Abstract
Objective
To compare serum uric acid levels in adolescents born prematurely and adolescents born at term and to assess the correlation between serum uric acid and blood pressure in those born prematurely.
Study design
In this observational cohort study, 124 adolescents born prematurely and 44 adolescents born at term were studied at 14 years of age. Multivariate analyses were used to describe the relationship of premature birth to serum uric acid, while adjusting for confounding variables. Pearson correlation was used to describe the relationship between uric acid and systolic blood pressure among those born prematurely.
Results
Adjusting for race, sex, maternal hypertension and fetal growth, preterm adolescents had higher serum uric acid levels than adolescents born at term [adjusted mean difference (95% confidence interval: 0.46 (0.10, 0.81) mg/dL, 27.4 (6, 48.2) μmol/L, p=0.012]. Among those born prematurely, uric acid was positively correlated with systolic blood pressure [Pearson correlation coefficient: 0.29 (0.12, 0.44; p= 0.0013).
Conclusions
Serum uric acid levels are higher in adolescents born prematurely than in those born at term and this difference could contribute to higher blood pressure among individuals born prematurely.
Keywords: very low birth weight, programming, blood pressure, follow-up, prematurity, hypertension
Preterm birth (<37 completed weeks gestation) and very low birth weight (VLBW; <1500g) are associated with elevated blood pressure (BP) in children and young adults.1,2 The etiology of this association is not well understood. Because systolic blood pressure (SBP) in adolescence is associated with adult hypertension3 and risk for coronary artery disease,4 information about the relationship of preterm birth and BP in adolescence could inform efforts to improve cardiovascular health among adults born prematurely.
There is growing interest in the role of uric acid in the etiology of essential hypertension. In animal models, increased serum uric acid causes hypertension.5 In childhood, uric acid levels are positively associated with BP 6,7,8,9,10,7 and predict adult BP.11 Treatment with allopurinol significantly lowers uric acid and BP in adolescents with newly diagnosed essential hypertension.12 Additionally, uric acid is negatively correlated with both birth weight 8,13,14,15 and gestational age 16 in cohorts of term or mostly term-born children. Thus, we hypothesized that adolescents born prematurely with VLBW would have elevated serum uric acid compared with term-born peers and that among those born preterm, serum uric acid levels would be positively correlated with blood pressure.
Methods
The preterm sample was derived from a cohort of consecutive VLBW births at the regional perinatal center in Forsyth County, North Carolina from January 1, 1992, to June 30, 1996. Eligible preterm infants (n = 479) were singleton at birth, had no major congenital malformation, and returned for evaluation at one year adjusted age. Among eligible children, 193 were studied at 14 years of age as part of a larger study of BP; participants with a blood sample for uric acid are included in the analysis. Adolescents who were born at the same medical center at term with birth weight ≥2500g were recruited using fliers, newspaper ads, and word of mouth. They were also singletons, had no major congenital malformation, but had not been evaluated at the medical center at one year of age. Data from participants born at term who provided a blood sample for uric acid are included in the analysis.
This study was approved by the Wake Forest School of Medicine Institutional Review Board. Written informed consent was obtained from parents or legal guardians and participants gave assent.
We reviewed medical records and delivery logs to determine birth weight, gestational age, and mode of delivery. For the preterm cohort, a first trimester ultrasound, when available, was used to estimate gestational age. Otherwise, we used, in order of priority, the mother’s last menstrual period or a clinical assessment of the newborn infant. Maternal hypertension during pregnancy was obtained by questionnaire administered to the parent or guardian. As an index of fetal growth we used sex-specific birth weight z-score, calculated using US natality data.17 Race was categorized as black or non-black, based on parent’s report.
A random non-fasting venous sample was obtained by venipuncture, after application of 4% lidocaine. Serum uric acid was determined by uricase.
Blood pressure was measured in the right arm with an oscillometric device (Dinamap® Pro 100, Critikon) by nursing staff certified in BP measurement. Guidelines established by the National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents were followed to determine cuff size.18 The participants were seated quietly for five minutes with back supported, the cubital fossa supported at heart level, and feet on the floor. The average of five measurements was used to estimate the SBP and diastolic (DBP) BP.
