledge related to diabetes mellitus or difficulty in compliance with diet, exercise, or drug therapy, the patients may have considered hypertension or dyslipidemia to be the major cause. Since this study was cross-sectional, a comparison with the state before onset of macrovascular complications was impossible, but it is necessary to pay attention to the fact that insufficient concern or knowledge related to diabetes mellitus was suggested even after onset of macrovascular complications.
Regarding the three barriers that showed a significant relationship with complications (difficulty in compliance with exercise therapy, lack of concern for diabetes mellitus, fear of hypoglycemia), we investigated whether patients with each of these barriers can be predicted from background factors. The background factors were compared by presence or absence of each barrier, but no background factor showed a significant difference in terms of concern for diabetes mellitus, and other items showing a significant difference were different from barrier to barrier, with no common characteristics (Table 3). This study suggests that it is at present difficult to use background factors to predict the presence of barriers to blood glucose control, as recognized by patients; priority should be given to checking whether patients are sufficiently aware of diabetes mellitus and its treatment.
There are some limitations in our study. In order to investigate the barriers in patients with insufficient glycemic control, only patients with insufficient glycemic control were included for analysis in this study. If we modify the expression of questions and question also patients with good glycemic control, further findings may be provided by comparison between patients with insufficient glycemic control versus those with good glycemic control. Although barriers to glycemic control were considered to change with the treatments, we could not show how to change barriers with change of treatments since the study was cross-sectional.
We considered that awareness of importance of glycemic control by patients themselves leads to prevention of diabetic complications. However, the patients might have additional risks other than hyperglycemia. Our results suggest that it is important to raise awareness of glycemic control by patients so that they continue to pay attention to glycemic control even if they care about other risks at the same time.
Conclusion
Patients’ awareness of barriers to blood glucose control were lower than physicians’ awareness for many issues, suggesting that we need to act to raise patient awareness. The presence of different barriers in relation to macrovascular and microvascular complications and the relationship between history of onset of macrovascular complications and a lack of concern about diabetes mellitus warrant further investigation.
Acknowledgments
The authors are grateful to the patients who participated in this study. They are also grateful to the investigators and staff members of each medical institution who contributed to this study, as follows: Dr Fumi Sawada (Ariyoshi Hospital), Dr Shoichi Natori, Dr Takehiko Kodera, Dr Makoto Ide (Iizuka Hospital), Dr Masahiro Matsumoto, Dr Hidehiro Ishii, Dr Tomokazu Hata, Dr Maki Maeda (Kitakyushu Municipal Medical Center), Dr Toyoshi Inoguchi, Dr Kunihisa Kobayashi, Dr Tetsuhide Ito, Dr Hisato Igarashi, Dr Akira Kawabe (Kyushu University Hospital), Dr Shinsuke Hiramatsu (National Hospital Organization Kyushu Medical Center), Dr Makito Tanabe, Dr Ryoko Saito (Kokura National Hospital), Dr Yasuhiro Sako, Dr Naotaka Sekiguchi, Dr Kenji Ashida (Saiseikai Fukuoka General Hospital), Dr Yasuhiro Ono (Takagi Hospital), Dr Hiroko Ino (Nishifukuoka Hospital), Dr Shizu Suzuki, Dr Yuka Matoba (Hakuaikai Hospital), Dr Toshiyo Sonta (Harasanshin Hospital), Dr Yasutaka Maeda (Fukuokaken Saiseikai Futsukaichi Hospital), Dr Fumio Umeda, Dr Kazuo Mimura, Dr Yuji Tajiri, Dr Eiichi Hirata (Fukuoka City Medical Association Hospital), Dr Toshihiko Hashimoto (Fukuoka City Hospital), Dr Koichiro Imamura (Fukuoka Chuo Hospital), Dr Tatsuya Kuroki (Munakata Medical Association Hospital), Dr Masakazu Fujii (Munakata Suikokai General Hospital), Dr Naoichi Sato (Moji Rosai Hospital), Dr Teruaki Yamauchi, Dr Yasuro Akashi, Dr Jun Watanabe (Yukuhashi Central Hospital), Dr Jun Aramaki (Aramaki Clinic), Dr Hiroaki Iwamoto (Iwamoto Clinic), Dr Naoki Nakashima (Emori Clinic), Dr Akira Ohkubo (Ohkubo Medical Clinic), Dr Akira Kawabe (Kawabe Clinic), Dr Makoto Kunisaki (Kunisaki Makoto Clinic), Dr Katsumi Noda (Clinic Tenjinkita), Dr Atsushi Kondo (Kondo Iin), Dr Takashi Sugimura (Sugimura Clinic), Dr Shinsuke Takei (Takei’s Clinic Internal Medicine), Dr Masafumi Tanaka (Tanaka Clinic), Dr Yuji Tsuji (Tsuji Medical Clinic), Dr Satoru Nakate (Nakate Medical Clinic), Dr Itsuro Nakano (Nakano Iin), Dr Kenjiro Narasaki (Narasaki Naika Iin), Dr Ryoko Takei (Hatta Naika Iin), Dr Takashi Eto (PS Clinic), Dr Shuji Sasaki (Hirata Medical Clinic), Dr Takashi Matsuura (Matsuura Iin), Dr Mitsunori Masakado (Yamauchi Naika Clinic), Dr Gentai Lee (Lee Medical Clinic).
