In this issue of EBioMedicine, Premer et al. report their study titled “Allogeneic Mesenchymal Stem Cells Restore Endothelial Function in Heart Failure by Stimulating Endothelial Progenitor Cells” (Premer et al., 2015). They recruited a cohort of heart failure patients from two ongoing clinical trials evaluating both autologous and allogeneic mesenchymal stem cell therapies and evaluated both molecular and functional markers of endothelial progenitor cell activity, showing significantly different outcomes between the allogeneic MSC recipients and the autologous MSC recipients. Mechanistically, Premer et al. show that MSCs can improve flow mediated vasodilation in their cohorts of patient while reducing the circulating VEGF to normal levels and increasing circulating endothelial progenitors.
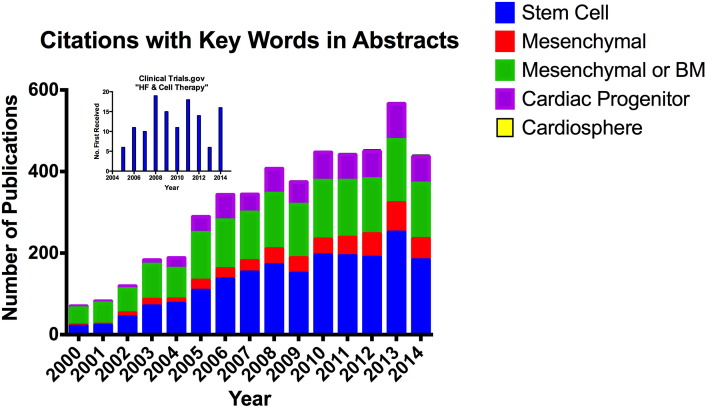
Mesenchymal Stem Cells (MSCs) were first reported by Friedenstein et al. in 1970 (Friedenstein et al., 1970). The finding that these cells could be induced to undergo cardiomyogenesis (Li et al., 2007, Xu et al., 2004) stimulated great excitement regarding their cardiac regenerative capacity as a treatment for ischemic cardiomyopathy, and more recently for dilated cardiomyopathy. In fact, it could be argued that these discoveries catalyzed the proliferation of reports exploring the benefits of cell therapies, in-vitro, in animal models of heart failure and in clinical trials. This effect on the biomedical community can be illustrated by Fig. 1, which shows results from PubMed and Grants.gov searches several key words. While these searches are not exhaustive, it clearly shows that we have experienced a rapid growing interest in the potential of stem cells to 1.) improve clinical outcomes for heart failure patients, 2.) improve cardiac performance and reverse cardiac remodeling in these patients and 3.) regenerate lost myocardium, especially cardiomyocytes. Our ability to show each of these effects is relatively diverse. While testing for improved clinical outcomes with quality of life, imaging and hemodynamic endpoints is relatively straightforward, the degree of cardiac regeneration has been very challenging and inconsistent. Furthermore, the optimistic outcomes reported in pre-clinical studies have not been realized in clinical trials. This is partially due to the undetermined mechanism of action at the molecular, cellular and organ levels. As we have progressed through the first decade and a half of MCS cell therapy studies, their safety has been clearly demonstrated and the use of allogeneic vs autologous sources are being explored in detail (Karantalis et al., 2015). It is becoming increasingly clear that several progenitor cell types including MSCs re-vascularize the damage heart muscle. In addition, the emphasis on the potential paracrine effects of MSCs in the heart (Williams and Hare, 2011, Centola et al., 2008, Champion and Hare, 2001) is emerging as a likely mode of action. From the more classical viewpoint, this involves cellular (such as MSCs) release of factors, including small proteins and growth factors, to either neighboring or remote cell types. These factors can be ligands of key receptor tyrosine kinases including vascular endothelial growth factor (VEGF) that bind to cell surface receptors such as VEGF receptors on endothelial cells.
Fig. 1.