Anthropometric measurements were made in triplicate. After the participant removed his or her shoes, height was measured using a wall-mounted stadiometer and weight was measured using a digital platform scale. Abdominal circumference was assessed to the nearest tenth of a centimeter with a measuring tape according to procedures of National Health and Nutrition Examination Survey (NHANES) III.19
Statistical Analyses
To describe the study groups, we used means and standard deviations for continuous variables, and counts and percentages for categorical variables. Stratified by sex, we compared characteristics in preterm and term groups using Wilcoxon Rank Sum Tests for continuous variables and Fisher’s Exact Test for categorical variables. We estimated the adjusted mean difference in uric acid between preterm and term participants using multivariate general linear models that included the variables sex, race, hypertensive pregnancy, and birth weight z-scores – variables which could confound the relationship between prematurity and uric acid. To evaluate whether sex modifies the preterm birth-uric acid relationship, an interaction term was used. Pearson correlation was used to describe the linear relationship between uric acid and SBP among those born prematurely.
Results
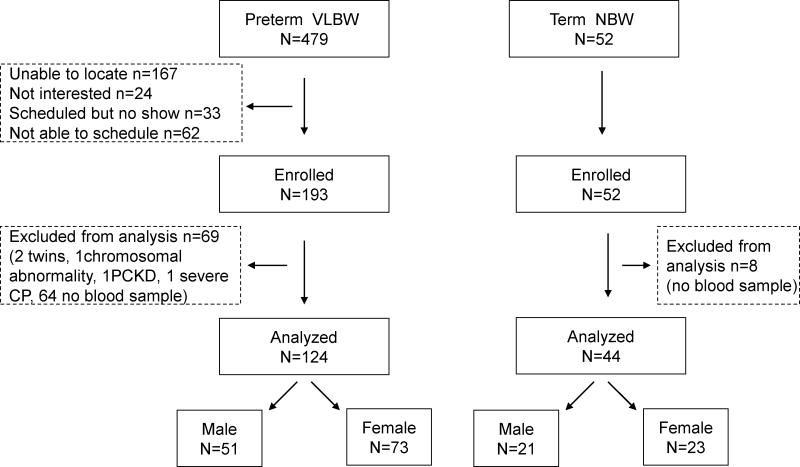
We studied 124 adolescents who were born prematurely (23–34 weeks) with VLBW and 44 adolescents born at term with birth weight ≥ 2500g at 14 years of age (Figure). The neonatal characteristics of those born prematurely who were eligible for, but not included in, the study were not different from those included; the BP, body mass index, race, and sex of the adolescents who participated in the main study of BP but did not have a blood sample for uric acid were not different from participants with a uric acid sample in either preterm or term group (data not shown). A description of the study sample and comparisons of preterm and term participants at birth and 14 years of age are shown in the Table.
Figure.
Progress of the participants through the observational study.
Table 1.
Characteristics of participants at birth expressed as mean ± SD or N (%).
| Entire group | Males | Females | ||||
|---|---|---|---|---|---|---|
| preterm n=124 |
term n=44 |
preterm n=51 |
term n=21 |
preterm n=73 |
term n=23 |
|
| Birth | ||||||
| Gestational age, weeks | 27.8 ± 2.6* | 39.6 ± 1.1 | 27.9 ± 2.7* | 39.6 ± 1.0 | 27.6 ± 2.6* | 39.7 ± 1.2 |
| Birth weight, g | 1056 ± 272* | 3457 ± 446 | 1090 ± 255* | 3543 ± 441 | 1033 ± 282* | 3379 ± 445 |
| Birth weight z-score | −0.23 ± 0.82 | −0.02 ± 0.96 | −0.29 ± 0.94 | 0.02 ± 0.99 | −0.19 ± 0.74 | −0.06 ± 0.96 |
| Cesarean delivery | 63 (51)* | 8 (18) | 30 (59)* | 5 (24) | 33 (45)* | 3 (13) |
| Antenatal steroid exposure | 70 (56)* | 0 | 30 (59)* | 0 | 40 (55)* | 0 |
| Male | 51 (41) | 21 (48) | -- | -- | -- | -- |
| Black | 46 (37) | 18 (41) | 20 (39) | 5 (24) | 26 (36) | 13 (57) |
| Hypertensive pregnancy | 44 (35)* | 3 (7) | 18 (35)* | 2 (10) | 26 (36)* | 1 (4) |
| 14 years of age | ||||||
| SBP, mmHg | 109.5 ± 10.8 * | 104.0 ± 8.2 | 111.5 ± 10.0 * | 104.3 ± 8.7 | 108.1 ± 11.1 | 103.7 ± 7.9 |
| DBP, mmHg | 60.1 ± 6.4 * | 56.9 ± 5.8 | 59.2 ± 5.1 * | 55.0 ± 6.0 | 60.8 ± 7.1 | 58.6 ± 5.2 |
| Weight, kg | 60.0 ± 15.4 | 64.7 ± 15.8 | 62.5 ± 17.3 | 62.4 ± 10.2 | 58.2 ± 13.8 | 66.7 ± 19.6 |
| Height, cm | 161.7 ± 9.3 * | 168.1 ± 7.2 | 167.4 ± 9.4 | 171.7 ± 5.3 | 157.8 ± 7.0 * | 164.8 ± 7.2 |
