Abstract
Objectives
To examine the association between six-minute walk test (6 MWT) performance and all-cause mortality, coronary heart disease mortality, and incident coronary heart disease in older adults.
Methods
We conducted a time-to-event analysis of 1,665 Cardiovascular Health Study participants with a 6 MWT and without prevalent cardiovascular disease.
Results
During a mean follow-up of 8 years, there were 305 incident coronary heart disease events, 504 deaths of which 100 were coronary heart disease-related deaths. The 6 MWT performance in the shortest two distance quintiles was associated with increased risk of all-cause mortality (290-338 meters: HR 1.7; 95% CI, 1.2-2.5; <290 meters: HR 2.1; 95% CI, 1.4-3.0). The adjusted risk of coronary heart disease mortality incident events among those with a 6 MWT <290 meters was not significant.
Discussion
Performance on the 6 MWT is independently associated with all-cause mortality and is of prognostic utility in community-dwelling older adults.
Keywords: exercise, mortality, physical function, geriatrics
Introduction
Exercise capacity has been shown to predict cardiovascular events and all-cause mortality in adult populations (Blair et al., 1996; Goraya et al., 2000; Gulati et al., 2003; Kokkinos et al., 2008; Messinger-Rapport, Pothier Snader, Blackstone, Yu, & Lauer, 2003; Mora et al., 2003; Myers et al, 2002; Spin et al., 2002; Sui, Laditka, Hardin, & Blair, 2007). Treadmill-based and walk-based testing represent alternate methods for the assessment of functional exercise capacity (Fleg et al., 2000). While exercise treadmill testing has been the most commonly applied method, older adults encounter greater limitations in their ability to execute a treadmill-based test (Gill, DiPietro, & Krumholz, 2000). A walk-based method may serve as a better reflection of daily activities and more practical for assessing functional capacity in older adults (Greig, Butler, Skelton, Mahmud, & Young, 1993; Hollenberg, Ngo, Turner, & Tager, 1998; Peeters & Mets, 1996).
The 6 MWT is a simple, safe, and easily administered test which has been studied in various disease-specific populations, including individuals with pulmonary disease, heart failure, pacemakers, peripheral arterial disease, and organ transplant candidates (Bernstein et al., 1994; Bittner et al., 1993; Cahalin, Pappagianopoulos, Prevost, Wain, & Ginns, 1995; Cahalin, Mathier, Semigran, Dec, & DiSalvo, 1996; Langenfeld, 1990; Milligan, Havey, & Dossa, 1997; Montgomery & Gardner, 1998; Wijkstra et al., 1994). Among older adults the 6 MWT has been shown to be a reliable and valid measure of functional capacity (Rikli & Jones, 1998).
While the 6-Minute Walk test (6 MWT) performance has been shown to be of prognostic significance in various disease-specific patient populations, the information on the association between the 6 MWT and health outcomes among community-dwelling older adults is limited. We investigated the association between the 6 MWT performance and all-cause mortality, coronary heart disease-specific mortality, and incident coronary heart disease among community-dwelling older adults.
Methods
Population
Cardiovascular Health Study (CHS) is an observational study with the primary goal of determining the risk factors for and consequences of cardiovascular disease in older adults. The design and methods of CHS have been previously described (Fried et al., 1991; Tell et al., 1993). Briefly, 5,888 community-dwelling older adults were recruited, including an original cohort of 5,201 participants recruited in 1989-1990 and an additional 687 predominantly African-American cohort recruited between years 1992-1993. Recruitment was from a random sample of the Health Care Finance Administration Medicare eligibility lists in 4 U.S. communities: Forsyth County, North Carolina; Sacramento County, California; Washington County, Maryland; and Pittsburgh (Allegheny County), Pennsylvania. Annual clinic visits and semi-annual telephone and clinic contacts included risk factors, measures of subclinical cardiovascular disease, cognitive and physical function. Of the 4,708 participants who remained enrolled in CHS between June 1996 and May 1997, 1,377 had a phone or proxy interview and did not have an in-person study visit. Among the 3,331 With an in-person study visit, there were 2,116 participants who completed, 163 partially completed, and 1,052 were either exclude due to the criteria listed below (n=764), or did not attempt the 6 MWT by either refusing testing (n=39), stating physical inability (n=34), lacking sufficient time (n=2), at technician discretion (n=28), or providing other reasons (n=30), while the remaining did not participate in the 6 MWT for unknown reason (n=155). Exclusion of participants with prevalent cardiovascular disease (n=614) from the 2,279 who had either completed or partially completed the 6 MWT resulted in 1,665 included in the current analysis.
Six Minute Walk Test
The 6 MWT was conducted between June 1996 and May 1997 according to a standard protocol (American Thoracic Society, 2002). Briefly, in a 100 foot section of an internal hallway with distance marked every five feet by colored tape along the baseboard, participants were instructed to walk at their own pace up and down the hallway while attempting to cover as much ground as possible. Technicians encouraged the participants with the standardized statements. Participants were allowed to stop and rest during the test, but were instructed to resume walking as soon as they could. If a participant stopped and refused to continue the test before the six minutes had elapsed, the distance walked was recorded and the walk was coded as a partial test. The technician used a mechanical lap counter to count the number of laps completed, and an electronic timer with a buzzer that sounded the completion of the 6 minutes. Due to safety concerns, participants were excluded from the 6 MWT due to presence of acute cardiac condition on the pre-test electrocardiogram (ECG), use of ambulatory aids, presence of severe aortic stenosis (<50 mm Hg gradient on echocardiogram), heart rate less than 50 beats per minute or greater than 110 beats per minute, systolic blood pressure greater than 200 mm Hg or diastolic blood pressure greater than 110 mm Hg, or a myocardial infarction or revascularization in the previous 3 months, new or worsening chest pain, dyspnea, or fainting in the past 8 weeks, a resting oxygen saturation less than 90%, or at the discretion of the technician.