Footnotes
Author contributions
Takeo Suzuki was involved in conception and design, and drafting the article. Toyoshi Inoguchi and Ryoichi Takayanagi were involved in conception and design, acquisition of data, and revising the draft article critically for important intellectual content. Ryoko Takei, Noriyuki Sonoda, Shuji Sasaki, and Toshihiko Kaise were involved in revising the draft article critically for important intellectual content. All authors were involved in analysis and interpretation of the data, as well as final approval of the version to be published.
Disclosure
This study was conducted using the contract research fund of GlaxoSmithKline K.K. Takeo Suzuki and Toshihiko Kaise are employees of GlaxoSmithKline K.K. Ryoko Takei, Toyoshi Inoguchi, Noriyuki Sonoda, Shuji Sasaki, and Ryoichi Takayanagi were contracted as investigators for this study. The findings and conclusion in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes mellitus: a patient-centered approach. Position statement of the American Diabetes mellitus Association (ADA) and the European Association for the Study of Diabetes mellitus (EASD) Diabetes Care. 2012;35:1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arakawa S, Watanabe T, Sone H, et al. The factors that affect exercise therapy for patients with type 2 diabetes in Japan: a nationwide survey. Diabetol Int. 2015;6:19–25. [Google Scholar]
- 3.Minet L, Møller S, Vach W, Wagner L, Henriksen JE. Mediating the effect of self-care management intervention in type 2 diabetes mellitus: a meta-analysis of 47 randomised controlled trials. Patient Educ Couns. 2010;80:29–41. doi: 10.1016/j.pec.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 4.Rachmani R, Levi Z, Slavachevski I, Avin M, Ravid M. Teaching patients to monitor their risk factors retards the progression of vascular complications in high-risk patients with type 2 diabetes mellitus – a randomized prospective study. Diabet Med. 2002;19:385–392. doi: 10.1046/j.1464-5491.2002.00701.x. [DOI] [PubMed] [Google Scholar]
- 5.Izumi K, Hayashino Y, Yamazaki K, et al. Multifaceted intervention to promote the regular visiting of patients with diabetes to primary care physicians: rationale, design and conduct of a cluster-randomized controlled trial. The Japan Diabetes Outcome Intervention Trial-2 study protocol. Diabetol Int. 2010;1:83–89. [Google Scholar]
- 6.Ministry of Health, Labour and Welfare Grants System Japanese. The Japan Diabetes Outcome Intervention Trial. [Accessed February 20, 2015]. Available from: http://mhlw-grants.niph.go.jp/niph/search/NIDD00.do?resrchNum=201222025B.
- 7.Yoshioka N, Ishii H, Tajima N, Iwamoto Y, the DAWN Japan group Differences in physician and patient perceptions about insulin therapy for management of type 2 diabetes mellitus: the DAWN Japan study. Curr Med Res Opin. 2014;30:177–183. doi: 10.1185/03007995.2013.855187. [DOI] [PubMed] [Google Scholar]
- 8.The Japan Diabetes Society . Evidence-based Practice Guideline for the Treatment for Diabetes in Japan 2007. 2nd. Tokyo, Japan: Nankodo; 2007. Japanese. [Google Scholar]
- 9.Japan Association for Diabetes Education and Care Japanese. The awareness survey on risks of complications in diabetes. [Accessed February 20, 2015]. Available from: http://www.nittokyo.or.jp/chousakenkyu_10004.html.
- 10.Mori A, Shiomi K, Kouno H, et al. About complications awareness in diabetic outpatients. J Jpn Diabetes Soc. 2011;54(Suppl 1):S–S265. Japanese. [Google Scholar]