| Body Mass Index, kg·m−2 | 22.8 ± 5.2 | 22.8 ± 5.2 | 22.0 ± 5.3 | 21.1 ± 2.7 | 23.2 ± 5.1 | 24.3 ± 6.4 |
| Waist circumference, cm | 79.0 ± 13.8 | 76.6 ± 10.1 | 77.8 ± 5.9 | 74.0 ± 7.4 | 79.4 ± 12.3 | 79.0 ± 11.7 |
| Uric acid, mg/dL | 5.2 ± 1.3 * | 4.7 ± 1.1 | 6.0 ± 1.3 * | 5.3 ± 0.9 | 4.7 ± 0.9* | 4.2 ± 1.0 |
| Uric acid, μmol/L | 309.3 ± 77.3 | 279.6 ± 65.4 | 356.9 ± 77.3 | 315.3 ± 53.5 | 279.6 ± 53.5 | 250.4 ± 59.5 |
p<0.05 Preterm v. term counterpart calculated by Wilcoxon Rank Sum test
The unadjusted mean difference (95% CI) in uric acid between preterm and term adolescents was 0.53 (0.11, 0.95) mg/dL, 31.5 (6.5, 56.5) μmol/L, p=0.014. When adjusted for potential confounding variables sex, race, maternal hypertension during pregnancy, and birth weight z-score, the mean difference was 0.46 (0.10, 0.81) mg/dL, 27.4 (6, 48.2) μmol/L, p=0.012. We explored the data for sex differences using an interaction term (preterm/term group x sex) for which the p value was 0.42. Thus, further analyses were not stratified by sex. In both unadjusted analyses as well as analyses adjusted for sex, race, maternal hypertension during pregnancy, and birth weight z-score, no difference was found for uric acid between preterm participants exposed to antenatal steroids and those not exposed (p=0.7 and p=0.14, respectively). The Pearson correlation coefficient for uric acid and SBP among those born preterm was 0.29 (0.12, 0.44), p= 0.0013.
Discussion
We found higher serum uric acid levels among adolescents who were born prematurely with VLBW when compared with peers who were born at term with normal birth weight. Uric acid was positively correlated with SBP among those born prematurely.
Similar to our findings, Park et al described an inverse relationship between uric acid and gestational age in a cohort of 3 year olds who were mostly born at term (mean gestational age for this cohort of 136 participants was 37.7 weeks with 16 born at ≤ 34 weeks gestation).16 Inverse associations between birth weight and uric acid have been described in children born at term, suggesting a link between intrauterine growth restriction and elevated uric acid.8,15,14 Likewise, lower birth weight was associated with increased uric acid in a cohort of Japanese school children; although the gestational age of this cohort was not available, their birth weights ranged from 1420–4704g, with a mean of 3.143g.13 In our cohort of VLBW infants, adjustment for birth weight z-score, an estimate of intrauterine growth, did not alter the preterm-term uric acid difference. Although we did not identify sex differences in the preterm-term uric acid relationship, DeBoer et al found that non-Hispanic white males in the NHANES sample had the strongest relationship between uric acid and metabolic syndrome, and non-Hispanic white females had the weakest.20
Even though our study is limited by its observational design and modest sample size, it is a large study of uric acid in children born prematurely and adds to the growing body of work showing positive associations of uric acid with BP in adolescents and increased uric acid in those born prematurely. It’s generalizability to the current VLBW population in the US may be limited by lack of participants of Hispanic ethnicity. Nonetheless, we hypothesize that programmed alterations in the kidney might lead to increased uric acid which contributes to the higher BP found in adolescents who were born prematurely with VLBW.