Potential Confounders
The CHS examinations were extensive including risk factors and potential confounding or mediating variables of age, sex, race, cigarette smoking status (current vs. former or never), education level (less than high school vs. more than high school), history of treated hypertension or diabetes, body mass index (kilograms per meters2), systolic blood pressure (mm Hg), C-Reactive Protein (mg/dL), total cholesterol (mg/dL), and fasting glucose (mg/dL). Cognitive function was assessed with the Mini-Mental Status Exam (Folstein, Folstein, & McHugh, 1975) and depressive symptoms using the Center for Epidemiological Studies Depression (CES-D) score (Orme, Reis, & Herz, 1986). Limitations in the Activities of Daily Living (ADL) or Instrumental Activities of Daily Living (IADL), self-reported general health status (fair or poor vs. good, very good, or excellent health) were assessed. Major ECG abnormalities included ventricular conduction defects, major Q or QS abnormalities, minor Q or QS with ST-T-wave abnormalities, left ventricular hypertrophy, isolated major ST-T-wave abnormalities, atrial fibrillation, or first degree atrioventricular block were determined by a centralized ECG Reading Center according to a standard protocol (Blackburn, 1969). The ankle arm index (AAI) was measured by trained technicians according to a standard protocol (Newman et al., 1993). Chronic pulmonary disease was defined as a history of chronic bronchitis, emphysema, or asthma. Arthritis of the knees or hips was assessed by self-report. At study entry, participants were classified as having prevalent cardiovascular disease if they had a clinical history of coronary heart disease, congestive heart failure, stroke, transient ischemic attack, and peripheral artery disease which were ascertained using methods previously described (Psaty et al., 1995). Coronary heart disease was defined as the presence of myocardial infarction, angina, coronary artery bypass grafting, or angioplasty. Prevalent coronary heart and cardiovascular diseases were defined as those present at the time of 6 MWT from 1996 to 1997.
Outcomes
The method used by CHS for surveillance and ascertainment of mortality and cardiovascular events have been published elsewhere (Ives et al., 1995). An incident coronary heart disease was defined as a myocardial infarction, angina, or coronary revascularization event among participants free of prevalent CHD at time of the 6 MWT. Incident cardiovascular disease was defined as incident coronary heart disease, congestive heart failure, stroke, or any atherosclerotic event. Mortality was documented by death certificates, inpatient records, nursing home or hospice records, physician questionnaires, and autopsy reports. A coronary heart disease-specific mortality was defined to include death from coronary heart disease and sudden death. Deaths and cardiovascular events were adjudicated by a CHS committee using a standardized protocol.
Statistical Analysis
Differences in covariates were tested using Analysis of Variance, Kruskal Wallis, or Chi Squared tests. The 6 MWT distance was categorized into quintiles of > 414 meters, 373 to 414 meters, 338 to 373 meters, 290 to 338 meters, and 0 to 290 meters. The longest distance quintile (>414 meters) served as the referent group. Crude event rates were calculated and reported per 1000 person-years. Cox proportional hazard regression was used to estimate hazard ratios (HR) and event rates (per 1,000 person-years). Kaplan-Meier analysis was used to evaluate differences in study endpoints between the 6 MWT distance quintiles. Multivariable models included controls for age and sex, and subsequently for other covariates. In order to evaluate discrimination and improvement imparted by 6 MWT, we compared the adjusted model without 6 MWT (Model A) to adjusted model with the 6 MWT (Model B). Discrimination, the ability of two Models to distinguish participants who develop a study endpoint from those who do not, was evaluated Harrell's C statistic. We calculated category-free Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI) to evaluate the improvement imparted by the addition of 6 MWT to Model A. All reported P-values are based on a two-sided test with P(value <0.05 considered statistically significant. Statistical analysis was performed using STATA MP 11.1 (StataCorp, College Station, Texas).
Results
There were 1,665 participants without prevalent cardiovascular disease among the 2,279 who attempted a 6 MWT with a mean age 77 years. The participants were predominantly women (65%) and less likely to be of nonwhite race (15%). The mean 6 MWT distance was 349 meters. As displayed on Table 1, participants with longer 6 MWT distance performance had a more favorable characteristic profile such as a younger age, lower body mass index, less likely to have limitations in IADL and ADLs, or to have arthritis of knees or hips.
Table 1.