PubMed Citations using “heart failure” and either “stem cell”, “mesenchymal”, “mesenchymal or bone marrow”, “cardiac progenitor”, or “cardiosphere”. Inset: citations in Clinical Trials.gov using “heart failure” and “cell therapy”.
The cohort of patients in this study was recruited from the TRansendocardial Stem Cell Injection Delivery Effects on Neomyogenesis STudy (TRIDENT) in ischemic cardiomyopathy patients as well as the PercutaneOus StEm Cell Injection Delivery Effects on Neomyogenesis in Dilated CardioMyopathy (POSEIDON-DM) study. While data are available from the POSEIDON-PILOT study (Hare et al., 2012) evaluating a cohort of patients with ischemic cardiomyopathy, the POSEIDON-DCM and TRIDENT study results are not yet available. In the POSEIDON-PILOT study, no significantly different outcomes were noted between allogenic and autologous MSC recipients. It should be noted that there was no placebo control in the POSEIDON-PILOT study, so efficacy cannot be rigorously tested.
MSCs have been reported to be immunoprivileged and immunosuppressive, because they do not express major histocompatibility class II antigens and they secrete T helper type 2 cytokines (Hare et al., 2012). Therefore, the potential benefits of allogenic cell include use as an “off-the-shelf” therapeutic, thus avoiding the necessity for additional procedures for patients and delays in therapy. In addition, cell quality and selection could be much more highly controlled. There are also some concerns that autologous MSCs could be impaired in patients with comorbidities or advanced age.
On a functional level, the percent flow mediated brachial artery vasodilation was impaired in HF patients relative to healthy controls. It should be noted that the healthy controls are younger than the patient cohorts, but the implications of this difference is not clear. At the cellular level, EPC-colony forming units (EPC-CFUs) isolated from peripheral blood were markedly reduced in HF patients compared to the healthy controls. At the molecular level, patients had elevated circulating (VEGF). Thus, based on these results, it was concluded that the heart failure patients suffered from endothelial dysfunction.
In order to understand the potential impact of MSCs to endothelial function, cultured medium from both autologous and allogeneic MSC cultures were introduced to HUVEC cultured with vasculogenesis inhibitors to evaluate the role of the MSC secretome in repair of endothelial dysfunction. The outcomes from these studies suggest that in contrast to autologous MSCs, allogeneic MSC culture medium contained factors that overcame the inhibitory effects and could restore endothelial progenitor cell function and vasculogenesis.
Functional, cellular and molecular parameters in the patient population were compared at baseline and three months post-treatment. The allogeneic MSC recipient endpoints improved while autologous MSC recipients did not. These outcomes included flow mediated vasodilation, increased propensity of circulating endothelial progenitors to form colonies, in-vitro, and MSC mediated decreased circulating VEGF.
Perhaps most convincing, are the correlations between functional, cellular and molecular endpoints. Namely, there is a strong correlation between increases in FMD% or decreases in VEGF with concomitant increases in EPC-CFUs.
Based on the results in this paper, it was concluded that allogeneic MSCs resulted in more optimistic outcomes for patients with DCM and ICM partially resulting from corrected endothelial function. There appears to be MSC produced soluble mediators that may be released into the extracellular matrix which correct the endothelial progenitor dysfunction, comorbidity in the cohort of patients studied. Since VEGF stimulates endothelial repair, it is somewhat surprising that allogenic MSCs drive the circulating VEGF level in these patients down, which results in improved vasculogenesis, and is inversely related to the population of circulating endothelial progenitors and with FMD. Therefore there is a need for further study to determine the exact cellular and molecular basis by which MSCs exert these effects via their secretome. There are some limitations that could be addressed in subsequent studies focusing on determining how the MSC secretome impacts endothelial progenitor dysfunction in heart failure patient. In order to unequivocally demonstrate that allogeneic MSC therapy has a positive effect on endothelial progenitor cell dysfunction in heart failure patients, a double-blinded study that includes placebo controls is necessary. In addition, there should be complete profiling of the allogeneic MSCs used in these studies, and they should be from individual as opposed to pooled sources to demonstrate how general this effect is as well as its clinical significance. In addition, while the parent clinical trials are still ongoing, it will be important to correlate the molecular, cellular and functional outcomes reported by Premer et al. to cardiac function and quality of life endpoints. Finally, while extremely challenging, understanding the fate of delivered MSCs is critically important to understanding their clinical value.