Uric acid is a breakdown product of the purine mononucleotides and since the early 20th century, uric acid levels have almost doubled with the increase in purine-rich foods and sugar in the Western diet. Two thirds of uric acid is excreted by the kidney. Nearly all blood urate enters the glomerular filtrate, so renal function can influence serum urate levels. Urate transport, both reabsorption and secretion, is localized in the proximal tubule and in humans only about 10% of the filtered urate load is excreted. Recent genome-wide association studies have identified multiple urate transporters for reabsorption and secretion.21 In a cohort of children with essential hypertension, hyperuricemia was attributed to decreased urate clearance, and as the glomerular filtration rates of the hyperuricemic participants were not different from those with lower uric acid, the decreased clearance was likely due to increased tubular reabsorption or diminished secretion.22 Likewise, Feig et al report no correlation between uric acid and glomerular filtration rate in a cohort containing both children with normal and elevated blood pressure.10
In animals, elevation of uric acid increases BP through stimulation of the renin-angiotensin system and decreased endothelial nitric oxide which is reversible with uric acid reduction or blockade of the renin angiotensin system.5,23 However, continued hyperuricemia causes microvascular disease in the kidney which results in sodium sensitive hypertension independent of uric acid levels.24 This finding might explain why the uric acid-BP relationship is weaker in older populations25 and suggests a window in which strategies to lower uric acid might have the most benefit.
Mechanisms that might explain the developmental origins of hypertension in those born preterm include decreased nephron number,26 altered renal tubular function,27,28 altered balance of the renin angiotensin system,29 decreased vascular dilation to nitric oxide,30 increased vascular stiffness,31 and increased sympathetic activity (higher heart rate)32. Clinical studies have linked uric acid levels to the renin angiotensin system,33, vascular stiffness34, and sympathetic activity.35 Thus, it is plausible that uric acid is involved in the development of programmed hypertension. To that end, Feig et al proposed that transplacental passage of maternal uric acid might cause intrauterine growth restriction and impair fetal nephron formation through endothelial dysfunction.14
Adolescents born prematurely with VLBW have higher uric acid than their peers born at term and this finding might contribute to their higher blood pressure. Further work is needed to determine why this difference in uric acid exists and the mechanism(s) through which it is correlated with BP. Uric acid might provide a target for treatment in this population to improve their future cardiovascular health.
Acknowledgments
Supported by the National Institute of Child Health and Human Development (PO1 HD047584), the Clinical Research Unit of Wake Forest Baptist Medical Center through MCRR/National Institute of Health (MO1-RR07122), Forsyth Medical Center, and the Wake Forest School of Medicine Department of Pediatrics Research Fund.
We thank Alice Scott, RN (study coordinator, supported by the National Institute of Child Health and Human Development [PO1 HD047584]), and the participants and their parents.
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.de Jong F, Monuteaux MC, van Elburg RM, Gillman MW, Belfort MB. Systematic Review and Meta-Analysis of Preterm Birth and Later Systolic Blood Pressure. Hypertension. 2012;59:226–34. doi: 10.1161/HYPERTENSIONAHA.111.181784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kajantie E, Hovi P. Is Very Preterm Birth a Risk Factor for Adult Cardiometabolic Disease? Seminars in Fetal and Neonatal Medicine. 2014;19:112–17. doi: 10.1016/j.siny.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential Hypertension Predicted by Tracking of Elevated Blood Pressure From Childhood to Adulthood: the Bogalusa Heart Study. Am J Hypertens. 