Characteristics by Distance Quintiles (range in parentheses) of Six Minute Walk Test Performance(meters) among participants without prevalent Cardiovascular disease
| Characteristics | (>414) (n=333) | (373-414) (n=332) | (338-373) (n=334) | (290-338) (n=327) | (0-290) (n=339) | P Value |
|---|---|---|---|---|---|---|
| Age, yr | 76.2±3.4 | 76.6±3.8 | 77.1±4.2 | 77.7±4.2 | 78.7±5.0 | <.001 |
| Male | 160(48.1) | 128(38.6) | 116(34.7) | 97(29.7) | 83(24.5) | <.001 |
| Non-white | 24(7.2) | 40(12.1) | 59(17.7) | 57(17.4) | 73(21.5) | <.001 |
| Education | 37(11.1) | 62(18.7) | 79(23.7) | 80(24.5) | 102(30.0) | <.001 |
| BMI, kg/m2 | 25.7±3.4 | 26.4±3.8 | 26.7±3.8 | 27.5±4.6 | 27.7±5.4 | <.001 |
| SBP | 133±18 | 136±18 | 136±19 | 137±19 | 139±22 | .01 |
| Diabetes | 20(6.0) | 41(12.4) | 35(10.5) | 33(10.1) | 50(14.8) | .006 |
| Arthritis | 69(22.0) | 61(19.6) | 79(24.7) | 118(37.6) | 125(37.9) | <.001 |
| Pulmonary disease | 41(12.8) | 29(9.0) | 27(8.3) | 47(15.0) | 58(17.8) | .001 |
| ADL limitation | 16 (4.8) | 27(8.1) | 28(8.5) | 40(12.3) | 62(18.9) | <.001 |
| IADL limitation | 34(10.2) | 51(15.4) | 61(18.3) | 101(31.0) | 122(36.0) | <.001 |
| Current Smoking | 13(3.9) | 17(5.2) | 30(9.0) | 22(6.9) | 30(9.2) | .027 |
| Fair/Poor Health | 12(3.6) | 21(6.4) | 37(11.1) | 44(13.6) | 63(18.8) | <.001 |
| CES-Depression | 4.2±4.0 | 4.6±4.1 | 5.1±4.2 | 5.3±4.5 | 5.9±4.5 | .05 |
| Mini-MMSE | 96.0±4.9 | 94.1±6.8 | 93.4±7.0 | 92.5±7.8 | 90.8±9.0 | <.001 |
| Major ECG | 67(20.2) | 65(19.8) | 74(22.8) | 77(23.8) | 92(27.4) | .13 |
| AAI (< 1.0) | 16(5.0) | 23(7.1) | 31(9.8) | 49(16.1) | 76(23.5) | <.001 |
| Chol, mg/dL | 198±36.6 | 203±38.2 | 205±37.5 | 207±36.2 | 205±42.0 | .04 |
| Glucose, mg/dL | 99±23.3 | 102±25.8 | 103±26.6 | 103±24.8 | 104±25.6 | .17 |
| C-RP | 1.5(.8,3.3) | 2.1(1.1,2.1) | 2.4(1.2,5.5) | 2.7(1.3,6.0) | 2.9(1.3,5.7) | <.001 |
| Medication Use | ||||||
| Aspirin | 12(3.6) | 13(3.9) | 14(4.2) | 15(4.6) | 15(4.2) | .97 |
| anti-HTN | 125(37.5) | 140(42.2) | 154(46.1) | 152(46.5) | 192(56.6) | <.001 |
| Lipid Lowering | 29(8.7) | 24(7.2) | 32(9.6) | 27(8.3) | 30(8.9) | .86 |
* Presented as mean ± SD or n(%).
Abbreviations: 6 MWT refers to 6 Minute Walk Test; yr, year; Education, Less than high school; BMI, Body Mass Index; SBP, systolic blood pressure; ADL, activities of daily living; IADL, independent activities of daily living; MMSE, Mini-Mental Status Exam; ECG Abn, electrocardiogram abnormality; AAI, ankle arm index; Chol, Total Cholesterol; Glucose, Fasting Glucose; C-RP, C-Reactive Protein; anti-HTN, antihypertensive medication.
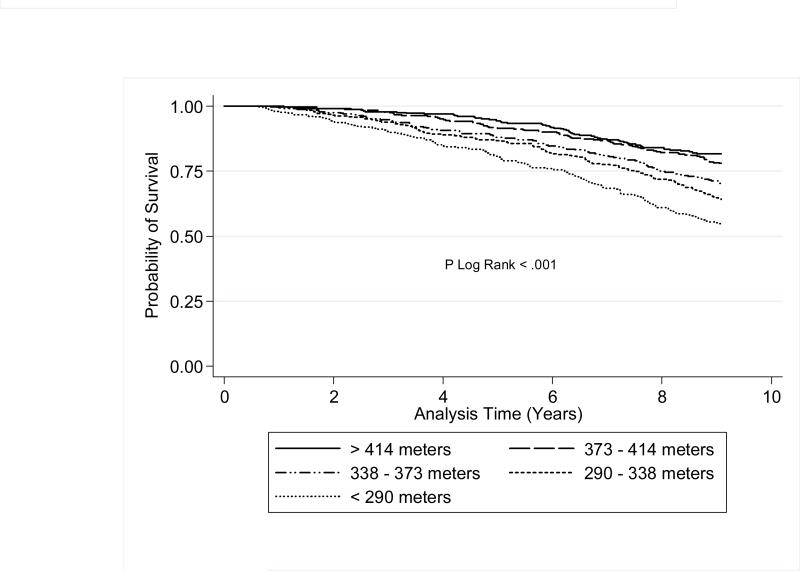
6 MWT Distance and Mortality
There were 504 deaths among the 1,665 of the 2,279 participants without prevalent cardiovascular disease who attempted a 6 MWT (TABLE 2). Figure 1 shows the all-cause mortality Kaplan-Meier Survival curve by 6 MWT distance quintiles. Among the participants with a 6 MWT, a distance in the two shortest distance quintiles (walk distance 290-338 meters and <290 meters) was associated with an increased risk of all-cause mortality relative to a 6 MWT distance >414 meters. The increased risk of all-cause mortality remained in age and sex-adjusted models. In a fully adjusted model, a 6 MWT distance in the shortest two performance quintiles remained associated with an increased risk of all-cause mortality. The adjusted risk of all-cause mortality was progressively higher with decreasing 6 MWT distance. Age- and sex-stratified analyses revealed a similar inverse association between 6 MWT performance and all-cause mortality (TABLE 3). Both older aged men and women who walked less than 338 meters were at increased risk of all-cause mortality. The association between 6 MWT distance and mortality differed between white and non-white participants, with a significant association only observed among the white participants. Due to the small sample size of non-white participants with a 6 MWT the lack of association in non-white participants should be interpreted with caution.