Acknowledgments
This work is supported by NIH RO1 HL083156, HL080498, HL093183, and P20HL100396 (R. J. H.) & a Leducq Transatlantic Foundation grant (R.J.H. & K.M.F.)
References
- Centola M., Schuleri K.H., Lardo A.C., Hare J.M. Stem cell therapy for myocardial regeneration: mechanisms and current clinical applications. G. Ital. Cardiol. (Rome) 2008;9(4):234–250. (PubMed PMID: 18543793) [PubMed] [Google Scholar]
- Champion H.C., Hare J.M. Emerging therapeutic targets in nitric oxide-dependent cardiac disease. Expert Opin. Ther. Targets. 2001;5(5):547–556. doi: 10.1517/14728222.5.5.547. (PubMed PMID: 12540282) [DOI] [PubMed] [Google Scholar]
- Friedenstein A.J., Chailakhjan R.K., Lalykina K.S. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 1970;3(4):393–403. doi: 10.1111/j.1365-2184.1970.tb00347.x. (PubMed PMID: 5523063) [DOI] [PubMed] [Google Scholar]
- Hare J.M., Fishman J.E., Gerstenblith G., DiFede Velazquez D.L., Zambrano J.P., Suncion V.Y., Tracy M., Ghersin E., Johnston P.V., Brinker J.A., Breton E., Davis-Sproul J., Schulman I.H., Byrnes J., Mendizabal A.M., Lowery M.H., Rouy D., Altman P., Wong Po Foo C., Ruiz P., Amador A., Da Silva J., McNiece I.K., Heldman A.W., George R., Lardo A. Comparison of allogeneic vs autologous bone marrow-derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. JAMA. 2012;308(22):2369–2379. doi: 10.1001/jama.2012.25321. (PubMed PMID: 23117550) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karantalis V., Schulman I.H., Balkan W., Hare J.M. Allogeneic cell therapy: a new paradigm in therapeutics. Circ. Res. 2015;116(1):12–15. doi: 10.1161/CIRCRESAHA.114.305495. (PubMed PMID: 25552688) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Yu X., Lin Q., Deng C., Shan Z., Yang M., Lin S. Bone marrow mesenchymal stem cells differentiate into functional cardiac phenotypes by cardiac microenvironment. J. Mol. Cell. Cardiol. 2007;42(2):295–303. doi: 10.1016/j.yjmcc.2006.07.002. (PubMed PMID: 16919679) [DOI] [PubMed] [Google Scholar]
- Premer C., Blum A., Bellio M.A., Schulman I.H., Hurwitz B.E., Parker M., Dermarkarian C.R., DiFede D.L., Balkan W., Khan A., Hare J.M. Allogeneic mesenchymal stem cells restore endothelial function in heart failure by stimulating endothelial progenitor cells. EBioMedicine. 2015;2(5):467–475. doi: 10.1016/j.ebiom.2015.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams A.R., Hare J.M. Mesenchymal stem cells: biology, pathophysiology, translational findings, and therapeutic implications for cardiac disease. Circ. Res. 2011;109(8):923–940. doi: 10.1161/CIRCRESAHA.111.243147. (PubMed PMID: 21960725; PMCID: 3604746) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu M., Wani M., Dai Y.S., Wang J., Yan M., Ayub A., Ashraf M. Differentiation of bone marrow stromal cells into the cardiac phenotype requires intercellular communication with myocytes. Circulation. 2004;110(17):2658–2665. doi: 10.1161/01.CIR.0000145609.20435.36. (PubMed PMID: 15492307) [DOI] [PubMed] [Google Scholar]