1995;8:657–65. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 4.Hartiala O, Magnussen CG, Kajander S, Knuuti J, Ukkonen H, Saraste A, et al. Adolescence Risk Factors Are Predictive of Coronary Artery Calcification at Middle Age: The Cardiovascular Risk in Young Finns Study. Journal of the American College of Cardiology. 2012;60:1364–70. doi: 10.1016/j.jacc.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 5.Mazzali M, Hughes J, Kim YG, Jefferson JA, Kang DH, Gordon KL, et al. Elevated Uric Acid Increases Blood Pressure in the Rat by a Novel Crystal-Independent Mechanism. Hypertension. 2001;38:1101–06. doi: 10.1161/hy1101.092839. [DOI] [PubMed] [Google Scholar]
- 6.Loeffler LF, Navas-Acien A, Brady TM, Miller ER, III, Fadrowski JJ. Uric Acid Level and Elevated Blood Pressure in US Adolescents: National Health and Nutrition Examination Survey, 1999–2006. Hypertension. 2012;59:811–17. doi: 10.1161/HYPERTENSIONAHA.111.183244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones DP, Richey PA, Alpert BS, Li R. Serum Uric Acid and Ambulatory Blood Pressure in Children With Primary Hypertension. Pediatr Res. 2008;64:556–61. doi: 10.1203/PDR.0b013e318183fd7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franco MCP, Christofalo DMJ, Sawaya AL, Ajzen SA, Sesso R. Effects of Low Birth Weight in 8-to 13-Year-Old Children - Implications in Endothelial Function and Uric Acid Levels. Hypertension. 2006;48:45–50. doi: 10.1161/01.HYP.0000223446.49596.3a. [DOI] [PubMed] [Google Scholar]
- 9.Viazzi F, Antolini L, Giussani M, Brambilla P, Galbiati S, Mastriani S, et al. Serum Uric Acid and Blood Pressure in Children at Cardiovascular Risk. Pediatrics. 2013;132:e93–e99. doi: 10.1542/peds.2013-0047. [DOI] [PubMed] [Google Scholar]
- 10.Feig DI, Johnson RJ. Hyperuricemia in Childhood Primary Hypertension. Hypertension. 2003;42:247–52. doi: 10.1161/01.HYP.0000085858.66548.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alper AB, Jr, Chen W, Yau L, Srinivasan SR, Berenson GS, Hamm LL. Childhood Uric Acid Predicts Adult Blood Pressure: the Bogalusa Heart Study. Hypertension. 2005;45:34–38. doi: 10.1161/01.HYP.0000150783.79172.bb. [DOI] [PubMed] [Google Scholar]
- 12.Feig DI, Soletsky B, Johnson RJ. Effect of Allopurinol on Blood Pressure of Adolescents With Newly Diagnosed Essential Hypertension - A Randomized Trial. Jama-Journal of the American Medical Association. 2008;300:924–32. doi: 10.1001/jama.300.8.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaneshi T, Yoshida T, Ohshiro T, Nagasaki H, Asato Y, Ohta T. Birthweight and Risk Factors for Cardiovascular Diseases in Japanese Schoolchildren. Pediatr Int. 2007;49:138–43. doi: 10.1111/j.1442-200X.2007.02333.x. [DOI] [PubMed] [Google Scholar]
- 14.Feig DI, Nakagawa T, Karumanchi SA, Oliver WJ, Kang DH, Finch J, et al. Hypothesis: Uric Acid, Nephron Number, and the Pathogenesis of Essential Hypertension. Kidney Int. 2004;66:281–87. doi: 10.1111/j.1523-1755.2004.00729.x. [DOI] [PubMed] [Google Scholar]
- 15.Lurbe E, Garcia-Vicent C, Torro MI, Aguilar F, Redon J. Associations of Birth Weight and Postnatal Weight Gain With Cardiometabolic Risk Parameters at 5 Years of Age. Hypertension. 2014;63:1326–32. doi: 10.1161/HYPERTENSIONAHA.114.03137. [DOI] [PubMed] [Google Scholar]
- 16.Park B, Park E, Cho S, Kim Y, Lee H, Min J, et al. The Association Between Fetal and Postnatal Growth Status and Serum Levels of Uric Acid in Children at 3 Years of Age. Am J Hypertens. 2009;22:403–08. doi: 10.1038/ajh.2009.12. [DOI] [PubMed] [Google Scholar]
- 17.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A Nearly Continuous Measure of Birth Weight for Gestational Age Using a United States National Reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a Working Group Report From the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics. 1996;98:649–58. [PubMed] [Google Scholar]
- 19.National Center for Health Statistics. NHANES III Anthropometric Procedures Video. 2012 [Google Scholar]