Table 2.
Association between Six Minute Walk Test Distance and Mortality among participants without prevalent Cardiovascular Disease
| Event | Events n (Rate†) | Unadjusted Model | Age- and Sex-Adjusted | Multivariable Adjustment* |
|---|---|---|---|---|
| Hazard Ratio(95% CI) | ||||
| All-Cause Mortality(n=504) | ||||
| >414 | 61(22) | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) |
| 373-414 | 73(26) | 1.2(0.9-1.7) | 1.2(0.9-1.7) | 1.1(0.8-1.7) |
| 338-373 | 99(37) | 1.7(1.3-2.4) | 1.7(1.2-2.4) | 1.4(0.9-2.0) |
| 290-338 | 117(46) | 2.2(1.6-3.0) | 2.1(1.5-2.9) | 1.7(1.2-2.5) |
| 0-290 | 154(62) | 3.0(2.2-4.1) | 2.7(2.0-3.7) | 2.1(1.4-3.0) |
| CVD Mortality(n=160) | ||||
| >414 | 22(8) | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) |
| 373-414 | 17(6) | 0.8(0.4-1.5) | 0.8(0.4-1.5) | 0.7(0.4-1.5) |
| 338-373 | 33(12) | 1.6(0.9-2.8) | 1.5(0.9-2.6) | 0.9(0.5-1.8) |
| 290-338 | 40(16) | 2.0(1.2-3.4) | 1.9(1.1-3.2) | 1.5(0.8-2.8) |
| 0-290 | 48(19) | 2.6(1.6-4.3) | 2.1(1.2-3.5) | 1.5(0.8-2.9) |
| CHD Mortality(n=100) | ||||
| >414 | 15(5) | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) |
| 373-414 | 13(5) | 0.9(0.4-1.9) | 0.9(0.4-1.9) | 1.0(0.4-2.2) |
| 338-373 | 19(7) | 1.4(0.7-2.7) | 1.3(0.7-2.6) | 0.8(0.3-2.0) |
| 290-338 | 21(8) | 1.6(0.8-3.1) | 1.5(0.8-3.0) | 1.5(0.6-3.3) |
| 0-290 | 32(13) | 2.6(1.4-4.8) | 2.2(1.2-4.3) | 1.8(0.8-4.1) |
Adjusted for age, sex, race, general health status, education level, smoking status, systolic blood pressure, total cholesterol, fasting glucose, C-Reactive Protein, body mass index, prevalent medical conditions (pulmonary disease, diabetes mellitus, arthritis), any difficulty in Activities of Daily Living or Instrumental Activities of Daily Living, CES-Depression scale score, Modified Mini-Mental State score, major electrocardiogram abnormalities, ankle-brachial index, and medication use (aspirin, any lipid lowering, any anti-hypertensive).
Rate per 1,000 person-years
Figure 1.
Kaplan-Meier Survival Plots of All-Cause Mortality by 6 MWT Distance Quintile
Table 3.
Association between Six Minute Walk Distance (meters) and All-Cause Mortality in Adjusted Models among Participants without Prevalent Cardiovascular disease as Stratified by Age-, Gender- and Race
| 6 MWT Distance | Age(years) | Gender | Race | |||
|---|---|---|---|---|---|---|
| Quintiles | 65-80 (n=1,231) | >80 (n=434) | Male (n=584) | Female (n=1,081) | White (n=1,412) | Nonwhite (n=253) |
| >414 | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) | 1.0(Referent) |
| 373-414 | 1.2 (0.8-1.8) | 0.6 (0.3-1.3) | 1.1 (0.7-1.9) | 1.1 (0.6-2.1) | 1.0 (0.7-1.5) | 4.2 (0.8-22.6) |
| 338-373 | 1.2 (0.7-1.8) | 1.3 (0.7-2.6) | 1.3 (0.8-2.2) | 1.3 (0.7-2.3) | 1.2 (0.8-1.8) | 2.1 (0.4-10.2) |
| 290-338 | 1.6 (1.0-2.4) | 1.7 (0.8-3.3) | 1.5 (0.9-2.4) | 1.9 (1.1-3.2) | 1.7 (1.2-2.5) | 1.1 (0.2-5.9) |
| 0-290 | 1.9 (1.2-3.1) | 2.2 (1.1-4.3) | 1.6 (0.9-2.7) | 2.4 (1.4-4.1) | 1.9 (1.3-2.7) | 3.8 (0.8-17.0) |
Association expressed in Hazard Ratio (95% Confidence Interval(CI)) with referent as 6 MWT distance Quintile>414 meters.
Models stratified by either age, gender or race and adjusting for all other covariates including general health status, education level, smoking status, systolic blood pressure, total cholesterol, fasting glucose, C-Reactive Protein, body mass index, prevalent medical conditions (pulmonary disease, diabetes mellitus, arthritis), any difficulty in Activities of Daily Living or Instrumental Activities of Daily Living, CES-Depression scale score, Modified Mini-Mental State score, major electrocardiogram abnormalities, ankle-brachial index, and medication use (aspirin, any lipid lowering, any anti-hypertensive).
Table 4 displays results of the Tests of discrimination and reclassification for the models with and without 6 MWT. The addition of 6 MWT to the Model resulted in an increase in Harrell's C statistic from 0.6897 to 0.7028 (p = 0.09) indicating a trend toward improvement of the Model with the addition of the 6 MWT. Adding 6 MWT to the adjusted model resulted in an IDI of 4.4% and provided category-free NRI of 28%. Of the 160 cardiovascular disease-related deaths among the 1,665 participants with a 6 MWT, coronary heart disease deaths accounted for more than half (100(63%)) while the remaining deaths were due to strokes (39(24%)), other atherosclerotic events (11(7%)), and other cardiovascular events (10(6%)).
Table 4.
Comparison of Models with and without 6 MWT association with All-Cause Mortality
| Test | Model A | Model B | P Value |
|---|---|---|---|
| Discrimination | |||
| Harrell's C Statistic | 0.6897 | 0.7028 | 0.09 |
| Reclassification | |||
| Net Reclassification Improvement | |||
| Relative (%) | 28.0 | ||
| Integrated Discrimination Index | |||
| Absolute | 0.0067 | 0.003 | |
| Relative (%) | 4.4 |
Model A adjusted for age, sex, race, general health status, education level, smoking status, systolic blood pressure, total cholesterol, fasting glucose, C-Reactive Protein, body mass index, prevalent medical conditions (pulmonary disease, diabetes mellitus, arthritis), any difficulty in Activities of Daily Living or Instrumental Activities of Daily Living, CES-Depression scale score, Modified Mini-Mental State score, major electrocardiogram abnormalities, ankle-brachial index, and medication use (aspirin, any lipid lowering, any anti-hypertensive).
Model B adjusted for variables in Model A plus 6 MWT.
The overall cardiovascular disease mortality rate was 12 per 1,000 person-years. A 6 MWT distance in the two shortest distance quintiles was associated with a two-fold greater risk of cardiovascular disease deaths relative to those with a 6 MWT distance >414 meters in an unadjusted model. After adjusting for age and sex, the two shortest 6 MWT distance quintiles remained at increased risk for cardiovascular mortality. In fully adjusted model, the risk of cardiovascular mortality associated with the two shortest 6 MWT distance quintiles was no longer statistically significant (Table 2).
One hundred of the 504 deaths were attributed to coronary heart disease with an even rate of 8 per 1,000 person-years. A 6 MWT distance in the shortest distance quintile was associated with a two-and-one half fold increased risk relative to those with a 6 MWT >414 meters. After adjusting for age and sex, participants in the shortest 6 MWT distance quintile remained at increased risk for coronary heart disease mortality but this association was no longer statistically significant in the fully adjusted model (Table 2).
6 MWT Distance and Incident Events
A total of 525 incident cardiovascular events and 305 incident coronary heart disease events occurred among the 1,665 participants with an overall incident rate of 36 per 1,000 person-years. Table 5 displays the association between 6 MWT distance and incident events. Participants who walked a distance of 290 to 338 meters and those with less than 290 meters in the 6 MWT were at 1.5-fold greater risk of incident cardiovascular events in the unadjusted model and also the model adjusted for age and sex. The inverse association between 6 MWT less than 290 meters and incident cardiovascular disease was no longer significant in the fully adjusted model (HR, 1.2; 95% CI, 0.8-1.7). Similarly, the observed association between those in the shortest 6 MWT distance quintile and incident coronary heart disease events in the unadjusted model (HR, 1.4; 95% CI, 1.0-1.9) was no longer statistically significant in the fully adjusted model (HR, 1.3; 95% CI, 0.8-2.1).
Table 5.
Association between Six Minute Walk Test Distance and Incident Cardiovascular Events among participants without prevalent Cardiovascular Disease
| Event | Events n (Rate†) | Unadjusted Model | Age- and Sex-Adjusted | Multivariable Adjustment* |
|---|---|---|---|---|
| Hazard Ratio(95% CI) | ||||
| Incident CVD(n=525) | ||||
| >414 | 90(36) | 1.0 | 1.0 | 1.0 |
| 373-414 | 83(33) | 0.9(0.7-1.2) | 0.9(0.7-1.3) | 0.9(0.7-1.3) |
| 338-373 | 114(48) | 1.3(1.0-1.8) | 1.4(1.0-1.8) | 1.1(0.8-1.6) |
| 290-338 | 116(52) | 1.5(1.1-1.9) | 1.5(1.1-1.9) | 1.3(0.9-1.8) |
| 0-290 | 122(55) | 1.6(1.2-2.1) | 1.5(1.1-2.0) | 1.2(0.8-1.7) |
| Incident CHD(n=305) | ||||
| >414 | 59(23) | 1.0 | 1.0 | 1.0 |
| 373-414 | 46(18) | 0.8(0.5-1.1) | 0.8(0.5-1.2) | 1.0(0.6-1.5) |
| 338-373 | 62(25) | 1.1(0.8-1.6) | 1.1(0.8-1.6) | 1.0(0.7-1.6) |
| 290-338 | 67(28) | 1.3(0.9-1.8) | 1.3(0.9-1.9) | 1.2(0.8-1.9) |
| 0-290 | 71(30) | 1.4(1.0-1.9) | 1.6(1.0-2.0) | 1.3(0.8-2.1) |
Adjusted for age, sex, race, general health status, education level, smoking status, systolic blood pressure, total cholesterol, fasting glucose, C-Reactive Protein, body mass index, prevalent medical conditions (pulmonary disease, diabetes mellitus, arthritis), any difficulty in Activities of Daily Living or Instrumental Activities of Daily Living, CES-Depression scale score, Modified Mini-Mental State score, major electrocardiogram abnormalities, ankle-brachial index, and medication use (aspirin, any lipid lowering, any anti-hypertensive).
Rate per 1,000 person-years
6 MWT Participants and Outcomes
Supplemental Tables 1 and 2 display the characteristics of participants with and without a 6 MWT and the association between 6 MWT and study endpoints, respectively. Participants with a 6 MWT were younger, more likely to be men, of white race, and to have achieved a higher education level; less reported depressive symptoms; less often report inability to perform ADLS or IADLS; higher cognitive function scores; and were less likely to have prevalent health conditions.