- 20.DeBoer MD, Dong L, Gurka MJ. Racial/Ethnic and Sex Differences in the Relationship Between Uric Acid and Metabolic Syndrome in Adolescents: an Analysis of National Health and Nutrition Survey 1999–2006. Metabolism. 2012;61:554–61. doi: 10.1016/j.metabol.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lipkowitz M. Regulation of Uric Acid Excretion by the Kidney. Curr Rheumatol Rep. 2012;14:179–88. doi: 10.1007/s11926-012-0240-z. [DOI] [PubMed] [Google Scholar]
- 22.Prebis JW, Gruskin AB, Polinsky MS, Baluarte HJ. Uric Acid in Childhood Essential Hypertension. J Pediatr. 1981;98:702–07. doi: 10.1016/s0022-3476(81)80828-1. [DOI] [PubMed] [Google Scholar]
- 23.Corry DB, Eslami P, Yamamoto K, Nyby MD, Makino H, Tuck ML. Uric Acid Stimulates Vascular Smooth Muscle Cell Proliferation and Oxidative Stress Via the Vascular Renin-Angiotensin System. J Hypertens. 2008;26:269–75. doi: 10.1097/HJH.0b013e3282f240bf. [DOI] [PubMed] [Google Scholar]
- 24.Watanabe S, Kang DH, Feng L, Nakagawa T, Kanellis J, Lan H, et al. Uric Acid, Hominoid Evolution, and the Pathogenesis of Salt-Sensitivity. Hypertension. 2002;40:355–60. doi: 10.1161/01.hyp.0000028589.66335.aa. [DOI] [PubMed] [Google Scholar]
- 25.Kosugi T, Nakagawa T, Kamath D, Johnson RJ. Uric Acid and Hypertension: an Age-Related Relationship? J Hum Hypertens. 2008;23:75–76. doi: 10.1038/jhh.2008.110. [DOI] [PubMed] [Google Scholar]
- 26.Hinchliffe SA, Lynch MR, Sargent PH, Howard CV, Van Velzen D. The Effect of Intrauterine Growth Retardation on the Development of Renal Nephrons. Br J Obstet Gynaecol. 1992;99:296–301. doi: 10.1111/j.1471-0528.1992.tb13726.x. [DOI] [PubMed] [Google Scholar]
- 27.Dagan A, Gattineni J, Cook V, Baum M. Prenatal Programming of Rat Proximal Tubule Na+/H+ Exchanger by Dexamethasone. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1230–R1235. doi: 10.1152/ajpregu.00669.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shirley D, Walter S. Acute and Chronic Changes in Renal Function Following Unilateral Nephrectomy. Kidney Int. 1991;40:62–68. doi: 10.1038/ki.1991.180. [DOI] [PubMed] [Google Scholar]
- 29.Shaltout HA, Figueroa JP, Rose JC, Diz DI, Chappell MC. Alterations in Circulatory and Renal Angiotensin-Converting Enzyme and Angiotensin-Converting Enzyme 2 in Fetal Programmed Hypertension. Hypertension. 2009;53:404–08. doi: 10.1161/HYPERTENSIONAHA.108.124339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goodfellow J, Bellamy MF, Gorman ST, Brownlee M, Ramsey MW, Lewis MJ, et al. Endothelial Function Is Impaired in Fit Young Adults of Low Birth Weight. Cardiovascular Research. 1998;40:600–06. doi: 10.1016/s0008-6363(98)00197-7. [DOI] [PubMed] [Google Scholar]
- 31.McEniery CM, Bolton CE, Fawke J, Hennessy E, Stocks J, Wilkinson IB, et al. Cardiovascular Consequences of Extreme Prematurity: the EPICure Study. J Hypertens. 2011;29:1367–73. doi: 10.1097/HJH.0b013e328347e333. [DOI] [PubMed] [Google Scholar]
- 32.Hovi P, Andersson S, Eriksson JG, Jarvenpaa AL, Strang-Karlsson S, Makitie O, et al. Glucose Regulation in Young Adults With Very Low Birth Weight. N Engl J Med. 2007;356:2053–63. doi: 10.1056/NEJMoa067187. [DOI] [PubMed] [Google Scholar]
- 33.Zhang J, Zhang Y, Deng W, Chen B. Elevated Serum Uric Acid Is Associated With Angiotensinogen in Obese Patients With Untreated Hypertension. The Journal of Clinical Hypertension. 2014;16:569–74. doi: 10.1111/jch.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bae JS, Shin DH, Park PS, Choi BY, Kim MK, Shin MH, et al. The Impact of Serum Uric Acid Level on Arterial Stiffness and Carotid Atherosclerosis: The Korean Multi-Rural Communities Cohort Study. Atherosclerosis. 2013;231:145–51. doi: 10.1016/j.atherosclerosis.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 35.Masuo K, Kawaguchi H, Mikami H, Ogihara T, Tuck ML. Serum Uric Acid and Plasma Norepinephrine Concentrations Predict Subsequent Weight Gain and Blood Pressure Elevation. Hypertension. 2003;42:474–80. doi: 10.1161/01.HYP.0000091371.53502.D3. [DOI] [PubMed] [Google Scholar]