Among the 4,708 participants who remained enrolled in CHS between 1996 and 1997, there were 2,286 deaths of which 556 were attributed to coronary heart disease. The overall mortality rate was 74.4 per 1,000 person-years. There was a significantly increased risk of death among participants without a 6 MWT (HR, 1.1; 95% CI, 1.0-1.3) and those without a clinic visit (HR, 1.8; 95% CI, 1.2-2.7). While a greater than two-fold coronary heart disease mortality rate was observed among participants without a clinic visit relative to those with a 6 MWT during the clinic visit in unadjusted and age- and sex-adjusted models, this association was no longer significant in the fully adjusted model (Supplemental Table 2). Similarly, the increased risk of incident events among participants without a 6 MWT was attenuated in a model adjusting for all other covariates.
Discussion
In a large cohort of community-dwelling older adults, we observed an independent inverse association between distance walked during a 6 MWT and mortality. Participants with a 6 MWT distance less than 338 meters had more than a 1.5-fold greater risk of mortality relative to those who were able to walk 414 meters or longer. Moreover, the 6 MWT provided additional information beyond various measures of psychosocial, physical, cognitive, and other comorbidities. However, the association between 6 MWT distance and coronary or cardiovascular related outcomes was mostly explained by the overall poorer health status of the participants.
Performance on walked-based testing has been shown to be correlated with cardiorespiratory fitness (Kligfield & Lauer, 2006). Both self-reported walking ability and performance on distance-based walk tests have been shown to be predictors of disability, cardiovascular morbidity, and all-cause mortality (Guralnik et al., 1994; Newman at al., 2006; Vestergaard, Patel, Bandinelli, Ferrucci, & Guralnik, 2009). Regarding the relationship between the 6 MWT distance and health outcomes, the inverse association with adverse outcomes has been previously demonstrated in disease-specific populations such as those with heart failure, pulmonary disease, end-stage liver disease (Alahdab, Mansour, Napan, & Stamos, 2008; Boxer et al., 2010; Castel et al., 2009; Enfield et al., 2009). However, the evidence on the association between 6 MWT and mortality in community-dwelling older adults has been limited. A study by Mutikainen et al. examined the association between 6 MWT performance and distance walked with all-cause mortality in a cohort of women aged 63(76 years (Mutikainen et al., 2010). Older women who did not perform the 6 MWT were at a nearly 7-fold greater risk of mortality relative to women with a 6 MWT and who were able to walk ≥561 meters. A similar increased mortality risk among those with no clinic and no 6 MWT was observed in our study of CHS participants which is likely a result of poorer physical and cognitive health status. There was a non-statistically significant trend towards an increased risk of death with shorter distance walked when comparing participants with a 6 MWT distance ≤495 meters relative to those with a distance ≥561 meters (HR 2.47; 95% CI, 0.81-7.56). Our study confirms the inverse association of both performance of the 6 MWT and distance walked with death in both men and women. In addition, our findings of the statistically significant association between distance walked on the 6 MWT and mortality extends on prior literature.
The conventional method for assessing functional capacity has been by treadmill testing. Beyond detection of obstructive coronary disease, the treadmill test provides measure of an individual's functional capacity and predict of mortality (Blair et al., 1996; Goraya et al., 2000; Gulati et al., 2003; Kligfield & Laurer, 2006; Kokkinos et al., 2008; Messinger-Rapport, Pothier Snader, Blackstone, Yu, & Lauer, 2003; Mora et al., 2003; Myers et al, 2002; Spin et al., 2002; Sui, Laditka, Hardin, & Blair, 2007). Based on a cohort of 556 participants with stable coronary heart disease from the Heart and Soul Study, Beatty et al reported a significant correlation (r=0.66; P <0.001) between 6 MWT distance and exercise capacity as measured by treadmill testing (Beatty, Schiller, & Whooley, 2012). In addition, the 6 MWT and treadmill testing had similar discrimination, integrated improvement, and net reclassification improvement for prediction of cardiovascular endpoints.
Our study has several strengths and limitations. First, 6 MWT performance may not reflect a maximal effort similar to that obtained via treadmill-based exercise protocols. Second, approximately one-third of participants with a clinic visit did not perform a 6 MWT. As shown in the supplementary analyses, 6 MWT participation status was association with mortality. The strengths of our study include the large sample size of community-dwelling older adults, long follow-up time, extensive clinical examination, and standardized surveillance and ascertainment of hard outcomes.
Our study shows that both participation and distance walked on a 6 MWT are associated with mortality. A 6 MWT walk distance of 338 meters appears to identify older aged men and women with poor prognosis. Moreover, the 6 MWT distance is of incremental prognostic value in community-dwelling older adults. Given the limited ability of older adults in completing treadmill-based protocols, the 6 MWT may provide a practical prognostic tool in older aged adults. Relative to treadmill testing, the 6 MWT has minimal associated equipment, safety, and cost issues. Our findings support the utility of the 6 MWT as a prognostic measure in community-dwelling older adults.
Supplementary Material
Footnotes
Conflict of Interest Statement: The work we are submitting is original, and all authors meet the criteria for authorship, including acceptance for responsibility for the scientific content. There are no conflicts of interest to report.
Contributor Information
Ali Yazdanyar, Department of Medicine, Reading Health System, West Reading, PA.
Michael M Aziz, Department of Obstetrics and Gynecology, Atlantic Health System, Morristown NJ.
Paul L Enright, Department of Medicine, University of Arizona, Tuscon, AZ.
Daniel Edmundowicz, Department of Medicine, Temple University, Philadelphia, PA.
Robert Boudreau, Department of Epidemiology, University of Pittsburgh, Pittsburgh, PA.
Kim Sutton-Tyrell, Department of Epidemiology, University of Pittsburgh, Pittsburgh, PA.
Lewis Kuller, Department of Epidemiology, University of Pittsburgh, Pittsburgh, PA.
Anne B Newman, Department of Epidemiology, University of Pittsburgh, Pittsburgh, PA.
References
- Alahdab MT, Mansour IN, Napan S, Stamos TD. Six minute walk test predicts long-term all-cause mortality and heart failure rehospitalization in African-American patients hospitalized with acute decompensated heart failure. Journal of Cardiac Failure. 2008;2:130–135. doi: 10.1016/j.cardfail.2008.10.006. [DOI] [PubMed] [Google Scholar]
- American Thoracic Society Guidelines for the six-minute walk test. American Journal of Respiratory and Critical Care Medicine. 2002;1:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- Beatty AL, Schiller NB, Whooley MA. Six-minute walk test as a prognostic tool in stable coronary heart disease: data from the heart and soul study. Archives of Internal Medicine. 2012;14:1096–1102. doi: 10.1001/archinternmed.2012.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein ML, Despars JA, Singh NP, Avalos K, Stansbury DW, Light RW. Reanalysis of the 12-minute walk in patients with chronic obstructive pulmonary disease. Chest. 1994;1:163–167. doi: 10.1378/chest.105.1.163. [DOI] [PubMed] [Google Scholar]
- Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, Kronenberg MW, Kostis JB, Kohn RM, Guillotte M. Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. The Journal of the American Medical Association. 1993;14:1702–1707. [PubMed] [Google Scholar]
- Blackburn H. Classification of the electrocardiogram for population studies: Minnesota Code. Journal of Electrocardiology. 1969;3:305–310. doi: 10.1016/s0022-0736(69)80120-2. [DOI] [PubMed] [Google Scholar]
- Blair SN, Kampert JB, Kohl HW, Barlow CE, Macera CA, Paffenbarger RS, Gibbons LW. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. The Journal of the American Medical Association. 1996;3:205–210. [PubMed] [Google Scholar]
- Boxer R, Kleppinger A, Ahmad A, Annis K, Hager D, Kenny A. The 6-minute walk is associated with frailty and predicts mortality in older adults with heart failure. Congestive Heart Failure-Greenwich, Conn.) 2010;5:208–213. doi: 10.1111/j.1751-7133.2010.00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahalin L, Pappagianopoulos P, Prevost S, Wain J, Ginns L. The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest. 1995;2:452–459. doi: 10.1378/chest.108.2.452. [DOI] [PubMed] [Google Scholar]
- Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;2:325–332. doi: 10.1378/chest.110.2.325. [DOI] [PubMed] [Google Scholar]
- Carey EJ, Steidley DE, Aqel BA, Byrne TJ, Mekeel KL, Rakela J, Vargas HE, Douglas DD. Six-minute walk distance predicts mortality in liver transplant candidates. Liver transplantation: Official Publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2010;12:1373–1378. doi: 10.1002/lt.22167. [DOI] [PubMed] [Google Scholar]
- Castel MA, Mendez F, Tamborero D, Mont L, Magnani S, Tolosana JM, Berruezo A, Godoy M, Sitges M, Vidal B, Roig E, Brugada J. Six-minute walking test predicts long-term cardiac death in patients who received cardiac resynchronization therapy. Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology. 2009;3:338–342. doi: 10.1093/europace/eun362. [DOI] [PubMed] [Google Scholar]
- Enfield K, Gammon S, Floyd J, Falt C, Patrie J, Platts-Mills TA, Truwit JD, Shim YM. Six-minute walk distance in patients with severe end-stage COPD: association with survival after inpatient pulmonary rehabilitation. Journal of Cardiopulmonary Rehabilitation and Prevention. 2009;3:195–202. doi: 10.1097/HCR.0b013e3181c565e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleg JL, Pina IL, Balady GJ, Chaitman BR, Fletcher B, Lavie C, Limacher MC, Stein RA, Williams M, Bazzarre T. Assessment of functional capacity in clinical and research applications: An advisory from the Committee on Exercise, Rehabilitation, and Prevention, Council on Clinical Cardiology, American Heart Association. Circulation. 2000;13:1591–1597. doi: 10.1161/01.cir.102.13.1591. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;3:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A. The Cardiovascular Health Study: design and rationale. Annals of Epidemiology. 1991;3:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- Gill TM, DiPietro L, Krumholz HM. Role of exercise stress testing and safety monitoring for older persons starting an exercise program. JAMA : The Journal of the American Medical Association. 2000;3:342–349. doi: 10.1001/jama.284.3.342. [DOI] [PubMed] [Google Scholar]
- Greig C, Butler F, Skelton D, Mahmud S, Young A. Treadmill walking in old age may not reproduce the real life situation. Journal of the American Geriatrics Society. 1993;1:15–18. doi: 10.1111/j.1532-5415.1993.tb05941.x. [DOI] [PubMed] [Google Scholar]
- Goraya TY, Jacobsen SJ, Pellikka PA, Miller TD, Khan A, Weston SA, Gersh BJ, Roger VL. Prognostic value of treadmill exercise testing in elderly persons. Annals of Internal Medicine. 2000;11:862–870. doi: 10.7326/0003-4819-132-11-200006060-00003. [DOI] [PubMed] [Google Scholar]
- Gulati M, Pandey DK, Arnsdorf MF, Lauderdale DS, Thisted RA, Wicklund RH, Al-Hani AJ, Black HR. Exercise capacity and the risk of death in women: the St James Women Take Heart Project. Circulation. 2003;13:1554–1559. doi: 10.1161/01.CIR.0000091080.57509.E9. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology. 1994;2:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Hollenberg M, Ngo LH, Turner D, Tager IB. Treadmill exercise testing in an epidemiologic study of elderly subjects. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 1998;4:B259–67. doi: 10.1093/gerona/53a.4.b259. [DOI] [PubMed] [Google Scholar]
- Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Annals of Epidemiology. 1995;4:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- Kligfield P, Lauer MS. Exercise electrocardiogram testing: beyond the ST segment. Circulation. 2006;19:2070–2082. doi: 10.1161/CIRCULATIONAHA.105.561944. [DOI] [PubMed] [Google Scholar]
- Kokkinos P, Myers J, Kokkinos JP, Pittaras A, Narayan P, Manolis A, Karasik P, Greenberg M, Papademetriou V, Singh S. Exercise capacity and mortality in black and white men. Circulation. 2008;5:614–622. doi: 10.1161/CIRCULATIONAHA.107.734764. [DOI] [PubMed] [Google Scholar]
- Langenfeld H, Schneider B, Grimm W, Beer M, Knoche M, Riegger G, Kochsiek K. The six-minute walk--an adequate exercise test for pacemaker patients? Pacing and Clinical Electrophysiology. 1990;12(Pt 2):1761–1765. doi: 10.1111/j.1540-8159.1990.tb06886.x. [DOI] [PubMed] [Google Scholar]
- Messinger-Rapport B, Pothier Snader CE, Blackstone EH, Yu D, Lauer MS. Value of exercise capacity and heart rate recovery in older people. Journal of the American Geriatrics Society. 2003;1:63–68. doi: 10.1034/j.1601-5215.2002.51011.x. [DOI] [PubMed] [Google Scholar]
- Milligan NP, Havey J, Dossa A. Using a 6-minute walk test to predict outcomes in patients with left ventricular dysfunction. Rehabilitation Nursing : The Official Journal of the Association of Rehabilitation Nurses. 1997;4:177–181. doi: 10.1002/j.2048-7940.1997.tb02095.x. [DOI] [PubMed] [Google Scholar]
- Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. Journal of the American Geriatrics Society. 1998;6:706–711. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- Mora S, Redberg RF, Cui Y, Whiteman MK, Flaws JA, Sharrett AR, Blumenthal RS. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: a 20-year follow-up of the lipid research clinics prevalence study. The Journal of the American Medical Association. 2003;12:1600–1607. doi: 10.1001/jama.290.12.1600. [DOI] [PubMed] [Google Scholar]
- Mutikainen S, Rantanen T, Alen M, Kauppinen M, Karjalainen J, Kaprio J, ujala UM. Walking ability and all-cause mortality in older women. Internationa Journal of Sports Medicine. 2010;3:216–222. doi: 10.1055/s-0030-1268506. [DOI] [PubMed] [Google Scholar]
- Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. The New England Journal of Medicine. 2002;11:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, Pahor M, Satterfield S, Brach JS, Studenski SA, Harris TB. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. The Journal of the American Medical Association. 2006;17:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP, Borhani NO, Wolfson SK. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Heart Study (CHS) Collaborative Research Group. Circulation. 1993;3:837–845. doi: 10.1161/01.cir.88.3.837. [DOI] [PubMed] [Google Scholar]
- Orme JG, Reis J, Herz EJ. Factorial and discriminant validity of the Center for Epidemiological Studies Depression (CES-D) scale. Journal of Clinical Psychology. 1986;1:28–33. doi: 10.1002/1097-4679(198601)42:1<28::aid-jclp2270420104>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Peeters P, Mets T. The 6-minute walk as an appropriate exercise test in elderly patients with chronic heart failure. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 1996;4:M147–51. doi: 10.1093/gerona/51a.4.m147. [DOI] [PubMed] [Google Scholar]
- Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, Price TR, Rautaharju PM, Robbins J. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Annals of Epidemiology. 1995;4:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- Rikli R, Jones C. The reliability and validity of a 6-Minute Walk test as a measure of physical endurance in older adults. J Aging and Phys Activity. 1998;6:363–375. [Google Scholar]
- Simonsick EM, Fan E, Fleg JL. Estimating cardiorespiratory fitness in well-functioning older adults: treadmill validation of the long distance corridor walk. Journal of the American Geriatrics Society. 2006;1:127–132. doi: 10.1111/j.1532-5415.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- Spin JM, Prakash M, Froelicher VF, Partington S, Marcus R, Do D, Myers J. The prognostic value of exercise testing in elderly men. The American Journal of Medicine. 2002;6:453–459. doi: 10.1016/s0002-9343(02)01065-3. [DOI] [PubMed] [Google Scholar]
- Sui X, Laditka JN, Hardin JW, Blair SN. Estimated functional capacity predicts mortality in older adults. Journal of the American Geriatrics Society. 2007;12:1940–1947. doi: 10.1111/j.1532-5415.2007.01455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tell GS, Fried LP, Hermanson B, Manolio TA, Newman AB, Borhani NO. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Annals of Epidemiology. 1993;4:358–366. doi: 10.1016/1047-2797(93)90062-9. [DOI] [PubMed] [Google Scholar]
- Vestergaard S, Patel KV, Bandinelli S, Ferrucci L, Guralnik JM. Characteristics of 400-meter walk test performance and subsequent mortality in older adults. Rejuvenation Research. 2009;3:177–184. doi: 10.1089/rej.2009.0853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijkstra PJ, TenVergert EM, Van Der Mark TW, Postma DS, Van Altena R, Kraan J, Koeter GH. Relation of lung function, maximal inspiratory pressure, dyspnoea, and quality of life with exercise capacity in patients with chronic obstructive pulmonary disease. Thorax. 1994;5:468–472. doi: 10.1136/thx.49.5.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.